The Prolonged Effect of Shift Work and the Impact of Reducing the Number of Nightshifts on Arterial Stiffness—A 4-Year Follow-Up Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design and Population

2.2. Demographics
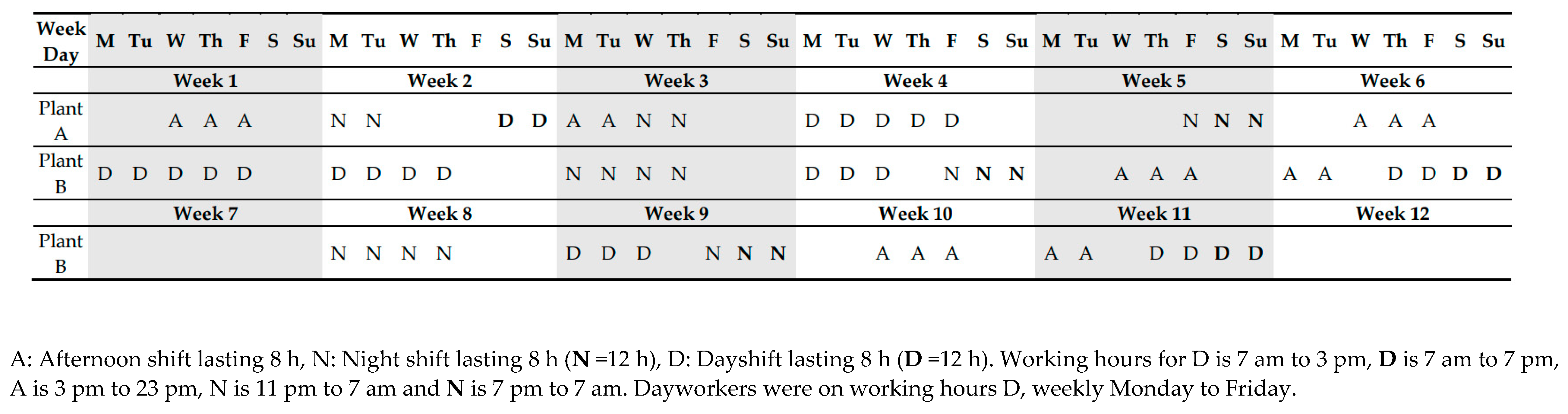
2.3. Shift Work Exposure
2.4. Brachial Blood Pressure and Resting Heart Rate
2.5. Arterial Stiffness
2.6. Sleep Measure
2.7. Statistical Analysis
3. Results
3.1. Demographic Characteristics in 2022
3.2. Cardiovascular Outcomes over the 4-Year Follow-Up
3.3. Cardiovascular Outcomes and Shift Work Schedules
3.4. Correlations
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boivin, D.B.; Boudreau, P.; Kosmadopoulos, A. Disturbance of the Circadian System in Shift Work and Its Health Impact. J. Biol. Rhythm. 2022, 37, 3–28. [Google Scholar] [CrossRef] [PubMed]
- Brum, M.C.B.; Filho, F.F.D.; Schnorr, C.C.; Bottega, G.B.; Rodrigues, T.C. Shift work and its association with metabolic disorders. Diabetol. Metab. Syndr. 2015, 7, 45. [Google Scholar] [CrossRef]
- Garde, A.H.; Harris, A.; Vedaa, Ø.; Bjorvatn, B.; Hansen, J.; Hansen, Å.M.; Kolstad, H.A.; Koskinen, A.; Pallesen, S.; Ropponen, A.; et al. Working hour characteristics and schedules among nurses in three Nordic countries—A comparative study using payroll data. BMC Nurs. 2019, 18, 12. [Google Scholar] [CrossRef]
- Kecklund, G.; Axelsson, J. Health consequences of shift work and insufficient sleep. BMJ 2016, 355, i5210. [Google Scholar] [CrossRef] [PubMed]
- Torquati, L.; Mielke, G.I.; Brown, W.J.; Kolbe-Alexander, T. Shift work and the risk of cardiovascular disease. A systematic review and meta-analysis including dose-response relationship. Scand. J. Work Environ. Health 2018, 44, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Vyas, M.V.; Garg, A.X.; Iansavichus, A.V.; Costella, J.; Donner, A.; Laugsand, L.E.; Janszky, I.; Mrkobrada, M.; Parraga, G.; Hackam, D.G. Shift work and vascular events: Systematic review and meta-analysis. BMJ 2012, 345, e4800. [Google Scholar] [CrossRef] [PubMed]
- Bigert, C.; Kader, M.; Andersson, T.; Selander, J.; Bodin, T.; Gustavsson, P.; Härmä, M.; Ljungman, P.; Albin, M. Night and shift work and incidence of cerebrovascular disease—A prospective cohort study of healthcare employees in Stockholm. Scand. J. Work. Environ. Health 2022, 48, 31–40. [Google Scholar] [CrossRef]
- Rivera, A.S.; Akanbi, M.; O’Dwyer, L.C.; McHugh, M. Shift work and long work hours and their association with chronic health conditions: A systematic review of systematic reviews with meta-analyses. PLoS ONE 2020, 15, e0231037. [Google Scholar] [CrossRef]
- Honma, S. The mammalian circadian system: A hierarchical multi-oscillator structure for generating circadian rhythm. J. Physiol. Sci. 2018, 68, 207–219. [Google Scholar] [CrossRef]
- Kim, H.-L.; Kim, S.-H. Pulse Wave Velocity in Atherosclerosis. Front. Cardiovasc. Med. 2019, 6, 41. [Google Scholar] [CrossRef]
- Donato, A.J.; Machin, D.R.; Lesniewski, L.A. Mechanisms of Dysfunction in the Aging Vasculature and Role in Age-Related Disease. Circ. Res. 2018, 123, 825–848. [Google Scholar] [CrossRef] [PubMed]
- Townsend, R.R.; Wilkinson, I.B.; Schiffrin, E.L.; Avolio, A.P.; Chirinos, J.A.; Cockcroft, J.R.; Heffernan, K.S.; Lakatta, E.G.; McEniery, C.M.; Mitchell, G.F.; et al. Recommendations for Improving and Standardizing Vascular Research on Arterial Stiffness: A Scientific Statement From the American Heart Association. Hypertension 2015, 66, 698–722. [Google Scholar] [CrossRef] [PubMed]
- Rey-García, J.; Townsend, R.R. Large Artery Stiffness: A Companion to the 2015 AHA Science Statement on Arterial Stiffness. Pulse 2021, 9, 1–10. [Google Scholar] [CrossRef]
- Mattace Raso, F.U.S.; Hofman, A.; Verwoert, C.G.; Wittemana, J.C.M.; Wilkinson, I.; Cockcroft, J.; McEniery, C.; Yasmin; Laurent, S.; Boutouyrie, P.; et al. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘establishing normal and reference values’. Eur. Heart J. 2010, 31, 2338–2350. [Google Scholar]
- Skogstad, M.; Mamen, A.; Lunde, L.-K.; Ulvestad, B.; Matre, D.; Aass, H.C.D.; Øvstebø, R.; Nielsen, P.; Samuelsen, K.N.; Skare, Ø.; et al. Shift Work Including Night Work and Long Working Hours in Industrial Plants Increases the Risk of Atherosclerosis. Int. J. Environ. Res. Public Health 2019, 16, 521. [Google Scholar] [CrossRef]
- Mamen, A.; Øvstebø, R.; Sirnes, P.A.; Nielsen, P.; Skogstad, M. High-Intensity Training Reduces CVD Risk Factors among Rotating Shift Workers: An Eight-Week Intervention in Industry. Int. J. Environ. Res. Public Health 2020, 17, 3943. [Google Scholar] [CrossRef]
- Matre, D.; Sirnes, P.A.; Goffeng, E.; Skare, Ø.; Skogstad, M. Sleep Duration, Number of Awakenings and Arterial Stiffness in In-dustrial Shift Workers: A Five-Week Follow-Up Study. Int. J. Environ. Res. Public Health 2022, 19, 1964. [Google Scholar] [CrossRef]
- Gusmão, W.D.P.; Pureza, I.R.O.M.; Moreno, C.R.C. Shift Work and Early Arterial Stiffness: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 14569. [Google Scholar] [CrossRef]
- Lunde, L.-K.; Skare, Ø.; Mamen, A.; Sirnes, P.A.; Aass, H.C.D.; Øvstebø, R.; Goffeng, E.; Matre, D.; Nielsen, P.; Heglum, H.S.A.; et al. Cardiovascular Health Effects of Shift Work with Long Working Hours and Night Shifts: Study Protocol for a Three-Year Prospective Follow-Up Study on Industrial Workers. Int. J. Environ. Res. Public Health 2020, 17, 589. [Google Scholar] [CrossRef]
- Skogstad, M.; Aas, H.C.D.; Sirnes, P.A.; Mamen, A.; Skare, Ø.; Matre, D.; Hammer, S.E.; Goffeng, E.; Lunde, L.-K. Influence of shift work on arterial stiffness and systematic inflammation: A three-year follow-up study in industry. J. Occup. Environ. Med. 2022. [Google Scholar] [CrossRef]
- Skogstad, M.; Aass, H.C.D.; Lunde, L.-K.; Skare, Ø.; Sirnes, P.A.; Matre, D. A cease in shift work reverses arterial stiffness but increases weight and glycosylated hemoglobin. A 5-month follow-up in industry. J. Cardiovasc. Dev. Dis 2022, 9, 190. [Google Scholar] [CrossRef]
- Pallesen, S.; Bjorvatn, B.; Nordhus, I.H.; Sivertsen, B.; Hjørnevik, M.; Morin, C.M. A New Scale for Measuring Insomnia: The Bergen Insomnia Scale. Percept. Mot. Ski. 2008, 107, 691–706. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. R. Stat. Soc. Ser. B 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Gamboa Madeira, S.; Fernandes, C.; Paiva, T.; Santos Moreira, C.; Caldeira, D. The Impact of Different Types of Shift Work on Blood Pressure and Hypertension: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6738. [Google Scholar] [CrossRef] [PubMed]
- Díaz, A.; Galli, C.; Tringler, M.; Ramírez, A.; Cabrera Fischer, E.I. Reference values of pulse wave velocity in healthy people from an urban and rural argentinean population. Int. J. Hypertens. 2014, 2014, 653239. [Google Scholar] [CrossRef] [PubMed]
- van Hout, M.J.; Dekkers, I.A.; Westenberg, J.J.; Schalij, M.J.; Widya, R.L.; de Mutsert, R.; Rosendaal, F.R.; de Roos, A.; Jukema, J.W.; Scholte, A.J.; et al. Normal and reference values for cardio-vascular magnetic resonance-based pulse wave velocity in the middle-aged general population. J. Cardiovasc. Magn. Reson. 2021, 23, 46. [Google Scholar] [CrossRef] [PubMed]
- Baier, D.; Teren, A.; Wirkner, K.; Loeffler, M.; Scholz, M. Parameters of pulse wave velocity: Determinants and reference values assessed in the population-based study LIFE-Adult. Clin. Res. Cardiol. 2018, 107, 1050–1061. [Google Scholar] [CrossRef]
- Chen, C.-C.; Shiu, L.-J.; Li, Y.-L.; Tung, K.-Y.; Chan, K.-Y.; Yeh, C.-J.; Chen, S.-C.; Wong, R.-H. Shift Work and Arteriosclerosis Risk in Professional Bus Drivers. Ann. Epidemiol. 2010, 20, 60–66. [Google Scholar] [CrossRef]
- Jankowiak, S.; Backe, E.; Liebers, F.; Schulz, A.; Hegewald, J.; Garthus-Niegel, S.; Nübling, M.; Blankenberg, S.; Pfeiffer, N.; Lackner, K.J.; et al. Current and cumulative night shift work and subclinical atherosclerosis: Results of the Gutenberg Health Study. Int. Arch. Occup. Environ. Health 2016, 89, 1169–1182. [Google Scholar] [CrossRef]
- Knutsson, A.; Bøggild, H. Shiftwork and Cardiovascular Disease: Review of Disease Mechanisms. Rev. Environ. Health 2000, 15, 359–372. [Google Scholar] [CrossRef] [PubMed]
- Knutsson, A. Health disorders of shift workers. Occup. Med. 2003, 53, 103–108. [Google Scholar] [CrossRef] [Green Version]
- Brown, D.L.; Feskanich, D.; Sánchez, B.N.; Rexrode, K.M.; Schernhammer, E.S.; Lisabeth, L.D. Rotating Night Shift Work and the Risk of Ischemic Stroke. Am. J. Epidemiol. 2009, 169, 1370–1377. [Google Scholar] [CrossRef]
- Aho, V.; Ollila, H.M.; Kronholm, E.; Bondia-Pons, I.; Soininen, P.; Kangas, A.J.; Hilvo, M.; Seppälä, I.; Kettunen, J.; Oikonen, M.; et al. Prolonged sleep restriction induces changes in pathways involved in cholesterol metabolism and inflammatory responses. Sci. Rep. 2016, 6, 24828. [Google Scholar] [CrossRef] [PubMed]
- Aho, V.; Ollila, H.; Rantanen, V.; Kronholm, E.; Surakka, I.; Van Leeuwen, W.M.A.; Lehto, M.; Matikainen, S.; Ripatti, S.; Härmä, M.; et al. Partial Sleep Restriction Activates Immune Response-Related Gene Expression Pathways: Experimental and Epidemiological Studies in Humans. PLoS ONE 2013, 8, e77184. [Google Scholar] [CrossRef] [PubMed]
- McAlpine, C.S.; Kiss, M.G.; Rattik, S.; He, S.; Vassalli, A.; Valet, C.; Anzai, A.; Chan, C.T.; Mindur, J.E.; Kahles, F.; et al. Sleep modulates haematopoiesis and protects against atherosclerosis. Nature 2019, 566, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Zieman, S.J.; Melenovsky, V.; Kass, D.A. Mechanisms, Pathophysiology, and Therapy of Arterial Stiffness. Arter. Thromb. Vasc. Biol. 2005, 25, 932–943. [Google Scholar] [CrossRef]
- Schäfer, C.; Mayr, B.; E Müller, E.; Augner, C.; Hannemann, J.; Böger, R.H.; Schönfelder, M.; Niebauer, J. Exercise training prior to night shift work improves physical work capacity and arterial stiffness. Eur. J. Prev. Cardiol. 2020, 27, 891–893. [Google Scholar] [CrossRef]
- Tenkanen, L.; Sjöblom, T.; Kalimo, R.; Alikoski, T.; Härmä, M. Shift work, occupation and coronary heart disease over 6 years of follow-up in the Helsinki Heart Study. Scand. J. Work Environ. Health 1997, 23, 257–265. [Google Scholar] [CrossRef] [PubMed]
- da Silva e Silva, W.C.; Costa, N.l.L.; Rodrigues, D.d.S.; da Silva, M.L.; Cunha, K.d.C. Sleep quality of adult tobacco users: A systematic review of literature and meta-analysis. Sleep Epidemiol. 2022, 2, 100028. [Google Scholar] [CrossRef]
- Sabanayagam, C.; Shankar, A. The association between active smoking, smokeless tobacco, second-hand smoke exposure and insufficient sleep. Sleep Med. 2010, 12, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Samet, J.; Caffo, B.; Punjabi, N.M. Cigarette Smoking and Nocturnal Sleep Architecture. Am. J. Epidemiol. 2006, 164, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Drager, L.F.; Diegues-Silva, L.; Diniz, P.M.; Lorenzi-Filho, G.; Krieger, E.M.; Bortolotto, L.A. Lack of Circadian Variation of Pulse Wave Velocity Measurements in Healthy Volunteers. J. Clin. Hypertens. 2011, 13, 19–22. [Google Scholar] [CrossRef] [PubMed]

| Dayworkers | Shift Workers | Differences between Shift vs. Dayworkers in 2022 | |||||
|---|---|---|---|---|---|---|---|
| Parameter | No | Mean | No | Mean | Diff. | 95% CI | p-Value |
| Age (years) | 25 | 47.2 | 84 | 39.7 | −7.4 | −12.8, −2.0 | 0.008 |
| Women, (No) | 2 | 6 | |||||
| BMI (kg/m2) | 25 | 27.3 | 84 | 27.3 | −0.09 | −1.5, 1.7 | 0.91 |
| PA (min/week) | 25 | 89.2 | 81 | 107.1 | 17.9 | −29.8, 65.6 | 0.46 |
| Smokers, (No) | 1 | 0.04 | 15 | 0.18 | 0.14 | 0.02, 0.25 | 0.02 |
| Pack-years, (No) | 25 | 9.4 | 84 | 5.5 | −3.9 | −9.3, 1.5 | 0.15 |
| Snuffers, (No) | 6 | 0.24 | 38 | 0.47 | 0.23 | 0.02, 0.44 | 0.03 |
| Years as snuffers | 24 | 3.3 | 81 | 5.8 | 2.5 | −0.6, 5.6 | 0.12 |
| Sleep score, (BIS) | 25 | 8.7 | 82 | 14.4 | 5.7 | 2.4, 8.9 | <0.001 |
| Years in shift, (No) | 25 | 5.8 | 82 | 12.9 | 7.1 | 4.0, 10.2 | <0.001 |
| BP medication | 9 | 0.36 | 9 | 0.11 | −0.25 | −0.46, −0.04 | 0.02 |
| Statin users | 4 | 0.16 | 6 | 0.07 | −0.09 | −0.25, 0.07 | 0.28 |
| sBP (mmHg) | 25 | 137.1 | 84 | 126.0 | 11.1 | 3.5, 18.7 | 0.006 |
| dBP (mmHg) | 25 | 87.8 | 84 | 84.2 | 3.6 | −0.1, 7.3 | 0.06 |
| AP (mmHg) | 25 | 11.4 | 84 | 8.7 | 2.7 | −0.7, 6.1 | 0.12 |
| cPP (mmHg) | 25 | 41.0 | 84 | 37.1 | 3.9 | 0.7, 7.1 | 0.02 |
| cSP (mmHg) | 25 | 117.8 | 84 | 110.8 | 7.0 | 1.4, 12.7 | 0.02 |
| cDP (mmHg) | 25 | 76.9 | 84 | 73.7 | 3.2 | −1.0, 7.3 | 0.13 |
| PWV (m/s) | 24 | 8.6 | 84 | 8.1 | 0.5 | −0.3, 1.4 | 0.22 |
| RHR (beats/min) | 25 | 65.0 | 84 | 70.5 | −5.5 | −9.8, −1.2 | 0.01 |
| Dayworkers | Shift Workers | Shift vs. Dayworkers | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | No Obs | No Persons | Annual Change | Lower | Upper | No Obs | No Persons | Annual Change | Lower | Upper | Diff. Change | Lower Change | Upper Change | p-Value | p-Corr |
| sBP (mmHg) | 86 | 34 | −0.32 | −1.62 | 0.99 | 136 | 51 | 0.10 | −1.00 | 1.20 | 0.41 | −1.33 | 2.16 | 0.64 | 0.82 |
| dBP (mmHg) | 86 | 34 | 0.00 | −0.70 | 0.70 | 136 | 51 | 0.22 | −0.37 | 0.81 | 0.22 | −0.71 | 1.15 | 0.64 | 0.82 |
| AP (mmHg) | 86 | 34 | −0.17 | −0.67 | 0.34 | 137 | 51 | 0.00 | −0.42 | 0.42 | 0.17 | −0.51 | 0.84 | 0.62 | 0.82 |
| cPP (mmHg) | 86 | 34 | −0.14 | −0.78 | 0.50 | 137 | 51 | −0.07 | −0.60 | 0.47 | 0.08 | −0.78 | 0.93 | 0.86 | 0.86 |
| cSP (mmHg) | 86 | 34 | −0.16 | −1.22 | 0.90 | 137 | 51 | 0.12 | −0.77 | 1.00 | 0.28 | −1.14 | 1.69 | 0.70 | 0.82 |
| cDP (mmHg) | 86 | 34 | −0.03 | −0.78 | 0.72 | 137 | 51 | 0.20 | −0.42 | 0.83 | 0.23 | −0.77 | 1.22 | 0.66 | 0.82 |
| PWV (m/s) | 83 | 34 | 0.09 | −0.05 | 0.23 | 135 | 51 | 0.34 | 0.22 | 0.46 | 0.25 | 0.06 | 0.43 | 0.0085 | 0.06 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skogstad, M.; Goffeng, E.; Skare, Ø.; Zardin, E. The Prolonged Effect of Shift Work and the Impact of Reducing the Number of Nightshifts on Arterial Stiffness—A 4-Year Follow-Up Study. J. Cardiovasc. Dev. Dis. 2023, 10, 70. https://doi.org/10.3390/jcdd10020070
Skogstad M, Goffeng E, Skare Ø, Zardin E. The Prolonged Effect of Shift Work and the Impact of Reducing the Number of Nightshifts on Arterial Stiffness—A 4-Year Follow-Up Study. Journal of Cardiovascular Development and Disease. 2023; 10(2):70. https://doi.org/10.3390/jcdd10020070
Chicago/Turabian StyleSkogstad, Marit, Elisabeth Goffeng, Øivind Skare, and Erika Zardin. 2023. "The Prolonged Effect of Shift Work and the Impact of Reducing the Number of Nightshifts on Arterial Stiffness—A 4-Year Follow-Up Study" Journal of Cardiovascular Development and Disease 10, no. 2: 70. https://doi.org/10.3390/jcdd10020070






