Competencies of a Healthcare Manager in the Context of Hospital and Ambulateral Diagnostic Imaging Centers
Abstract
1. Introduction
2. Purpose of the Article
3. Materials and Methods
3.1. Research Techniques and Tools
3.2. Characteristics of the Study Group
4. Results
4.1. Survey Results
4.2. In-Depth Interview Results
5. Discussion
- The Global Consortium for Healthcare Management Professionalization (a consortium created by The International Hospital Federation)—developed the Competency Directory Model indicating five important domains, i.e., “leadership, communication and relationship management, professional and social responsibility, health and healthcare environment and skills business”.
- National Center for Healthcare Leadership (NCHL) [2005], based on research conducted by the Hay Group with the participation of managers of healthcare organizations. The NCHL competency model contains three domains, as follows:
- a
- “transformation—achievement orientation, analytical thinking, social orientation, strategic orientation, innovative thinking,
- b
- implementation—responsibility, cooperation, communication, initiative, organizational awareness,
- c
- people—human resources management, professionalism, relationship building, self-development, and talent development, team leadership”.
| Article | Type of Research | Research Results |
|---|---|---|
| Burak A., Mućka J., Ferenc A. (2015), Specyfika zachowań przywódczych kadry kierowniczej współczesnej ochrony zdrowia (The specificity of leadership behaviors of the management staff of modern healthcare—own translation) [29] | A survey among hospital managers | According to respondents, maintaining the quality of services at the highest possible level was considered the most important attribute |
| Striker M. (2016), Zmiany w postrzeganiu ról zawodowych menedżerów medycznych w publicznym szpitalu (Changes in the perception of professional roles of medical managers in a public hospital—own translation) [42] | A survey among medical staff of two hospital departments | A difference in the perspective on management competencies between nurses and doctors was demonstrated, although the most important competencies were combining management and medical functions to be an efficient manager |
| Wysocka, M. and Lewandowski, R. (2017). Key competences of a health care manager [44] | A survey among study participants and healthcare workers | Professional competence in the field of organization and management dominates; these competencies were also diagnosed as those with the greatest deficiencies, hindering effective work |
| Bebel D. (2019), Ocena kompetencji menedżerskich kadry zarządzającej podmiotami leczniczymi (Assessment of managerial competences of management staff of healthcare entities—own translation) [35] | A survey among medical and administrative staff in hospitals | The importance of soft skills and their insufficient level among managers were pointed out |
| Manuszek M. (2019). Profile kompetencyjne menedżerów sektora publicznego (Competency profiles of public sector managers—own translation) [44] | Based on the competency profiles, the most important competencies were identified | The need for further, diverse research was indicated, and the development of ethical and moral values was considered very important, as well as the significance of the manager having formal and informal authority |
| Krawczyk-Sołtys A. (2019), Kompetencje menedżerskie w kształtowaniu kompetencji organizacyjnych jednostek ratownictwa medycznego w świetle badań (Managerial competences in shaping the organizational competences of emergency medical services units in the light of research—own translation) [43] | A survey among medical personnel of emergency medical units | The greatest importance was given to business, professional and social competencies |
| Sexton J.B., Adair K.C., Profit J. et al. (2021). Safety Culture and Workforce Well-Being Associations with Positive Leadership WalkRounds [45] | A survey among medical and non-medical academic staff | The importance of patient safety, willingness to engage in quality improvement activities, good accessibility of leaders, and their constructive feedback were appreciated |
| Bairros da Silva L., Sousa M.H.O. and Iniguez-Rueda L. (2022), Managers’ Views on Professional Competencies for Primary Health Care [46] | Qualitative study—semi-structured interviews among primary healthcare employees | The following competencies were distinguished: emotional preparation, leadership, active attitude, empathetic availability and professional self-fulfillment, and responsibility |
- Supervising the offer preparation process;
- Selection of customer groups to which the message will be addressed;
- Selection of the most effective and correlated with budget possibilities and forms of communication.
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Kakemam, E.; Liang, Z.; Janati, A.; Arab-Zozani, M.; Mohaghegh, B.; Gholizadeh, M. Leadership and Management Competencies for Hospital Managers: A Systematic Review and Best-Fit Framework Synthesis. J. Healthc. Leadersh. 2020, 12, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Feldman, S.S.; Allgood, A.; Hall, A.G.; Lemak, C.H.; Berner, E.S. Competency analysis and educational strategies to meet the demand for a learning health system workforce. Learn. Health Syst. 2022, 6, e10324. [Google Scholar] [CrossRef]
- Parikh, P.; Klanderman, M.; Teck, A.; Kunzelman, J.; Banerjee, I.; DeYoung, D.; Hara, A.; Tan, N.; Yano, M. Effects of patient demographics and examination factors on patient experience in outpatient MRI appointments. J. Am. Coll. Radiol. 2024, 21, 601–608. [Google Scholar] [CrossRef]
- Verboeket, V.; Krikke, H.; Salmi, M. Implementing Additive Manufacturing in Orthopedic Shoe Supply Chains—Cost and Lead Time Comparison. Logistics 2024, 8, 49. [Google Scholar] [CrossRef]
- Božić, D.; Šego, D.; Stanković, R.S.; Šafran, M. Logistics in healthcare: A selected review of literature from 2010 to 2022. Transp. Res. Procedia 2022, 64, 288–298. [Google Scholar] [CrossRef]
- Nanda, S.K.; Panda, S.K.; Dash, M. Medical supply chain integrated with blockchain and IoT to track the logistics of medical products. Multimed. Tools Appl. 2023, 82, 32917–32939. [Google Scholar] [CrossRef] [PubMed]
- Alipour-Vaezi, M.; Aghsami, A.; Jolai, F. Prioritizing and queueing the emergency departments’ patients using a novel data-driven decision-making methodology, a real case study. Expert Syst. Appl. 2022, 195, 116568. [Google Scholar] [CrossRef] [PubMed]
- Nosrati-Abarghooee, S.; Sheikhalishahi, M.; Nasiri, M.M.; Gholami-Zanjani, S.M. Designing reverse logistics network for healthcare waste management considering epidemic disruptions under uncertainty. Appl. Soft Comput. 2023, 142, 110372. [Google Scholar] [CrossRef] [PubMed]
- Jarzynkowski, P.; Książek, J.; Piotrkowska, R. Specyfika procesów logistycznych ochrony zdrowia w Polsce. Logistyka 2016, 5, 13–16. [Google Scholar]
- Oborska-Kumaszyńska, D. Zarządzanie Wyposażeniem do Radioterapii. In Proceedings of the V Konferencja z Zakresu Detekcji Promieniowania Jonizujacego Oraz Kontroli Jakości w Rentgenodiagnostyce, Radioterapii i Medycynie Nuklearnej, Klimkówka, Poland, 5–9 September 2022; Available online: https://www.researchgate.net/publication/364587544 (accessed on 22 September 2024).
- Zhou, Y.; Song, L.; Liu, Y.; Vijayakumar, P.; Gupta, B.B.; Alhalabi, W.; Alsharif, H. A privacy-preserving logistic regression-based diagnosis scheme for digital healthcare. Future Gener. Comput. Syst. 2023, 144, 63–73. [Google Scholar] [CrossRef]
- Hussain, S.; Mubeen, I.; Ullah, N.; Shah, S.S.U.D.; Khan, B.A.; Zahoor, M.; Ullah, R.; Khan, F.A.; Sultan, M.A. Modern Diagnostic Imaging Technique Applications and Risk Factors in the Medical Field: A Review. Biomed Res Int. 2022, 2022, 5164970. [Google Scholar] [CrossRef] [PubMed]
- Beker, K.; Garces-Descovich, A.; Mangosing, J.L.; Cabral-Goncalves, I.; Hallett, D.; Mortelé, K.J. Optimizing MRI logistics: Prospective analysis of performance, efficiency, and patient throughput. Am. J. Roentgenol. 2017, 209, 836–844. [Google Scholar] [CrossRef]
- Alivia Onkofundacja. Available online: https://alivia.org.pl/aktualnosci/krotkie-kolejki-do-badan-zalezy-gdzie-mieszkasz/ (accessed on 18 April 2024).
- Alivia Onkoskaner. Available online: https://onkoskaner.pl/ (accessed on 18 April 2024).
- Brownell, J. Leading on land and sea: Competencies and context. Int. J. Hosp. Manag. 2008, 27, 137–150. [Google Scholar] [CrossRef]
- Duarte, R.G. The development of transversal competence of health service managers. Rev. De Saúde Pública 2019, 53, 53–74. [Google Scholar] [CrossRef]
- Dobska, M. Zarządzanie w Opiece Zdrowotnej w Czasie COVID-19; Wydawnictwo Uniwersytetu Ekonomicznego w Poznaniu: Poznań, Poland, 2021. [Google Scholar] [CrossRef]
- Song, E.Y.; Chuang, J.; Frakes, J.M.; Dilling, T.; Quinn, J.F.; Rosenberg, S.; Johnstone, P.; Harrison, L.; Hoffe, S.E. Developing a Dedicated Leadership Curriculum for Radiation Oncology Residents. J. Cancer Educ. 2021, 37, 1446–1453. [Google Scholar] [CrossRef]
- Kelm, H.; Szymaniec-Mlicka, K. Od Industry 4.0 do Society 5.0—Wyzwania dla zarządzania. In Zarządzanie Publiczne. Perspektywa Teorii i Praktyki; Frączkiewicz-Wronka, A., Ćwiklicki, M., Eds.; Wydawnictwo Uniwersytetu Ekonomicznego w Katowicach: Katowice, Poland, 2023; pp. 272–297. [Google Scholar]
- Sidor-Rządkowska, M. Zarządzanie zasobami ludzkimi w szpitalach publicznych—Problemy i wyzwania. Stud. I Pr. Kol. Zarządzania I Finans. 2019, 167, 127–141. [Google Scholar] [CrossRef]
- Barsbay, M.C.; Öktem, M.K. The Competency Movement in Public Hospitals: Analysing the Competencies of Hospitalhh Executive Managers. Transylv. Rev. Adm. Sci. 2021, 17, 22–43. [Google Scholar] [CrossRef]
- Detyna, B. Dojrzałość Procesowa Szpitali a Jakość Usług Medycznych; Wydawnictwo Politechniki Częstochowskiej: Częstochowa, Poland, 2020. [Google Scholar]
- Muryjas, P. Business Intelligence w zarządzaniu współczesnymi zakładami opieki zdrowotnej. Roczniki Kolegium Analiz Ekonomicznych. Technol. Inform. W Służbie Zdrowia 2014, 35, 273–290. Available online: https://rocznikikae.sgh.waw.pl/p/roczniki_kae_z35_17.pdf (accessed on 17 January 2024).
- Pye, A. Management competence in the public sector. Public Money Manag. 1988, 8, 62–64. [Google Scholar] [CrossRef]
- Rostkowski, T.; Strzemiński, J. Przywództwo w systemie ochrony zdrowia. Educ. Econ. Manag. 2019, 51, 133–144. [Google Scholar] [CrossRef]
- Strudsholm, T.; Vollman, A.R. Public health leadership: Competencies to guide practice. Healthc. Manag. Forum 2021, 34, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Walsh, A.; Harrington, D.; Hines, P. Are hospital managers ready for value-based healthcare? Int. J. Organ. Anal. 2020, 28, 49–65. [Google Scholar] [CrossRef]
- Burak, A.; Mućka, J.; Ferenc, A. Specyfika zachowań przywódczych kadry kierowniczej współczesnej ochrony zdrowia. Piel. Zdr. Public Health 2015, 5, 53–65. Available online: https://omega.umk.pl/info/article/UMKbd94b29bb77d40ecb88f0bca512ad83f?r=publication&ps=20&tab=&title=Publikacja%2B%25E2%2580%2593%2BSpecyfika%2Bzachowa%25C5%2584%2Bprzyw%25C3%25B3dczych%2Bkadry%2Bkierowniczej%2Bwsp%25C3%25B3%25C5%2582czesnej%2Bochrony%2Bzdrowia%2B%25E2%2580%2593%2BUniwersytet%2BMiko%25C5%2582aja%2BKopernika%2Bw%2BToruniu&lang=pl (accessed on 17 January 2024).
- Borkowski, S.; Rosak-Szyrocka, J. Jakość i Satysfakcja w Usługach Medycznych; Wydawnictwo PTM: Warszawa, Poland, 2020. [Google Scholar]
- Ciekanowski, Z. Rola menedżera w organizacji. Zesz. Nauk. Uniw. Przyr.-Humanist. W Siedlcach. Adm. I Zarządzanie 2015, 34, 185–195. Available online: https://bazekon.uek.krakow.pl/en/rekord/171410543 (accessed on 9 September 2024).
- Ćwiklicki, M. Tworzenie wartości publicznej jako cel zarządzania publicznego. In Zarządzanie Publiczne. Perspektywa Teorii i Praktyki; Frączkiewicz-Wronka, A., Ćwiklicki, M., Eds.; Wydawnictwo Uniwersytetu Ekonomicznego w Katowicach: Katowice, Poland, 2023; pp. 272–297. [Google Scholar]
- Baran, K.; Mazur, S.; Tyrańska, M.; Żabiński, M. Przywództwo w organizacjach publicznych. In Zarządzanie Publiczne. Perspektywa Teorii i Praktyki; Frączkiewicz-Wronka, A., Ćwiklicki, M., Eds.; Wydawnictwo Uniwersytetu Ekonomicznego w Katowicach: Katowice, Poland, 2023; pp. 272–297. [Google Scholar]
- Gilson, L.; Agyepong, I.A. Strengthening health system leadership for better governance: What does it take? Health Policy Plan. 2018, 33 (Suppl. 2), ii1–ii4. [Google Scholar] [CrossRef] [PubMed]
- Bebel, D. Ocena kompetencji menedżerskich kadry zarządzającej podmiotami leczniczymi. Zesz. Stud. Ruchu Nauk. W Kielc. 2019, 28, 13–21. Available online: https://zeszytysrn.ujk.edu.pl/wp-content/uploads/2020/04/Zeszyty-Studenckiego-Ruchu-Naukowego_t_28_cz_1.pdf#page=13 (accessed on 17 January 2024).
- Bittencourt, J.P.; Duim, E.; Godoi, D.F.; Hasner, M.S.; Lobo, N.R.; Nielsen, F.A.G. Frameworks, competencies, and evaluation: The different conceptual perspectives and challenges for defining the required skills of a healthcare manager. TechRxiv 2023. [Google Scholar] [CrossRef]
- Howard, P.; Liang, Z.; Leggat, S.G.; Karimi, L. Validation of a management competency assessment tool for health service managers. J. Health Organ. Manag. 2018, 32, 113–134. [Google Scholar] [CrossRef]
- Calhoun, J.G.; Dollett, L.; Sinioris, M.E.; Wainio, J.A.; Butler, P.; Griffith, J.R.; Warden, G.L. Development of an interprofessional competency model for healthcare leadership. J. Healthc. Manag. 2008, 53, 375–389. [Google Scholar] [CrossRef] [PubMed]
- Stefl, M.E. Common competencies for all healthcare managers: The healthcare leadership alliance model. J. Healthc. Manag. 2008, 53, 360–373. [Google Scholar] [CrossRef] [PubMed]
- Health 2020. A European Policy Framework and Strategy for 21st Century; WHO: Copenhagen, Denmark, 2013. [Google Scholar]
- World Health Organization. Strengthening Public Health Capacities and Services in Europe: A Framework for Action. In Proceedings of the Regional Committee for Europe 61st Session, Baku, Azerbaijan, 12–15 September 2011; EUR/RC61/10. Available online: https://iris.who.int/handle/10665/335897 (accessed on 10 September 2024).
- Striker, M. Zmiany w postrzeganiu ról zawodowych menedżerów medycznych w publicznym szpitalu. Eduk. Ekon. I Menedżerów 2016, 41, 135–150. [Google Scholar] [CrossRef]
- Krawczyk-Sołtys, A. Kompetencje menedżerskie w kształtowaniu kompetencji organizacyjnych jednostek ratownictwa medycznego w świetle badań. Stud. I Pr. Kol. Zarządzania I Finans. 2019, 175, 95–104. [Google Scholar] [CrossRef]
- Manuszek, M. Profile kompetencyjne menedżerów sektora publicznego. Stud. I Pr. Kol. Zarządzania I Finans. 2019, 172, 123–141. [Google Scholar] [CrossRef]
- Sexton, J.B.; Adair, K.C.; Profit, J.; Bae, J.; Rehder, K.J.; Gosselin, T.; Milne, J.; Leonard, M.; Frankel, A. Safety Culture and Workforce Well-Being Associations with Positive Leadership WalkRounds. Jt. Comm. J. Qual. Patient Saf. 2021, 47, 403–411. [Google Scholar] [CrossRef]
- Bairros da Silva, L.; Sousa, M.H.O.; Íñiguez-Rueda, L. Managers’ Views on Professional Competencies for Primary Health Care. SAGE Open 2022, 12, 1–11. [Google Scholar] [CrossRef]
- Karniej, P. Zarządzanie kompetencjami pozamedycznymi lekarzy, pielęgniarek i położnych. Pielęg. Zdr. Publ. 2013, 3, 23–29. Available online: https://www.dbc.wroc.pl/Content/30602/103.pdf (accessed on 17 January 2024).
- Hahn, C.A.; Lapetra, M.G. Development and use of the leadership competencies for healthcare services managers assessment. Front. Public Health 2019, 7, 34. [Google Scholar] [CrossRef] [PubMed]
- Wysocka, M.; Lewandowski, R. Key competences of a health care manager. J. Intercult. Manag. 2017, 9, 165–184. [Google Scholar] [CrossRef][Green Version]
- Bratnicki, M.; Frączkiewicz-Wronka, A.; Austen, A. Procesy uczenia się w organizacjach sektora publicznego. In Dylematy i Wyzwania Współczesnego Zarzadzania Organizacjami Publicznymi; Białas, T., Ed.; Wyższa Szkoła Administracji i Biznesu im. E. Kwiatkowskiego: Gdynia, Poland, 2007; pp. 27–38. [Google Scholar]
- Matecka, M.; Sielska, J.; Dąbrowska, E. Competences of the healthcare entity manager. Zesz. Nauk. Uniw. Szczecińskiego. Probl. Zarządzania Finans. I Mark. 2015, 41, 293–304. [Google Scholar] [CrossRef][Green Version]
- Frączkiewicz-Wronka, A. Organizacja publiczna jako środowisko pracy menedżera. In Przedsiębiorczy Menedżer w Przedsiębiorczej Organizacji; Laszuk, M., Ed.; Szkoła Główna Handlowa w Warszawie: Warszawa, Poland, 2007. [Google Scholar]
- van Assen, M.; Tariq, A.; Razavi, A.C.; Yang, C.; Banerjee, I.; De Cecco, C.N. Fusion modeling: Combining clinical and imaging data to advance cardiac care. Circ. Cardiovasc. Imaging 2023, 16, e014533. [Google Scholar] [CrossRef] [PubMed]
- Dako, F.; Cook, T.; Zafar, H.; Schnall, M. Population health management in radiology: Economic considerations. J. Am. Coll. Radiol. 2023, 20, 962–968. [Google Scholar] [CrossRef]
- Nalepka, A. Restrukturyzacja Przedsiębiorstwa. Zarys Problematyki; Wydawnictwo Naukowe PWN: Warszawa-Kraków, Poland, 1999. [Google Scholar]
- Herdman, D. Advances in the diagnosis and management of acute vertigo. J. Laryngol. Amp; Otol. 2024, 138, S8–S13. [Google Scholar] [CrossRef]
- Solow, M.; Perry, T.E. Change management and health care culture. Anesthesiol. Clin. 2023, 41, 693–705. [Google Scholar] [CrossRef] [PubMed]
- Liang, Z.; Howard, P.; Leggat, S.G.; Bartram, T. Development and validation of health service management competencies. J. Health Organ. Manag. 2018, 32, 157–175. [Google Scholar] [CrossRef]
- Lustri, D.A.; Miura, I.K.; Takahashi, S. Knowledge management model: Practical application for competency development. Learn. Organ. 2007, 14, 186–202. [Google Scholar] [CrossRef]
- Kruskal, J.B.; Reedy, A.; Pascal, L.; Rosen, M.P.; Boiselle, P.M. Quality initiatives: Lean approach to improving performance and efficiency in a radiology department. Radiographics 2012, 32, 573–587. [Google Scholar] [CrossRef] [PubMed]
- Chiroli, D.M.D.G.; Coradazi, R.C.; Branco, F.J.C.; Kachba, Y.R.; Aragão, F.V.; Zola, F.C.; Tebcherani, S.M.; Cruz, T.B.R.E. Health care logistics: Mapping and optimization of patients logistics. Indep. J. Manag. Prod. 2021, 12, 2161–2179. [Google Scholar] [CrossRef]
- Loving, V.A.; Ellis, R.L.; Rippee, R.; Steele, J.R.; Schomer, D.F.; Shoemaker, S. Time is not on our side: How radiology practices should manage customer queues. J. Am. Coll. Radiol. 2017, 14, 1481–1488. [Google Scholar] [CrossRef] [PubMed]
- Recht, M.P.; Donoso-Bach, L.; Brkljačić, B.; Chandarana, H.; Jankharia, B.; Mahoney, M.C. Patient-centered radiology: A roadmap for outpatient imaging. Eur. Radiol. 2023, 34, 4331–4340. [Google Scholar] [CrossRef]
- Jessome, R. Improving patient flow in diagnostic imaging: A case report. J. Med. Imaging Radiat. Sci. 2020, 51, 678–688. [Google Scholar] [CrossRef]
- Lee, S.; Groß, S.E.; Pfaff, H.; Dresen, A. Waiting time, communication quality, and patient satisfaction: An analysis of moderating influences on the relationship between perceived waiting time and the satisfaction of breast cancer patients during their inpatient stay. Patient Educ. Couns. 2020, 103, 819–825. [Google Scholar] [CrossRef] [PubMed]
- More, R.; Dunn, E.; Dunwell, S. Improving radiology: A whole-system opportunity. Clin. Radiol. 2023, 78, 395–400. [Google Scholar] [CrossRef] [PubMed]
- Aminololama-Shakeri, S.; Ford, K.M. Patient communication innovations in breast imaging. Radiol. Clin. N. Am. 2024, 62, 717–724. [Google Scholar] [CrossRef]
- Bhat, N.; Singh, V.; Jain, A.; Bagde, H. Enhancing dental diagnostics on leveraging ai for precise imaging analysis. In Advances in Computer and Electrical Engineering; IGI Global: Hershey, PA, USA, 2024; pp. 391–416. [Google Scholar] [CrossRef]
- Hull, M.L. Can ai improve imaging diagnostics? Fertil. Amp; Reprod. 2023, 5, 211. [Google Scholar] [CrossRef]
- Reddy, S. Generative ai in healthcare: An implementation science informed translational path on application, integration and governance. Implement. Sci. 2024, 19, 27. [Google Scholar] [CrossRef] [PubMed]
| Category | Number (n) | Percentage (%) | Additional Information |
|---|---|---|---|
| Gender | |||
| Women | 188 | 62.7% | |
| Men | 112 | 37.3% | |
| Age | Average age: 44.73 ± 11.47 years | ||
| ≤30 years | 44 | 14.7% | |
| 31–40 years | 64 | 21.3% | |
| 41–50 years | 98 | 32.% | Largest group |
| 51–60 years | 70 | 23.3% | |
| >60 years | 24 | 8.0% | |
| Work experience in diagnostic imaging | Average experience: 14.45 ± 10.04 years | ||
| 1–10 years | 113 | 37.7% | |
| 11–20 years | 105 | 35.0% | |
| 21–30 years | 60 | 20.0% | |
| >30 years | 22 | 7.3% | |
| Position | |||
| Nurses | 90 | 30.0% | |
| Technicians | 113 | 37.7% | |
| Radiologists | 97 | 32.2% | |
| Type of employment contract | |||
| Civil law contract | 204 | 68.0% | |
| Employment contract | 96 | 32.0% |
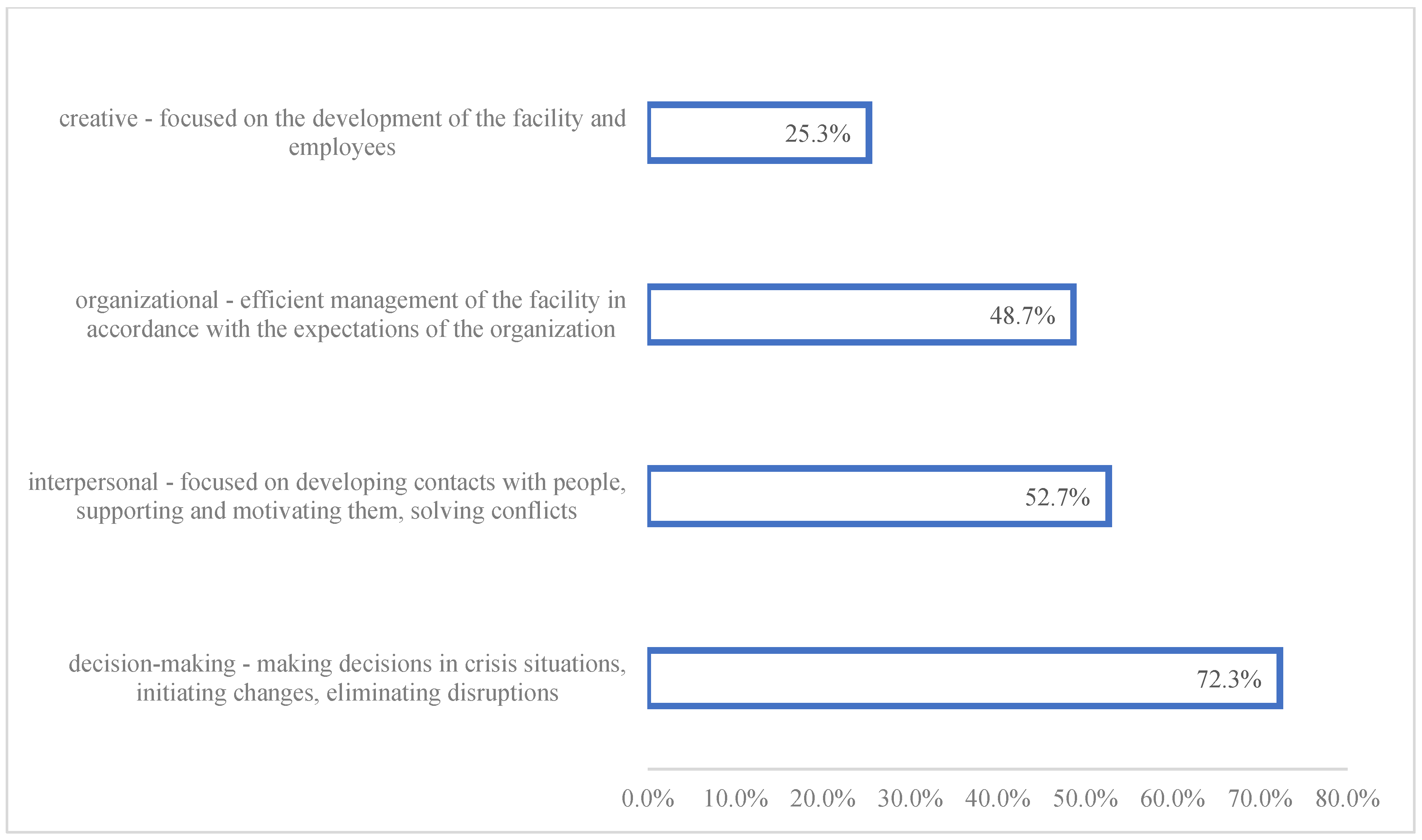
| Role of the Manager | Number of Respondents (N) | Percentage (%) |
|---|---|---|
| Decision-making role | 217 | 72.3% |
| Interpersonal role | 158 | 52.7% |
| Organizational role | 146 | 48.7% |
| Creative role | 76 | 25.3% |
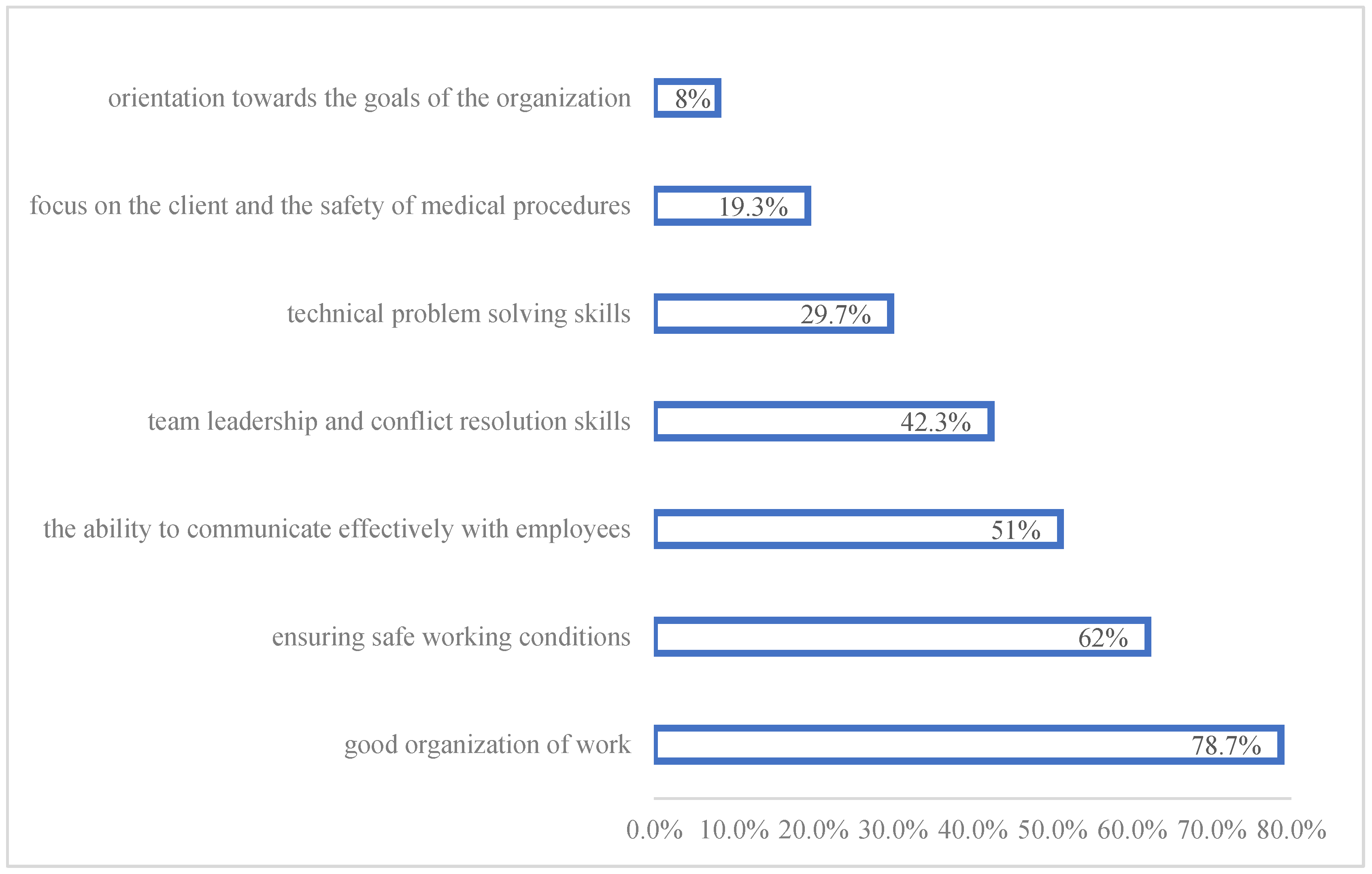
| Category | Number of Respondents (N) | Percentage (%) |
|---|---|---|
| Good work organization | 236 | 78.8% |
| Safe working conditions | 186 | 62.0% |
| Effective communication with employees | 153 | 51.0% |
| Leading teams and conflict resolution | 127 | 42.3% |
| Solving technical and equipment problems | 89 | 29.7% |
| Focus on client and safety | 58 | 19.3% |
| Orientation towards facility goals | 24 | 8.0% |
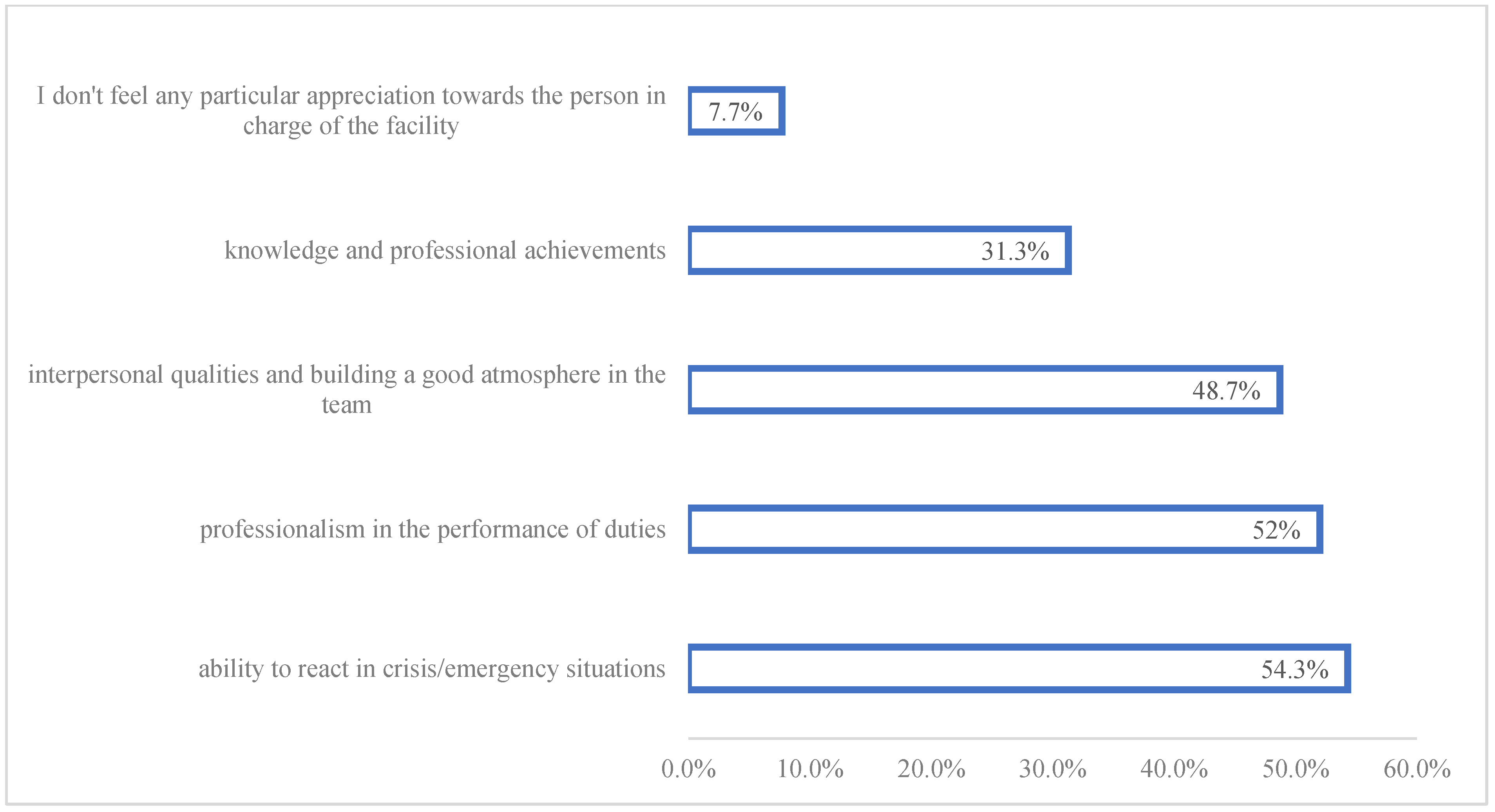
| Competence | Number of Respondents (N) | Percentage (%) |
|---|---|---|
| Ability to react in difficult and crisis situations | 163 | 54.3% |
| Professionalism in the performance of duties | 156 | 52.0% |
| Interpersonal qualities and team atmosphere | 146 | 48.7% |
| Manager’s knowledge and professional achievements | 94 | 31.3% |
| No special appreciation for the manager | 23 | 7.7% |
| Category | Details | Percentage (%) |
|---|---|---|
| Most important role of a manager | Decision-making role | 100% |
| Ability to adapt to changing conditions | Desirable feature of a DI manager | 80% |
| Importance of the interpersonal role | Indicated by respondents | 80% |
| Most important psychological and social competence | Ability to communicate and resolve conflicts | 90% |
| Safety assurance | Safety of patients and staff | 100% |
| Leadership and conflict resolution | Considered very important | 60% |
| Focus on problem solving | Solve specific problems, not find culprits | 70% |
| Culture of learning from mistakes | Appreciated by managers | 70% |
| Gaining trust in difficult decisions | Trust gained by managers | 60% |
| Admitting mistakes | Important for credibility and respect | 70% |
| Good manager characteristics | Decision-making, competence, leadership | 100% (decision making, competence), 60% (leadership) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mierzwa, A.; Syrkiewicz-Świtała, M.; Kuraszewska, B.; Świtała, R.; Grzebieluch, J.; Detyna, B.; Detyna, J.D. Competencies of a Healthcare Manager in the Context of Hospital and Ambulateral Diagnostic Imaging Centers. Logistics 2024, 8, 133. https://doi.org/10.3390/logistics8040133
Mierzwa A, Syrkiewicz-Świtała M, Kuraszewska B, Świtała R, Grzebieluch J, Detyna B, Detyna JD. Competencies of a Healthcare Manager in the Context of Hospital and Ambulateral Diagnostic Imaging Centers. Logistics. 2024; 8(4):133. https://doi.org/10.3390/logistics8040133
Chicago/Turabian StyleMierzwa, Agnieszka, Magdalena Syrkiewicz-Świtała, Bernadeta Kuraszewska, Rafał Świtała, Jolanta Grzebieluch, Beata Detyna, and Jerzy Dariusz Detyna. 2024. "Competencies of a Healthcare Manager in the Context of Hospital and Ambulateral Diagnostic Imaging Centers" Logistics 8, no. 4: 133. https://doi.org/10.3390/logistics8040133
APA StyleMierzwa, A., Syrkiewicz-Świtała, M., Kuraszewska, B., Świtała, R., Grzebieluch, J., Detyna, B., & Detyna, J. D. (2024). Competencies of a Healthcare Manager in the Context of Hospital and Ambulateral Diagnostic Imaging Centers. Logistics, 8(4), 133. https://doi.org/10.3390/logistics8040133







