Best Practice Guide for Cryoballoon Ablation in Atrial Fibrillation: The Compilation Experience of More than 1000 Procedures
Abstract
:1. Introduction
2. Patient Selection for AF Ablation through Cryoablation
2.1. Paroxysmal AF
2.2. Persistent AF
2.3. Heart Failure
3. Preprocedural Imaging
4. Procedural Tips and Tricks
- Deep sedation or general anesthesia
- Femoral access
- Transeptal access
- Technical tips and tricks for PVI using CB
- ➢
- Approaching the veins
- i.
- As a general rule, depth of the sheath and/or balloon is assessed with the ipsilateral (relative to the target PVs) projection (e.g., left anterior oblique for the left PVs), providing a more longitudinal view of the vein taking into account the borders of the cardiac silhouette, whilst their orientation with regards to the frontal plane of each vein is assessed using the contralateral projection (e.g., right anterior oblique for the left PVs), where veins course relatively perpendicularly to the imaging plane [54].
- ii.
- It is extremely important to be mindful and to note the presence of antral potentials at the time of vein catheterization through the circular multipolar catheter (Achieve) since proper position of the CB may preclude such recording later during lesion formation (e.g., Achieve catheter may be needed to provide support and to be lodged distantly in the vein to ensure balloon stability).
- iii.
- In order to transit from the left PVs to the right ones, the sheath (obviously with the balloon in the retracted position and the Achieve catheter projecting from its tip) should be flexed slightly rather than excessively in order to avoid missing the most cranial right PV. Given the more anteriorly placed transseptal puncture site used for PV isolation, to facilitate access to the right inferior PV, clockwise rotation is preferred in order to avoid scraping the anterior atrial wall.
- iv.
- In more horizontal orientation of the heart, as in obese individuals, it is likely that the most inferior right PV will apparently course behind the diaphragm, with the contrast appearing at the level of the liver (since the posterior basal-most part of the right inferior pulmonary lobe extends caudally to this level). If no such image is obtained during previous PV occlusions, the operator should try and map the area of interest and, once a vein with the proper contrast staining is located, either confirm its isolation (Achieve was placed in a more cranial branch during previous lesion delivery) or promptly isolate it.
- v.
- The PVs may be targeted either in the sequence of LSPV–LIPV–RSPV–RIPV or in a clockwise sequence (LSPV–LIPV–RIPV–RSPV).
- ➢
- Occluding the veins
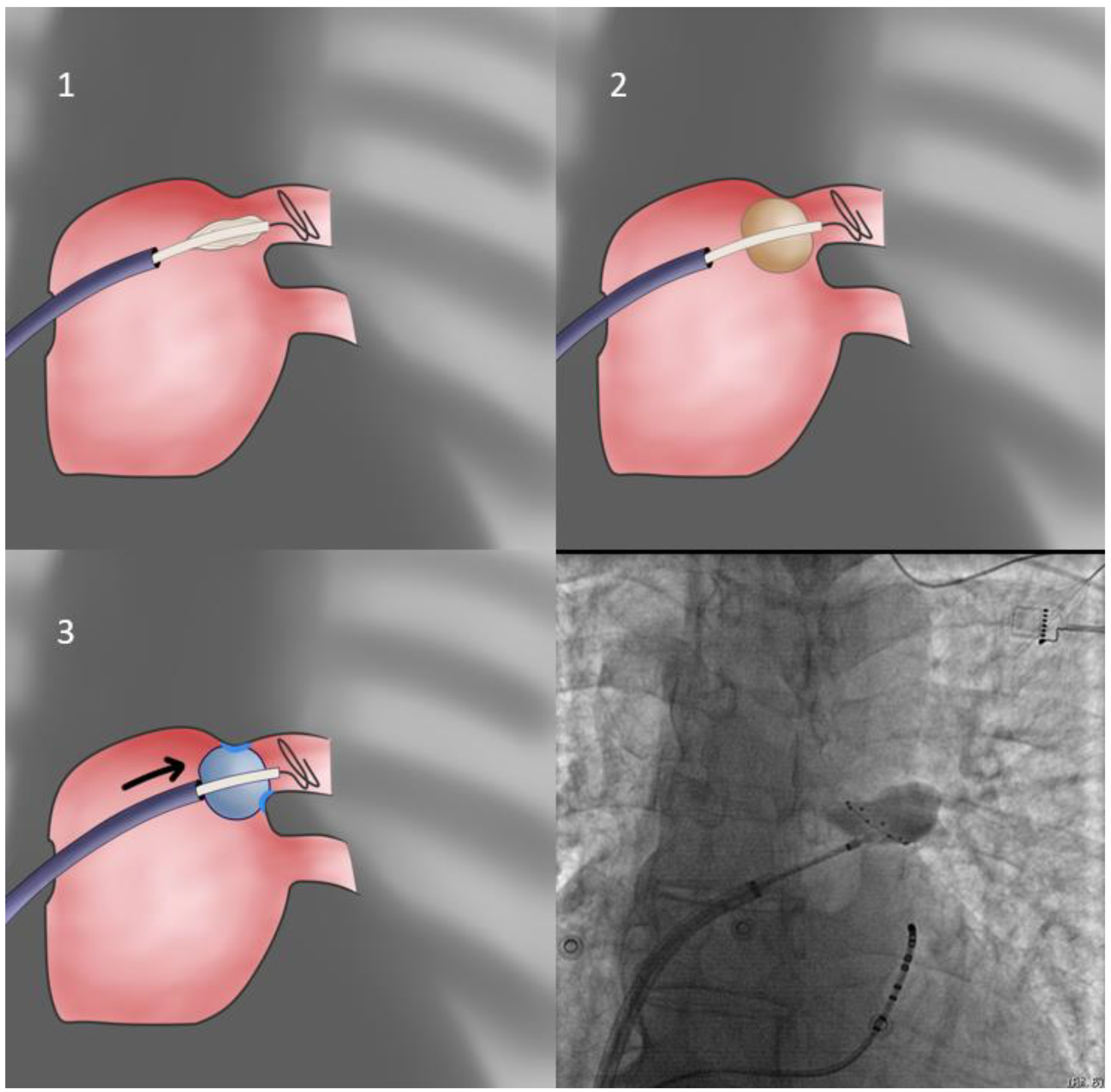
- Our first approach is using the sheath as the support for PV sealing (FlexCath based direct approach—Figure 1). With the whole system (Achieve catheter, cryoballoon and sheath) in contact and the sheath slightly flexed, we aim to align its distal part with the axis of the balloon and the Achieve catheter. Given that a vein may change the orientation of its course very near its antrum, it is the proximal part of the Achieve catheter that should be used for defining proper system alignment [53].
- 2.
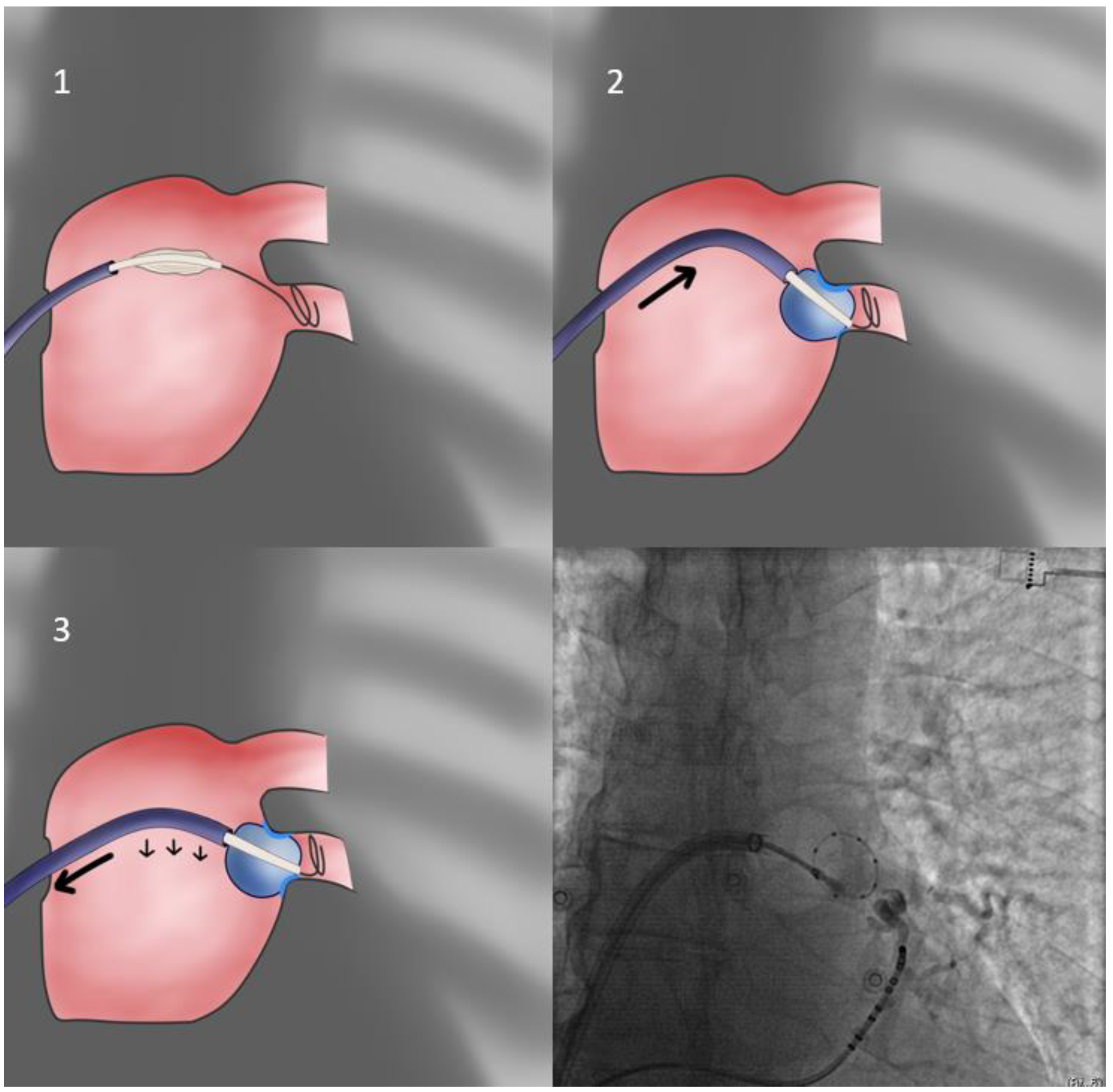
- In cases of cranial superior veins and horizontal inferior veins, we apply the CB-only approach (Figure 3) without the sheath (second approach). The sheath is relaxed and placed near but not in contact with the CB since even minimal flexion to the sheath will preclude proper sealing of the antrum. Selection of the more horizontal branch of the PV facilitates the CB-only approach, even if repositioning of the Achieve catheter is required. Additionally, cranial flexion of the CB shaft assists cranial superior PV sealing.
- 3.
- In cases of extremely sized antra and despite proper orientation, sealing is unattainable; the operator may elect to push the sheath forward only after freezing has begun, since freezing increases CB diameter from 26 to 28 mm, rendering it more likely to properly occlude the antrum (delayed occlusion approach—Figure 4). Usually, the cue for sheath pushing is the initiation of a steep temperature drop on the monitoring console screen, several seconds after freezing has commenced. In even rarer cases, where this approach is ineffective, and conversion to a point-by-point approach is undesirable, one may deliver lesions in a sequential manner, targeting each quadrant of the antrum separately, without occlusion, evaluating the effect after completion of the quartet of applications (segmental approach).
- 4.
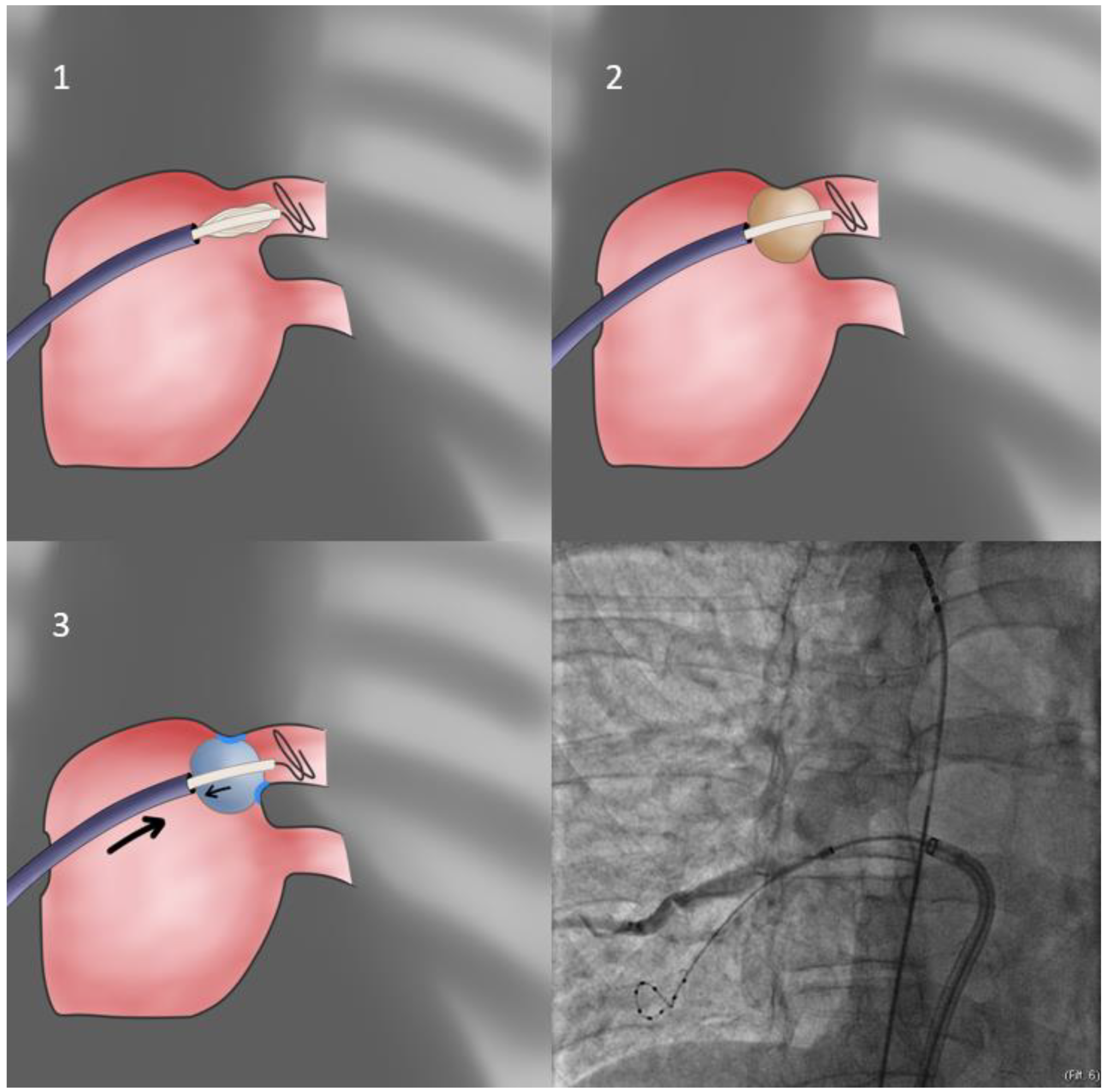
- When, despite all efforts and maneuvers already described, the operator cannot achieve proper alignment of the Achieve/CB/sheath system with the vein, a final solution entails allowing the PV itself to position the CB in its antrum. This is achieved by purposefully and warily inflating slightly inside the PV ostium (obviously the operator must be alert and retract the system if severe CB distortion is observed), whilst the sheath is placed in the approximately anticipated orientation, slightly flexed in order to be rigid. It is expected that the PV will eject the inflating balloon while imparting its orientation to it—thus, the operator must be vigilant and immediately use the prepped sheath to intercept the motion and achieve apposition of the CB to the antrum in the vein-determined orientation (trap-based approach—Figure 5). If more pressure is needed to achieve occlusion, it is more prudent to use the balloon catheter shaft since pushing the rigid sheath may undo the achieved proper orientation of the system.
- ➢
- Avoiding postablation PV stenosis
- ➢
- Circular catheter maneuvers
- ➢
- Cryoapplications in right antra
- ➢
- Cryoapplications in left common PV
- ➢
- Cryoapplications in superior vena cava (SVC)
5. Cryoablation Dosing
- ➢
- TTI < 40 s and nadir temperature < −60 °C: total duration 180 s without bonus
- ➢
- TTI 40–60 s and nadir temperature > −60 °C: total duration 240 s without bonus
- ➢
- No TTI, temperature −40 °C within 60 s and nadir temperature < −60 °C total duration 180 s without bonus
- ➢
- No TTI, temperature −40 °C within 60 s and nadir temperature > −60 °C total duration 240 s without bonus
- ➢
- No TTI, temperature −40 °C > 60 s and nadir temperature > −60 °C total duration 240 s plus bonus
6. Predictors of PV Reconnection
7. Complications
7.1. Atrioesophageal Fistula
7.2. Prevention of Phrenic Nerve Injury
- If neuromuscular blocking drugs have been administered during the induction of general anesthesia and sufficient time has not passed for the paralytic effect to reverse, neostigmine should be used.
- PN should be paced at the maximal output using a deflectable catheter placed above the level of the ablation in the junction of the superior vena cava and the right subclavian vein. Alternatively, the decapolar catheter can be placed in the anterolateral portion of the superior vena cava near the atrial–SVC junction.
- In case PN capture cannot be achieved or is not steady, the pacing dipole could be switched to the more distal (1 to 10 instead of 1 to 2 in the decapolar catheter).
- Palpation of the strength of diaphragmatic excursion during PN pacing, below the costal margin, is the most common method of monitoring PN function.
- It is crucial to terminate ablation and deflate balloon immediately at the first sign of PN injury.
- In any case, CB should be positioned as antral as possible for PN injury avoidance.
- If recovery is fast and additional ablation is required, a different PV branch with a more antral position of the balloon should be preferred.
- In case PN injury persists the day after the procedure and confirmed by an inhalation–exhalation chest X-ray, physical therapy is essential with deep breathing exercises.
7.3. Postablation Pericarditis
8. Post-Ablation and Post-Discharge Care
9. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef] [PubMed]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm 2019, 16, e66–e93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawamura, I.; Neuzil, P.; Shivamurthy, P.; Kuroki, K.; Lam, J.; Musikantow, D.; Chu, E.; Turagam, M.K.; Minami, K.; Funasako, M.; et al. How does the level of pulmonary venous isolation compare between pulsed field ablation and thermal energy ablation (radiofrequency, cryo, or laser)? EP Eur. 2021, 23, 1757–1766. [Google Scholar] [CrossRef] [PubMed]
- Knecht, S.; Kühne, M.; Osswald, S.; Sticherling, C. Quantitative assessment of a second-generation cryoballoon ablation catheter with new cooling technology—A perspective on potential implications on outcome. J. Interv. Card. Electrophysiol. 2014, 40, 17–21. [Google Scholar] [CrossRef]
- Coulombe, N.; Paulin, J.; Su, W. Improved in vivo performance of second-generation cryoballoon for pulmonary vein isolation. J. Cardiovasc. Electrophysiol. 2013, 24, 919–925. [Google Scholar] [CrossRef]
- Di Giovanni, G.; Wauters, K.; Chierchia, G.-B.; Sieira, J.; Levinstein, M.; Conte, G.; de Asmundis, C.; Baltogiannis, G.; Saitoh, Y.; Ciconte, G.; et al. One-year follow-up after single procedure Cryoballoon ablation: A comparison between the first and second generation balloon. J. Cardiovasc. Electrophysiol. 2014, 25, 834–839. [Google Scholar] [CrossRef]
- Aytemir, K.; Gurses, K.M.; Yalcin, M.U.; Kocyigit, D.; Dural, M.; Evranos, B.; Yorgun, H.; Ates, A.H.; Sahiner, M.L.; Kaya, E.B.; et al. Safety and efficacy outcomes in patients undergoing pulmonary vein isolation with second-generation cryoballoon. EP Eur. 2015, 17, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Blaauw, Y.; Timmermans, C.; Pison, L.; Vernooy, K.; Crijns, H. Adenosine testing after second-generation balloon devices (cryothermal and laser) mediated pulmonary vein ablation for atrial fibrillation. J. Interv. Card. Electrophysiol. 2014, 41, 91–97. [Google Scholar] [CrossRef]
- Fürnkranz, A.; Bordignon, S.; Dugo, D.; Perotta, L.; Gunawardene, M.; Schulte-Hahn, B.; Nowak, B.; Schmidt, B.; Chun, J.K.R. Improved 1-year clinical success rate of pulmonary vein isolation with the second-generation cryoballoon in patients with paroxysmal atrial fibrillation. J. Cardiovasc. Electrophysiol. 2014, 25, 840–844. [Google Scholar] [CrossRef]
- Metzner, A.; Reissmann, B.; Rausch, P.; Mathew, S.; Wohlmuth, P.; Tilz, R.; Rillig, A.; Lemes, C.; Deiss, S.; Heeger, C.; et al. One-year clinical outcome after pulmonary vein isolation using the second-generation 28-mm cryoballoon. Circ. Arrhythmia Electrophysiol. 2014, 7, 288–292. [Google Scholar] [CrossRef]
- Jourda, F.; Providencia, R.; Marijon, E.; Bouzeman, A.; Hireche, H.; Khoueiry, Z.; Cardin, C.; Combes, N.; Combes, S.; Boveda, S.; et al. Contact-force guided radiofrequency vs. second-generation balloon cryotherapy for pulmonary vein isolation in patients with paroxysmal atrial fibrillation-a prospective evaluation. EP Eur. 2015, 17, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Aryana, A.; Morkoch, S.; Bailey, S.; Lim, H.W.; Sara, R.; d’Avila, A.; O’Neill, P.G. Acute procedural and cryoballoon characteristics from cryoablation of atrial fibrillation using the first- and second-generation cryoballoon: A retrospective comparative study with follow-up outcomes. J. Interv. Card. Electrophysiol. 2014, 41, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Chierchia, G.B.; Di Giovanni, G.; Ciconte, G.; de Asmundis, C.; Conte, G.; Sieira-Moret, J.; Rodriguez-Mañero, M.; Casado, R.; Baltogiannis, G.; Namdar, M.; et al. Second-generation cryoballoon ablation for paroxysmal atrial fibrillation: 1-year follow-up. EP Eur. 2014, 16, 639–644. [Google Scholar] [CrossRef] [Green Version]
- Ciconte, G.; de Asmundis, C.; Sieira, J.; Conte, G.; Di Giovanni, G.; Mugnai, G.; Saitoh, Y.; Baltogiannis, G.; Irfan, G.; Coutiño-Moreno, H.E.; et al. Single 3-minute freeze for second-generation cryoballoon ablation: One-year follow-up after pulmonary vein isolation. Heart Rhythm 2015, 12, 673–680. [Google Scholar] [CrossRef] [PubMed]
- Iliodromitis, K.; Lenarczyk, R.; Scherr, D.; Conte, G.; Farkowski, M.M.; Marin, F.; Garcia-Seara, J.; Simovic, S.; Potpara, T. Patient selection, peri-procedural management, and ablation techniques for catheter ablation of atrial fibrillation: An EHRA survey. Eurospace 2022, euac236. [Google Scholar] [CrossRef]
- Kuck, K.H.; Brugada, J.; Fürnkranz, A.; Metzner, A.; Ouyang, F.; Chun, K.R.; Elvan, A.; Arentz, T.; Bestehorn, K.; Pocock, S.J.; et al. Cryoballoon or Radiofrequency Ablation for Paroxysmal Atrial Fibrillation. N. Engl. J. Med. 2016, 374, 2235–2245. [Google Scholar] [CrossRef]
- Luik, A.; Radzewitz, A.; Kieser, M.; Walter, M.; Bramlage, P.; Hörmann, P.; Schmidt, K.; Horn, N.; Brinkmeier-Theofanopoulou, M.; Kunzmann, K.; et al. Cryoballoon Versus Open Irrigated Radiofrequency Ablation in Patients With Paroxysmal Atrial Fibrillation: The Prospective, Randomized, Controlled, Noninferiority FreezeAF Study. Circulation 2015, 132, 1311–1319. [Google Scholar] [CrossRef]
- Neumann, T.; Kuniss, M.; Conradi, G.; Janin, S.; Berkowitsch, A.; Wojcik, M.; Rixe, J.; Erkapic, D.; Zaltsberg, S.; Rolf, A.; et al. MEDAFI-Trial (Micro-embolization during ablation of atrial fibrillation): Comparison of pulmonary vein isolation using cryoballoon technique vs. radiofrequency energy. Europace 2011, 13, 37–44. [Google Scholar] [CrossRef]
- Kuck, K.H.; Fürnkranz, A.; Chun, K.R.; Metzner, A.; Ouyang, F.; Schlüter, M.; Elvan, A.; Lim, H.W.; Kueffer, F.J.; Arentz, T.; et al. Cryoballoon or radiofrequency ablation for symptomatic paroxysmal atrial fibrillation: Reintervention, rehospitalization, and quality-of-life outcomes in the FIRE AND ICE trial. Eur. Heart J. 2016, 37, 2858–2865. [Google Scholar] [CrossRef] [Green Version]
- Bollmann, A.; Ueberham, L.; Schuler, E.; Wiedemann, M.; Reithmann, C.; Sause, A.; Tebbenjohanns, J.; Schade, A.; Shin, D.I.; Staudt, A.; et al. Cardiac tamponade in catheter ablation of atrial fibrillation: German-wide analysis of 21 141 procedures in the Helios atrial fibrillation ablation registry (SAFER). EP Eur. 2018, 20, 1944–1951. [Google Scholar] [CrossRef]
- Ueberham, L.; Schuler, E.; Hindricks, G.; Kuhlen, R.; Bollmann, A. SAFER. Eur. Heart J. 2018, 39, 2023–2024. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cosedis Nielsen, J.; Johannessen, A.; Raatikainen, P.; Hindricks, G.; Walfridsson, H.; Kongstad, O.; Pehrson, S.; Englund, A.; Hartikainen, J.; Mortensen, L.S.; et al. Radiofrequency ablation as initial therapy in paroxysmal atrial fibrillation. N. Engl. J. Med. 2012, 367, 1587–1595. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morillo, C.A.; Verma, A.; Connolly, S.J.; Kuck, K.H.; Nair, G.M.; Champagne, J.; Sterns, L.D.; Beresh, H.; Healey, J.S.; Natale, A. Radiofrequency ablation vs. antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrillation (RAAFT-2): A randomized trial. JAMA 2014, 311, 692–700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wazni, O.M.; Marrouche, N.F.; Martin, D.O.; Verma, A.; Bhargava, M.; Saliba, W.; Bash, D.; Schweikert, R.; Brachmann, J.; Gunther, J.; et al. Radiofrequency ablation vs. antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: A randomized trial. JAMA 2005, 293, 2634–2640. [Google Scholar] [CrossRef] [Green Version]
- Andrade, J.G.; Wells, G.A.; Deyell, M.W.; Bennett, M.; Essebag, V.; Champagne, J.; Roux, J.-F.; Yung, D.; Skanes, A.; Khaykin, Y.; et al. Cryoablation or Drug Therapy for Initial Treatment of Atrial Fibrillation. N. Engl. J. Med. 2020, 384, 305–315. [Google Scholar] [CrossRef]
- Wazni, O.M.; Dandamudi, G.; Sood, N.; Hoyt, R.; Tyler, J.; Durrani, S.; Niebauer, M.; Makati, K.; Halperin, B.; Gauri, A.; et al. Cryoballoon Ablation as Initial Therapy for Atrial Fibrillation. N. Engl. J. Med. 2021, 384, 316–324. [Google Scholar] [CrossRef]
- Kuniss, M.; Pavlovic, N.; Velagic, V.; Hermida, J.S.; Healey, S.; Arena, G.; Badenco, N.; Meyer, C.; Chen, J.; Iacopino, S.; et al. Cryoballoon ablation vs. antiarrhythmic drugs: First-line therapy for patients with paroxysmal atrial fibrillation. EP Eur. 2021, 23, 1033–1041. [Google Scholar] [CrossRef] [PubMed]
- Kanagaratnam, P.; McCready, J.; Tayebjee, M.; Shepherd, E.; Sasikaran, T.; Todd, D.; Johnson, N.; Kyriacou, A.; Hayat, S.; Hobson, N.A.; et al. Ablation versus anti-arrhythmic therapy for reducing all hospital episodes from recurrent atrial fibrillation: A prospective, randomized, multi-centre, open label trial. EP Eur. 2022. [Google Scholar] [CrossRef]
- Andrade, J.G.; Wazni, O.M.; Kuniss, M.; Hawkins, N.M.; Deyell, M.W.; Chierchia, G.B.; Nissen, S.; Verma, A.; Wells, G.A.; Turgeon, R.D. Cryoballoon Ablation as Initial Treatment for Atrial Fibrillation: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 78, 914–930. [Google Scholar] [CrossRef]
- Leung, L.W.M.; Akhtar, Z.; Seshasai, S.R.K.; Gallagher, M.M. First-line management of paroxysmal atrial fibrillation: Is it time for a ‘pill in the bin’ approach? A discussion on the STOP AF First, EARLY AF, Cryo-FIRST, and EAST-AF NET 4 clinical trials. EP Eur. 2022, 24, 533–537. [Google Scholar] [CrossRef]
- Andrade, J.G.; Deyell, M.W.; Macle, L.; Wells, G.A.; Bennett, M.; Essebag, V.; Champagne, J.; Roux, J.F.; Yung, D.; Skanes, A.; et al. Progression of Atrial Fibrillation after Cryoablation or Drug Therapy. N. Engl. J. Med. 2022. [Google Scholar] [CrossRef] [PubMed]
- Walters, T.E.; Nisbet, A.; Morris, G.M.; Tan, G.; Mearns, M.; Teo, E.; Lewis, N.; Ng, A.; Gould, P.; Lee, G.; et al. Progression of atrial remodeling in patients with high-burden atrial fibrillation: Implications for early ablative intervention. Heart Rhythm 2016, 13, 331–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Atienza, F.; Almendral, J.; Ormaetxe, J.M.; Moya, A.; Martínez-Alday, J.D.; Hernández-Madrid, A.; Castellanos, E.; Arribas, F.; Arias, M.; Tercedor, L.; et al. Comparison of radiofrequency catheter ablation of drivers and circumferential pulmonary vein isolation in atrial fibrillation: A noninferiority randomized multicenter RADAR-AF trial. J. Am. Coll. Cardiol. 2014, 64, 2455–2467. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vogler, J.; Willems, S.; Sultan, A.; Schreiber, D.; Lüker, J.; Servatius, H.; Schäffer, B.; Moser, J.; Hoffmann, B.A.; Steven, D. Pulmonary Vein Isolation Versus Defragmentation: The CHASE-AF Clinical Trial. J. Am. Coll. Cardiol. 2015, 66, 2743–2752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Verma, A.; Jiang, C.Y.; Betts, T.R.; Chen, J.; Deisenhofer, I.; Mantovan, R.; Macle, L.; Morillo, C.A.; Haverkamp, W.; Weerasooriya, R.; et al. Approaches to catheter ablation for persistent atrial fibrillation. N. Engl. J. Med. 2015, 372, 1812–1822. [Google Scholar] [CrossRef]
- Fink, T.; Schlüter, M.; Heeger, C.H.; Lemes, C.; Maurer, T.; Reissmann, B.; Riedl, J.; Rottner, L.; Santoro, F.; Schmidt, B.; et al. Stand-Alone Pulmonary Vein Isolation Versus Pulmonary Vein Isolation With Additional Substrate Modification as Index Ablation Procedures in Patients With Persistent and Long-Standing Persistent Atrial Fibrillation: The Randomized Alster-Lost-AF Trial (Ablation at St. Georg Hospital for Long-Standing Persistent Atrial Fibrillation). Circulation. Arrhythmia Electrophysiol. 2017, 10, e005114. [Google Scholar] [CrossRef]
- Dohi, T.; Nakatani, D.; Inoue, K.; Hikoso, S.; Oka, T.; Hayashi, K.; Masuda, M.; Furukawa, Y.; Kawasaki, M.; Egami, Y.; et al. Effect of Extensive Ablation on Recurrence in Patients with Persistent Atrial Fibrillation Treated with Pulmonary Vein Isolation (EARNEST-PVI) trial: Design and rationale. J. Cardiol. 2019, 74, 164–168. [Google Scholar] [CrossRef]
- Lee, J.M.; Shim, J.; Park, J.; Yu, H.T.; Kim, T.H.; Park, J.K.; Uhm, J.S.; Kim, J.B.; Joung, B.; Lee, M.H.; et al. The Electrical Isolation of the Left Atrial Posterior Wall in Catheter Ablation of Persistent Atrial Fibrillation. JACC Clin. Electrophysiol. 2019, 5, 1253–1261. [Google Scholar] [CrossRef]
- Omran, H.; Gutleben, K.J.; Molatta, S.; Fischbach, T.; Wellmann, B.; Horstkotte, D.; Körber, B.; Nölker, G. Second generation cryoballoon ablation for persistent atrial fibrillation: An updated meta-analysis. Clin. Res. Cardiol. 2018, 107, 182–192. [Google Scholar] [CrossRef]
- Romero, J.; Gabr, M.; Alviz, I.; Briceno, D.; Diaz, J.C.; Rodriguez, D.; Patel, K.; Polanco, D.; Trivedi, C.; Mohanty, S.; et al. Improved survival in patients with atrial fibrillation and heart failure undergoing catheter ablation compared to medical treatment: A systematic review and meta-analysis of randomized controlled trials. J. Cardiovasc. Electrophysiol. 2022, 33, 2356–2366. [Google Scholar] [CrossRef]
- Rordorf, R.; Scazzuso, F.; Chun, K.R.J.; Khelae, S.K.; Kueffer, F.J.; Braegelmann, K.M.; Okumura, K.; Al-Kandari, F.; On, Y.K.; Földesi, C. Cryoballoon Ablation for the Treatment of Atrial Fibrillation in Patients With Concomitant Heart Failure and Either Reduced or Preserved Left Ventricular Ejection Fraction: Results From the Cryo AF Global Registry. J. Am. Heart Assoc. 2021, 10, e021323. [Google Scholar] [CrossRef] [PubMed]
- Prabhu, S.; Ahluwalia, N.; Tyebally, S.M.; Dennis, A.S.C.; Malomo, S.O.; Abiodun, A.T.; Tyrlis, A.; Dhillon, G.; Segan, L.; Graham, A.; et al. Long-term outcomes of index cryoballoon ablation or point-by-point radiofrequency ablation in patients with atrial fibrillation and systolic heart failure. J. Cardiovasc. Electrophysiol. 2021, 32, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, T.; Murakami, M.; Saito, S.; Iwasaki, K. Characteristics of anatomical difficulty for cryoballoon ablation: Insights from CT. Open Heart 2022, 9, e001724. [Google Scholar] [CrossRef] [PubMed]
- Thorning, C.; Hamady, M.; Liaw, J.V.; Juli, C.; Lim, P.B.; Dhawan, R.; Peters, N.S.; Davies, D.W.; Kanagaratnam, P.; O’Neill, M.D.; et al. CT evaluation of pulmonary venous anatomy variation in patients undergoing catheter ablation for atrial fibrillation. Clin. Imaging 2011, 35, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Merchant, F.M.; Levy, M.R.; Iravanian, S.; Clermont, E.C.; Kelli, H.M.; Eisner, R.L.; El-Chami, M.F.; Leon, A.R.; Delurgio, D.B. Pulmonary vein anatomy assessed by cardiac magnetic resonance imaging in patients undergoing initial atrial fibrillation ablation: Implications for novel ablation technologies. J. Interv. Card. Electrophysiol. 2016, 46, 89–96. [Google Scholar] [CrossRef]
- Beiert, T.; Lodde, P.C.; Linneborn, L.P.T.; Werner, J.; Prinz, L.; Stöckigt, F.; Linhart, M.; Lickfett, L.; Nickenig, G.; Schrickel, J.W.; et al. Outcome in patients with left common pulmonary vein after cryoablation with second-generation cryoballoon. Pacing Clin. Electrophysiol. PACE 2018, 41, 22–27. [Google Scholar] [CrossRef]
- Ströker, E.; Takarada, K.; de Asmundis, C.; Abugattas, J.P.; Mugnai, G.; Velagić, V.; de Regibus, V.; Coutiño, H.E.; Choudhury, R.; Iacopino, S.; et al. Second-generation cryoballoon ablation in the setting of left common pulmonary veins: Procedural findings and clinical outcome. Heart Rhythm 2017, 14, 1311–1318. [Google Scholar] [CrossRef]
- Garcia, R.; Waldmann, V.; Vanduynhoven, P.; Nesti, M.; Jansen de Oliveira Figueiredo, M.; Narayanan, K.; Conte, G.; Guerra, J.M.; Boveda, S.; Duncker, D. Worldwide sedation strategies for atrial fibrillation ablation: Current status and evolution over the last decade. EP Eur. 2021, 23, 2039–2045. [Google Scholar] [CrossRef]
- Di Biase, L.; Conti, S.; Mohanty, P.; Bai, R.; Sanchez, J.; Walton, D.; John, A.; Santangeli, P.; Elayi, C.S.; Beheiry, S.; et al. General anesthesia reduces the prevalence of pulmonary vein reconnection during repeat ablation when compared with conscious sedation: Results from a randomized study. Heart Rhythm 2011, 8, 368–372. [Google Scholar] [CrossRef]
- Attanasio, P.; Huemer, M.; Shokor Parwani, A.; Boldt, L.H.; Mügge, A.; Haverkamp, W.; Wutzler, A. Pain Reactions during Pulmonary Vein Isolation under Deep Sedation: Cryothermal versus Radiofrequency Ablation. Pacing Clin. Electrophysiol. PACE 2016, 39, 452–457. [Google Scholar] [CrossRef]
- Chang, T.Y.; Lo, L.W.; Te, A.L.D.; Ishigaki, S.; Maesato, A.; Lin, Y.J.; Chang, S.L.; Hu, Y.F.; Chung, F.P.; Lin, C.Y.; et al. Deep Sedation with Intravenous Anesthesia Is Associated with Outcome in Patients Undergoing Cryoablation for Paroxysmal Atrial Fibrillation. Int. Heart J. 2021, 62, 779–785. [Google Scholar] [CrossRef] [PubMed]
- Ströker, E.; de Asmundis, C.; Kupics, K.; Takarada, K.; Mugnai, G.; De Cocker, J.; Stockman, D.; Sieira, J.; Schwagten, B.; Brugada, P.; et al. Value of ultrasound for access guidance and detection of subclinical vascular complications in the setting of atrial fibrillation cryoballoon ablation. EP Eur. 2019, 21, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Bordignon, S.; Chen, S.; Bologna, F.; Thohoku, S.; Urbanek, L.; Willems, F.; Zanchi, S.; Bianchini, L.; Trolese, L.; Konstantinou, A.; et al. Optimizing cryoballoon pulmonary vein isolation: Lessons from >1000 procedures- the Frankfurt approach. EP Eur. 2021, 23, 868–877. [Google Scholar] [CrossRef]
- Su, W.; Kowal, R.; Kowalski, M.; Metzner, A.; Svinarich, J.T.; Wheelan, K.; Wang, P. Best practice guide for cryoballoon ablation in atrial fibrillation: The compilation experience of more than 3000 procedures. Heart Rhythm 2015, 12, 1658–1666. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coutiño, H.E.; Takarada, K.; Sieira, J.; Abugattas, J.P.; Salghetti, F.; De Regibus, V.; Ströker, E.; Brugada, P.; Iacopino, S.; de Asmundis, C.; et al. Anatomical and procedural predictors of pulmonary vein stenosis in the setting of second-generation cryoballoon ablation. J. Cardiovasc. Med. 2018, 19, 290–296. [Google Scholar] [CrossRef]
- Su, W.; Aryana, A.; Passman, R.; Singh, G.; Hokanson, R.; Kowalski, M.; Andrade, J.; Wang, P. Cryoballoon Best Practices II: Practical guide to procedural monitoring and dosing during atrial fibrillation ablation from the perspective of experienced users. Heart Rhythm 2018, 15, 1348–1355. [Google Scholar] [CrossRef]
- Chun, K.J.; Bordignon, S.; Gunawardene, M.; Urban, V.; Kulikoglu, M.; Schulte-Hahn, B.; Nowak, B.; Schmidt, B. Single transseptal big Cryoballoon pulmonary vein isolation using an inner lumen mapping catheter. Pacing Clin. Electrophysiol. PACE 2012, 35, 1304–1311. [Google Scholar] [CrossRef]
- Aryana, A.; Mugnai, G.; Singh, S.M.; Pujara, D.K.; de Asmundis, C.; Singh, S.K.; Bowers, M.R.; Brugada, P.; d’Avila, A.; O’Neill, P.G.; et al. Procedural and biophysical indicators of durable pulmonary vein isolation during cryoballoon ablation of atrial fibrillation. Heart Rhythm 2016, 13, 424–432. [Google Scholar] [CrossRef] [Green Version]
- Ciconte, G.; Mugnai, G.; Sieira, J.; Velagić, V.; Saitoh, Y.; Irfan, G.; Hunuk, B.; Ströker, E.; Conte, G.; Di Giovanni, G.; et al. On the Quest for the Best Freeze: Predictors of Late Pulmonary Vein Reconnections After Second-Generation Cryoballoon Ablation. Circ. Arrhythmia Electrophysiol. 2015, 8, 1359–1365. [Google Scholar] [CrossRef]
- Chierchia, G.B.; de Asmundis, C.; Namdar, M.; Westra, S.; Kuniss, M.; Sarkozy, A.; Bayrak, F.; Ricciardi, D.; Casado-Arroyo, R.; Rodriguez Manero, M.; et al. Pulmonary vein isolation during cryoballoon ablation using the novel Achieve inner lumen mapping catheter: A feasibility study. EP Eur. 2012, 14, 962–967. [Google Scholar] [CrossRef]
- Kühne, M.; Knecht, S.; Altmann, D.; Ammann, P.; Schaer, B.; Osswald, S.; Sticherling, C. Validation of a novel spiral mapping catheter for real-time recordings from the pulmonary veins during cryoballoon ablation of atrial fibrillation. Heart Rhythm 2013, 10, 241–246. [Google Scholar] [CrossRef]
- Chan, N.Y.; Yuen, H.C.; Chu, P.S.; Choy, C.C.; Chow, H.F.; Fong, H.F.; Lau, C.L.; Lo, Y.K.; Tsui, P.T.; Lau, S.T.; et al. Inner lumen mapping catheter-facilitated big cryoballoon treatment for atrial fibrillation shortens procedural duration and fluoroscopic exposure with comparable mid-term efficacy. J. Interv. Card. Electrophysiol. 2013, 37, 169–177. [Google Scholar] [CrossRef]
- Aryana, A.; Kowalski, M.; O’Neill, P.G.; Koo, C.H.; Lim, H.W.; Khan, A.; Hokanson, R.B.; Bowers, M.R.; Kenigsberg, D.N.; Ellenbogen, K.A. Catheter ablation using the third-generation cryoballoon provides an enhanced ability to assess time to pulmonary vein isolation facilitating the ablation strategy: Short- and long-term results of a multicenter study. Heart Rhythm 2016, 13, 2306–2313. [Google Scholar] [CrossRef] [Green Version]
- Tsiachris, D.; Doundoulakis, I.; Antoniou, C.K.; Pagkalidou, E.; Zafeiropoulos, S.; Kordalis, A.; Gatzoulis, K.A.; Chierchia, G.B.; de Asmundis, C.; Tsioufis, K.; et al. Effectiveness and safety of a time to isolation strategy of cryoballoon ablation of atrial fibrillation: A systematic review and meta-analysis. J. Cardiovasc. Electrophysiol. 2022, 33, 2640–2648. [Google Scholar] [CrossRef]
- Bordignon, S.; Fürnkranz, A.; Perrotta, L.; Dugo, D.; Konstantinou, A.; Nowak, B.; Schulte-Hahn, B.; Schmidt, B.; Chun, K.R. High rate of durable pulmonary vein isolation after second-generation cryoballoon ablation: Analysis of repeat procedures. EP Eur. 2015, 17, 725–731. [Google Scholar] [CrossRef]
- Ciconte, G.; Velagić, V.; Mugnai, G.; Saitoh, Y.; Irfan, G.; Hunuk, B.; Ströker, E.; Conte, G.; Sieira, J.; Di Giovanni, G.; et al. Electrophysiological findings following pulmonary vein isolation using radiofrequency catheter guided by contact-force and second-generation cryoballoon: Lessons from repeat ablation procedures. EP Eur. 2016, 18, 71–77. [Google Scholar] [CrossRef] [Green Version]
- Reddy, V.Y.; Sediva, L.; Petru, J.; Skoda, J.; Chovanec, M.; Chitovova, Z.; Di Stefano, P.; Rubin, E.; Dukkipati, S.; Neuzil, P. Durability of Pulmonary Vein Isolation with Cryoballoon Ablation: Results from the Sustained PV Isolation with Arctic Front Advance (SUPIR) Study. J. Cardiovasc. Electrophysiol. 2015, 26, 493–500. [Google Scholar] [CrossRef]
- Miyazaki, S.; Taniguchi, H.; Hachiya, H.; Nakamura, H.; Takagi, T.; Hirao, K.; Iesaka, Y. Clinical recurrence and electrical pulmonary vein reconnections after second-generation cryoballoon ablation. Heart Rhythm 2016, 13, 1852–1857. [Google Scholar] [CrossRef]
- Miyazaki, S.; Kajiyama, T.; Watanabe, T.; Nakamura, H.; Hachiya, H.; Tada, H.; Iesaka, Y. Predictors of durable pulmonary vein isolation after second-generation cryoballoon ablation with a single short freeze strategy—Different criteria for the best freeze of the 4 individual PVs. Int. J. Cardiol. 2020, 301, 96–102. [Google Scholar] [CrossRef]
- Scala, O.; Borio, G.; Paparella, G.; Varnavas, V.; Ströker, E.; Guimaraes Osorio, T.; Terasawa, M.; Sieira, J.; Maj, R.; Rizzo, A.; et al. Predictors of durable electrical isolation in the setting of second-generation cryoballoon ablation: A comparison between left superior, left inferior, right superior, and right inferior pulmonary veins. J. Cardiovasc. Electrophysiol. 2020, 31, 128–136. [Google Scholar] [CrossRef]
- Heeger, C.H.; Wissner, E.; Mathew, S.; Deiss, S.; Lemes, C.; Rillig, A.; Wohlmuth, P.; Reissmann, B.; Tilz, R.R.; Ouyang, F.; et al. Once Isolated, Always Isolated? Incidence and Characteristics of Pulmonary Vein Reconduction After Second-Generation Cryoballoon-Based Pulmonary Vein Isolation. Circ. Arrhythmia Electrophysiol. 2015, 8, 1088–1094. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mugnai, G.; Cecchini, F.; Stroker, E.; Paparella, G.; Iacopino, S.; Sieira, J.; De Greef, Y.; Tomasi, L.; Bolzan, B.; Bala, G.; et al. Durability of pulmonary vein isolation following cryoballoon ablation: Lessons from a large series of repeat ablation procedures. Int. J. Cardiology. Heart Vasc. 2022, 40, 101040. [Google Scholar] [CrossRef]
- Mörtsell, D.; Arbelo, E.; Dagres, N.; Brugada, J.; Laroche, C.; Trines, S.A.; Malmborg, H.; Höglund, N.; Tavazzi, L.; Pokushalov, E.; et al. Cryoballoon vs. radiofrequency ablation for atrial fibrillation: A study of outcome and safety based on the ESC-EHRA atrial fibrillation ablation long-term registry and the Swedish catheter ablation registry. EP Eur. 2018, 21, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Piccini, J.P.; Braegelmann, K.M.; Simma, S.; Koneru, J.N.; Ellenbogen, K.A. Risk of atrioesophageal fistula with cryoballoon ablation of atrial fibrillation. Heart Rhythm O2 2020, 1, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Kapur, S.; Barbhaiya, C.; Deneke, T.; Michaud, G.F. Esophageal Injury and Atrioesophageal Fistula Caused by Ablation for Atrial Fibrillation. Circulation 2017, 136, 1247–1255. [Google Scholar] [CrossRef] [PubMed]
- John, R.M.; Kapur, S.; Ellenbogen, K.A.; Koneru, J.N. Atrioesophageal fistula formation with cryoballoon ablation is most commonly related to the left inferior pulmonary vein. Heart Rhythm 2017, 14, 184–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pappone, C.; Vicedomini, G.; Santinelli, V. Atrio-Esophageal Fistula After AF Ablation: Pathophysiology, Prevention &Treatment. J. Atr. Fibrillation 2013, 6, 860. [Google Scholar] [CrossRef]
- Packer, D.L.; Kowal, R.C.; Wheelan, K.R.; Irwin, J.M.; Champagne, J.; Guerra, P.G.; Dubuc, M.; Reddy, V.; Nelson, L.; Holcomb, R.G.; et al. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation: First results of the North American Arctic Front (STOP AF) pivotal trial. J. Am. Coll. Cardiol. 2013, 61, 1713–1723. [Google Scholar] [CrossRef] [Green Version]
- Lakhani, M.; Saiful, F.; Parikh, V.; Goyal, N.; Bekheit, S.; Kowalski, M. Recordings of diaphragmatic electromyograms during cryoballoon ablation for atrial fibrillation accurately predict phrenic nerve injury. Heart Rhythm 2014, 11, 369–374. [Google Scholar] [CrossRef]
- Mondésert, B.; Andrade, J.G.; Khairy, P.; Guerra, P.G.; Dyrda, K.; Macle, L.; Rivard, L.; Thibault, B.; Talajic, M.; Roy, D.; et al. Clinical experience with a novel electromyographic approach to preventing phrenic nerve injury during cryoballoon ablation in atrial fibrillation. Circ. Arrhythmia Electrophysiol. 2014, 7, 605–611. [Google Scholar] [CrossRef]
- Mugnai, G.; de Asmundis, C.; Iacopino, S.; Ströker, E.; Longobardi, M.; Negro, M.C.; De Regibus, V.; Coutino-Moreno, H.E.; Takarada, K.; Choudhury, R.; et al. Acute pericarditis following second-generation cryoballoon ablation for atrial fibrillation. J. Interv. Card. Electrophysiol. 2018, 51, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Cappato, R.; Calkins, H.; Chen, S.A.; Davies, W.; Iesaka, Y.; Kalman, J.; Kim, Y.H.; Klein, G.; Natale, A.; Packer, D.; et al. Delayed cardiac tamponade after radiofrequency catheter ablation of atrial fibrillation: A worldwide report. J. Am. Coll. Cardiol. 2011, 58, 2696–2697. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Portoles-Hernandez, A.; Toquero-Ramos, J.; Garcia-Gomez, S.; Castro-Urda, V.; Garcia-Izquierdo, E.; Jimenez-Sanchez, D.; Segura-Dominguez, M.; Aguilera-Agudo, C.; Veloza-Urrea, D.; Fernandez-Lozano, I. Same-day discharge for atrial fibrillation ablation: Use of suture-mediated vascular closure device. EP Eur. 2021, 23, euab116-291. [Google Scholar] [CrossRef]
- Rashedi, S.; Tavolinejad, H.; Kazemian, S.; Mardani, M.; Masoudi, M.; Masoudkabir, F.; Haghjoo, M. Efficacy and safety of same-day discharge after atrial fibrillation ablation: A systematic review and meta-analysis. Clin. Cardiol. 2022, 45, 162–172. [Google Scholar] [CrossRef]
- Deyell, M.W.; Hoskin, K.; Forman, J.; Laksman, Z.W.; Hawkins, N.M.; Bennett, M.T.; Yeung-Lai-Wah, J.A.; Chakrabarti, S.; Krahn, A.D.; Andrade, J.G. Same-day discharge for atrial fibrillation ablation: Outcomes and impact of ablation modality. EP Eur. 2022, euac170. [Google Scholar] [CrossRef] [PubMed]


| Patients (% Males) | Age | LAd (mm) | Monitoring Method | Cryo Protocol | Freedom from AF/AT (%) | |
|---|---|---|---|---|---|---|
| EARLY AF [23] | 303 (71%) | 59 | 39 | ECG ILR | (26.1), TTI | (89 vs. 73.8)—ECG (67.8 vs. 42.9)—ILR |
| STOP AF [24] | 203 (59%) | 61 | 38.5 | 24 h Holter | (20.9), no TTI | (74 vs. 45) |
| CRYO FIRST [25] | 218 (68%) | 52 | 38.5 | 7d Holter | Not standard | (82.2 vs. 67.6) |
| Redo Period | Patients | PVI | PVs Isolated | Predictors of Durability | |
|---|---|---|---|---|---|
| Bordignon 2015 [56] | 192 days | 18 | 6 | 55/71 | CB2 vs. CB1 |
| Ciconte 2015 [58] | 11.6 months | 29 | 9 | 90/115 | TTI < 60 s, Time to −40 °C < 60 s |
| Aryana 2016 [54] | 14 months | 112 | 41 | 324/435 | TTI < 60 s, thawing time to 0 °C >10 s |
| Ciconte 2016 [57] | 9.8 months | 26 | 8 | 82/103 | TTI, nadir T |
| Reddy 2015 [59] | 3 months | 21 (19) | 15 | 68/75 | Occlusion grade |
| Miyazaki 2016 [60] | 6 months | 40 | 15 | 119/158 | Conduction delay |
| Miyazaki 2019 [61] | 7 months | 101 | 46 | 303/369 | Nadir T, TTI, freezing and thawing speed |
| Scala 2020 [62] | 18.8 months | 148 | 68 | 377/487 (581) | Time to −40 °C, Nadir T, T at 60 s |
| Heeger 2015 [63] | 205 days | 66 | 17 | 178/258 | Mean nadir T |
| Mugnai 2022 [64] | 18.2 months | 300 | 123 | 969/1178 | Nadir T, TTI, time to −40 °C < 60 s |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsiachris, D.; Antoniou, C.-K.; Doundoulakis, I.; Manolakou, P.; Sougiannis, D.; Kordalis, A.; Gatzoulis, K.A.; Chierchia, G.-B.; de Asmundis, C.; Stefanadis, C.; et al. Best Practice Guide for Cryoballoon Ablation in Atrial Fibrillation: The Compilation Experience of More than 1000 Procedures. J. Cardiovasc. Dev. Dis. 2023, 10, 55. https://doi.org/10.3390/jcdd10020055
Tsiachris D, Antoniou C-K, Doundoulakis I, Manolakou P, Sougiannis D, Kordalis A, Gatzoulis KA, Chierchia G-B, de Asmundis C, Stefanadis C, et al. Best Practice Guide for Cryoballoon Ablation in Atrial Fibrillation: The Compilation Experience of More than 1000 Procedures. Journal of Cardiovascular Development and Disease. 2023; 10(2):55. https://doi.org/10.3390/jcdd10020055
Chicago/Turabian StyleTsiachris, Dimitriοs, Christos-Konstantinos Antoniou, Ioannis Doundoulakis, Panagiota Manolakou, Demetrios Sougiannis, Athanasios Kordalis, Konstantinos A. Gatzoulis, Gian-Battista Chierchia, Carlo de Asmundis, Christodoulos Stefanadis, and et al. 2023. "Best Practice Guide for Cryoballoon Ablation in Atrial Fibrillation: The Compilation Experience of More than 1000 Procedures" Journal of Cardiovascular Development and Disease 10, no. 2: 55. https://doi.org/10.3390/jcdd10020055
APA StyleTsiachris, D., Antoniou, C.-K., Doundoulakis, I., Manolakou, P., Sougiannis, D., Kordalis, A., Gatzoulis, K. A., Chierchia, G.-B., de Asmundis, C., Stefanadis, C., & Tsioufis, K. (2023). Best Practice Guide for Cryoballoon Ablation in Atrial Fibrillation: The Compilation Experience of More than 1000 Procedures. Journal of Cardiovascular Development and Disease, 10(2), 55. https://doi.org/10.3390/jcdd10020055










