Health-Seeking Behavior Regarding Coughs in Urban Slums in Lagos, Nigeria
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Definition of Terms
2.4. Study Size
2.5. Sampling Technique
2.6. Participants
2.7. Inclusion and Exclusion Criteria
2.8. Data Sources/Measurement
2.9. Data Collection
2.10. Data Analysis
2.11. Ethical Consideration
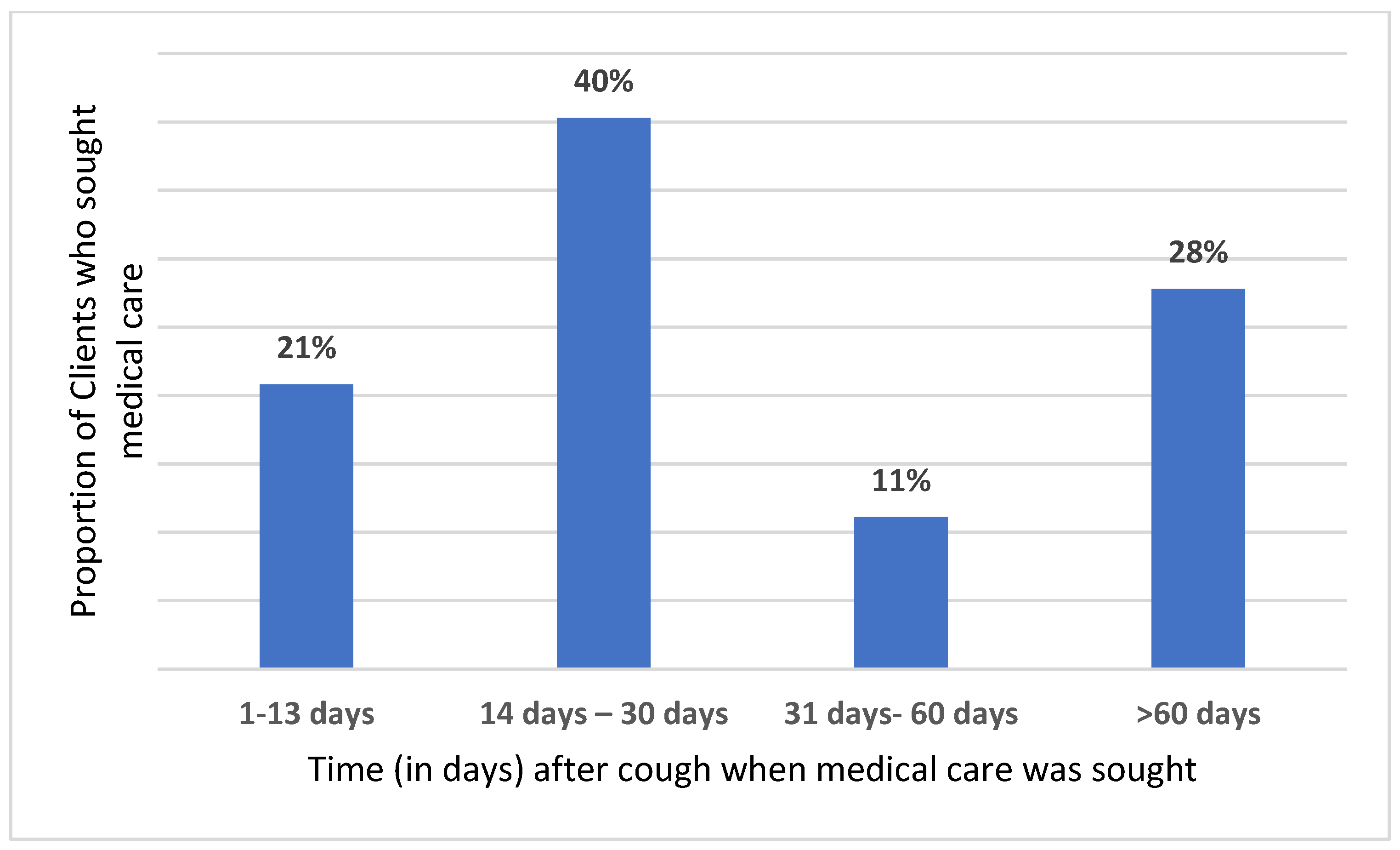
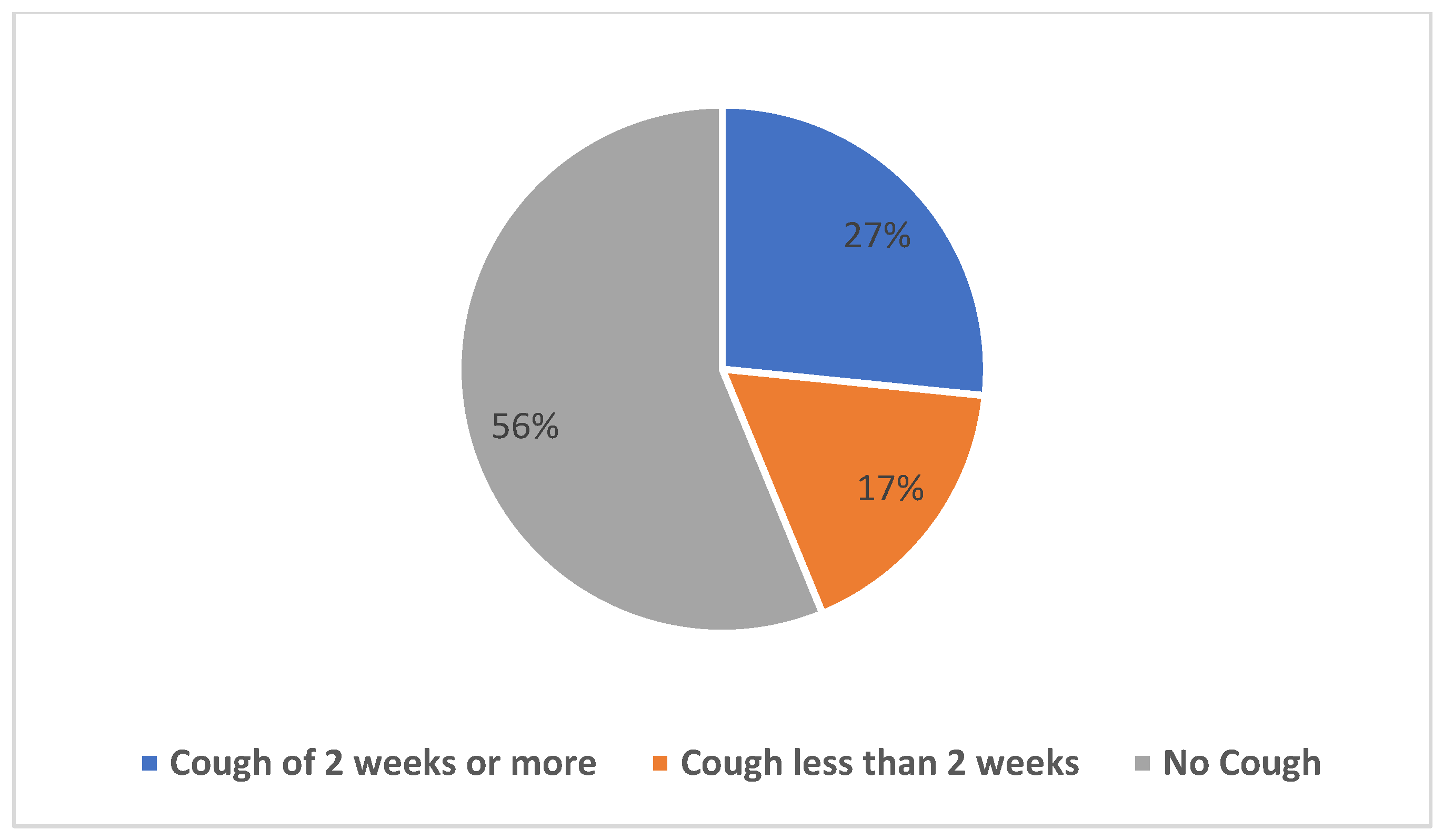
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AIDS | Acquired Immunodeficiency Syndrome |
| ART | Anti-Retroviral Therapy |
| DR-TB | Drug-Resistant Tuberculosis |
| DSTB | Drug-Susceptible Tuberculosis |
| HIV | Human Immunodeficiency Virus |
| LCDA | Local Council Development Area |
| LGA | Local Government Area |
| LSTBLCP | Lagos State Tuberculosis and Leprosy Control Program |
| LTFU | Lost to Follow Up |
| NTBLCP | National Tuberculosis and Leprosy Control Program |
| NTP | National Tuberculosis Program |
| PPMV | Patent Proprietary Medicine Vendors |
| SPSS | Statistical Package for Social Sciences |
| TB | Tuberculosis |
| WHO | World Health Organization |
References
- Global TB Report; World Health Organisation: Geneva, Switzerland, 2020.
- NTBLCP (National Tuberculosis and Leprosy Control Programme) (2019) 2019 Annual TB Report [Internet]. 1–43. Available online: https://www.health.gov.ng/doc/Draft-2019-NTBLCP-Annual-report-22032020.pdf (accessed on 21 November 2022).
- Yates, T.A.; Khan, P.A.; Knight, G.M.; Taylor, J.G.; McHugh, T.D.; Lipman, M.; White, R.G.; Cohen, T.; Cobelens, F.G.; Wood, R.; et al. The transmission of Mycobacterium tuberculosis in high burden settings. Lancet Infect. Dis. 2016, 16, 227–238. [Google Scholar] [CrossRef] [Green Version]
- Noykhovich, E.; Mookherji, S.; Roess, A. The Risk of Tuberculosis among Populations Living in Slum Settings: A Systematic Review and Meta-analysis. J. Urban Health 2019, 96, 262–275. [Google Scholar] [CrossRef] [PubMed]
- Lönnroth, K.; Jaramillo, E.; Williams, B.G.; Dye, C.; Raviglione, M. Drivers of tuberculosis epidemics: The role of risk factors and social determinants. Soc. Sci. Med. 2009, 68, 2240–2246. [Google Scholar] [CrossRef] [PubMed]
- Banu, S.; Rahman, M.T.; Uddin MK, M.; Khatun, R.; Ahmed, T.; Rahman, M.M.; Husain, M.A.; van Leth, F. Epidemiology of Tuberculosis in an Urban Slum of Dhaka City, Bangladesh. PLoS ONE 2013, 8, e77721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogbudebe, C.L.; Chukwu, J.N.; Nwafor, C.C.; Meka, A.O.; Ekeke, N.; Madichie, N.O.; Anyim, M.C.; Osakwe, C.; Onyeonoro, U.; Ukwaja, K.N.; et al. Reaching the underserved: Active tuberculosis case finding in urban slums in southeastern Nigeria. Int. J. Mycobacteriolog 2015, 4, 18–24. [Google Scholar] [CrossRef] [Green Version]
- Chanda-Kapata, P.; Kapata, N.; Masiye, F.; Maboshe, M.; Klinkenberg, E.; Cobelens, F.; Grobusch, M.P. Health Seeking Behaviour among Individuals with Presumptive Tuberculosis in Zambia. PLoS ONE 2016, 11, e0163975. [Google Scholar] [CrossRef] [Green Version]
- Ehsanul Huq KA, T.M.; Moriyama, M.; Zaman, K.; Chisti, M.J.; Long, J.; Islam, A.; Hossain, S.; Shirin, H.; Raihan, M.J.; Chowdhury, S.; et al. Health seeking behaviour and delayed management of tuberculosis patients in rural Bangladesh. BMC Infect. Dis. 2018, 18, 515. [Google Scholar] [CrossRef] [Green Version]
- Mistry, N.; Rangan, S.; Dholakia, Y.; Lobo, E.; Shah, S.; Patil, A. Durations and Delays in Care Seeking, Diagnosis and Treatment Initiation in Uncomplicated Pulmonary Tuberculosis Patients in Mumbai, India. PLoS ONE 2016, 11, e0152287. [Google Scholar] [CrossRef]
- Engeda, E.H.; Dachew, B.A.; Kassa Woreta, H.; Mekonnen Kelkay, M.; Ashenafie, T.D. Health Seeking Behaviour and Associated Factors among Pulmonary Tuberculosis Suspects in Lay Armachiho District, Northwest Ethiopia: A Community-Based Study. Tuberc. Res. Treat. 2016, 2016, 7892701. [Google Scholar] [CrossRef] [Green Version]
- Macrotrends. Lagos, Nigeria Metro Area Population 1950–2021. Available online: https://www.macrotrends.net/cities/22007/lagos/population (accessed on 21 November 2022).
- Senkoro, M.; Hinderaker, S.G.; Mfinanga, S.G.; Range, N.; Kamara, D.V.; Egwaga, S.; Van Leth, F. Health care-seeking behaviour among people with cough in Tanzania: Findings from a tuberculosis prevalence survey. Int. J. Tuberc. Lung. Dis. 2015, 19, 640–664. [Google Scholar] [CrossRef]
- Tong, Y.; Guan, X.; Hou, S.; Cai, L.; Huang, Y.; Wang, L.; Zhan, F.; Shi, Y.; Liu, J. Determinants of Health Care-Seeking Delay among Tuberculosis Patients in Rural Area of Central China. Int. J. Environ. Res. Public Health 2018, 15, 1998. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ndubuisi, N.O.; Chibuike, O.A.; Esther, U.A.; Christopher, O.U. Delay in Diagnosis of Pulmonary Tuberculosis among Presumptive Tuberculosis Cases in Parts of Anambra State, Nigeria. J. Emerg. Infect. Dis. 2016, 1, 120. [Google Scholar] [CrossRef] [Green Version]
- Hoa, N.P.; Diwan, V.K.; Co, N.V.; Thorson, A.E. Knowledge about tuberculosis and its treatment among new pulmonary TB patients in the north and central regions of Vietnam. Int. J. Tuberc. Lung. Dis. 2004, 8, 603–608. [Google Scholar]
- Muttamba, W.; Ssengooba, W.; Kirenga, B.; Sekibira, R.; Walusimbi, S.; Katamba, A.; Joloba, M. Health seeking behavior among individuals presenting with chronic cough at referral hospitals in Uganda; missed opportunity for early tuberculosis diagnosis. PLoS ONE 2019, 14, e0217900. [Google Scholar] [CrossRef] [PubMed]
- Buregyeya, E.; Kulane, A.; Colebunders, R.; Wajja, A.; Kiguli, J.; Mayanja, H.; Musoke, P.; Pariyo, G.; Mitchell, E.M. Tuberculosis knowledge, attitudes and health-seeking behaviour in rural Uganda. Int. J. Tuberc. Lung. Dis. 2011, 15, 938–942. [Google Scholar] [CrossRef] [PubMed]
- Godfrey-Faussett, P.; Kaunda, H.; Kamanga, J.; Van Beers, S.; Van Cleeff, M.; Kumwenda-Phiri, R.; Tihon, V. Why do patients with a cough delay seeking care at Lusaka urban health centres? A health systems research approach. Int. J. Tuberc. Lung. Dis. 2002, 6, 796–805. [Google Scholar] [PubMed]
- Makgopa, S.; Madiba, S. Tuberculosis Knowledge and Delayed Health Care Seeking among New Diagnosed Tuberculosis Patients in Primary Health Facilities in an Urban District, South Africa. Health Serv. Insights 2021, 14, 11786329211054035. [Google Scholar] [CrossRef] [PubMed]
- Getnet, F.; Demissie, M.; Assefa, N.; Mengistie, B.; Worku, A. Delay in diagnosis of pulmonary tuberculosis in low-and middle-income settings: Systematic review and meta-analysis. BMC Pulm. Med. 2017, 17, 202. [Google Scholar] [CrossRef]
- Soubra, R.; Hlais, S.; Houmani, N.; Ghandour, L.; El Haj Hassan, R.; Joujou, M.; Shaarani, I. Health seeking behaviour among Lebanese population: A highlight on seeking care from pharmacists. Eur. J. Gen. Pract. 2021, 27, 51–59. [Google Scholar] [CrossRef]
- Sudhinaraset, M.; Ingram, M.; Lofthouse, H.K.; Montagu, D. What is the role of informal healthcare providers in developing countries? A systematic review. PLoS ONE 2013, 8, e54978. [Google Scholar] [CrossRef]
- Lönnroth, K.; Lambregts, K.; Nhien, D.T.; Quy, H.T.; Diwan, V.K. Private pharmacies and tuberculosis control: A survey of case detection skills and reported anti-tuberculosis drug dispensing in private pharamcies in Ho Chi Minh City, Vietnam. Int. J. Tuberc. Lung Dis. 2000, 4, 1052–1059. [Google Scholar] [PubMed]
- Van der Werf, M.J.; Chechulin, Y.; Yegorova, O.B.; Marcinuk, T.; Stopolyanskiy, A.; Voloschuk, V.; Zlobinec, M.; Vassall, A.; Veen, J.; Hasker, E.; et al. Health care seeking behaviour for tuberculosis symptoms in Kiev City, Ukraine. Int. J. Tuberc. Lung Dis. 2006, 10, 390–395. [Google Scholar] [PubMed]
- Onyeneho, N.G.; Chukwu, J.N. Is there a role for patent medicine vendors in tuberculosis control in southern Nigeria? J. Health Popul. Nutr. 2010, 28, 567–577. [Google Scholar] [CrossRef]
- WHO. Public-Private Mix for TB Prevention and Care: A Roadmap; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Smith, F. The quality of private pharmacy services in low and middle-income countries: A systematic review. Pharm. World Sci. 2009, 31, 351–361. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Frequency | Percentage |
|---|---|---|
| Age (years) | ||
| <15 | 8 | 1.3 |
| 15–24 | 33 | 5.2 |
| 25–34 | 156 | 24.7 |
| 35–44 | 151 | 23.9 |
| 45–54 | 138 | 21.8 |
| 55–64 | 82 | 13.0 |
| >65 | 64 | 10.1 |
| Sex | ||
| Male | 416 | 65.8 |
| Female | 216 | 34.2 |
| Religion | ||
| Christianity | 352 | 55.7 |
| Islam | 277 | 43.8 |
| Traditional religion | 3 | 0.5 |
| Ethnicity | ||
| Yoruba | 469 | 74.2 |
| Ibo | 69 | 10.9 |
| Hausa/Fulani | 44 | 7.0 |
| Other | 50 | 7.9 |
| Marital Status | ||
| Single | 91 | 14.4 |
| Married | 466 | 73.7 |
| Separated/divorced | 23 | 3.7 |
| Widowed | 52 | 8.2 |
| Education | ||
| No formal education | 132 | 20.9 |
| Primary | 170 | 26.9 |
| Secondary | 239 | 37.8 |
| Tertiary | 91 | 14.4 |
| Average no of household | ||
| 1–2 | 99 | 15.7 |
| 3–4 | 259 | 41.0 |
| 5–6 | 180 | 28.5 |
| 7–8 | 51 | 8.1 |
| 8–10 | 16 | 2.5 |
| >10 | 27 | 4.3 |
| No of persons per room | ||
| 1–2 | 281 | 44.5 |
| 3–4 | 243 | 38.4 |
| 5–6 | 90 | 14.2 |
| >6 | 18 | 2.9 |
| Symptoms | Frequency | Percentage |
|---|---|---|
| Cough | 216 | 34.2 |
| Weight loss | 112 | 17.7 |
| Night sweats | 123 | 19.5 |
| Fever | 149 | 23.6 |
| Hemoptysis | 20 | 3.2 |
| Loss of appetite | 72 | 11.4 |
| Health-Seeking Behavior | Frequency | Percentage |
|---|---|---|
| Did nothing | 15 | 8.8 |
| Self-medication/home remedy | 26 | 15.5 |
| Private hospital | 25 | 15.0 |
| Government hospital | 35 | 20.8 |
| Patent medicine store | 62 | 37.2 |
| Mission hospital | 1 | 0.4 |
| Traditional healer | 4 | 2.2 |
| Overall health-seeking behavior (n = 226) | ||
| Good health-seeking behavior | 82 | 36.3 |
| Poor health-seeking behavior | 144 | 63.7 |
| Variable | B (Regression Coefficient) | S.E. (Standard Error) | Wald (Wald Chi-Square Test) | df (Degrees of Freedom) | Sig. (Significance) | aOR (Adjusted Odds Ratio) | 95% C.I. (Confidence Interval) Lower | 95% C.I. (Confidence Interval) Upper |
|---|---|---|---|---|---|---|---|---|
| Hx of Contact with TB patient | −0.112 | 0.401 | 0.078 | 1 | 0.78 | 0.894 | 0.407 | 1.964 |
| Smoking | −0.481 | 0.72 | 0.446 | 1 | 0.504 | 0.618 | 0.151 | 2.536 |
| Knowledge of TB spread | −0.345 | 0.339 | 1.035 | 1 | 0.309 | 0.708 | 0.364 | 1.377 |
| Knowledge of TB symptoms | −0.429 | 0.333 | 1.667 | 1 | 0.197 | 0.651 | 0.339 | 1.249 |
| Education | −0.255 | 0.454 | 0.315 | 1 | 0.575 | 0.775 | 0.319 | 1.886 |
| Income level | 0 | 0 | 0.17 | 1 | 0.68 | 1 | 1 | 1 |
| Religion | −0.283 | 0.324 | 0.766 | 1 | 0.382 | 0.753 | 0.399 | 1.421 |
| Sex | 0.303 | 0.333 | 0.827 | 1 | 0.363 | 1.354 | 0.705 | 2.6 |
| BMI (Kg/meter square) | −0.011 | 0.022 | 0.251 | 1 | 0.616 | 0.989 | 0.948 | 1.032 |
| Age | 0.018 | 0.011 | 2.753 | 1 | 0.097 | 1.018 | 0.997 | 1.039 |
| Constant | −0.102 | 1.019 | 0.01 | 1 | 0.92 | 0.903 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adepoju, V.A.; Oladimeji, O.; Sokoya, O.D. Health-Seeking Behavior Regarding Coughs in Urban Slums in Lagos, Nigeria. Medicines 2023, 10, 38. https://doi.org/10.3390/medicines10070038
Adepoju VA, Oladimeji O, Sokoya OD. Health-Seeking Behavior Regarding Coughs in Urban Slums in Lagos, Nigeria. Medicines. 2023; 10(7):38. https://doi.org/10.3390/medicines10070038
Chicago/Turabian StyleAdepoju, Victor Abiola, Olanrewaju Oladimeji, and Olusola Daniel Sokoya. 2023. "Health-Seeking Behavior Regarding Coughs in Urban Slums in Lagos, Nigeria" Medicines 10, no. 7: 38. https://doi.org/10.3390/medicines10070038






