Abstract
Background: Traditional procurement and price negotiation methods in public hospitals in Thailand involve group purchasing agreements and bulk orders, posing challenges to improving inventory management efficiency. The vendor-managed inventory (VMI) model is a promising alternative for enhancing hospital performance, especially during crises. This study aimed to assess the potential cost savings in implementing VMI in a large general hospital in Thailand. Methods: A simulation modeling approach was used to compare the current inventory system with three VMI models: VMI1, focused on improving inventory turnover rate (ITR); VMI2, emphasized frequent replenishment with a 1-month supply; and VMI3, eliminated safety stock. Results: The results demonstrated significant cost savings, with potential reductions in total inventory management expenses. Specifically, VMI1 improved ITR from 6.31 to 7.76, reducing average inventory by 36% and cutting management costs by 40%. VMI2, with an ITR of 12.80, reduced inventory by 44% and saved 47% in management costs, while VMI3 achieved a 70% reduction in inventory and a 69% saving in management costs. Conclusions: This study highlights the VMI’s transformative potential in hospital inventory management, demonstrating significant cost savings. However, in the public sector, the feasibility of procurement regulations requires further exploration.
1. Introduction
Owing to the increasing costs of medicines, pharmacy supplies represent the largest portion of hospital expenses. This financial burden has led hospitals to seek cost-effective inventory management systems that balance overstocking and shortages, ensuring sufficient stock levels at minimal costs while maintaining operational efficiency. Purchasing, inventory management, and waste reduction are key pharmacy activities [].
A recent study in Australia exemplified the benefits of vendor stock management (VSM) systems, reporting substantial enhancements in operational efficiencies with a 51% reduction in stock levels and a 42% decrease in inventory management time. Furthermore, these systems facilitated an annual labor cost savings of USD 550,000, underscoring the potential of advanced inventory solutions to alleviate financial pressures on hospitals [].
To enhance supply chain efficiency, reduce costs, and improve customer satisfaction, vendor-managed inventory (VMI) systems have been adopted as a solution. VMI operates on the principle of collaboration, wherein the supplier is responsible for maintaining appropriate inventory levels in the hospital’s warehouse and autonomously managing replenishments [,]. This approach shifts the burden of inventory management from the hospital to the supplier, fostering improved coordination and efficiency.
Despite the benefits observed in other regions, the application of VMI models in Thailand’s healthcare sector remains limited and under-researched [,,]. Thai hospitals continue to face significant inventory management challenges, characterized by inefficiencies and information inaccuracies due largely to a lack of sophisticated management tools [,]. This gap in effective practice often leads to elevated costs and compromised patient care due to inadequate stock levels [].
This study aimed to address this gap through evaluating impacts of VMI on cost savings and operational efficiency within public hospitals in Thailand. This study sought to provide insights into whether VMI can be a viable solution for improving inventory management and reducing costs in the healthcare system in Thailand using real-world data.
The literature review focuses on effective drug supply chain performance and VMI and its application in hospital settings.
1.1. Supply Chain Coordination in Healthcare
The pharmaceutical supply chain system comprises a network of multiple stakeholders working on a series of processes. It is composed of five core areas including procurement, storage, distribution, dispensing, and utilization. These components play a vital role in ensuring that quality medicines are efficiently delivered to patients []. Key performance indicators, including holding cost, stockout rate, and inventory turnover rate (ITR) are used to assess the efficiency of inventory management practices. Studies have shown that companies with effective inventory management have lower holding costs, reduced stockout rates, and better ITRs [,].
In healthcare settings, supply chain coordination between hospitals and external vendors is essential for optimizing performances, reducing costs and waste, as well as increasing patient satisfaction [,]. VMI, by allowing suppliers to monitor and manage inventory directly at the healthcare facility, has proven to significantly reduce inventory-related costs and improve distribution efficiency [,].
1.2. Benefits and Models of VMI
VMI allows suppliers to access real-time information on inventory levels, sales trends, and other relevant data, enabling informed decisions about inventory replenishment, thereby resulting in a more streamlined and effective inventory management that benefits suppliers and buyers through enhancing accuracy, reducing lead times, and improving supply chain transparency [,].
The following are the five VMI models:
- Vendor-Replenished Inventory (VRI);
- Vendor-Managed Inventory Services (VMIS);
- Third Party-Replenished Inventory (3RI);
- Third Party-Managed Inventory Services (3MIS);
- Inventory Management Technical Assistance (IMTA).
The first four models involve either true vendors or third parties managing inventory with varying levels of additional services. The fifth model, IMTA, provides technical assistance along with inventory services, regardless of whether the service is from a true vendor or a third party. The 3MIS model is an advanced VMI system where inventory replenishment and additional management services are assigned to a third party, adding a layer of intermediation between customers and suppliers. This model offers adaptability and effectiveness; however, the selection and handling of the third party plays a pivotal role in its success [].
While the primary goal of VMI implementation is to cut down the operation costs, it is important to note that it must not affect the quality of the products [,,]. To ensure that quality is not compromised during cost negotiations, hospitals can implement several strategies [,], including:
- Strict Quality Control Measures: Enforcing strict quality-control standards through well-defined contractual agreements that specify quality expectations.
- Supplier Audits and Performance Reviews: Regularly auditing and reviewing supplier performance to ensure compliance with quality standards.
- Collaborative Relationships: Establishing a collaborative relationship with suppliers, like the strategies in trade credit models. This ensures that both parties prioritize quality in addition to cost efficiency. This approach is supported by the findings of Zavanella and Zanoni [], which discussed the success of integrating VMI with consignment agreements to benefit both buyers and vendors through maintaining high-quality standards while managing costs effectively.
It is important to note that the objective of VMI is not to compel vendors into reducing drug prices but to minimize excessive or unnecessary operational costs. The focus of this study’s savings was on reducing capital costs through lower average inventory volumes, improved inventory turnover rates (ITRs), and reduced holding and procurement expenses.
1.3. Application of VMI in Hospitals
Hospitals experience significant challenges in managing their supply chains and inventory. To address these issues, researchers have introduced various strategies for improving inventory management, including the VMI model. VMI empowers suppliers to take a proactive role in inventory management to make informed decisions about inventory reinforcement and timing based on real-time data. This model incorporates a third party that is responsible for replenishment via sharing demand information with the supplier.
The adoption of VMI is underscored by its ability to improve data collection methods and establish robust electronic communication systems between hospitals and suppliers. These enhancements are crucial for reducing inventory costs, minimizing administrative burdens, lowering error rates, and improving the reliability of information []. VMI systems enable vendors to access real-time hospital inventory data, ensuring continuous medical supply replenishment. This capability allows healthcare organizations to optimize their stock levels effectively, ensuring they are well-equipped to meet patient needs without surplus. Moreover, VMI contributes to a competitive advantage through enhancing the efficiency of physical distribution, reducing lead time variability, and lowering transportation costs. It also improves warehouse operations and adds flexibility to purchasing processes []. Despite these benefits, the implementation of VMI is not without challenges. Issues such as low trust and dependability on suppliers, the significant investment required for IT infrastructure, lengthy purchasing processes, and the lack of controlling authority over suppliers can hinder the effectiveness of VMI systems. Additionally, hospitals must navigate challenges related to accurately forecasting supplier sales, which can impact the overall success of VMI implementation. By addressing these obstacles, hospitals can better leverage VMI to streamline their inventory management and enhance overall supply chain performance.
2. Materials and Methods
This section outlines the study design, details of the case study hospital, and the development and validation of the simulation models used to analyze inventory management costs under different scenarios.
2.1. Study Design
This study used the simulation modeling approach to compare the inventory management costs between the current practice and three VMI models in a large general hospital in Thailand. The hospital had a capacity of 602 inpatient beds, 1750 employees, and 47 pharmacists. The pharmacy department managed five dispensing units and a procurement and inventory management unit. The study aimed to evaluate the efficiency and costs of different inventory management systems within this setting.
- Simulation Modeling Approach
Two simulation models were developed, one representing the current inventory management practice and the other representing the VMI approach. The model for the current practice was based on actual procurement and inventory data from the hospital, ensuring an accurate representation of existing operations. The VMI model was constructed using expert opinions and hospital inventory statistics to simulate inventory-related parameters. This approach enabled a direct cost comparison between the current practice and the proposed VMI models.
2.2. Data Collection and Preparation
Data for each medication item were collected from the hospital’s inventory database, including drug name, beginning-of-year volume, end-of-year volume, unit price, and annual procurement volume. All data, except for drug names, were quantitative and related to the hospital’s current inventory.
Data cleaning was conducted to ensure the correct formatting and completeness of the dataset. Missing inventory turnover rate (ITR) values for each medication were identified. The average ITR for the entire inventory was calculated and used to impute the missing ITR values for individual items. Once the ITR was imputed, any missing data for other variables were subsequently computed based on the imputed ITR, ensuring a consistent and reliable dataset for further analysis.
2.3. Model Development and Validation
Two additional sets of variables—performance variables and process variables—were calculated to facilitate the comparison between the current practice and the VMI models.
- Performance Variables
These included annual procurement value, actual average inventory volume and value, annual use rate and value, and ITR. Each variable’s definition and operationalization were based on established inventory management principles [].
- Process Variables
Variables, including safety stock level, reorder point, minimum/maximum/average stock levels and estimated procurement, were calculated using specific equations tailored to the hospital’s context []. These helped to maintain adequate inventory levels, minimizing both stockouts and excess inventory.
The simulation model for the current practice was validated by adjusting process variables to align simulated results with actual hospital data, specifically total annual medicine procurement and average inventory values. This validation step ensured the model’s accuracy in reflecting real-world conditions.
Scenarios of VMI Model Development
Three VMI scenarios were simulated through the following:
- VMI1 Model: This model aimed to enhance efficiency for items with lower turnover rates by targeting items with below-average ITR, adjusting purchase volumes to achieve an average ITR while maintaining annual medicine procurement values consistent with the current model.
- VMI2 Model: This model aimed to reduce holding costs and ensure timely availability of medicines through implementing more frequent replenishments to maintain a 1-month supply for each order.
- VMI3 Model: This scenario eliminated safety stock via automatically reordering once stock levels reached a minimum threshold thus minimizing stockouts and excess inventory.
2.4. Cost Analysis of Inventory Management
Costs associated with inventory management, including procurement and holding costs, were calculated using activity-based costing [,]. Holding costs were estimated at approximately 25% of the average inventory values [] and procurement costs varied depending on the methods used by the hospital:
- The Current Model utilized group purchasing to procure 400 items annually and a special procurement method for the remaining 500 items, requiring individual processing.
- The VMI Models employed a fixed procurement cost with automated transaction, eliminating traditional procurement processes.
The flow chart (Figure 1) and Table 1 and Table 2 provide a detailed description of the simulation model development and the operational definitions for performance and process variables.
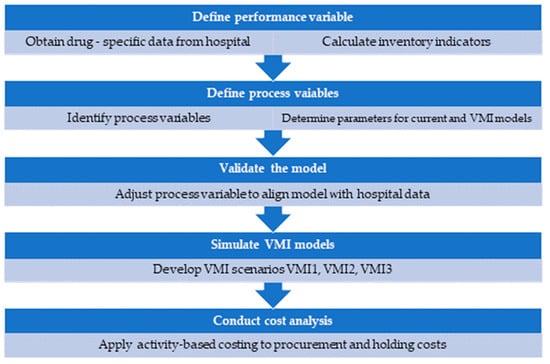
Figure 1.
Flow chart of simulation model development.

Table 1.
Description of the performance variables used in the simulation model.

Table 2.
Description of the process variables used in the simulation model.
3. Results
This section details the comparative analysis of the current inventory management system and the three VMI scenarios. The analysis focuses on key metrics including ITRs, average inventory values, and overall cost savings.
3.1. Performance of Current Inventory Management System
The current inventory system at the hospital was validated using actual procurement and inventory data. The simulation reported an ITR of 6.31, closely aligning the hospital’s current data. The established reorder point was set at 20 days, with a safety stock of 15 days and a lead time of 5 days. The system maintained an average inventory value of approximately USD 1.6 million, with total procurement costs amounting to USD 76,921 annually.
3.2. Performance of VMI Scenarios
VMI1 Model:
- Objective: Enhance efficiency for items with low ITR.
- Results: This model increased the ITR to 7.76, reducing the average inventory value by 36% from USD 1.6 million to USD 1.01 million. It demonstrated significant improvements in managing low turnover items.
VMI2 Model:
- Objective: Maintain a 1-month supply with more frequent replenishments.
- Results: The ITR further increased to 12.80, reducing the average inventory value by 44% from the current model and 13% from the VMI1 model. This model balanced inventory reduction with a timely availability of medicines.
VMI3 Model:
- Objective: Minimize safety stock with automatic reordering at minimum levels.
- Results: The inventory was reduced by 70% compared to the current model and by over 50% compared to the VMI1 model, maintaining an ITR of 12.80. This model demonstrated significant cost savings by minimizing safety stock.
The parameters used in the simulation across all models are summarized in Table 3, outlining adjustments in safety stock, reorder points, and inventory values.

Table 3.
Parameters in the current simulation and VMI models.
3.3. Cost Analysis of Inventory Management
Current Model Costs: Total inventory management cost was USD 488.5 K with procurement activities forming a significant portion due to frequent orders (over 3000), with individual order costs ranging from USD 4.64 to USD 11.60, depending on the procurement method.
VMI Models Costs:
- VMI1 reduced total costs by 40% to USD 295.1 K primarily through fixed management and lower order processing costs.
- VMI2 further decreased costs by 47%, aligning with the model’s strategy of a 1-month supply and lower inventory holding.
- VMI3 achieved a 70% reduction in inventory costs and a 69% reduction in total holding and capital costs by eliminating safety stock.
Cost comparisons between the current and VMI models are detailed in Table 4 and Table 5, highlighting reductions in procurement, holding, and capital costs.

Table 4.
Cost comparison between the current and VMI models.

Table 5.
Comparison of costs between models with adjusted inventory turnover rate (ITR) and safety stock levels.
3.4. Summary of Key Findings
The analyses illustrate that all VMI models yielded substantial cost savings and efficiency improvements compared to the current inventory management system. VMI1 provided moderate improvements, while VMI2 and VMI3 provided more aggressive strategies, leading to significant reductions in costs and more streamlined operations across the hospital’s supply chain.
4. Discussion
This section addresses the benefits and challenges of implementing VMI models in hospital inventory management, focusing on financial impact, comparative performance in different context, demand variability, real-world challenges, impact on patient care, and data security.
Implementing VMI models in hospital inventory management has shown significant performance enhancements, marking a novel strategy in the healthcare industry. This study reveals marked reductions in total procurement, holding, and capital costs. Although VMI incurs higher order processing costs for supplier selection, these are annual costs, contrasting with the frequent expenditures in the current model. These findings align with previous studies, such as those by Sharma and Singhi, which reported significant improvements in ITRs and cost savings in Indian hospitals following VMI implementation [].
VMI performance can vary based on the specific context. Recent research demonstrated that integrating VMI with vehicle route planning can optimize distribution networks, significantly reducing transportation and inventory costs []. However, other studies have shown less pronounced improvement, depending on the different environmental and operational conditions. For example, Krichanchai and MacCarthy reported that VMI reduced errors and process inefficiencies without substantial IT investments. Similar outcomes were observed in studies where VMI, supported by Internet of Things (IoT), improved time efficiency by over 95% []
This study acknowledges high medicine demand variability due to seasonal illnesses and epidemics. The simulation model incorporates safety stock levels to buffer against demand fluctuations.
VMI implementation experiences real-world challenges. A case study in a public hospital in Thailand highlighted the significance of trust, information sharing, and IT in supplier selection for VMI []. Establishing trust between hospitals and vendors is crucial, as vendor reliability, quality assurance, and timely deliveries impact VMI success. To address data accuracy, system integration, and initial IT infrastructure investment challenges, accurate inventory data and robust IT systems are essential []. Transitioning to VMI involves additional management costs and organizational changes, necessitating effective change management strategies. Furthermore, outsourcing inventory management increases regulatory and compliance challenges that must be carefully managed.
By streamlining inventory management, VMI reduces the administrative workload on hospital staff, allowing them to focus more on patient care rather than inventory tasks []. Additionally, VMI ensures that high-quality products are available when needed, which minimizes the risk of product expiration and stockouts []. This reliability in inventory helps prevent interruptions in the availability of essential medications and medical supplies, thereby supporting timely and effective patient care. Overall, the VMI model contributes to improved operational efficiency and patient safety by ensuring that critical supplies are consistently available and reducing the time staff spend on inventory management. These benefits underscore the broader advantages of VMI in enhancing the quality of patient care [].
Data security and privacy are critical in implementing VMI systems, especially in sensitive settings like healthcare. Effective data sharing between hospitals and vendors must be balanced with strong security measures. Traditional methods, such as formal contracts and clearly defined vendor responsibilities, are essential for safeguarding sensitive information []. As VMI systems increasingly rely on data sharing, integrating advanced security technologies, such as privacy-preserving data publishing (PPDP) techniques and blockchain technology, could address data integrity and security of sensitive information [,].
To ensure successful VMI implementation, it is crucial to balance between benefits with potential challenges and regulatory considerations. Hospitals should adopt a phased approach, starting with a pilot project to reduce risks and establish relationships with vendors. This transition can be supported by policymakers through developing clear regulatory frameworks that facilitate vendor partnerships. Establishing robust IT infrastructure and ensuring accurate inventory data are also critical steps for successful VMI implementation.
- Contributions of the Study:
This study provides valuable insights into the implementation and impact of VMI models in hospital settings. Our research evaluates various VMI scenarios, demonstrating their potential to achieve significant cost savings and improve inventory management efficiency, especially in resource-constrained environments. Key contributions include:
- Empirical Evidence: The study provides empirical evidence of the effectiveness of VMI models in enhancing inventory turnover rates (ITR) and reducing inventory holding costs. This evidence supports the practical application of VMI in improving hospital inventory management.
- Customized Strategies: The study highlights the importance of tailored inventory management strategies, such as the elimination of safety stock, which can lead to greater operational efficiency. The study also emphasizes the need for customized VMI approaches to address specific challenges and optimize inventory practices.
- Study Limitations
This study primarily relied on a single supplier to manage the hospital’s entire inventory for the year. While this approach can streamline operations and reduce complexity, it also increases the risk of supply chain disruptions in the event of supplier failure or emergencies. Additionally, unpredictable circumstances, such as geopolitical tensions, natural disasters, or pandemics, which can significantly affect the efficiency of inventory management and VMI systems, were not explored.
- Future Research
Future research should explore issues such as the following:
- The detailed cost structures and categories of medicines and supplies suitable for VMI.
- The levels of information sharing and hospital readiness for VMI implementation.
- Regulations necessary to support comprehensive VMI implementation, particularly for public hospitals.
- The long-term sustainability of VMI models.
- The integration of AI and real-time optimization tools to assess their impact on reducing stockouts and waste in VMI systems.
5. Conclusions
This study demonstrates that VMI models can effectively reduce total inventory management and capital inventory costs in a hospital setting while improving inventory management performance and customer satisfaction. The findings emphasize the importance of the careful evaluation of procurement regulations and associated costs before adopting VMI. Hospitals and suppliers must prioritize data security and transparency in their VMI partnerships. A comprehensive assessment of the existing supply chain systems is necessary to determine the suitability of the VMI model for specific hospital needs, ensuring a smooth implementation process and optimal outcomes.
Author Contributions
Conceptualization, S.A., A.T. and R.C.S.; methodology, S.A. and R.C.S.; software, S.A.; validation, S.A., A.T. and R.C.S.; formal analysis, S.A. and R.C.S.; investigation, S.A.; resources, S.A. and R.C.S.; data curation, S.A.; writing—original draft preparation, S.A.; writing—review and editing, R.C.S.; visualization, S.A.; supervision, R.C.S.; project administration, S.A.; funding acquisition, S.A. and R.C.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research is supported by the 90th Anniversary of Chulalongkorn University, Rachadapisek Sompote Fund, grant number [GCUGR1125613041D]. I also would like to express my appreciation to the Chulalongkorn University Graduate Scholarship to commemorate the 72nd Anniversary of His Majesty King Bhumibol Adulyadej for their joint support through the Pharmaceutical Science Ph.D. Program.
Data Availability Statement
The data generated and analyzed in this study are available from the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Monton, C.; Charoenchai, L.; Suksaeree, J. Purchasing and Inventory Management by Pharmacist of a Private Hospital in Northeast of Thailand. Int. J. Pharm. Pharm. Sci. 2014, 6, 401–405. [Google Scholar]
- Khalil, V.; Foo, S. A Lean Approach for Improving Medicines Management in Australia’s First Cardiac Hospital Inventory System. Int. J. Health Plann Manag. 2024, 39, 1642–1651. [Google Scholar] [CrossRef] [PubMed]
- Krichanchai, S.; MacCarthy, B.L. The Adoption of Vendor Managed Inventory for Hospital Pharmaceutical Supply. Int. J. Logist. Manag. 2017, 28, 755–780. [Google Scholar] [CrossRef]
- van den Bogaert, J.; van Jaarsveld, W. Vendor-Managed Inventory in Practice: Understanding and Mitigating the Impact of Supplier Heterogeneity. Int. J. Prod. Res. 2022, 60, 6087–6103. [Google Scholar] [CrossRef]
- Sharma, N.; Singhi, R. Performance Evaluation of Vendor Managed Inventory Variables in Hospitals Using ANOVA Technique. Int. J. Supply Chain Inventory Manag. 2018, 3, 66. [Google Scholar] [CrossRef]
- Sumrit, D. Understanding Critical Success Factors of Vendor-Managed Inventory in Healthcare Sector: A Case Study in Thailand. Int. J. Healthc. Manag. 2021, 14, 629–640. [Google Scholar] [CrossRef]
- Kritchanchai, D. A Framework for Healthcare Supply Chain Improvement in Thailand. Oper. Supply Chain Manag. Int. J. 2014, 5, 103–113. [Google Scholar] [CrossRef]
- Kanyakam, S.; Pimpa, W.; Kamlai, K. Inventory Management in Medical Stores of Secondary Care Unit Service Level Hospitals in Northeast of Thailand. Eng. Access 2018, 4, 17–23. [Google Scholar] [CrossRef]
- World Health Organization Health Products Policy and Standards. Available online: https://www.who.int/teams/health-product-policy-and-standards/medicines-selection-ip-and-affordability/medicines-policy/medicines-supply (accessed on 27 June 2024).
- Williams, B.D.; Tokar, T. A Review of Inventory Management Research in Major Logistics Journals: Themes and Future Directions. Int. J. Logist. Manag. 2008, 19, 212–232. [Google Scholar] [CrossRef]
- Panigrahi, R.R.; Shrivastava, A.K.; Kapur, P.K. Impact of Inventory Management Practices on the Operational Performances of SMEs: Review and Future Research Directions. Int. J. Syst. Assur. Eng. Manag. 2024, 15, 1934–1955. [Google Scholar] [CrossRef]
- Arshinder; Kanda, A.; Deshmukh, S.G. Supply Chain Coordination: Perspectives, Empirical Studies and Research Directions. Int. J. Prod. Econ. 2008, 115, 316–335. [Google Scholar] [CrossRef]
- Li, X.; Wang, Q. Coordination Mechanisms of Supply Chain Systems. Eur. J. Oper. Res. 2007, 179, 1–16. [Google Scholar] [CrossRef]
- Achabal, D.D.; McIntyre, S.H.; Smith, S.A.; Kalyanam, K. A Decision Support System for Vendor Managed Inventory. J. Retail. 2000, 76, 430–454. [Google Scholar] [CrossRef]
- Zhao, R. A Review on Theoretical Development of Vendor-Managed Inventory in Supply Chain. Am. J. Ind. Bus. Manag. 2019, 9, 999–1010. [Google Scholar] [CrossRef]
- Kong, H.; Feng, D.; Fan, W.; Li, Q. Design and Implementation of Pharmaceutical Logistics and Supply Chain Management System for Hospital. In Proceedings of the 2015 International Conference on Advances in Mechanical Engineering and Industrial Informatics, Zhengzhou, China, 11–12 April 2015; Atlantis Press: Paris, France, 2015. [Google Scholar]
- Watson, N.; Serumaga, B.; McCord, J. Selecting and Implementing Vendor Managed Inventory Systems for Public Health Supply Chains; International Association of Public Health Logisticians: Arlington, VA, USA, 2012. [Google Scholar]
- Chen, B.; Xie, W.; Huang, F.; He, J. Quality Competition and Coordination in a VMI Supply Chain with Two Risk-Averse Manufacturers. J. Ind. Manag. Optim. 2021, 17, 2903. [Google Scholar] [CrossRef]
- Gümüş, M.; Jewkes, E.M.; Bookbinder, J.H. Impact of Consignment Inventory and Vendor-Managed Inventory for a Two-Party Supply Chain. Int. J. Prod. Econ. 2008, 113, 502–517. [Google Scholar] [CrossRef]
- Abad, P.L.; Jaggi, C.K. A Joint Approach for Setting Unit Price and the Length of the Credit Period for a Seller When End Demand Is Price Sensitive. Int. J. Prod. Econ. 2003, 83, 115–122. [Google Scholar] [CrossRef]
- Zavanella, L.; Zanoni, S. A One-Vendor Multi-Buyer Integrated Production-Inventory Model: The ‘Consignment Stock’ Case. Int. J. Prod. Econ. 2009, 118, 225–232. [Google Scholar] [CrossRef]
- Chopra, S.; Meindl, P. Supply Chain Management: Strategy, Planning, and Operation; Pearson: London, UK, 2016; ISBN 9780133800203. [Google Scholar]
- Kaplan, R.S.; Anderson, S.R. Time-Driven Activity-Based Costing. Harv. Bus. Rev. 2004, 82, 131–138, 150. [Google Scholar] [CrossRef]
- Law, A.M.; Kelton, W.D. Simulation Modeling and Analysis; Mcgraw-Hill: New York, NY, USA, 2014. [Google Scholar]
- Durlinger, P. Inventory and Holding Costs; Durlinger Consultancy: Posterholt, The Netherlands, 2015. [Google Scholar]
- Badi, I.; Bouraima, M.B.; Stević, Ž.; Oloketuyi, E.A.; Makinde, O.O. Optimizing Vendor-Managed Inventory in Multi-Tier Distribution Systems. Spectr. Oper. Res. 2024, 1, 33–43. [Google Scholar] [CrossRef]
- Joseph, J.F.; Sundarakani, B.; Hosie, P.; Nagarajan, S. Analysis of Vendor Managed Inventory Practices for Greater Supply Chain Performance. Int. J. Logist. Econ. Glob. 2010, 2, 297. [Google Scholar] [CrossRef]
- Brummelhuis, B. Coping with Variability: Improving the Inbound Process of the VMI Holland Warehouse. Master’s Thesis, University of Twente, Enschede, The Netherlands, 2016. [Google Scholar]
- Ganesan, S.; Wicaksono, H.; Fatahi Valilai, O. Enhancing Vendor Managed Inventory with the Application of Blockchain Technology. In Advances in System-Integrated Intelligence; Springer: Cham, Switzerland, 2023; Volume 546, pp. 262–275. [Google Scholar] [CrossRef]
- Viswanadham, Y.V.R.S.; Jayavel, K. A Framework for Data Privacy Preserving in Supply Chain Management Using Hybrid Meta-Heuristic Algorithm with Ethereum Blockchain Technology. Electronics 2023, 12, 1404. [Google Scholar] [CrossRef]
- Zingirian, N. Privacy-Preserving Data Publishing in Small-Sized Business Communities. In Proceedings of the 2023 International Conference on Computational Intelligence, Networks and Security (ICCINS), Mylavaram, India, 22–23 December 2023; pp. 1–6. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).