Mid-Term Clinical Outcomes and Hemodynamic Performances of Trifecta and Perimount Bioprostheses following Aortic Valve Replacement
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Study Endpoints
2.3. Surgical Details
2.4. Statistical Analysis
3. Results
3.1. Procedural Details
3.2. Hospital Outcome
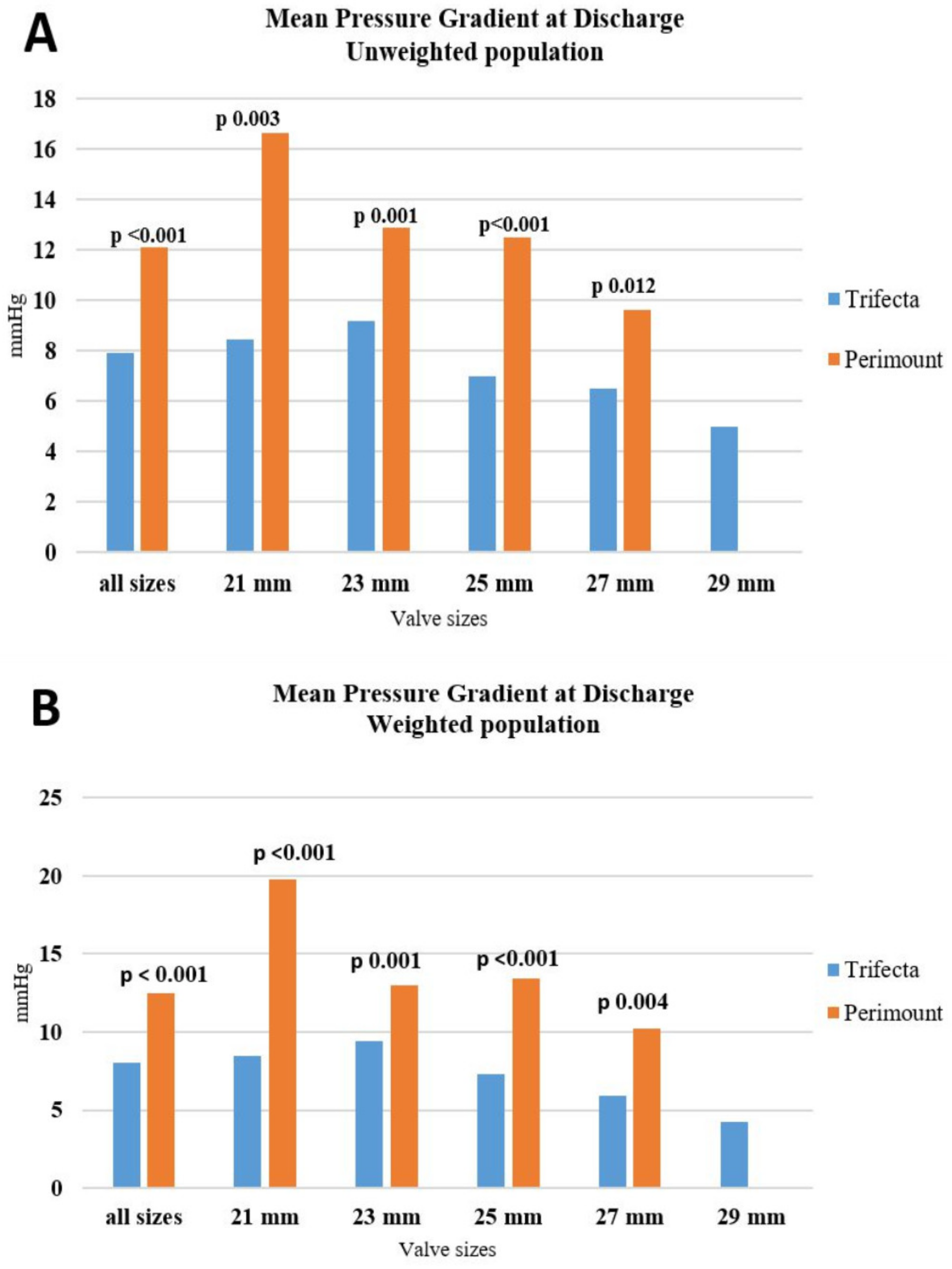
3.3. Echocardiographic Analysis at Discharge
3.4. Follow-Up
3.5. Echocardiographic Analysis at Follow-Up
4. Discussion
- (1)
- The peak and mean gradients across all labelled prosthetic valves were significantly lower in the Trifecta than in the Perimount cohort soon after surgery, a finding that persisted after propensity weighting. In the mid-term follow-up, the superior hemodynamic performance of the Trifecta valve decreased, both in unweighted and weighted groups.
- (2)
- In-hospital and 36-month outcomes did not differ between the two groups.
- (3)
- No patients in either group underwent re-operation for SVD at mid-term follow-up.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Biancari, F.; Valtola, A.; Juvonen, T.; Husso, A.; Dahlbacka, S.; Laakso, T.; Jalava, M.P.; Tauriainen, T.; Ahvenvaara, T.; Kinnunen, E.-M.; et al. Trifecta versus Perimount Magna Ease aortic valve prostheses. Ann. Thorac. Surg. 2020, 110, 879–888. [Google Scholar] [CrossRef]
- Caporali, E.; Bonato, R.; Klersy, C.; Ferrari, E. Hemodynamic performance and clinical outcome of pericardial Perimount Magna and porcine Hancock II valves in aortic position. J. Card. Surg. 2019, 34, 1055–1106. [Google Scholar] [CrossRef]
- Kume, Y.; Fujita, T.; Fukushima, S.; Hata, H.; Shimahara, Y.; Matsumoto, Y.; Yamashita, K.; Kobayashi, J. Reducing prosthesis-patient mismatch with Edwards Magna prosthesis for aortic valve replacement. Circ. J. 2017, 81, 468–475. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fiegl, K.; Deutsch, M.-A.; Rondak, I.-C.; Lange, R.; Guenzinger, R. Matched comparison of two different biological prostheses for complete supra-annular aortic valve replacement. Thorac. Cardiovasc. Surg. 2015, 63, 459–466. [Google Scholar] [PubMed] [Green Version]
- Thorp, S.D.; Khazaal, J.; Yu, G.; Parker, J.L.; Timek, T.A. Magna ease bioprosthetic aortic valve: Mid-term haemodynamic outcomes in 1126 patients. Interact. Cardiovasc. Thorac. Surg. 2021, 32, 839–845. [Google Scholar] [CrossRef]
- Rajab, T.K.; Ali, J.M.; Hernández-Sánchez, J.; Mackie, J.; Grimaudo, V.; Sinichino, S.; Mills, C.; Rana, B.; Dunning, J.; Abu-Omar, Y.; et al. Mid-term follow-up after aortic valve replacement with the Carpentier Edwards Magna Ease prosthesis. J. Cardiothorac. Surg. 2020, 15, 209. [Google Scholar] [CrossRef] [PubMed]
- Bach, D.S.; Patel, H.J.; Kolias, T.J.; Deeb, G.M. Randomized comparison of exercise hemodynamics of Freestyle, Magna Ease and Trifecta bioprostheses after aortic valve replacement for severe aortic stenosis. Eur. J. Cardiothorac. Surg. 2016, 50, 361–367. [Google Scholar] [CrossRef] [Green Version]
- Colli, A.; Marchetto, G.; Salizzoni, S.; Rinaldi, M.; Di Marco, L.; Pacini, D.; Di Bartolomeo, R.; Nicolini, F.; Gherli, T.; Agrifoglio, M.; et al. The TRIBECA study: (TRI) fecta (B)ioprosthesis (E)valuation versus (C)arpentier Magna-Ease in (A)ortic position. Eur. J. Cardiothorac. Surg. 2016, 49, 478–485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yanagawa, B.; Tam, D.Y.; Hong, K.; Mazine, A.; Bagai, A.; Shahbaz, N.K.; Ouzounian, M.; Verma, S. Magna Ease versus Trifecta early hemodynamics: A systematic review and meta-analysis. Innovations 2018, 13, 267–272. [Google Scholar] [CrossRef]
- Maruyama, M.; Daimon, M.; Kawata, T.; Kasai, T.; Ichikawa, R.; Miyazaki, S. Early hemodynamic performance of the trifecta bioprosthetic valve in patients with aortic valve disease. Circ. J. 2014, 78, 1372–1378. [Google Scholar] [CrossRef] [Green Version]
- Yadlapati, A.; Diep, J.; Barnes, M.J.; Grogan, T.; Bethencourt, D.M.; Vorobiof, G. Comprehensive hemodynamic performance and frequency of patient-prosthesis mismatch of the St. Jude Medical Trifecta bioprosthetic aortic valve. J. Heart Valve Dis. 2014, 23, 516–523. [Google Scholar] [PubMed]
- Rubens, F.D.; Gee, Y.-Y.; Ngu, J.M.C.; Chen, L.; Burwash, I.G. Effect of aortic pericardial valve choice on outcomes and left ventricular mass. J. Thorac. Cardiovasc. Surg. 2016, 152, 1291–1298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phan, K.; Ha, H.; Phan, S.; Misfeld, M.; Di Eusanio, M.; Yan, T.D. Early hemodynamic performance of the third generation St Jude Trifecta aortic prosthesis: A systematic review and meta-analysis. J. Thorac. Cardiovasc. Surg. 2015, 149, 1567–1575. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nardi, P.; Pisano, C.; Bertoldo, F.; Vacirca, S.R.; Greci, M.; Bassano, C.; Scafuri, A.; Pellegrino, A.; Ruvolo, G. Clinical outcome and hemodynamic performance of St. Jude Trifecta aortic prosthesis: Short-term follow-up and risk factors analysis. J. Thorac. Dis. 2019, 11, 1465–1474. [Google Scholar] [CrossRef] [PubMed]
- Fukuhara, S.; Shiomi, S.; Yang, B.; Kim, K.; Bolling, S.F.; Haft, J.; Tang, P.; Pagani, F.; Prager, R.L.; Chetcuti, S.; et al. Early structural valve degeneration of trifecta bioprosthesis. Ann. Thorac. Surg. 2020, 109, 720–727. [Google Scholar] [CrossRef]
- Stubeda, H.; Aliter, H.; Gainer, R.A.; Theriault, C.; Doucette, S.; Hirsch, G.M. Six-year follow-up of aortic valve reoperation rates: Carpentier Edwards Perimount versus St. Jude Medical Trifecta. J. Card. Surg. 2020, 35, 3347–3353. [Google Scholar] [CrossRef]
- Yongue, C.; Lopez, D.C.; Soltesz, E.G.; Roselli, E.E.; Bakaeen, F.G.; Gillinov, A.M.; Pettersson, G.B.; Semple, M.E.; Rajeswaran, J.; Tong, M.Z.; et al. Durability and performance of 2298 Trifecta aortic valve prostheses: A propensity-matched analysis. Ann. Thorac. Surg. 2021, 111, 1198–1205. [Google Scholar] [CrossRef]
- Suzuki, R.; Ito, T.; Suzuki, M.; Ohori, S.; Takayanagi, R.; Miura, S. Trifecta versus Perimount Magna Ease aortic valve: Failure mechanisms. Asian Cardiovasc. Thorac. Ann. 2022, 30, 797–806. [Google Scholar] [CrossRef]
- Yokoyama, Y.; Kuno, T.; Takagi, H.; Fukuhara, S. Trifecta versus perimount bioprosthesis for surgical aortic valve replacement; systematic review and meta-analysis. J. Card. Surg. 2021, 36, 4335–4342. [Google Scholar] [CrossRef]
- Lange, R.; Alalawi, Z.; Voss, S.; Boehm, J.; Krane, M.; Vitanova, K. Different rates of bioprosthetic aortic valve failure with Perimount and Trifecta bioprostheses. Front. Cardiovasc. Med. 2022, 8, 822893. [Google Scholar] [CrossRef]
- Baumgartner, H.; Hung, J.; Bermejo, J.; Chambers, J.B.; Edvardsen, T.; Goldstein, S.; Lancellotti, P.; LeFevre, M.; Miller, F., Jr.; Otto, C.M.; et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: A focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. Eur. Heart J. Cardiovasc. Imaging 2017, 18, 254–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Capodanno, D.; Petronio, A.S.; Prendergast, B.; Eltchaninoff, H.; Vahanian, A.; Modine, T.; Lancellotti, P.; Sondergaard, L.; Ludman, P.F.; Tamburino, C.; et al. Standardized definitions of structural deterioration and valve failure in assessing long-term durability of transcatheter and surgical aortic bioprosthetic valves: A consensus statement from the European Association of Percutaneous Cardiovascular Interventions (EAPCI) endorsed by the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2017, 38, 3382–3390. [Google Scholar]
- Dvir, D.; Bourguignon, T.; Otto, C.M.; Hahn, R.T.; Rosenhek, R.; Webb, J.G.; Treede, H.; Sarano, M.E.; Feldman, T.; Wijeysundera, H.C.; et al. Standardized definition of structural valve degeneration for surgical and transcatheter bioprosthetic aortic valves. Circulation 2018, 137, 388–399. [Google Scholar] [CrossRef] [PubMed]
- Généreux, P.; Piazza, N.; Alu, M.C.; Nazif, T.; Hahn, R.; Pibarot, P.; Bax, J.J.; Leipsic, J.A.; Blanke, P.; Blackstone, E.H.; et al. Valve Academic Research Consortium 3: Updated endpoint definitions for aortic valve clinical research. Eur. Heart J. 2021, 42, 1825–1857. [Google Scholar] [CrossRef] [PubMed]
- Heinz, G.; Juni, P. An overview of the objectives of and the approaches to propensity score analyses. Eur. Heart J. 2011, 32, 1704–1708. [Google Scholar] [CrossRef] [Green Version]
- Da Costa, R.; Gahl, B.; Juni, P. Tool & Techniques—Statistics: Propensity score techniques. EuroIntervention 2014, 10, 761–767. [Google Scholar]
- Goldman, S.; Cheung, A.; Bavaria, J.E.; Petracek, M.R.; Groh, M.A.; Schaff, H.V. Midterm, multicenter clinical, and hemodynamic results for the Trifecta aortic pericardial valve. J. Thorac. Cardiovasc. Surg. 2017, 153, 561–569. [Google Scholar] [CrossRef] [Green Version]
- Anselmi, A.; Ruggieri, V.G.; Lelong, B.; Flecher, E.; Corbineau, H.; Langanay, T.; Verhoye, J.-P.; Leguerrier, A. Mid-term durability of the Trifecta bioprosthesis for aortic valve replacement. J. Thorac. Cardiovasc. Surg. 2017, 153, 21–28. [Google Scholar] [CrossRef] [Green Version]
- Kilic, A.; Sultan, I.; Navid, F.; Aranda-Michel, E.; Chu, D.; Thoma, F.; Gleason, T.G. Trifecta Aortic Bioprosthesis: Midterm results in 1953 Patients from a Single Center. Ann. Thorac. Surg. 2019, 107, 1356–1362. [Google Scholar] [CrossRef]
- Tadakoro, N.; Fukushima, S.; Shimahara, Y.; Matsumoto, Y.; Yamashita, K.; Kawamoto, N.; Minami, K.; Kobayashi, J.; Fujita, T. Trifecta vs. magna for aortic valve replacement-differences in clinical outcome and valve hemodynamics. Circ. J. 2018, 82, 2767–2775. [Google Scholar] [CrossRef] [Green Version]


| Unweighted Population (Total 168) | Weighted Population (Total 133) | |||||
|---|---|---|---|---|---|---|
| Trifecta n 86 | Perimount n 82 | p Value | Trifecta n 79 | Perimount n 54 | p Value | |
| Age, (years) * | 70.8 ± 8.6 | 68.8 ± 8.6 | 0.120 | 70.5 ± 8.5 | 69.4 ± 7.5 | 0.931 |
| Male sex * | 63 (73.2) | 68 (82.9) | 0.141 | 57 (72.1) | 43 (79.6) | 0.970 |
| BMI (Kg/m2) * | 26.0 ± 4.2 | 27.6 ± 4.5 | 0.022 | 26.0 ± 4.1 | 27.1 ± 4.4 | 0.826 |
| Hypertension * | 62 (72.1) | 65 (79.3) | 0.288 | 57 (72.1) | 42 (77.8) | 0.989 |
| Hypercholesterolemia | 47 (54.6) | 51 (62.2) | 0.350 | 43 (54.4) | 35 (64.8) | 0.449 |
| Smoking * | 33 (38.4) | 38 (46.3) | 0.349 | 31 (39.2) | 23 (42.6) | 0.635 |
| Diabetes with insulin treatment * | 3 (3.5) | 6 (7.3) | 0.321 | 3 (3.8) | 2 (3.7) | 0.739 |
| Peripheral vascular disease * | 15 (17.4) | 12 (14.6) | 0.678 | 12 (15.2) | 9 (16.7) | 0.997 |
| Chronic lung disease * | 8 (9.3) | 11 (13.4) | 0.469 | 7 (8.8) | 7 (12.9) | 0.943 |
| † Chronic kidney disease * | … | … | 0.180 | … | … | … |
| Severely decreased | 6 (6.9) | 11 (13.4) | … | 6 (7.6) | 8 (14.8) | 0.204 |
| Kidney failure | 1 (1.2) | 0 (0.0) | … | - | - | - |
| NYHA class III-IV * | 26 (30.2) | 28 (34.1) | 0.623 | 24 (30.4) | 18 (33.3) | 0.732 |
| CCS Angina score class 2–3 * | 5 (5.8) | 19 (23.2) | 0.002 | 5 (6.3) | 4 (7.4) | 0.166 |
| Critical state * | 11 (12.8) | 8 (9.7) | 0.629 | 8 (10.1) | 5 (9.3) | 0.709 |
| Active endocarditis * | 7 (8.1) | 3 (3.7) | 0.330 | 5 (6.3) | 2 (3.7) | 0.434 |
| Previous cardiac surgery * | 9 (10.5) | 5 (6.1) | 0.405 | 8 (10.1) | 3 (5.6) | 0.339 |
| Recent myocardial infarction * | 7 (8.1) | 6 (7.3) | 1.000 | 5 (6.3) | 3 (5.6) | 0.622 |
| EuroSCORE-II * | 3 (IQR: 2–8) (Mean: 7 ± 11) | 3 (IQR: 1–6) (Mean: 6 ± 9) | 0.553 | 2 (IQR: 1.7) (Mean: 6 ± 9) | 3 (IQR: 1–5) (Mean: 5 ± 6) | 0.445 |
| Urgent timing * | 14 (16.3) | 11 (13.4) | 0.668 | 10 (12.6) | 7 (12.9) | 0.758 |
| Prevalent aortic valve stenosis * | 60 (69.7) | 56 (68.3) | 0.869 | 58 (73.4) | 39 (72.2) | 0.604 |
| Prevalent aortic valve regurgitation | 34 (39.5) | 37 (45.1) | 0.533 | 30 (37.9) | 24 (44.4) | 0.952 |
| Mean left ventricular ejection fraction (%) * | 53.7 ± 11.9 | 54.5 ± 10.4 | 0.994 | 54.3 ± 11.9 | 54.2 ± 11.1 | 0.780 |
| Mean aortic valve area (cm2) | 0.8 ± 0.3 | 0.9 ± 0.3 | 0.046 | 0.8 ± 0.3 | 0.9 ± 0.4 | 0.792 |
| Mean gradient (mmHg) | 40.4 ± 15.9 | 42.3 ± 20.6 | 0.710 | 41.7 ± 15.2 | 47.9 ± 19.2 | 0.042 |
| Pulmonary hypertension * | 21 (24.4) | 18 (21.9) | 0.719 | 17 (21.5) | 13 (24.1) | 0.923 |
| Unweighted Population (Total 168) | Weighted Population (Total 133) | |||||
|---|---|---|---|---|---|---|
| Trifecta n 86 | Perimount n 82 | p Value | Trifecta n 79 | Perimount n 54 | p Value | |
| Surgical access: | ||||||
| Sternotomy | 55 (63.9) | 55 (67.1) | 0.746 | 49 (62.0) | 33 (61.1) | 0.340 |
| Upper mini sternotomy | 32 (37.2) | 30 (36.6) | 1.000 | 31 (39.2) | 24 (44.4) | 0.143 |
| Conversion to sternotomy | 2 (2.3) | 4 (4.9) | 0.435 | 2 (2.5) | 3 (5.6) | 0.221 |
| Isolated aortic valve replacement | 39 (45.3) | 22 (26.8) | 0.016 | 37 (46.8) | 21 (38.9) | 0.545 |
| Combined procedure: | ||||||
| CABG | 18 (20.9) | 16 (19.5) | 0.850 | 17 (21.5) | 7 (12.9) | 0.313 |
| Ascending aorta replacement * | 6 (6.9) | 9 (10.9) | 0.424 | 6 (7.6) | 6 (11.1) | 0.933 |
| Ascending aorta replacement plus CABG | 1 (1.2) | 3 (3.9) | 0.359 | 1 (1.27) | 1 (1.85) | 0.983 |
| Bentall | 11 (12.8) | 18 (21.9) | 0.153 | 10 (12.6) | 10 (18.5) | 0.944 |
| CABG plus mitral valve repair | 0 (0) | 4 (4.8) | 0.055 | 0 (0) | 2 (3.7) | … |
| Bioprosthesis mean size (mm) | 24.1 ± 2.1 | 24.5 ± 1.9 | 0.102 | 24.0 ± 2.0 | 24.6 ± 1.9 | 0.771 |
| Valve size distribution: * | … | … | 0.050 | … | … | … |
| 19 | 1 (1.2) | 0 (0.0) | … | 1 (1.3) | 0 (0.0) | - |
| 21 | 10 (11.6) | 8 (9.7) | … | 9 (11.4) | 5 (9.3) | 0.664 |
| 23 | 36 (41.8) | 24 (29.3) | … | 34 (43.0) | 16 (29.6) | 0.380 |
| 25 | 23 (26.7) | 30 (36.6) | … | 22 (27.8) | 18 (33.3) | 0.421 |
| 27 | 12 (13.9) | 20 (24.4) | … | 10 (12.7) | 15 (27.8) | … |
| 29 | 4 (4.6) | 0 (0.0) | … | 3 (3.8) | 0 (0.0) | - |
| Aortic annulus enlargement | 9 (10.5) | 2 (2.4) | 0.058 | 9 (11.4) | 1 (1.8) | 0.001 |
| Intraaortic balloon pump | 2 (2.33) | 6 (7.32) | 0.161 | 1 (1.27) | 4 (7.41) | 0.026 |
| Post-procedural ECMO | 1 (1.2) | 3 (3.7) | 0.359 | 1 (1.3) | 1 (1.8) | 0.921 |
| Mean surgical time (min) | 275.2 ± 84.1 | 278.8 ± 96.1 | 0.846 | 272.9 ± 84.9 | 255.7 ± 88.6 | 0.085 |
| Mean cardiopulmonary bypass time (min) | 137.1 ± 57.5 | 141.9 ± 67.6 | 0.962 | 134.2 ± 55.8 | 126.7 ± 62.0 | 0.128 |
| Mean aortic cross-clamp time (min) | 101.0 ± 35.1 | 104.7 ± 45.8 | 0.985 | 95.4 ± 41.3 | 99.3 ± 33.6 | 0.052 |
| Unweighted Population | Weighted Population | |||||
|---|---|---|---|---|---|---|
| Trifecta | Perimount | p Value | Trifecta | Perimount | p Value | |
| 30-day mortality | n 86 3 (3.5) | n 82 7 (8.5) | 0.203 | n 79 2 (2.5) | n 54 4 (7.4) | 0.223 |
| Cause of death: | ||||||
| Multi-organ failure | 2 | 4 | … | … | … | … |
| Heart failure | 0 | 2 | … | … | … | … |
| Haemorrhagic shock (TAAD) | 0 | 1 | … | … | … | … |
| Bowel ischemia | 1 | 0 | … | … | … | … |
| Perioperative myocardial infarction | n 86 2 (2.3) | n 81 2 (2.5) | 1.000 | n 79 1 (1.3) | n 54 1 (1.8) | 0.921 |
| New pacemaker implantation | n 86 1 (1.2) | n 80 2 (2.5) | 0.609 | n 79 1 (1.3) | n 53 1 (1.9) | 0.933 |
| Stroke | n 86 1 (1.2) | n 80 2 (2.5) | 0.609 | n 79 1 (1.3) | n 53 1 (1.9) | 0.531 |
| Reoperation for bleeding | n 86 8 (9.3) | n 80 19 (23.7) | 0.019 | n 79 7 (8.8) | n 53 9 (16.9) | 0.274 |
| † Acute kidney injury | n 86 16 (18.6) | n 80 18 (22.5) | 0.568 | n 79 12 (15.2) | n 53 8 (15.1) | 0.598 |
| Continuous veno-venous hemofiltration | n 86 2 (2.3) | n 80 7 (8.7) | 0.090 | n 79 0 (0) | n 53 3 (5.6) | - |
| Respiratory failure | n 86 8 (9.3) | n 80 10 (12.5) | 0.620 | n 79 5 (6.3) | n 53 5 (9.4) | 0.645 |
| Acute MACCE | n 86 4 (5) | n 82 8 (9) | 0.196 | n 79 4 (5) | n 54 5 (9) | 0.836 |
| Hospital stay (days) | n 86 10.5 (IQR: 8–14) | n 82 8 (IQR: 8–10) | 0.002 | n 79 10 (8–14) | n 54 8 (7–10) | <0.001 |
| Intensive care unit stay (days) | n 86 1 (IQR: 1–2) | n 82 1 (IQR: 1–3) | 0.897 | n 79 1 (IQR: 1–2) | n 54 1 (IQR: 1–2) | 0.415 |
| Unweighted Population | Weighted Population | |||||
|---|---|---|---|---|---|---|
| Trifecta | Perimount | p Value | Trifecta | Perimount | p Value | |
| Mean left ventricular ejection fraction (%) | n 83 52 ± 10.6 | n 76 52.6 ± 11.2 | 0.773 | n 77 52.6 ± 10.6 | n 51 52.0 ± 11.8 | 0.908 |
| Mean aortic valve area (cm2) | n 81 2.3 ± 0.7 | n 67 2.4 ± 0.6 | 0.456 | n 75 2.3 ± 0.6 | n 45 2.4 ± 0.5 | 0.967 |
| Aortic valve area (cm2/m2) | n 81 1.2 ± 0.3 | n 67 1.2 ± 0.3 | 0.826 | n 75 1.2 ± 0.3 | n 45 1.2 ± 0.3 | 0.947 |
| Peak pressure gradient (mmHg): | n 82 15.5 ± 6.0 | n 75 21.9 ± 8.5 | <0.001 | n 76 15.6 ± 6.2 | n 50 22.7 ± 8.5 | <0.001 |
| Size 21 | n 9 16.3 ± 2.9 | n 5 28.8 ± 12.2 | 0.011 | n 9 16.5 ± 2.6 | n 3 34.1 ± 10.9 | 0.001 |
| Size 23 | n 35 18.2 ± 6.8 | n 21 23.6 ± 6.9 | 0.006 | n 33 18.6 ± 6.8 | n 14 23.9 ± 5.8 | 0.007 |
| Size 25 | n 22 13.4 ± 4.9 | n 29 22.5 ± 9.2 | <0.001 | n 21 13.9 ± 5.5 | n 18 24.6 ± 10.3 | <0.001 |
| Size 27 | n 12 12.6 ± 4.0 | n 20 17.5 ± 6.1 | 0.018 | n 10 11.7 ± 4.6 | n 15 18.6 ± 5.5 | 0.003 |
| Size 29 | n 4 9.7 ± 3.1 | - | - | n 3 8.1 ± 1.4 | - | - |
| Mean pressure gradient (mmHg): | n 82 7.9 ± 3.2 | n 75 12.1 ± 4.7 | <0.001 | n 76 8.0 ± 3.3 | n 50 12.4 ± 4.6 | <0.001 |
| Size 21 | n 9 8.4 ± 2.0 | n 5 16.6 ± 6.1 | 0.003 | n 9 8.4 ± 1.9 | n 3 19.7 ± 5.0 | <0.001 |
| Size 23 | n 35 9.2 ± 3.7 | n 21 12.8 ± 4.3 | 0.001 | n 33 9.4 ± 3.7 | n 14 13.1 ± 3.4 | 0.001 |
| Size 25 | n 22 7.0 ± 2.6 | n 29 12.5 ± 4.9 | <0.001 | n 21 7.3 ± 3.0 | n 18 13.3 ± 5.1 | <0.001 |
| Size 27 | n 12 6.5 ± 2.5 | n 20 9.6 ± 3.5 | 0.012 | n 10 6.1 ± 2.8 | n 15 10.1 ± 3.3 | 0.004 |
| Size 29 | n 4 5.0 ± 1.4 | - | - | n 3 4.2 ± 0.5 | - | - |
| Moderate paravalvular leak | n 83 2 (2.4) | n 75 2 (2.7) | 1.000 | n 77 2 (2.6) | n 50 2 (4.0) | 0.646 |
| Patient-prosthesis mismatch: | … | … | 0.437 | … | … | 0.661 |
| Mild | n 81 19 (23.5) | n 67 17 (25.4) | … | n 75 17 (22.7) | n 45 13 (28.9) | … |
| Moderate and severe | n 81 10 (12.3) | n 67 4 (5.9) | … | n 75 10 (13.3) | n 45 2 (4.4) | … |
| Unweighted Population | Weighted Population | |||||
|---|---|---|---|---|---|---|
| Trifecta | Perimount | p Value | Trifecta | Perimount | p Value | |
| Mean aortic valve area (cm2) | n 14 2.1 ± 0.5 | n 8 2.3 ± 0.6 | 0.315 | n 14 2.1 ± 0.5 | n 7 2.4 ± 0.5 | 0.517 |
| Aortic valve area (cm2/m2) | n 5 1.2 ± 0.3 | n 3 0.9 ± 0.1 | 0.166 | n 5 1.2 ± 0.3 | n 2 1.0 ± 0.1 | 0.139 |
| Peak valve gradient (mmHg): | n 80 15.4 ± 7.3 | n 73 16.7 ± 6.1 | 0.238 | n 75 15.5 ± 7.5 | n 49 16.5 ± 5.5 | 0.175 |
| Size 21 | n 9 14.6 ± 5.0 | n 5 19.6 ± 6.1 | 0.120 | n 9 13.6 ± 5.5 | n 3 17.1 ± 2.5 | 0.276 |
| Size 23 | n 35 18.1 ± 9.1 | n 21 16.5 ± 4.7 | 0.477 | n 33 18.0 ± 8.5 | n 14 16.5 ± 5.6 | 0.484 |
| Size 25 | n 21 13.6 ± 5.1 | n 28 17.2 ± 6.6 | 0.043 | n 20 13.5 ± 5.2 | n 18 18.0 ± 6.1 | 0.018 |
| Size 27 | n 11 13.3 ± 4.6 | n 19 15.4 ± 6.7 | 0.354 | n 10 14.0 ± 4.5 | n 14 15.4 ± 5.9 | 0.543 |
| Size 29 | n 4 9.7 ± 2.6 | - | - | n 3 9.1 ± 2.7 | - | - |
| Mean valve gradient (mmHg): | n 80 8.2 ± 3.7 | n 74 8.9 ± 3.6 | 0.224 | n 75 8.2 ± 3.7 | n 49 8.8 ± 3.5 | 0.121 |
| Size 21 | n 9 7.9 ± 2.4 | n 5 10.6 ± 2.9 | 0.088 | n 9 7.5 ± 2.7 | n 3 9.9 ± 2.2 | 0.158 |
| Size 23 | n 35 9.4 ± 4.5 | n 21 8.4 ± 3.2 | 0.376 | n 33 9.4 ± 4.2 | n 14 8.7 ± 3.9 | 0.579 |
| Size 25 | n 21 7.0 ± 2.6 | n 29 9.5 ± 4.0 | 0.017 | n 20 6.9 ± 2.7 | n 18 10.1 ± 3.7 | 0.005 |
| Size 27 | n 11 7.2 ± 2.6 | n 19 7.9 ± 3.4 | 0.528 | n 10 7.6 ± 2.8 | n 14 7.9 ± 3.2 | 0.812 |
| Size 29 | n 4 6.2 ± 2.2 | - | - | n 3 6.1 ± 2.7 | - | - |
| Moderate paravalvular leaks | n 80 1 (1.2) | n 74 1 (1.3) | 1.000 | n 75 1 (1.3) | n 49 1 (2.0) | 1.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toto, F.; Leo, L.; Klersy, C.; Torre, T.; Theologou, T.; Pozzoli, A.; Caporali, E.; Demertzis, S.; Ferrari, E. Mid-Term Clinical Outcomes and Hemodynamic Performances of Trifecta and Perimount Bioprostheses following Aortic Valve Replacement. J. Cardiovasc. Dev. Dis. 2023, 10, 139. https://doi.org/10.3390/jcdd10040139
Toto F, Leo L, Klersy C, Torre T, Theologou T, Pozzoli A, Caporali E, Demertzis S, Ferrari E. Mid-Term Clinical Outcomes and Hemodynamic Performances of Trifecta and Perimount Bioprostheses following Aortic Valve Replacement. Journal of Cardiovascular Development and Disease. 2023; 10(4):139. https://doi.org/10.3390/jcdd10040139
Chicago/Turabian StyleToto, Francesca, Laura Leo, Catherine Klersy, Tiziano Torre, Thomas Theologou, Alberto Pozzoli, Elena Caporali, Stefanos Demertzis, and Enrico Ferrari. 2023. "Mid-Term Clinical Outcomes and Hemodynamic Performances of Trifecta and Perimount Bioprostheses following Aortic Valve Replacement" Journal of Cardiovascular Development and Disease 10, no. 4: 139. https://doi.org/10.3390/jcdd10040139
APA StyleToto, F., Leo, L., Klersy, C., Torre, T., Theologou, T., Pozzoli, A., Caporali, E., Demertzis, S., & Ferrari, E. (2023). Mid-Term Clinical Outcomes and Hemodynamic Performances of Trifecta and Perimount Bioprostheses following Aortic Valve Replacement. Journal of Cardiovascular Development and Disease, 10(4), 139. https://doi.org/10.3390/jcdd10040139








