Socioeconomic Macro-Level Determinants of Hypertension: Ecological Analysis of 138 Low- and Middle-Income Countries
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Source
2.3. Outcome
2.4. Socioeconomic Determinants
2.5. Statistical Analyses
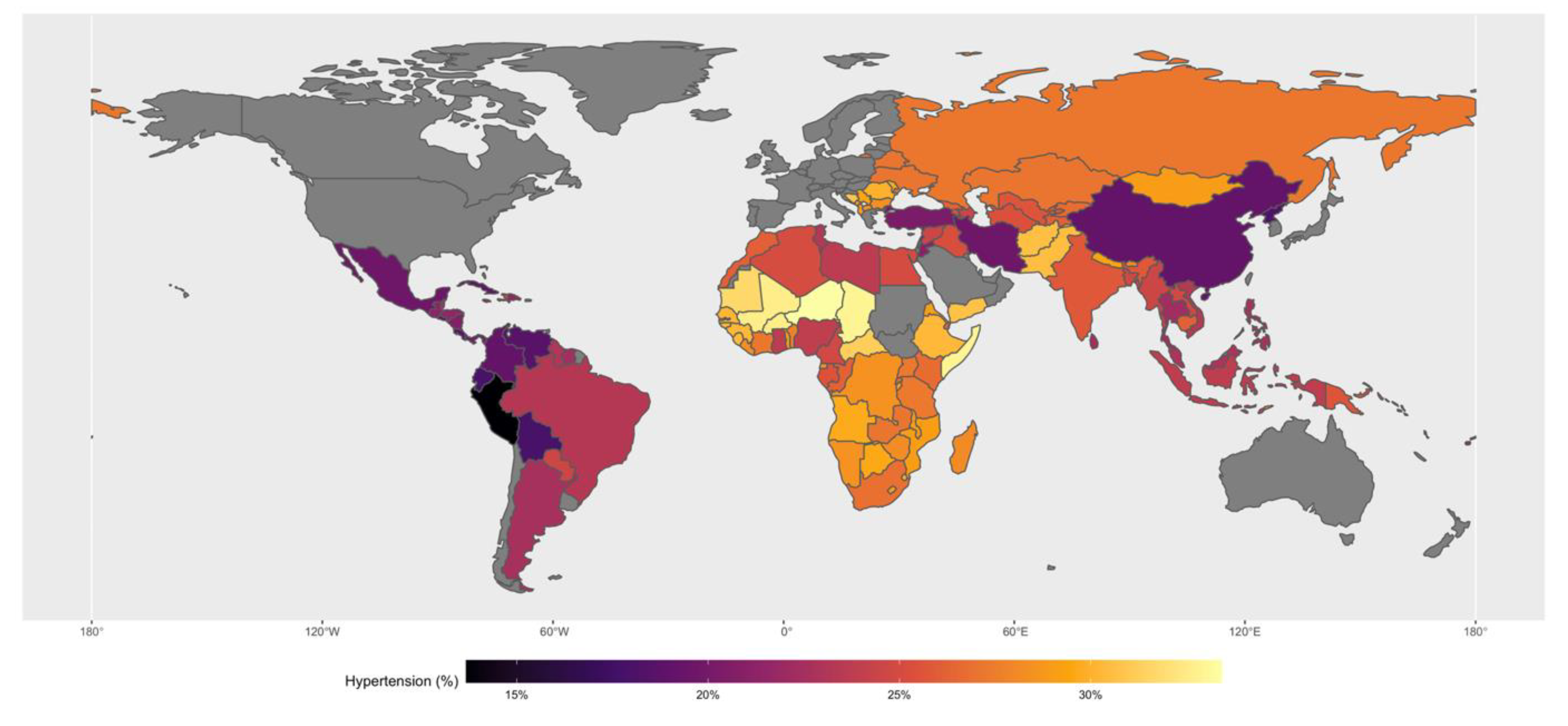
3. Results
4. Discussion
4.1. Limitations
4.2. Policy Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | VIF | SQRT VIF | Tolerance | R-Squared |
|---|---|---|---|---|
| CHE | 1.33 | 1.15 | 0.754 | 0.246 |
| DHE | 2.23 | 1.49 | 0.4487 | 0.5513 |
| GDP | 3.15 | 1.77 | 0.3178 | 0.6822 |
| Literacy | 3.97 | 1.99 | 0.2519 | 0.7481 |
| Unemployment | 1.27 | 1.13 | 0.7888 | 0.2112 |
| Urban | 1.82 | 1.35 | 0.5492 | 0.4508 |
| MPI_person | 5.26 | 2.29 | 0.19 | 0.81 |
| Population | 1.07 | 1.04 | 0.9305 | 0.0695 |
| Mean VIF | 2.51 |
References
- Ridwanah, A.A.; Megatsari, H.; Laksono, A.D. Hypertension in Indonesia in 2018: An Ecological Analysis. Indian J. Forensic. Med. Toxicol. 2021, 15, 2073. [Google Scholar]
- World Health Organisation. A Global Brief on Hypertension: Silent Killer, Global Public Health Crisis: World Health Day 2013; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Mozaffarian, D. Global scourge of cardiovascular disease: Time for health care systems reform and precision population health. J. Am. Coll. Cardiol. 2017, 70, 26–28. [Google Scholar] [CrossRef] [PubMed]
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Kumar, J. Epidemiology of hypertension. Clin. Queries Nephrol. 2013, 2, 56–61. [Google Scholar] [CrossRef]
- Geldsetzer, P.; Manne-Goehler, J.; Marcus, M.-E.; Ebert, C.; Zhumadilov, Z.; Wesseh, C.S.; Tsabedze, L.; Supiyev, A.; Sturua, L.; Bahendeka, S.K.; et al. The state of hypertension care in 44 low-income and middle-income countries: A cross-sectional study of nationally representative individual-level data from 1· 1 million adults. Lancet 2019, 394, 652–662. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, B.; Bentham, J.; Di Cesare, M.; Bixby, H.; Danaei, G.; Cowan, M.J.; Paciorek, C.J.; Singh, G.; Hajifathalian, K.; Bennett, J.E.; et al. Worldwide trends in blood pressure from 1975 to 2015: A pooled analysis of 1479 population-based measurement studies with 19· 1 million participants. Lancet 2017, 389, 37–55. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cuschieri, S.; Vassallo, J.; Calleja, N.; Pace, N.; Mamo, J. The effects of socioeconomic determinants on hypertension in a cardiometabolic at-risk European country. Int. J. Hypertens. 2017, 2017, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Abba, M.S.; Nduka, C.U.; Anjorin, S.; Mohamed, S.F.; Agogo, E.; Uthman, O.A. Influence of contextual socioeconomic position on hypertension risk in low-and middle-income countries: Disentangling context from composition. BMC Public Health 2021, 21, 1–13. [Google Scholar] [CrossRef]
- Gupta, R.; Kaur, M.; Islam, S.; Mohan, V.; Mony, P.; Kumar, R.; Kutty, V.R.; Iqbal, R.; Rahman, O.; Deepa, M.; et al. Association of household wealth index, educational status, and social capital with hypertension awareness, treatment, and control in South Asia. Am. J. Hypertens. 2017, 30, 373–381. [Google Scholar] [CrossRef] [Green Version]
- Cois, A.; Ehrlich, R. Analysing the socioeconomic determinants of hypertension in South Africa: A structural equation modelling approach. BMC Public Health 2014, 14, 414. [Google Scholar] [CrossRef] [Green Version]
- Grotto, I.; Huerta, M.; Sharabi, Y. Hypertension and socioeconomic status. Curr. Opin. Cardiol. 2008, 23, 335–339. [Google Scholar] [CrossRef] [PubMed]
- Leng, B.; Jin, Y.; Li, G.; Chen, L.; Jin, N. Socioeconomic status and hypertension: A meta-analysis. J. Hypertens. 2015, 33, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Angkurawaranon, C.; Nitsch, D.; Larke, N.; Rehman, A.M.; Smeeth, L.; Addo, J. Ecological study of HIV infection and hypertension in sub-Saharan Africa: Is there a double burden of disease? PLoS ONE 2016, 11, e0166375. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andrade, J.M.O.; Rios, L.R.; Teixeira, L.S.; Vieira, F.S.; Mendes, D.C.; Vieira, M.A.; Kutty, V.R.; Kutty, V.R. Influence of socioeconomic factors on the quality of life of elderly hypertensive individuals. Ciência Saúde Coletiva 2014, 19, 3497–3504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anyabolu, E.N.; Okoye, I.C.; Chukwumobi, A.N.; Eke, O.D. Hypertension and its socioeconomic factors in a market population in Awka, Nigeria. Am. J. Med. Sci. Med. 2017, 5, 40–48. [Google Scholar]
- Sokolov-Mladenović, S.; Cvetanović, S.; Mladenović, I. R&D expenditure and economic growth: EU28 evidence for the period 2002–2012. Econ. Res.-Ekon. Istraživanja 2016, 29, 1005–1020. [Google Scholar]
- Gheorghe, A.; Griffiths, U.; Murphy, A.; Legido-Quigley, H.; Lamptey, P.; Perel, P. The economic burden of cardiovascular disease and hypertension in low-and middle-income countries: A systematic review. BMC Public Health 2018, 18, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Zeng, Z.; Chen, J.; Xiao, C.; Chen, W. A global view on prevalence of hypertension and human develop index. Ann. Glob. Health 2020, 86, 67. [Google Scholar] [CrossRef]
- Lu, C.; Schneider, M.T.; Gubbins, P.; Leach-Kemon, K.; Jamison, D.; Murray, C.J. Public financing of health in developing countries: A cross-national systematic analysis. Lancet 2010, 375, 1375–1387. [Google Scholar] [CrossRef]
- Wierzejska, E.; Giernaś, B.; Lipiak, A.; Karasiewicz, M.; Cofta, M.; Staszewski, R. A global perspective on the costs of hypertension: A systematic review. Arch. Med. Sci. AMS 2020, 16, 1078. [Google Scholar] [CrossRef]
- Krzysztoszek, J.; Koligat, D.; Ratajczak, P.; Bryl, W.; Cymerys, M.; Hoffmann, K.; Wierzejska, E.; Kleka, P.; Kleka, P. Economic aspects of hypertension treatment in Poland. Arch. Med. Sci. AMS 2014, 10, 607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schell, C.O.; Reilly, M.; Rosling, H.; Peterson, S.; Mia Ekström, A. Socioeconomic determinants of infant mortality: A worldwide study of 152 low-, middle-, and high-income countries. Scand. J. Public Health 2007, 35, 288–297. [Google Scholar] [CrossRef]
- World Health Organisation. The Top 10 Causes of Death; World Health Organisation: Geneva, Switzerland, 2020. [Google Scholar]
- World Bank. World Bank Open Data; 2020. Available online: https://data.worldbank.org/ (accessed on 17 October 1985).
- Lim, Y.-H.; Kim, H.; Kim, J.H.; Bae, S.; Park, H.Y.; Hong, Y.-C. Air pollution and symptoms of depression in elderly adults. Environ. Health Perspect. 2012, 120, 1023–1028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Glass, T.A.; McAtee, M.J. Behavioral science at the crossroads in public health: Extending horizons, envisioning the future. Soc. Sci. Med. 2006, 62, 1650–1671. [Google Scholar] [CrossRef] [PubMed]
- Shaw, C.R.; McKay, H.D. Juvenile Delinquency in Urban. Areas; University of Chicago Press: Chicago, IL, USA, 1942. [Google Scholar]
- Sposato, L.A.; Saposnik, G. Letter by Sposato and Saposnik Regarding Article,“Incidence of Stroke and Socioeconomic Neighborhood Characteristics: An Ecological Analysis of Dijon Stroke Registry”. Stroke 2011, 42, e557. [Google Scholar] [CrossRef] [Green Version]
- Dzudie, A.; Rayner, B.; Ojji, D.; Schutte, A.E.; Twagirumukiza, M.; Damasceno, A.; Ba, S.A.; Kane, A.; Kramoh, E.; Kacou, J.B.A.; et al. Roadmap to achieve 25% hypertension control in Africa by 2025. Glob. Heart 2018, 13, 45–59. [Google Scholar] [CrossRef] [Green Version]
- Cappuccio, F.P. Commentary: Epidemiological transition, migration, and cardiovascular disease. Int. J. Epidemiol. 2004, 33, 387–388. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Wilkens, J.; Meijer, E.; Sekher, T.; Bloom, D.E.; Hu, P. Hypertension awareness, treatment, and control and their association with healthcare access in the middle-aged and older Indian population: A nationwide cohort study. PLoS Med. 2022, 19, e1003855. [Google Scholar] [CrossRef]
- Giles-Corti, B.; Vernez-Moudon, A.; Reis, R.; Turrell, G.; Dannenberg, A.L.; Badland, H.; Damasceno, M.; Damasceno, M. City planning and population health: A global challenge. Lancet 2016, 388, 2912–2924. [Google Scholar] [CrossRef]
- Beaglehole, R.; Bonita, R. Global public health: A scorecard. Lancet 2008, 372, 1988–1996. [Google Scholar] [CrossRef]
- Burgoyne, D.S. Reducing economic burden and improving quality of life in pulmonary arterial hypertension. Am. J. Manag. Care 2021, 27, S53–S58. [Google Scholar] [PubMed]
| Country | Raised Blood Pressure (SBP ≥ 140 OR DBP ≥ 90), Age-Standardized (%) | Current Health Expenditure (% of GDP) | Domestic General GovernMent Health Expenditure Per Capita | GDP Per Capita (Current US$) | Literacy Rate, Adult Total (% of People Ages 15 and Above) | Unemployment, Total (% of the Total Labour Force) | Urban Population (% of the Total Population) | Multidimensional Poverty Index | Total Population |
|---|---|---|---|---|---|---|---|---|---|
| Afghanistan | 30.6 | 10.1 | 10.9 | 556.0 | 31.4 | 11.1 | 24.8 | 55.9 | 34,413,603 |
| Angola | 29.7 | 2.6 | 90.6 | 4167.0 | 66.0 | 7.4 | 63.4 | 51.1 | 27,884,380 |
| Albania | 29 | 4.9 | 317.4 | 3952.8 | 98.1 | 17.2 | 57.4 | 0.7 | 2,880,703 |
| Argentina | 22.6 | 10.2 | 1373.9 | 13,789.1 | 99.0 | 7.5 | 91.5 | N/A | 43,131,966 |
| Armenia | 25.5 | 10.1 | 160.5 | 3607.3 | 99.8 | 18.3 | 63.1 | 0.2 | 2,925,559 |
| Azerbaijan | 24.5 | 4.1 | 195.1 | 5500.3 | 99.8 | 5.0 | 54.7 | N/A | 9,649,341 |
| Burundi | 29.2 | 6.4 | 20.4 | 305.5 | 68.4 | 1.6 | 12.1 | 74.3 | 10,160,034 |
| Benin | 27.7 | 2.9 | 16.9 | 1076.8 | 42.4 | 2.0 | 45.7 | 66.8 | 10,575,962 |
| Burkina Faso | 32.6 | 5.1 | 25.0 | 653.3 | 39.3 | 4.3 | 27.5 | 83.8 | 18,110,616 |
| Bangladesh | 24.7 | 2.6 | 16.5 | 1248.5 | 74.9 | 4.4 | 34.3 | 24.6 | 156,256,287 |
| Bulgaria | 28.4 | 7.4 | 757.3 | 7074.7 | 98.4 | 9.1 | 74.0 | N/A | 7,177,991 |
| Bosnia and Herzegovina | 30.8 | 9.4 | 777.4 | 4729.7 | 97.0 | 27.7 | 47.2 | 2.2 | 3,429,362 |
| Belarus | 27.1 | 6.1 | 668.7 | 5967.1 | 99.9 | 5.8 | 77.2 | N/A | 9,461,076 |
| Belize | 22.7 | 5.9 | 292.3 | 4770.2 | N/A | 7.6 | 45.4 | 4.3 | 360,926 |
| Bolivia | 17.9 | 6.6 | 307.2 | 3036.0 | 92.5 | 3.1 | 68.4 | 20.4 | 10,869,732 |
| Brazil | 23.3 | 8.9 | 568.2 | 8814.0 | 93.2 | 8.4 | 85.8 | 3.8 | 204,471,759 |
| Bhutan | 28.1 | 3.8 | 252.6 | 2752.6 | 66.6 | 2.5 | 38.7 | 37.3 | 727,885 |
| Botswana | 29.6 | 5.7 | 603.2 | 6402.9 | 86.8 | 20.6 | 67.2 | 17.2 | 2,120,716 |
| Central African Republic | 31.2 | 5.0 | 3.6 | 377.4 | 37.4 | 5.6 | 40.3 | 79.4 | 4,493,171 |
| China | 19.2 | 4.9 | 377.7 | 8016.4 | 96.8 | 4.6 | 55.5 | 3.9 | 1,379,860,000 |
| Cote d’ Ivoire | 27.2 | 3.2 | 37.4 | 1972.5 | 89.9 | 3.1 | 49.4 | 46.1 | 23,226,148 |
| Cameroon | 24.8 | 3.7 | 12.4 | 1382.5 | 77.1 | 3.6 | 54.6 | 45.3 | 23,298,376 |
| Congo, Dem. Rep. | 28.5 | 4.0 | 6.0 | 497.3 | 77.0 | 4.5 | 42.7 | 64.5 | 76,244,532 |
| Congo, Rep. | 26.2 | 2.5 | 51.9 | 2447.5 | 80.3 | 20.4 | 65.5 | 24.3 | 4,856,093 |
| Colombia | 19.2 | 7.5 | 699.9 | 6175.9 | 95.6 | 8.3 | 79.8 | 4.8 | 47,520,667 |
| Comoros | 27.9 | 4.6 | 12.6 | 1242.6 | 58.8 | 8.1 | 28.5 | 37.3 | 777,435 |
| Cabo Verde | 29.5 | 4.8 | 190.3 | 3043.0 | 86.8 | 11.8 | 64.3 | N/A | 524,740 |
| Costa Rica | 18.7 | 7.6 | 943.4 | 11,642.8 | 97.9 | 9.0 | 76.9 | N/A | 4,847,805 |
| Cuba | 19 | 12.8 | 2872.8 | 7694.0 | 99.8 | 2.4 | 76.9 | 0.4 | 11,324,777 |
| Djibouti | 26.8 | 3.1 | 77.9 | 2658.9 | N/A | 26.3 | 77.4 | N/A | 913,998 |
| Dominica | 22.5 | 5.2 | 362.4 | 7597.3 | N/A | N/A | 69.6 | N/A | 71,175 |
| Dominican Republic | 21.5 | 5.8 | 349.1 | 6921.5 | 93.8 | 7.6 | 78.6 | 3.9 | 10,281,675 |
| Algeria | 25.1 | 7.0 | 590.8 | 4177.9 | 81.4 | 11.2 | 70.8 | 2.1 | 39,728,020 |
| Ecuador | 17.9 | 7.5 | 477.0 | 6124.5 | 93.6 | 3.6 | 63.4 | 4.6 | 16,212,022 |
| Egypt, Arab Rep. | 25 | 5.3 | 191.9 | 3562.9 | 71.2 | 13.1 | 42.8 | 5.2 | 92,442,549 |
| Eritrea | 29.1 | 4.5 | 11.8 | N/A | 76.6 | 5.8 | N/A | N/A | N/A |
| Ethiopia | 30.3 | 3.8 | 16.0 | 640.5 | 51.8 | 2.3 | 19.4 | 83.5 | 100,835,453 |
| Fiji | 21.7 | 3.3 | 260.5 | 5390.7 | N/A | 4.3 | 54.7 | N/A | 868,632 |
| Micronesia, Fed. Sts. | 25 | 12.5 | 94.7 | 2906.6 | N/A | N/A | 22.5 | N/A | 108,886 |
| Gabon | 25.5 | 2.7 | 230.1 | 7384.7 | 84.7 | 20.6 | 88.1 | 14.8 | 1,947,690 |
| Georgia | 26.3 | 7.4 | 295.5 | 4014.2 | 99.6 | 16.5 | 57.4 | 0.3 | 3,725,276 |
| Ghana | 23.7 | 4.6 | 83.0 | 1774.1 | 79.0 | 6.8 | 54.1 | 30.1 | 27,849,203 |
| Guinea | 30.3 | 5.8 | 7.8 | 769.3 | 39.6 | 4.9 | 35.1 | 66.2 | 11,432,096 |
| Gambia, The | 29.1 | 3.2 | 20.6 | 660.7 | 50.8 | 9.5 | 59.2 | 41.6 | 2,085,860 |
| Guinea-Bissau | 30.3 | 8.1 | 9.4 | 603.4 | 45.6 | 5.9 | 42.1 | 67.3 | 1,737,207 |
| Equatorial Guinea | 28.4 | 2.9 | 133.3 | 11,283.4 | 94.4 | 8.5 | 70.6 | N/A | 1,168,575 |
| Grenada | 24.3 | 4.6 | 273.8 | 9096.5 | 98.6 | N/A | 36.0 | N/A | 109,603 |
| Guatemala | 21.2 | 6.0 | 178.8 | 3994.6 | 80.8 | 2.5 | 50.0 | 28.9 | 15,567,419 |
| Guyana | 23.1 | 4.0 | 263.9 | 5576.8 | 85.6 | 13.2 | 26.4 | 3.4 | 767,433 |
| Honduras | 21.4 | 7.5 | 142.2 | 2286.2 | 88.5 | 6.2 | 55.2 | 19.3 | 9,112,904 |
| Haiti | 24.5 | 5.1 | 16.3 | 1386.9 | 61.7 | 14.0 | 52.4 | 41.3 | 10,695,540 |
| Indonesia | 23.8 | 2.9 | 118.7 | 3331.7 | 96.0 | 4.5 | 53.3 | 3.6 | 258,383,257 |
| India | 25.8 | 3.6 | 50.4 | 1605.6 | 74.4 | 5.4 | 32.8 | 27.9 | 1,310,152,392 |
| Iran, Islamic Rep. | 19.7 | 7.5 | 531.5 | 4904.3 | 85.5 | 11.2 | 73.4 | N/A | 78,492,208 |
| Iraq | 25.2 | 3.1 | 75.9 | 4688.3 | 85.6 | 10.7 | 69.9 | 8.6 | 35,572,269 |
| Jamaica | 21.8 | 5.6 | 312.9 | 4907.9 | 88.1 | 13.5 | 54.8 | 4.7 | 2,891,024 |
| Jordan | 21 | 7.5 | 378.1 | 4164.1 | 98.2 | 13.1 | 90.3 | 0.4 | 9,266,573 |
| Kazakhstan | 27.1 | 3.0 | 445.1 | 10,510.8 | 99.8 | 4.9 | 57.2 | 0.5 | 17,542,806 |
| Kenya | 26.7 | 5.2 | 70.9 | 1464.6 | 81.5 | 2.8 | 25.7 | 38.7 | 47,878,339 |
| Kyrgyz Republic | 26.7 | 7.1 | 114.2 | 1121.1 | 99.6 | 7.6 | 35.8 | 0.4 | 5,956,900 |
| Cambodia | 26.1 | 6.2 | 45.6 | 1162.9 | 80.5 | 0.4 | 22.2 | 37.2 | 15,521,435 |
| Kiribati | 21.5 | 8.0 | 143.7 | 1542.6 | N/A | N/A | 51.6 | 19.8 | 110,927 |
| Lao PDR | 24.8 | 2.5 | 53.3 | 2140.0 | 84.7 | 0.8 | 33.1 | 23.1 | 6,741,160 |
| Lebanon | 20.7 | 7.4 | 500.3 | 7663.9 | 95.1 | 9.3 | 88.1 | N/A | 6,532,681 |
| Liberia | 28.3 | 10.6 | 15.2 | 721.6 | 48.3 | 2.1 | 49.8 | 62.9 | 4,472,229 |
| Libya | 23.7 | N/A | N/A | 4337.9 | N/A | 19.5 | 79.3 | 2.0 | 6,418,315 |
| St. Lucia | 27.1 | 4.6 | 269.9 | 10,093.6 | N/A | 20.6 | 18.5 | 1.9 | 179,131 |
| Sri Lanka | 22.4 | 3.9 | 198.2 | 3843.8 | 92.3 | 4.5 | 18.3 | 2.9 | 20,970,000 |
| Lesotho | 29 | 9.0 | 165.2 | 1146.1 | 76.6 | 23.8 | 26.9 | 19.6 | 2,059,011 |
| Morocco | 26.1 | 5.1 | 150.1 | 2875.3 | 73.8 | 9.5 | 60.8 | 18.6 | 34,663,608 |
| Moldova | 29.8 | 8.6 | 287.6 | 2732.5 | 99.4 | 4.7 | 42.5 | 0.9 | 2,834,530 |
| Madagascar | 28.1 | 5.0 | 30.8 | 467.2 | 76.7 | 1.8 | 35.2 | 69.1 | 24,234,080 |
| Maldives | 24.4 | 8.7 | 1050.7 | 9033.4 | 97.7 | 6.9 | 38.5 | 0.8 | 454,914 |
| Mexico | 19.7 | 5.7 | 546.7 | 9616.6 | 95.2 | 4.3 | 79.3 | 6.6 | 121,858,251 |
| Marshall Islands | 21.3 | 17.0 | 195.4 | 3199.9 | 98.3 | N/A | 75.8 | N/A | 57,444 |
| North Macedonia | 28.5 | 6.3 | 569.6 | 4861.6 | 98.4 | 26.1 | 57.4 | 2.5 | 2,070,226 |
| Mali | 32.6 | 4.1 | 18.7 | 751.5 | 30.8 | 7.7 | 40.0 | 68.3 | 17,438,772 |
| Myanmar | 24.6 | 5.5 | 49.5 | 1196.7 | 89.1 | 0.8 | 29.9 | 38.3 | 52,680,724 |
| Montenegro | 29.1 | 9.0 | 874.6 | 6514.3 | 98.8 | 17.5 | 65.8 | 1.2 | 622,159 |
| Mongolia | 29 | 4.2 | 257.3 | 3875.3 | 99.2 | 4.9 | 68.2 | 7.3 | 2,998,433 |
| Mozambique | 29.1 | 6.7 | 23.4 | 589.9 | 60.7 | 3.4 | 34.4 | 72.5 | 27,042,001 |
| Mauritania | 31.7 | 3.7 | 59.6 | 1524.1 | 53.5 | 10.1 | 51.1 | 50.6 | 4,046,304 |
| Mauritius | 25 | 5.7 | 457.9 | 9260.4 | 91.3 | 7.4 | 41.0 | N/A | 1,262,605 |
| Malawi | 28.9 | 9.3 | 27.4 | 380.6 | 62.1 | 5.9 | 16.3 | 52.6 | 16,745,305 |
| Malaysia | 22.9 | 3.8 | 504.4 | 9955.2 | 95.0 | 3.1 | 74.2 | N/A | 30,270,965 |
| Namibia | 28.5 | 10.0 | 447.9 | 4896.6 | 91.5 | 20.9 | 46.9 | 38.0 | 2,314,901 |
| Niger | 33.4 | 5.3 | 12.7 | 484.2 | 35.0 | 0.5 | 16.2 | 90.5 | 20,001,663 |
| Nigeria | 23.9 | 3.6 | 32.0 | 2687.5 | 62.0 | 4.3 | 47.8 | 46.4 | 181,137,454 |
| Nicaragua | 20.8 | 8.0 | 236.4 | 2049.9 | 82.6 | 4.7 | 57.9 | 16.3 | 6,223,234 |
| Nepal | 29.4 | 5.5 | 27.2 | 901.7 | 67.9 | 3.1 | 18.6 | 34.0 | 27,015,033 |
| Pakistan | 30.5 | 2.7 | 32.4 | 1356.7 | 58.0 | 3.6 | 36.0 | 38.3 | 199,426,953 |
| Panama | 19.9 | 6.8 | 1089.2 | 13,630.3 | 95.7 | 3.0 | 66.7 | N/A | 3,968,490 |
| Peru | 13.7 | 5.0 | 353.7 | 6229.1 | 94.5 | 3.3 | 77.4 | 7.4 | 30,470,739 |
| Philippines | 22.6 | 3.9 | 105.5 | 3001.0 | 96.3 | 3.1 | 46.3 | 5.8 | 102,113,206 |
| Papua New Guinea | 25.6 | 1.8 | 54.7 | 2679.3 | 61.6 | 2.5 | 13.0 | 56.6 | 8,107,772 |
| Korea, Dem. People’s Rep. | 18.2 | N/A | N/A | N/A | N/A | 2.7 | 61.3 | N/A | 25,183,832 |
| Paraguay | 24.6 | 6.7 | 362.6 | 5413.8 | 94.5 | 4.6 | 60.8 | 4.5 | 6,688,746 |
| Romania | 30 | 4.9 | 830.8 | 8969.1 | 98.8 | 6.8 | 53.9 | N/A | 19,815,616 |
| Russian Federation | 27.2 | 5.3 | 756.3 | 9313.0 | 99.7 | 5.6 | 74.1 | N/A | 144,096,870 |
| Rwanda | 26.7 | 6.6 | 38.0 | 751.1 | 73.2 | 1.1 | 17.0 | 54.4 | 11,369,066 |
| Senegal | 30.2 | 4.4 | 32.0 | 1219.2 | 51.9 | 6.8 | 45.9 | 53.2 | 14,578,450 |
| Solomon Islands | 22 | 4.6 | 78.5 | 2167.1 | N/A | 0.7 | 22.4 | N/A | 603,133 |
| Sierra Leone | 30.3 | 20.4 | 26.2 | 588.2 | 43.2 | 4.7 | 40.8 | 57.9 | 7,171,909 |
| El Salvador | 18.7 | 7.6 | 372.8 | 3705.6 | 89.1 | 4.0 | 69.7 | 7.9 | 6,325,121 |
| Somalia | 32.9 | N/A | N/A | 386.4 | N/A | 18.9 | 43.2 | N/A | 13,797,204 |
| Serbia | 29.5 | 8.8 | 756.9 | 5589.0 | 99.5 | 17.7 | 55.7 | 0.3 | 7,095,383 |
| Sao Tome and Principe | 25.8 | 5.3 | 64.8 | 1584.8 | 92.8 | 13.8 | 70.2 | 22.1 | 199,439 |
| Suriname | 22.4 | 6.2 | 544.6 | 9168.2 | 94.4 | 7.2 | 66.1 | 2.9 | 559,136 |
| Eswatini | 29.8 | 7.1 | 259.8 | 3680.3 | 88.4 | 23.3 | 23.3 | 19.2 | 1,104,038 |
| Syrian Arab Republic | 24.5 | N/A | N/A | 916.4 | N/A | 8.7 | 52.2 | 7.4 | 17,997,411 |
| Chad | 32.9 | 4.5 | 17.5 | 776.0 | 22.3 | 1.1 | 22.5 | 85.7 | 14,110,971 |
| Togo | 28.9 | 5.0 | 17.8 | 570.9 | 66.5 | 2.2 | 40.1 | 37.6 | 7,323,162 |
| Thailand | 22.3 | 3.7 | 434.9 | 5840.1 | 93.8 | 0.6 | 47.7 | 0.8 | 68,714,519 |
| Tajikistan | 26.1 | 6.9 | 61.2 | 978.4 | 99.8 | 7.6 | 26.7 | 7.4 | 8,454,019 |
| Turkmenistan | 25.4 | 6.3 | 206.5 | 6432.7 | 99.7 | 4.1 | 50.3 | 0.4 | 5,565,283 |
| Timor-Leste | 27.6 | 7.7 | 128.3 | 1332.8 | 68.1 | 4.4 | 29.5 | 45.8 | 1,196,294 |
| Tonga | 23.7 | 4.7 | 159.8 | 4336.2 | 99.4 | 2.5 | 23.3 | N/A | 100,780 |
| Tunisia | 23.2 | 6.6 | 365.0 | 4094.8 | 79.0 | 15.2 | 68.1 | 0.8 | 11,179,951 |
| Turkey | 20.3 | 4.1 | 828.4 | 11,006.3 | 96.7 | 10.2 | 73.6 | N/A | 78,529,413 |
| Tuvalu | 23.7 | 16.7 | 473.9 | 3197.8 | N/A | N/A | 59.7 | N/A | 11,099 |
| Tanzania | 27.3 | 3.6 | 28.7 | 947.9 | 77.9 | 2.1 | 31.6 | 55.4 | 51,482,638 |
| Uganda | 27.3 | 5.1 | 17.2 | 847.3 | 76.5 | 1.9 | 22.1 | 55.1 | 38,225,447 |
| Ukraine | 27.1 | 7.8 | 356.9 | 2124.7 | 100.0 | 9.1 | 69.1 | 0.2 | 45,154,036 |
| Uzbekistan | 25.6 | 5.0 | 159.4 | 2754.0 | 100.0 | 5.2 | 50.8 | N/A | 31,298,900 |
| St. Vincent and the Grenadines | 23.3 | 4.1 | 306.2 | 6921.7 | N/A | 19.1 | 51.0 | N/A | 109,135 |
| Venezuela, RB | 18.6 | 4.3 | 337.1 | N/A | 97.1 | 6.1 | 88.2 | N/A | 30,081,827 |
| Vietnam | 23.4 | 4.6 | 144.2 | 2085.1 | 95.8 | 1.9 | 33.8 | 4.9 | 92,677,082 |
| Vanuatu | 24.2 | 4.3 | 59.6 | 2695.7 | 87.5 | 1.9 | 25.0 | N/A | 271,128 |
| Samoa | 24 | 5.8 | 266.8 | 4071.9 | 99.1 | 8.5 | 18.9 | N/A | 193,510 |
| Yemen, Rep. | 30.7 | 4.3 | 11.2 | 1601.8 | N/A | 13.8 | 34.8 | 47.7 | 26,497,881 |
| South Africa | 26.9 | 8.8 | 629.8 | 6259.8 | 95.0 | 25.1 | 64.8 | 6.3 | 55,386,369 |
| Zambia | 27.1 | 4.4 | 71.7 | 1338.3 | 86.7 | 10.1 | 41.9 | 47.9 | 15,879,370 |
| Zimbabwe | 28.2 | 7.5 | 41.6 | 1445.1 | 88.7 | 4.8 | 32.4 | 25.8 | 13,814,642 |
| Sudan | N/A | 7.3 | 100.4 | 1329.6 | 60.7 | 17.5 | 33.9 | 52.3 | 38,902,948 |
| South Sudan | N/A | N/A | N/A | 1119.7 | 34.5 | 12.3 | 18.9 | 91.9 | 10,715,657 |
| American Samoa | N/A | N/A | N/A | 12,059.6 | N/A | N/A | 87.2 | N/A | 55,806 |
| Kosovo | N/A | N/A | N/A | 3520.8 | N/A | N/A | N/A | N/A | 1,788,196 |
| West Bank and Gaza | N/A | N/A | N/A | 3272.2 | 97.5 | 23.0 | 75.4 | 1.0 | 4,270,092 |
| Pearson Correlation | Unadjusted Association | Adjusted Association | |
|---|---|---|---|
| Current health expenditure (% of GDP) | −0.07 (−0.24 to 0.10) | −0.93 (−3.26 to 1.40) | −0.03 (−2.25 to 2.19) |
| Domestic general government health expenditure per capita, PPP (in US$) | −0.36 (−0.50 to −0.20) | −0.04 (−0.06 to −0.02) | 0.00 (−0.02 to 0.02) |
| GDP per capita (in US$) | −0.46 (−0.59 to −0.31) | −0.55 (−0.73 to −0.36) | −0.08 (−0.44 to 0.28) |
| Literacy rate, adult total (% of people ages 15 and above) | −0.56 (−0.67 to −0.42) | −1.12 (−1.43 to −0.82) | −0.37 (−0.88 to 0.14) |
| Unemployment, total (% of total labour force) | 0.18 (0.00 to 0.34) | 1.06 (0.01 to 2.10) | 2.70 (1.82 to 3.58) |
| Urban population (% of total population) | −0.46 (−0.59 to −0.32) | −0.89 (−1.19 to −0.59) | −0.63 (−1.00 to −0.26) |
| Multidimensional poverty index | 0.59 (0.45 to 0.71) | 0.09 (0.06 to 0.11) | 0.06 (0.01 to 0.10) |
| Total population | −0.12 (−0.29 to 0.05) | −0.03 (−0.07 to 0.01) | −0.02 (−0.04 to 0.01) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abba, M.S.; Nduka, C.U.; Anjorin, S.; Zanna, F.H.; Uthman, O.A. Socioeconomic Macro-Level Determinants of Hypertension: Ecological Analysis of 138 Low- and Middle-Income Countries. J. Cardiovasc. Dev. Dis. 2023, 10, 57. https://doi.org/10.3390/jcdd10020057
Abba MS, Nduka CU, Anjorin S, Zanna FH, Uthman OA. Socioeconomic Macro-Level Determinants of Hypertension: Ecological Analysis of 138 Low- and Middle-Income Countries. Journal of Cardiovascular Development and Disease. 2023; 10(2):57. https://doi.org/10.3390/jcdd10020057
Chicago/Turabian StyleAbba, Mustapha S., Chidozie U. Nduka, Seun Anjorin, Fatima H. Zanna, and Olalekan A. Uthman. 2023. "Socioeconomic Macro-Level Determinants of Hypertension: Ecological Analysis of 138 Low- and Middle-Income Countries" Journal of Cardiovascular Development and Disease 10, no. 2: 57. https://doi.org/10.3390/jcdd10020057





