Inspiratory Muscle and Functional Performance of Patients Entering Cardiac Rehabilitation after Cardiac Valve Replacement
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Inspiratory Muscle and Functional Performance
3.2. Correlation Analyses
4. Discussion
4.1. Effect of Surgical Technique on Inspiratory Muscle and Functional Performance
4.2. Pulmonary and Inspiratory Muscle Impairments in Patients Undergoing Valve Replacement Surgery
4.3. Correlation of Inspiratory Muscle Performance to Functional Performance
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eggebrecht, H.; Mehta, R.H. Transcatheter aortic valve implantation (TAVI) in Germany: More than 100,000 procedures and now the standard of care for the elderly. EuroIntervention 2019, 14, e1549–e1552. [Google Scholar] [CrossRef] [Green Version]
- Phan, K.; Xie, A.; Di Eusanio, M.; Yan, T.D. A meta-analysis of minimally invasive versus conventional sternotomy for aortic valve replacement. Ann. Thorac. Surg. 2014, 98, 1499–1511. [Google Scholar] [CrossRef] [PubMed]
- Lamelas, J. Minimally invasive aortic valve replacement: The “Miami Method”. Ann. Cardiothorac. Surg. 2015, 4, 71–77. [Google Scholar] [PubMed]
- Still, S.; Szerlip, M.; Mack, M. TAVR Vs. SAVR in Intermediate-Risk Patients: What Influences Our Choice of Therapy. Curr. Cardiol. Rep. 2018, 20, 82. [Google Scholar] [CrossRef]
- Arora, S.; Vavalle, J.P. Minimally invasive aortic valve replacement-where are we? J. Thorac. Dis. 2017, 9, E514–E518. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.A.; Rasania, S.P.; Afilalo, J.; Popma, J.J.; Lipsitz, L.A.; Kim, D.H. Functional status and quality of life after transcatheter aortic valve replacement: A systematic review. Ann. Intern. Med. 2014, 160, 243–254. [Google Scholar] [CrossRef] [Green Version]
- Savage, P.D.; Rengo, J.L.; Menzies, K.E.; Ades, P.A. Cardiac Rehabilitation After Heart Valve Surgery: Comparison with Coronary Artery Bypass Graft Patients. J. Cardiopulm. Rehabil. Prev. 2015, 35, 231–237. [Google Scholar] [CrossRef]
- Cargnin, C.; Karsten, M.; Guaragna, J.; Dal Lago, P. Inspiratory Muscle Training After Heart Valve Replacement Surgery Improves Inspiratory Muscle Strength, Lung Function, and Functional Capacity: A Randomized Controlled Trial. J. Cardiopulm. Rehabil. Prev. 2019, 39, E1–E7. [Google Scholar] [CrossRef]
- Saxena, P.; Luthra, S.; Dhaliwal, R.S.; Rana, S.S.; Behera, D. Early changes in pulmonary functions after mitral valve replacement. Ann. Thorac. Med. 2007, 2, 111–117. [Google Scholar]
- American Thoracic Society/European Respiratory Society. ATS/ERS Statement on respiratory muscle testing. Am. J. Respir. Crit. Care Med. 2002, 166, 518–624. [Google Scholar] [CrossRef]
- Cahalin, L.P.; Garcia, C.; Denis, T.S.; Colas-Salgado, S.; Eisenhardt, B.; Formiga, M.F.; Cohen, M. Normative values for the test of incremental respiratory endurance (TIRE). Am. J. Respir. Crit. Care Med. 2016, 193, A6363. [Google Scholar]
- Chen, Y.C.; Chen, K.C.; Lu, L.H.; Wu, Y.L.; Lai, T.J.; Wang, C.H. Validating the 6-minute walk test as an indicator of recovery in patients undergoing cardiac surgery: A prospective cohort study. Medicine 2018, 97, e12925. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys. Ther. 2000, 80, 896–903. [Google Scholar] [PubMed] [Green Version]
- Bohannon, R.W. Reference values for the five-repetition sit-to-stand test: A descriptive meta-analysis of data from elders. Percept Mot. Ski. 2006, 103, 215–222. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Baldwin, M.; Polissar, N.L.; Gruber, W. Predicting the probability for falls in community-dwelling older adults. Phys. Ther. 1997, 77, 812–819. [Google Scholar] [CrossRef] [Green Version]
- Formiga, M.F.; Roach, K.E.; Vital, I.; Urdaneta, G.; Balestrini, K.; Calderon-Candelario, R.A.; Campos, M.A.; Cahalin, L.P. Reliability and validity of the test of incremental respiratory endurance measures of inspiratory muscle performance in COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2018, 15, 1569–1576. [Google Scholar] [CrossRef] [Green Version]
- Cribier, A.; Eltchaninoff, H.; Bash, A.; Borenstein, N.; Tron, C.; Bauer, F.; Derumeaux, G.; Anselme, F.; Laborde, F.; Leon, M.B. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: First human case description. Circulation 2002, 106, 3006–3008. [Google Scholar] [CrossRef]
- Nguyen, T.C.; Terwelp, M.D.; Thourani, V.H.; Zhao, Y.; Ganim, N.; Hoffmann, C.; Justo, M.; Estrera, A.L.; Smalling, R.W.; Balan, P.; et al. Clinical trends in surgical, minimally invasive and transcatheter aortic valve replacement. Eur. J. Cardiothorac. Surg. 2017, 51, 1086–1092. [Google Scholar] [CrossRef] [Green Version]
- Hall, D.E.; Youk, A.; Allsup, K.; Kennedy, K.; Byard, T.D.; Dhupar, R.; Chu, D.; Rahman, A.M.; Wilson, M.; Cahalin, L.P.; et al. Preoperative rehabilitation is feasible in the weeks prior to surgery and significantly improves functional performance. J. Frailty Aging 2022, 1–10. [Google Scholar] [CrossRef]
- Komaki, K.; Yoshida, N.; Satomi-Kobayashi, S.; Tsuboi, Y.; Ogawa, M.; Wakida, K.; Toba, T.; Kawamori, H.; Otake, H.; Omura, A.; et al. Preoperative frailty affects postoperative complications, exercise capacity, and home discharge rates after surgical and transcatheter aortic valve replacement. Heart Vessel. 2021, 36, 1234–1245. [Google Scholar] [CrossRef]
- Ribeiro, G.S.; Melo, R.D.; Deresz, L.F.; Dal Lago, P.; Pontes, M.R.; Karsten, M. Cardiac rehabilitation programme after transcatheter aortic valve implantation versus surgical aortic valve replacement: Systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2017, 24, 688–697. [Google Scholar] [CrossRef] [PubMed]
- Tarro Genta, F.; Tidu, M.; Bouslenko, Z.; Bertolin, F.; Salvetti, I.; Comazzi, F.; Giannuzzi, P. Cardiac rehabilitation after transcatheter aortic valve implantation compared to patients after valve replacement. J. Cardiovasc. Med. 2017, 18, 114–120. [Google Scholar] [CrossRef]
- Pardaens, S.; Moerman, V.; Willems, A.M.; Calders, P.; Bartunek, J.; Vanderheyden, M.; De Sutter, J. Impact of the preoperative risk and the type of surgery on exercise capacity and training after valvular surgery. Am. J. Cardiol. 2014, 113, 1383–1389. [Google Scholar] [CrossRef] [PubMed]
- Russell, K.L.; Holloway, T.M.; Brum, M.; Caruso, V.; Chessez, C.; Grace, S.L. Cardiac rehabilitation wait times: Effect on enrollment. J. Cardiopulm. Rehabil. Prev. 2011, 31, 373–377. [Google Scholar] [CrossRef]
- Adachi, D.; Yamada, M.; Nishiguchi, S.; Fukutani, N.; Hotta, T.; Tashiro, Y.; Morino, S.; Shirooka, H.; Nozaki, Y.; Hirata, H.; et al. Age-related decline in chest wall mobility: A cross-sectional study among community-dwelling elderly women. J. Am. Osteopat. Assoc. 2015, 115, 384–389. [Google Scholar] [CrossRef] [Green Version]
- Dsouza, F.V.; Amaravadi, S.K.; Samuel, S.R.; Raghavan, H.; Ravishankar, N. Effectiveness of Inspiratory Muscle Training on Respiratory Muscle Strength in Patients Undergoing Cardiac Surgeries: A Systematic Review With Meta-Analysis. Ann. Rehabil. Med. 2021, 45, 264–273. [Google Scholar] [CrossRef] [PubMed]
- Westerdahl, E.; Jonsson, M.; Emtner, M. Pulmonary function and health-related quality of life 1-year follow up after cardiac surgery. J. Cardiothorac. Surg. 2016, 11, 99. [Google Scholar] [CrossRef] [Green Version]
- Hegazy, F.A.; Mohamed Kamel, S.M.; Abdelhamid, A.S.; Aboelnasr, E.A.; Elshazly, M.; Hassan, A.M. Effect of postoperative high load long duration inspiratory muscle training on pulmonary function and functional capacity after mitral valve replacement surgery: A randomized controlled trial with follow-up. PLoS ONE 2021, 16, e0256609. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.; Klein, U.; Weigert, A.; Schiller, W.; Bayley-Ezziddin, V.; Wirtz, D.C.; Welz, A.; Werner, N.; Grube, E.; Nickenig, G.; et al. Use of Pre- and Intensified Postprocedural Physiotherapy in Patients with Symptomatic Aortic Stenosis Undergoing Transcatheter Aortic Valve Replacement Study (the 4P-TAVR Study). J. Interv. Cardiol. 2021, 2021, 8894223. [Google Scholar] [CrossRef]
- Ferreira, P.E.; Rodrigues, A.J.; Evora, P.R. Effects of an inspiratory muscle rehabilitation program in the postoperative period of cardiac surgery. Arq. Bras. Cardiol. 2009, 92, 275–282. [Google Scholar]
- Cordeiro, A.L.; de Melo, T.A.; Neves, D.; Luna, J.; Esquivel, M.S.; Guimarães, A.R.; Borges, D.L.; Petto, J. Inspiratory Muscle Training and Functional Capacity in Patients Undergoing Cardiac Surgery. Braz. J. Cardiovasc. Surg. 2016, 31, 140–144. [Google Scholar] [PubMed] [Green Version]
- de Menezes, T.C.; Bassi, D.; Cavalcanti, R.C.; Barros, J.E.S.L.; Granja, K.S.B.; Calles, A.C.D.N.; Exel, A.L. Comparisons and correlations of pain intensity and respiratory and peripheral muscle strength in the pre- and postoperative periods of cardiac surgery. Rev. Bras. Ter. Intensiv. 2018, 30, 479–486. [Google Scholar] [CrossRef] [PubMed]




| Demographic Variable | All Patients (n = 27) | TC-VRS * (n = 12) | MI-VRS ** (n = 8) | MS-VRS *** (n = 7) | p Value | |
|---|---|---|---|---|---|---|
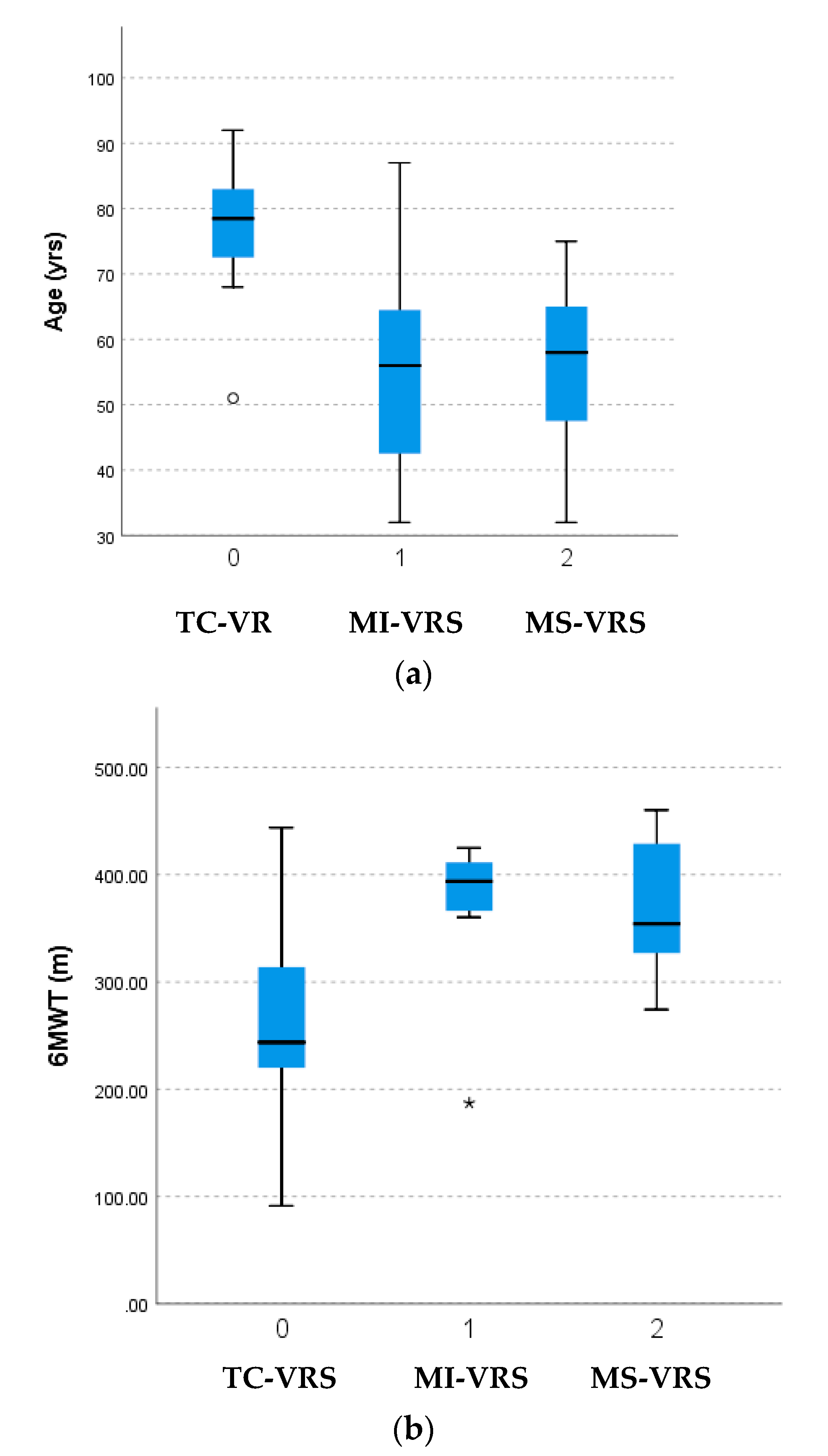
| Age (years) † | 65.0 (17.2) | 76.7 (10.3) | 55.6 (17.4) | 55.7 (15.4) | 0.01 † | |
| Gender (male/female) | 11 (40.7%)/16 (59.3%) | 6 (50.0%)/6 (50.0%) | 2 (22.2%)/7 (77.8%) | 3 (50%)/3 (50%) | 0.397 | |
| Ejection fraction (%) | 48.57 (14.06) | 48.00 (16.02) | 50.00 (11.72) | 48.33 (14.72) | 0.889 | |
| Body mass index (kg/m2) | 28.06 (5.60) | 28.80 (6.77) | 29.03 (3.57) | 25.68 (5.31) | 0.488 | |
| Occupation | Currently working | 10 (40.0%) | 4 (36.3%) | 5 (55.6%) | 1 (20.0%) | 0.622 |
| Unemployed | 3 (12.0%) | 1 (9.1%) | 1 (11.1%) | 1 (20.0%) | ||
| Retired | 11 (44.0%) | 6 (54.5%) | 2 (22.2%) | 3 (60%) | ||
| Disability | 1 (4%) | 0 (0%) | 1 (11.1%) | 0 (0%) | ||
| Race and ethnicity | African American | 4 (14.8%) | 0 (0%) | 3 (33.3%) | 1 (16.7%) | 0.779 |
| Asian | 2 (7.4%) | 2 (16.7%) | 0 (0%) | 0 (0%) | ||
| White | 20 (74.1%) | 9 (81.8%) | 6 (66.7%) | 5 (83.3%) | ||
| Hispanic | 18 (66.7%) | 9 (81.8%) | 5 (55.6%) | 4 (66.6%) | ||
| Education level | High school graduate | 4 (28.6%) | 1 (25.0%) | 2 (28.6%) | 1 (33.3%) | 0.507 |
| 2- or 4-year college | 4 (28.6%) | 1 (25.0%) | 1 (14.3%) | 2 (66.7) | ||
| Post-graduate | 6 (42.9%) | 2 (50.0%) | 4 (57.1%) | 0 (0%) | ||
| Number of comorbidities | 5.74 (3.07) | 7.50 (2.93) | 4.00 (2.13) | 4.71 (2.87) | 0.070 | |
| Days since surgery | 80.29 (79.21) | 70.64 (53.99) | 43.57 (32.59) | 140.83 (123.53) | 0.070 | |
| Length of stay (# days) † | 3.14 (2.00) | 1.91 (1.08) | 4.75 (2.05) | 4.00 (1.41) | 0.006 † | |
| Exercised prior to surgery | 11 (41%) | 6 (50%) | 4 (57.1%) | 1 (17%) | 0.267 | |
| TC-VRS (n = 12) | MI-VRS (n = 8) | MS-VRS (n = 7) | p Values | |
|---|---|---|---|---|
| Maximum inspiratory pressure (cmH2O) (MIP) | 47.92 (18.35) | 57.71 (28.38) | 64.43 (24.34) | 0.400 |
| Sustained maximum inspiratory pressure (PTU) * (SMIP) | 167.83 (67.99) | 256.71 (99.10) | 348.14 (177.52) | 0.017 * |
| Chest wall expansion at xiphoid process (in) (CWE) | 1.14 (0.64) | 2.00 (0.71) | 1.23 (0.80) | 0.324 |
| 6-min walk test (m) * (6MWT) | 258.76 (88.52) | 369.39 (76.65) | 371.44 (70.65) | 0.035 * |
| 5x sit to stand (s) * (5xSTS) | 24.39 (9.03) | 17.97 (3.06) | 13.21 (1.59) | 0.016 * |
| Timed up and go (s) (TUG) | 13.77 (8.22) | 10.29 (1.88) | 8.54 (1.42) | 0.116 |
| Berg balance scale (BBS) | 46.11 (7.81) | 52.00 (4.12) | 52.33 (3.45) | 0.080 |
| Patient health questionnaire-9 (PHQ-9) | 7.88 (7.86) | 6.33 (3.16) | 10.20 (6.22) | 0.427 |
| % Predicted 6MWT | 60.76 (19.27) | 70.90 (9.74) | 65.60 (15.55) | 0.418 |
| % Predicted MIP | 58.77 (20.20) | 66.09 (35.50) | 67.30 (29.41) | 0.759 |
| % Predicted SMIP | 57.44 (29.95) | 61.88 (23.81) | 60.67 (22.57) | 0.262 |
| MIP (cmH2O) | SMIP (PTU) | 6MWT (m) | Berg Balance Scale | TUG (s) | 5x StS (s) | Age (yr) | |
|---|---|---|---|---|---|---|---|
| MIP (cmH2O) | r = 1 | ||||||
| SMIP (PTU) | r = 0.505 p = 0.010 ‡ | r = 1 | |||||
| 6MWT (m) | r = 0.476 p = 0.016 † | r = 0.591 p = 0.002 ‡ | r = 1 | ||||
| Berg Balance Scale | r = 0.472 p = 0.031 † | r = 0.310 p = 0.172 | r = 0.565 p = 0.006 ‡ | r = 1 | |||
| TUG (s) | r = −0.513 p = 0.017 ‡ | r = −0.500 p = 0.021 † | r = −0.761 p < 0.001 ‡ | r = −0.443 p = 0.050 | r = 1 | ||
| 5x StS (s) | r = −0.284 p = 0.212 | r = −0.292 p = 0.199 | r = −0.635 p = 0.001 ‡ | r = −0.439 p = 0.060 | r = 0.716 p = 0.001 ‡ | r = 1 | |
| Age (years) | r = −0.555 p = 0.004 ‡ | r = −0.661 p < 0.001 ‡ | r = −0.688 p < 0.001 ‡ | r = −0.683 p < 0.001 ‡ | r = 0.517 p = 0.014 † | r = 0.402 p = 0.064 | r = 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gempel, S.; Cohen, M.; Milian, E.; Vidret, M.; Smith, A.; Jones, I.; Orozco, Y.; Kirk-Sanchez, N.; Cahalin, L.P. Inspiratory Muscle and Functional Performance of Patients Entering Cardiac Rehabilitation after Cardiac Valve Replacement. J. Cardiovasc. Dev. Dis. 2023, 10, 142. https://doi.org/10.3390/jcdd10040142
Gempel S, Cohen M, Milian E, Vidret M, Smith A, Jones I, Orozco Y, Kirk-Sanchez N, Cahalin LP. Inspiratory Muscle and Functional Performance of Patients Entering Cardiac Rehabilitation after Cardiac Valve Replacement. Journal of Cardiovascular Development and Disease. 2023; 10(4):142. https://doi.org/10.3390/jcdd10040142
Chicago/Turabian StyleGempel, Sabine, Meryl Cohen, Eryn Milian, Melany Vidret, Andrew Smith, Ian Jones, Yessenia Orozco, Neva Kirk-Sanchez, and Lawrence P. Cahalin. 2023. "Inspiratory Muscle and Functional Performance of Patients Entering Cardiac Rehabilitation after Cardiac Valve Replacement" Journal of Cardiovascular Development and Disease 10, no. 4: 142. https://doi.org/10.3390/jcdd10040142
APA StyleGempel, S., Cohen, M., Milian, E., Vidret, M., Smith, A., Jones, I., Orozco, Y., Kirk-Sanchez, N., & Cahalin, L. P. (2023). Inspiratory Muscle and Functional Performance of Patients Entering Cardiac Rehabilitation after Cardiac Valve Replacement. Journal of Cardiovascular Development and Disease, 10(4), 142. https://doi.org/10.3390/jcdd10040142





