Is Conduction System Pacing a Valuable Alternative to Biventricular Pacing for Cardiac Resynchronization Therapy?
Abstract
:1. Introduction
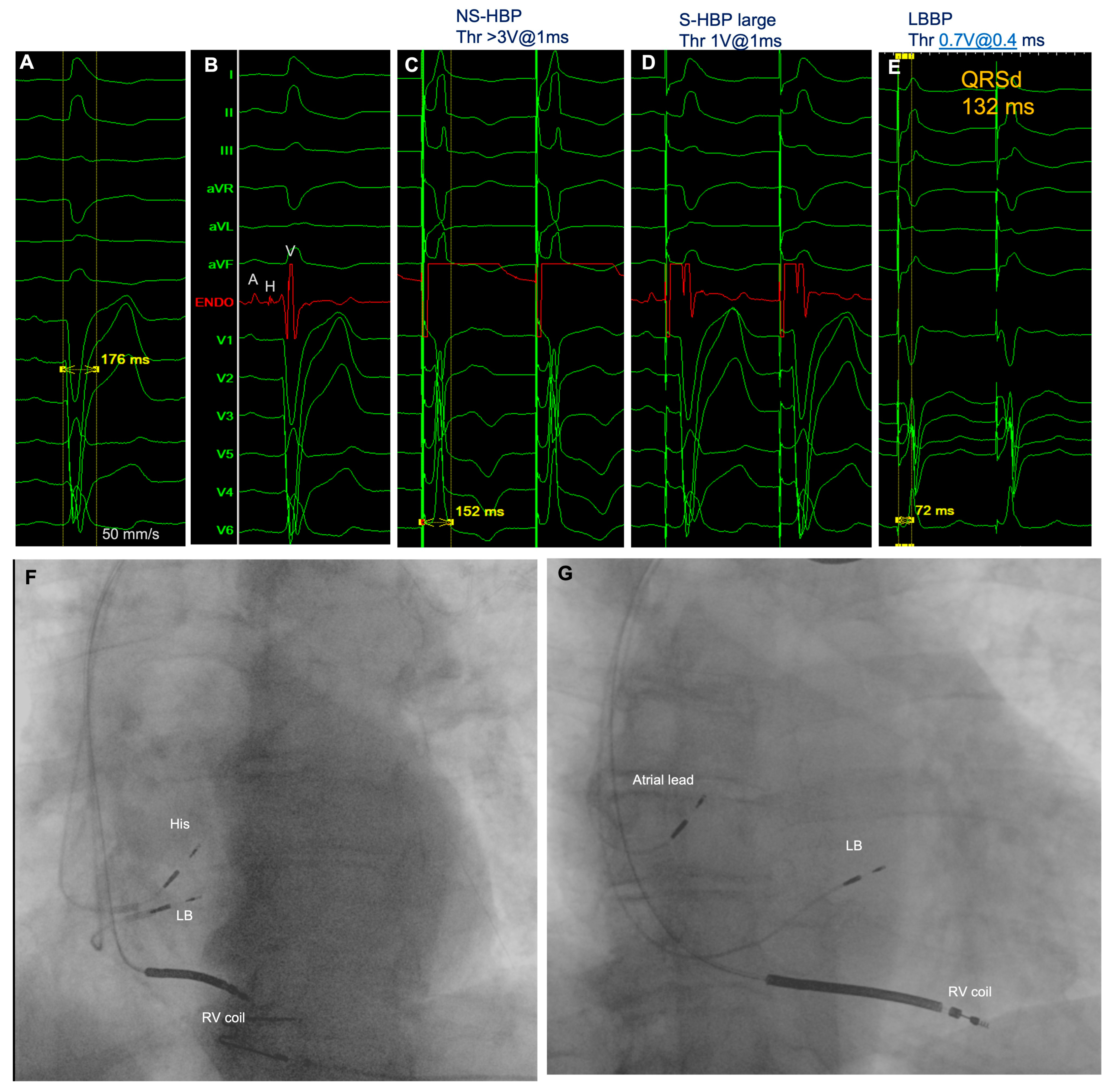
2. The Rationale for Using CSP as CRT Strategy: LBBB Correction
3. Dyssynchrony
4. Hemodynamics
5. CSP to Achieve CRT: Preliminary Experiences
6. Technical Considerations
7. Procedural Success Rate
8. Complications
9. Current Guidelines
10. Relevant Studies and Ongoing Trial
11. Gaps and Unmet Needs
12. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Glikson, M.; Nielsen, J.C.; Kronborg, M.B.; Michowitz, Y.; Auricchio, A.; Barbash, I.M.; Barrabés, J.A.; Boriani, G.; Braunschweig, F.; Brignole, M.; et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur. Heart J. 2021, 42, 3427–3520. [Google Scholar] [CrossRef] [PubMed]
- Chung, M.K.; Patton, K.K.; Lau, C.P.; Dal Forno, A.R.J.; Al-Khatib, S.M.; Arora, V.; Birgersdotter-Green, U.M.; Cha, Y.M.; Chung, E.H.; Cronin, E.M.; et al. 2023 HRS/APHRS/LAHRS guideline on cardiac physiologic pacing for the avoidance and mitigation of heart failure. Heart Rhythm. 2023, 20, e17–e91. [Google Scholar] [CrossRef] [PubMed]
- Keene, D.; Whinnett, Z. Advances in cardiac resynchronization therapy: Review of indications and delivery options. Heart 2022, 108, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Deif, B.; Ballantyne, B.; Almehmadi, F.; Mikhail, M.; McIntyre, W.F.; Manlucu, J.; Yee, R.; Sapp, J.L.; Roberts, J.D.; Healey, J.S.; et al. Cardiac resynchronization is pro-arrhythmic in the absence of reverse ventricular remodelling: A systematic review and meta-analysis. Cardiovasc. Res. 2018, 114, 1435–1444. [Google Scholar] [CrossRef] [PubMed]
- Daubert, C.; Behar, N.; Martins, R.P.; Mabo, P.; Leclercq, C. Avoiding non-responders to cardiac resynchronization therapy: A practical guide. Eur. Heart J. 2017, 38, 1463–1472. [Google Scholar] [CrossRef] [PubMed]
- Kircanski, B.; Boveda, S.; Prinzen, F.; Sorgente, A.; Anic, A.; Conte, G.; Burri, H. Conduction system pacing in everyday clinical practice: EHRA physician survey. Europace. 2023, 25, 682–687. [Google Scholar] [CrossRef]
- Moss, A.J.; Hall, W.J.; Cannom, D.S.; Klein, H.; Brown, M.W.; Daubert, J.P.; Estes, N.A.M.; Foster, E.; Greenberg, E.; Higgins, S.L.; et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N. Engl. J. Med. 2009, 361, 1329–1338. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Zhang, P.; Li, X.; Gao, Y.; Zhu, T.; Wang, L.; Li, D.; Wang, J.; Yuan, C.; Guo, J. True complete left bundle branch block morphology strongly predicts good response to cardiac resynchronization therapy. Europace 2013, 15, 1499–1506. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, I.; Kutyifa, V.; Klein, H.U.; Cannom, D.S.; Brown, M.W.; Dan, A.; Daubert, J.P.; Mark Estes, N.A., 3rd; Foster, E.; Greenberg, H.; et al. Survival with cardiac-resynchronization therapy in mild heart failure. N. Engl. J. Med. 2014, 370, 1694–1701. [Google Scholar] [CrossRef]
- James, T.N.; Sherf, L. Fine structure of the His bundle. Circulation 1971, 44, 9–28. [Google Scholar] [CrossRef]
- El-Sherif, N.; Amay-Y-Leon, F.; Schonfield, C.; Scherlag, B.J.; Rosen, K.; Lazzara, R.; Wyndham, C. Normalization of bundle branch block patterns by distal His bundle pacing. Clinical and experimental evidence of longitudinal dissociation in the pathologic his bundle. Circulation 1978, 57, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Narula, O.S. Longitudinal dissociation in the His bundle. Bundle branch block due to asynchronous conduction within the His bundle in man. Circulation 1977, 56, 996–1006. [Google Scholar] [CrossRef] [PubMed]
- Ginks, M.R.; Shetty, A.K.; Lambiase, P.D.; Duckett, S.G.; Bostock, J.; Peacock, J.L.; Rhode, K.S.; Bucknall, C.; Gill, J.; Taggart, P.; et al. Benefits of endocardial and multisite pacing are dependent on the type of left ventricular electric activation pattern and presence of ischemic heart disease: Insights from electroanatomic mapping. Circ. Arrhythm Electrophysiol. 2012, 5, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, G.A.; Cherian, T.; Shatz, D.Y.; Beaser, A.D.; Aziz, Z.; Ozcan, C.; Broman, M.T.; Nayak, H.M.; Tung, R. Intracardiac Delineation of Septal Conduction in Left Bundle-Branch Block Patterns. Circulation 2019, 139, 1876–1888. [Google Scholar] [CrossRef] [PubMed]
- Jastrzębski, M.; Kukla, P.; Kisiel, R.; Fijorek, K.; Moskal, P.; Czarnecka, D. Comparison of four LBBB definitions for predicting mortality in patients receiving cardiac resynchronization therapy. Ann. Noninvasive Electrocardiol. 2018, 23, e12563. [Google Scholar] [CrossRef] [PubMed]
- Caputo, M.L.; van Stipdonk, A.; Illner, A.; D’Ambrosio, G.; Regoli, F.; Conte, G.; Moccetti, T.; Klersy, C.; Prinzen, F.W.; Vernooy, K.; et al. The definition of left bundle branch block influences the response to cardiac resynchronization therapy. Int. J. Cardiol. 2018, 269, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Arnold, A.D.; Shun-Shin, M.J.; Keene, D.; Howard, J.P.; Sohaib, S.M.A.; Wright, I.J.; Cole, G.D.; Qureshi, N.A.; Lefroy, D.C.; Koa-Wing, M.; et al. His Resynchronization Versus Biventricular Pacing in Patients With Heart Failure and Left Bundle Branch Block. J. Am. Coll. Cardiol. 2018, 72, 3112–3122. [Google Scholar] [CrossRef] [PubMed]
- Baroni, M.; Preda, A.; Varrenti, M.; Vargiu, S.; Carbonaro, M.; Giordano, F.; Gigli, L.; Mazzone, P. Left Bundle Branch Area Pacing over His Bundle Pacing: How Far Have We Come? J. Clin. Med. 2023, 12, 3251. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhu, H.; Hou, X.; Wang, Z.; Zou, F.; Qian, Z.; Wei, Y.; Wang, X.; Zhang, L.; Li, X.; et al. Randomized Trial of Left Bundle Branch vs Biventricular Pacing for Cardiac Resynchronization Therapy. J. Am. Coll. Cardiol. 2022, 80, 1205–1216. [Google Scholar] [CrossRef]
- Padeletti, L.; Pieragnoli, P.; Ricciardi, G.; Innocenti, L.; Checchi, L.; Padeletti, M.; Michelucci, A.; Picariello, F.; Valsecchi, S. Simultaneous His Bundle and Left Ventricular Pacing for Optimal Cardiac Resynchronization Therapy Delivery: Acute Hemodynamic Assessment by Pressure-Volume Loops. Circ. Arrhythm Electrophysiol. 2016, 9, e003793. [Google Scholar] [CrossRef]
- Salden, F.C.W.M.; Luermans, J.G.L.M.; Westra, S.W.; Weijs, B.; Engels, E.B.; Heckman, L.I.B.; Lamerichs, L.J.M.; Janssen, M.H.G.; Clerx, K.J.H.; Cornelussen, R.; et al. Short-Term Hemodynamic and Electrophysiological Effects of Cardiac Resynchronization by Left Ventricular Septal Pacing. J. Am. Coll. Cardiol. 2020, 75, 347–359. [Google Scholar] [CrossRef]
- Zweerink, A.; Zubarev, S.; Bakelants, E.; Potyagaylo, D.; Stettler, C.; Chmelevsky, M.; Lozeron, E.D.; Hachulla, A.L.; Vallée, J.P.; Burri, H. His-Optimized Cardiac Resynchronization Therapy with Ventricular Fusion Pacing for Electrical Resynchronization in Heart Failure. JACC Clin. Electrophysiol. 2021, 7, 881–892. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Wang, J.; Gong, X.; Lu, H.; Yu, Z.; Zhang, L.; Li, M.; Pan, L.; Chen, X.; Cui, J.; et al. Left Bundle Branch Pacing Versus Biventricular Pacing for Acute Cardiac Resynchronization in Patients with Heart Failure. Circ. Arrhythm Electrophysiol. 2022, 15, e011181. [Google Scholar] [CrossRef]
- Pujol-Lopez, M.; Jiménez-Arjona, R.; Garre, P.; Guasch, E.; Borràs, R.; Doltra, A.; Ferró, E.; García-Ribas, C.; Niebla, M.; Carro, E.; et al. Conduction System Pacing vs Biventricular Pacing in Heart Failure and Wide QRS Patients: LEVEL-AT Trial. JACC Clin. Electrophysiol. 2022, 8, 1431–1445. [Google Scholar] [CrossRef] [PubMed]
- Ali, N.; Arnold, A.D.; Miyazawa, A.A.; Keene, D.; Chow, J.J.; Little, I.; Peters, N.S.; Kanagaratnam, P.; Qureshi, N.; Ng, F.S.; et al. Comparison of methods for delivering cardiac resynchronization therapy: An acute electrical and haemodynamic within-patient comparison of left bundle branch area, His bundle, and biventricular pacing. Europace 2023, 25, 1060–1067. [Google Scholar] [CrossRef] [PubMed]
- Deshmukh, P.; Casavant, D.A.; Romanyshyn, M.; Anderson, K. Permanent, direct His-bundle pacing: A novel approach to cardiac pacing in patients with normal His-Purkinje activation. Circulation 2000, 101, 869–877. [Google Scholar] [CrossRef]
- Barba-Pichardo, R.; Manovel Sanchez, A.; Fernandez-Gomez, J.M.; Morina-Vazquez, P.; Venegas-Gamero, J.; Herrera-Carranza, M. Ventricular resynchronization therapy by direct His-bundle pacing using an internal cardioverter defibrillator. Europace 2013, 15, 83–88. [Google Scholar] [CrossRef]
- Lustgarten, D.L.; Crespo, E.M.; Arkhipova-Jenkins, I.; Lobel, R.; Winget, J.; Koehler, J.; Liberman, E.; Sheldon, T. His-bundle pacing versus biventricular pacing in cardiac resynchronization therapy patients: A crossover design comparison. Heart Rhythm 2015, 12, 1548–1557. [Google Scholar] [CrossRef] [PubMed]
- Manovel, A.; Barba-Pichardo, R.; Tobaruela, A. Electrical and mechanical cardiac resynchronisation by novel direct his-bundle pacing in a heart failure patient. Heart Lung Circ. 2011, 20, 769–772. [Google Scholar] [CrossRef]
- Ponnusamy, S.S.; Ramalingam, V.; Mariappan, S.; Ganesan, V.; Anand, V.; Syed, T.; Murugan, S.; Kumar, M.; Vijayaraman, P. Left bundle branch pacing lead for sensing ventricular arrhythmias in implantable cardioverter-defibrillator: A pilot study (LBBP-ICD study). Heart Rhythm 2023, 21, 419–426. [Google Scholar] [CrossRef]
- Shresthaa, D.B.; Baniya, A.; Lamichhane, S.; Shahi, M.; Shtembari, J.; Deshmukhc, A.J.; Voruganti, D.; Patel, N.K.; Sangal, K.; Vallabhajosyulaf, S.; et al. Conduction system pacing vs. biventricular pacing for cardiac resynchronization therapy in heart failure with reduced ejection fraction: An updated systematic review and meta-analysis. Health Sci. Rev. 2023, 8, 100104. [Google Scholar] [CrossRef]
- Clementy, N.; Bodin, A.; Ah-Fat, V.; Babuty, D.; Bisson, A. Dual-chamber ICD for left bundle branch area pacing: The cardiac resynchronization and arrhythmia sensing via the left bundle (cross-left) pilot study. J. Interv. Card. Electrophysiol. 2023, 66, 905–912. [Google Scholar] [CrossRef] [PubMed]
- Mahajan, A.; Pokharel, P.; Vijayaraman, P. Lead-to-lead interaction leading to left bundle branch area pacing lead failure. Heart Rhythm Case Rep. 2022, 9, 72–75. [Google Scholar] [CrossRef]
- Pokharel, P.; Mahajan, A.; Himes, A.; Lowell, M.; Budde, R.; Vijayaraman, P. Mechanisms of damage related to ICD and pacemaker lead interaction. Heat Rhythm. O2 2023, 4, 820–822. [Google Scholar] [CrossRef] [PubMed]
- Francois, C.; De Becker, B.; De Smet, M.; Knecht, S.; Duytschaever, M.; Tavernier, R.; le Polain de, W. Interaction between left bundle branch area pacing and defibrillator lead: A case report. Heart Rhythm Case Rep. 2023, 10, 72–75. [Google Scholar] [CrossRef]
- Upadhyay, G.A.; Vijayaraman, P.; Nayak, H.M.; Verma, N.; Dandamudi, G.; Sharma, P.S.; Saleem, M.; Mandrola, J.; Genovese, D.; Tung, R.; et al. His Corrective Pacing or Biventricular Pacing for Cardiac Resynchronization in Heart Failure. J. Am. Coll. Cardiol. 2019, 74, 157–159. [Google Scholar] [CrossRef]
- Huybrechts, W.L.H.; Bergonti, M.; Saenen, J.B.; Miljoen, H.; Van Leuven, O.; Van Assche, L.; Van Herck, P.; Wittock, A.; De Cleen, D.; Sarkozy, A.; et al. Left Bundle Branch Area Defibrillator (LBBAD): A First-in-Human Feasibility Study. JACC Clin. Electrophysiol. 2023, 9, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Vinther, M.; Risum, N.; Svendsen, J.H.; Møgelvang, R.; Philbert, B.T. A Randomized Trial of His Pacing Versus Biventricular Pacing in Symptomatic HF Patients With Left Bundle Branch Block (His-Alternative). JACC Clin. Electrophysiol. 2021, 7, 1422–1432. [Google Scholar] [CrossRef]
- Jastrzębski, M.; Kiełbasa, G.; Cano, O.; Curila, K.; Heckman, L.; De Pooter, J.; Chovanec, M.; Rademakers, L.; Huybrechts, W.; Grieco, D.; et al. Left bundle branch area pacing outcomes: The multicentre European MELOS study. Eur. Heart J. 2022, 43, 4161–4173. [Google Scholar] [CrossRef]
- Ponnusamy, S.S.; Murugan, M.; Ganesan, V.; Vijayaraman, P. Predictors of procedural failure of left bundle branch pacing in scarred left ventricle. J. Cardiovasc. Electrophysiol. 2023, 34, 760–764. [Google Scholar] [CrossRef]
- Kim, J.A.; Kim, S.E.; Ellenbogen, K.A.; Vijayaraman, P.; Chelu, M.G. Clinical outcomes of conduction system pacing versus biventricular pacing for cardiac resynchronization therapy: A systematic review and meta-analysis. J. Cardiovasc. Electrophysiol. 2023, 34, 1718–1729. [Google Scholar] [CrossRef] [PubMed]
- Parlavecchio, A.; Vetta, G.; Caminiti, R.; Coluccia, G.; Magnocavallo, M.; Ajello, M.; Pistelli, L.; Dattilo, G.; Foti, R.; Carerj, S.; et al. Left bundle branch pacing versus biventricular pacing for cardiac resynchronization therapy: A systematic review and meta-analysis. Pacing Clin. Electrophysiol. 2023, 46, 432–439. [Google Scholar] [CrossRef] [PubMed]
- Beer, D.; Subzposh, F.A.; Colburn, S.; Naperkowski, A.; Vijayaraman, P. His bundle pacing capture threshold stability during long-term follow-up and correlation with lead slack. Europace 2021, 23, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Özpak, E.; Van Heuverswyn, F.; Timmermans, F.; De Pooter, J. Lead performance of stylet-driven leads in left bundle branch area pacing: Results from a large single-center cohort and insights from in vitro bench testing. Heart Rhythm. 2024. [Google Scholar] [CrossRef] [PubMed]
- Rangaswamy, V.V.; Ponnusamy, S.S. Late distal conductor fracture of the lumenless pacing lead after left bundle branch area pacing. Heart Rhythm. 2024, 21, 490–491. [Google Scholar] [CrossRef] [PubMed]
- Gui, Y.; Ye, L.; Wu, L.; Mai, H.; Yan, Q.; Wang, L. Clinical Outcomes Associated With His-Purkinje System Pacing vs. Biventricular Pacing, in Cardiac Resynchronization Therapy: A Meta-Analysis. Front. Cardiovasc. Med. 2022, 9, 707148. [Google Scholar] [CrossRef] [PubMed]
- Gin, J.; Chow, C.L.; Voskoboinik, A.; Nalliah, C.; Wong, C.; Van Gaal, W.; Farouque, O.; Mohamed, U.; Lim, H.S.; Kalman, J.M.; et al. Improved outcomes of conduction system pacing in heart failure with reduced ejection fraction: A systematic review and meta-analysis. Heart Rhythm. 2023, 20, 1178–1187. [Google Scholar] [CrossRef] [PubMed]
- Whinnett, Z.I.; Shun-Shin, M.J.; Tanner, M.; Foley, P.; Chandrasekaran, B.; Moore, P.; Adhya, S.; Qureshi, N.; Muthumala, A.; Lane, R.; et al. Effects of haemodynamically atrio-ventricular optimized His bundle pacing on heart failure symptoms and exercise capacity: The His Optimized Pacing Evaluated for Heart Failure (HOPE-HF) randomized, double-blind, cross-over trial. Eur. J. Heart Fail. 2023, 25, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Vijayaraman, P.; Pokharel, P.; Subzposh, F.A.; Oren, J.W.; Storm, R.H.; Batul, S.A.; Beer, D.A.; Hughes, G.; Leri, G.; Manganiello, M.; et al. His-Purkinje Conduction System Pacing Optimized Trial of Cardiac Resynchronization Therapy vs Biventricular Pacing: HOT-CRT Clinical Trial. JACC-EP 2023, 9, 2628–2638. [Google Scholar]
- Brugada, J.; Katritsis, D.G.; Arbelo, E.; Arribas, F.; Bax, J.J.; Blomström-Lundqvist, C.; Calkins, H.; Corrado, D.; Deftereos, S.G.; Diller, G.P.; et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur. Heart J. 2020, 41, 655–720. [Google Scholar] [CrossRef]
- Burri, H.; Jastrzebski, M.; Cano, O.; Kurila, C.; de Pooter, J.; Huang, W.; Israel, C.; Joza, J.; Romer, J.; Vernooy, K.; et al. EHRA clinical consensus statement on conduction system pacing implantation: Endorsed by the Asia Pacific Heart Rhythm Society (APHRS), Canadian Heart Rhythm Society (CHRS), and Latin American Heart Rhythm Society (LAHRS). Europace 2023, 25, 1208–1236. [Google Scholar] [CrossRef] [PubMed]
- Marcantoni, L.; Pastore, G.; Biffi, M.; Zanon, F. The weakest point of cardiac resynchronization therapy: New technologies facing old terminology. Front. Cardiovasc. Med. 2023, 10, 1236369. [Google Scholar] [CrossRef] [PubMed]


| Nct Number | Study Title | Location | Status | Study Design | Primary Outcomes | Number of Patients | Follow-up |
|---|---|---|---|---|---|---|---|
| NCT06278844 | Exercise Capacity Improvement by Conduction System Pacing in heArt Failure patieNts Without Compelling CRT inDication (ESCPAND) | Belgium | Recruiting | Interventional Randomized Parallel assignment Open label | Exercise capacity (change in VO2 peak from baseline to 24 weeks) | 75 | 24 weeks |
| NCT04409119 | Direct HIS/LBB Pacing as an Alternative to Biventricular Pacing in Patients with HFrEF and a Typical LBBB (HIS-alt_2) | Denmark | Recruiting | Randomized Parallel assignment Double masking (participant, outcome assessor) | Change in Left ventricular end-systolic volume (decrease in left ventricular systolic volume of ≥15% of baseline) Success rate of implanting a HIS-bundle lead with capture of the left bundle branch or a LBB-lead with narrowing of QRS | 125 | 6 months |
| NCT05650658 | Left vs. Left Randomized Clinical Trial | USA | Recruiting | Randomized Parallel assignment Triple masking (participant, care provider, outcome assessor) | Combined clinical endpoint of all-cause mortality and hospitalization for heart failure | 2136 | 5.5 years |
| NCT06105580 | Conduction System Pacing vs. Biventricular Pacing in Systolic Dysfunction and Wide QRS: Mortality, Heart Failure Hospitalization or Cardiac Transplant (CONSYST-CRT II) | Spain | Recruiting | Interventional Randomized Parallel assignment Single masking (participant) | All-cause mortality, cardiac transplant, or heart failure hospitalization | 320 | 12 months |
| NCT06241651 | CSP Versus BiVP for Heart Failure Patients With RVP Upgraded to Cardiac Resynchronization Therapy: a Prospective Multicenter Non-inferiority Randomized Controlled Study (CSP-UPGRADE) | China | Recruiting | Interventional Randomized Parallel assignment Open label | ΔLVEF (change in LVEF from baseline) | 66 | 6 months |
| NCT05467163 | Conduction System Pacing Versus Biventricular Pacing After Atrioventricular Node Ablation (CONDUCT-AF trial) | Austria, Bulgaria, Belgium, Croatia | Recruiting | Interventional Randomized Parallel assignment Open label | Change in left ventricular ejection fraction | 82 | 6 months |
| NCT05428787 | Resynchronization in Patients With HF in AF Trial Undergoing Pace & AVNA Strategy With LBBAP Compared With BiV Pacing (RAFT-P&A) | Canada | Recruiting | Randomized Parallel assignment Masking double (participant, outcome assessor) | Change in NT-proBNP from baseline | 284 | 6 months |
| NCT05434962 | The Left Bundle Cardiac Resynchronization Therapy Trial (LEFT-BUNDLE-CRT) | Spain | Recruiting | Randomized Parallel assignment Open label Non-inferiority. | CRT response (improvement of a clinical composite score or ≥15% reduction in left ventricular end-systolic volume) | 176 | 6 months |
| NCT06052475 | Physiological Versus Right Ventricular Outcome Trial Evaluated for Bradycardia Treatment Upgrades (PROTECT-UP) | UK | Recruiting | Randomized Crossover assignment Masking quadruple (participant, care provider, investigator, outcome assessor) | SF-36 physical component summary | 155 | 14 months |
| NCT05265520 | His-Bundle Corrective Pacing in Heart Failure (HIS-CRT) | USA | Recruiting | Randomized Parallel assignment Single masking (outcome assessor) | Change in left ventricular ejection fraction in heart failure patients with Right bundle branch block (RBBB) | 120 | 6 months |
| NCT05572957 | LBBP as Initial Therapy in Patients With Non-ischemic Heart Failure and LBBB (LIT-HF) | China | Recruiting | Randomized Parallel assignment Open label | Proportion of patients requiring ICD implantation for prevention of sudden cardiac death after treatment with two strategies (GDMT, LBBP + GDMT), the percentages of LVEF still ≤35% and/or ventricular arrhythmia events was assessed in both groups. | 50 | 6 months |
| NCT05814263 | HIS Alternative II—UK Site | UK | Recruiting | Randomized Parallel assignment Double masking (participant, outcome assessor) | Change in left ventricular end-systolic volume (decrease in left ventricular systolic volume of ≥ 15% of baseline) Success rate of implanting a HIS-bundle lead with capture of the left bundle branch or a LBB-lead with narrowing of QRS The success rate of implanting a pacing lead to the HIS-bundle, with capture of the left bundle at a threshold < 2.5 V at 1 ms or implantation of a LBB lead with narrowing of the QRS duration and maintaining this effect at 6 month follow-up | 40 | 6 months |
| NCT03803995 | Mapping and Pacing of the His Bundle for Heart Failure Patients With Left Bundle Branch Block (MAP HIS HF) | USA | Recruiting | Single group assignment Open label | Successful HB pacing sites Collect 3D Locations and electrogram characteristics (morphology and activation time) at the sites where His bundle (HB) pacing is associated with left bundle recruitment and corrects electrical dyssynchrony at HB pacing implant procedure. | 30 | N/A |
| NCT05769036 | Conventional Biventricular Versus Left Bundle Branch Pacing on Outcomes in Heart Failure Patients (RECOVER-HF) | Russia | Recruiting | Randomized Parallel assignment Open label | All-cause mortality or worsening of heart failure requiring unplanned hospitalization (%) | 60 | 24 months |
| NCT05187611 | Conduction System Pacing vs. Biventricular Resynchronization Therapy in Systolic Dysfunction and Wide QRS: CONSYST-CRT. | Spain | Active, not recruiting | non-inferiority trial Randomized Parallel assignment Single masking (participant) | Composite endpoint consisting of all-cause mortality, cardiac transplant, heart failure hospitalizations, and left ventricular ejection fraction (LVEF) improvement <5 points | 130 | 1 year |
| NCT05572736 | Conduction System Pacing Versus Biventricular Resynchronization in Patients With Chronic Heart Failure (PhysioSync-HF) | Brazil | Active, not recruiting | Interventional Randomized Parallel assignment Masking Double (participant, outcomes assessor) | Non-inferiority of clinical benefit, a hierarchical composite of all-cause death, any hospitalization for heart failure, any urgent heart failure visit, and left ventricular ejection fraction change at 12 months. | 179 | 12 months |
| NCT05155865 | Conduction System Pacing Versus Biventricular Pacing for Cardiac resynchronization (CSP-SYNC) | Slovenia | Active, not recruiting | Interventional Randomized Parallel assignment Open label | Change in left ventricular volume, left ventricular ejection fraction, difference in heart failure class, proBNP value, 6-min walk test distance, EQ-5D index score | 62 | 12 months |
| NCT05760924 | Left Bundle Branch Pacing on Outcomes and Ventricular Remodeling in Biventricular CRT Nonresponders (RESCUE) | Russia | Not yet recruiting | Randomized Parallel assignment Open label | All-cause mortality or worsening of heart failure requiring unplanned hospitalization (%) | 30 | 24 months |
| NCT06207383 | Atrial Fibrillation Ablation Versus Atrioventricular Nodal Ablation With Conduction System Pacing in Heart Failure (ABACUS trial) | Geneve | Not yet recruiting | Interventional Randomized Parallel assignment Masking single (outcome assessor) | Superiority endpoint: incidence of mortality and cardiovascular hospitalization in each arm Non-inferiority endpoint: incidence of mortality and heart failure hospitalization in each arm | 220 | 1–4 years |
| NCT06342492 | Conduction System Vs Surgical Left Ventricular Epicardial Pacing For Coronary Sinus Lead Failure (KCHRRF_CS Lead Failure_0025) | USA | Not yet recruiting | Observational Cohort Retrospective | Need for lead revision between conduction system pacing (CSP) and transthoracic left ventricular (LV) epicardial pacing approach | 100 | N/A |
| NCT05793502 | Left Bundle Branch Pacing (LBBP) for the Treatment of Cardiac Dysfunction With Safety and Efficacy Study in Patients With Atrioventricular Block | China | Not yet recruiting | Prospective Case-control | Change in LVEF | 160 | 12 months |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castagno, D.; Zanon, F.; Pastore, G.; De Ferrari, G.M.; Marcantoni, L. Is Conduction System Pacing a Valuable Alternative to Biventricular Pacing for Cardiac Resynchronization Therapy? J. Cardiovasc. Dev. Dis. 2024, 11, 144. https://doi.org/10.3390/jcdd11050144
Castagno D, Zanon F, Pastore G, De Ferrari GM, Marcantoni L. Is Conduction System Pacing a Valuable Alternative to Biventricular Pacing for Cardiac Resynchronization Therapy? Journal of Cardiovascular Development and Disease. 2024; 11(5):144. https://doi.org/10.3390/jcdd11050144
Chicago/Turabian StyleCastagno, Davide, Francesco Zanon, Gianni Pastore, Gaetano Maria De Ferrari, and Lina Marcantoni. 2024. "Is Conduction System Pacing a Valuable Alternative to Biventricular Pacing for Cardiac Resynchronization Therapy?" Journal of Cardiovascular Development and Disease 11, no. 5: 144. https://doi.org/10.3390/jcdd11050144
APA StyleCastagno, D., Zanon, F., Pastore, G., De Ferrari, G. M., & Marcantoni, L. (2024). Is Conduction System Pacing a Valuable Alternative to Biventricular Pacing for Cardiac Resynchronization Therapy? Journal of Cardiovascular Development and Disease, 11(5), 144. https://doi.org/10.3390/jcdd11050144





