Multimodality Imaging of the Anatomy of the Aortic Root
Abstract
:1. Introduction
2. Aortic Root
3. Terminology
3.1. The Function of the Aortic Root
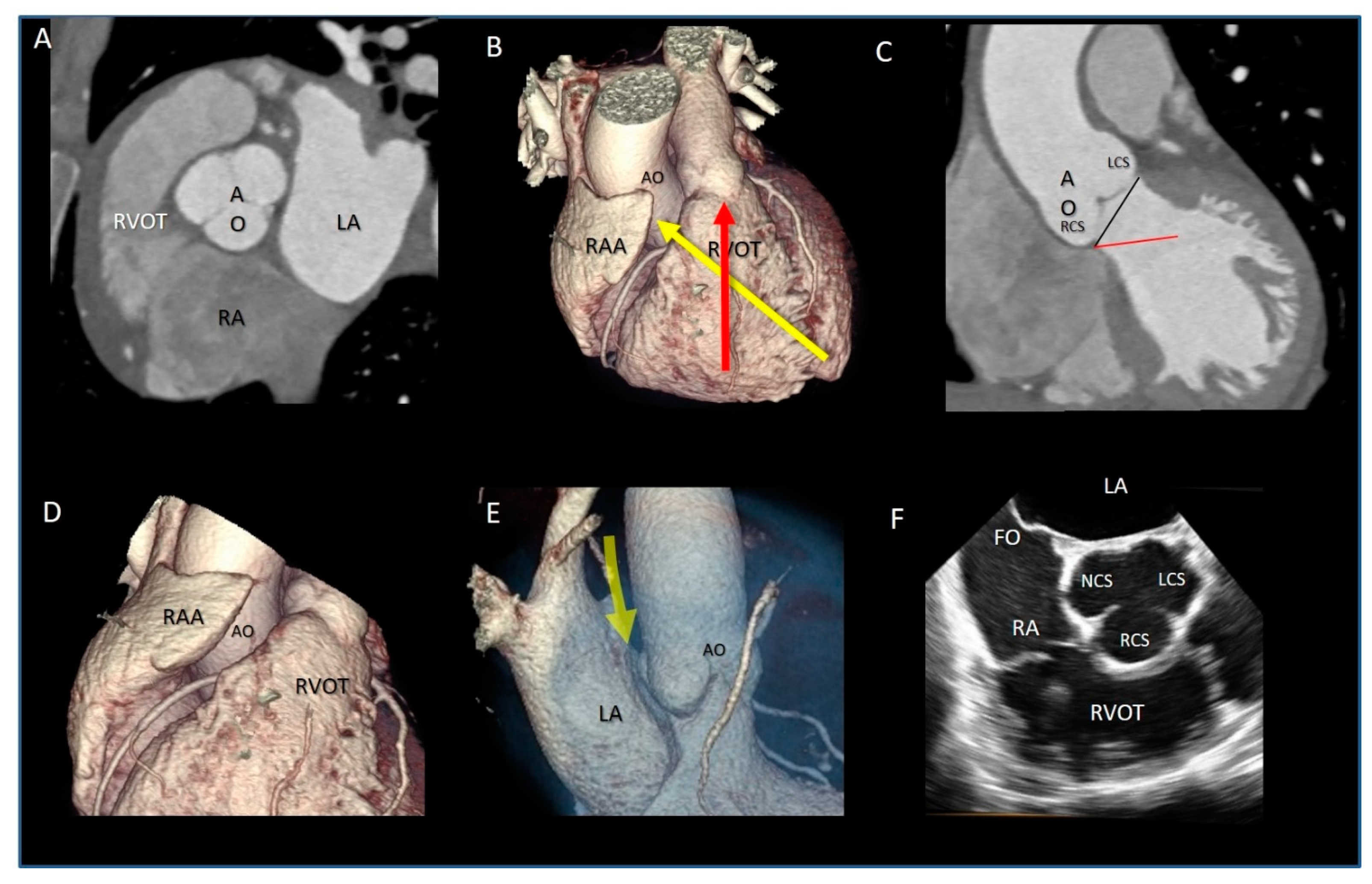
3.2. Aortic Root and Surrounding Structures
3.3. The Components of the Aortic Root
3.3.1. The Ventricular–Arterial Junction (VAJ)
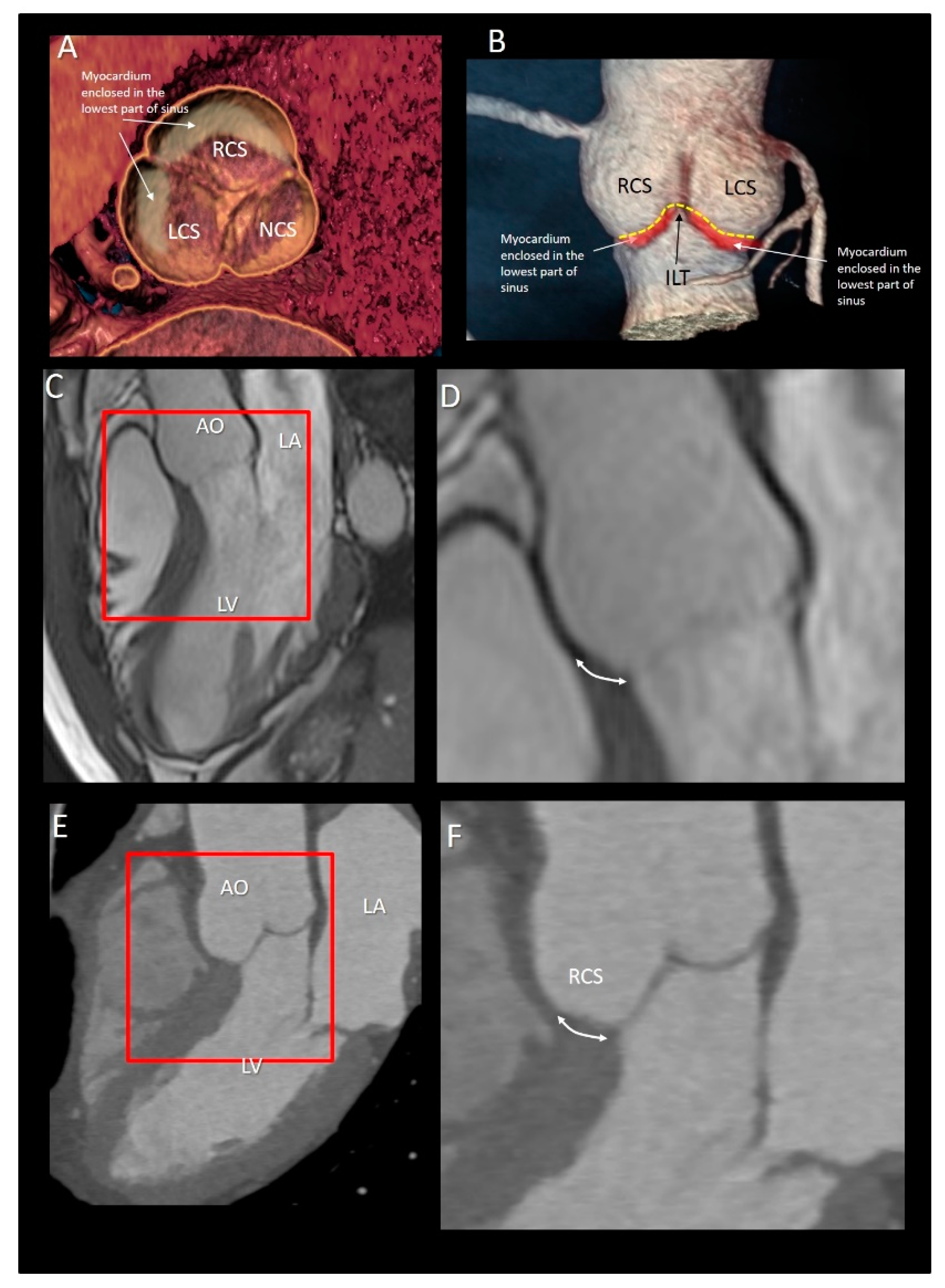
3.3.2. The Muscular Component of VAJ
3.4. The Fibrous Component of VAJ
3.5. The Aortic Annulus
3.6. The Interleaflets Triangles
3.7. The Sinuses of Valsalva
3.8. Leaflets
3.9. The Sinutubular Junction
3.10. The Coronary Ostia
4. Conclusions
Funding
Conflicts of Interest
References
- Faletra, F.F.; Leo, L.A.; Paiocchi, V.L.; Caretta, A.; Viani, G.M.; Schlossbauer, S.A.; Demertzis, S.; Ho, S.Y. Anatomy of Mitral Annulus Insights from Non-Invasive Imaging Techniques. Eur. Heart J. Cardiovasc. Imaging 2019, 20, 843–857. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faletra, F.F.; Leo, L.A.; Paiocchi, V.; Schlossbauer, S.; Narula, J.; Ho, S.Y. Multimodality Imaging Anatomy of Interatrial Septum and Mitral Annulus. Heart 2020. [Google Scholar] [CrossRef]
- Leo, L.A.; Paiocchi, V.L.; Schlossbauer, S.A.; Gherbesi, E.; Faletra, F.F. Anatomy of Mitral Valve Complex as Revealed by Non-Invasive Imaging: Pathological, Surgical and Interventional Implications. J. Cardiovasc. Dev. Dis. 2020, 7, 49. [Google Scholar] [CrossRef]
- Faletra, F.F.; Leo, L.A.; Paiocchi, V.L.; Schlossbauer, S.A.; Pedrazzini, G.; Moccetti, T.; Ho, S.Y. Revisiting Anatomy of the Interatrial Septum and its Adjoining Atrioventricular Junction Using Noninvasive Imaging Techniques. J. Am. Soc. Echocardiogr. 2019, 32, 580–592. [Google Scholar] [CrossRef]
- Saremi, F.; Hassani, C.; Sánchez-Quintana, D. Septal Atrioventricular Junction Region: Comprehensive Imaging in Adults. Radiography 2016, 36, 1966–1986. [Google Scholar] [CrossRef]
- Yasunaga, D.; Hamon, M. MDCT of Interatrial Septum. Diagn. Interv. Imaging 2015, 96, 891–899. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hassani, C.; Saremi, F. Comprehensive Cross-sectional Imaging of the Pulmonary Veins. Radiography 2017, 37, 1928–1954. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Quintana, D.; López-Mínguez, J.R.; Macías, Y.; Cabrera, J.A.; Saremi, S. Left Atrial Anatomy relevant to Catheter Ablation. Cardiol. Res. Pract. 2014, 2014, 289720. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Quintana, D.; Doblado-Calatrava, M.; Cabrera, J.A.; Macías, Y.; Saremi, F. Anatomical Basis for the Cardiac Interventional Electrophysiologist. Biomed. Res. Int. 2015, 2015, 547364. [Google Scholar] [CrossRef] [PubMed]
- David, T.E.; Feindel, C.M. An Aortic Valve-Sparing Operation for Patients with Aortic Incompetence and Aneurysm of the Ascending Aorta. J. Thorac. Cardiovasc. Surg. 1992, 103, 617–621. [Google Scholar] [CrossRef]
- Cribier, A.; Eltchaninoff, H.; Bash, A.; Borenstein, N.; Tron, C.; Bauer, F.; Derumeaux, G.; Anselme, F.; Laborde, F.; Leon, M.B. Percutaneous Transcatheter Implantation of an Aortic Valve Prosthesis for Calcific Aortic Stenosis: First Human Case Description. Circulation 2002, 106, 3006–3008. [Google Scholar] [CrossRef] [PubMed]
- Mori, S.; Tretter, J.T.; Spicer, D.E.; Bolender, D.L.; Anderson, R.H. What Is the Real Cardiac Anatomy? Clin. Anat. 2019, 32, 288–309. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mori, S.; Izawa, Y.; Shimoyama, S.; Tretter, J.T. Three-Dimensional Understanding of Complexity of the Aortic Root Anatomy as the Basis of Routine Two-Dimensional Echocardiographic Measurements. Circ. J. 2019, 83, 2320–2323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ho, S.Y. Structure and Anatomy of the Aortic Root. Eur. J. Echocardiogr. 2009, 10, i3–i10. [Google Scholar]
- Anderson, R.H. Clinical Anatomy of the Aortic Root. Heart 2000, 84, 670–675. [Google Scholar] [PubMed] [Green Version]
- Koshkelashvili, N.; Jalife Bucay, M.; Goykhman, I. Pressman GS. Aortic root and Valve Proportions: An Example of the Golden Ratio? Monaldi Arch. Chest. Dis. 2019, 89. [Google Scholar] [CrossRef]
- O’Brien, B.; Zafar, H.; De Freitas, S.; Sharif, F. Transseptal Puncture—Review of Anatomy, Techniques, Complications and Challenges. Int. J. Cardiol. 2017, 233, 12–22. [Google Scholar] [PubMed]
- Hasdemir, C.; Aktas, S.; Govsa, F.; Aktas, E.O.; Kocak, A.; Bozkaya, Y.T.; Demirbas, M.I.; Ulucan, C.; Ozdogan, O.; Kayikcioglu, M.; et al. Demonstration of Ventricular Myocardial Extensions into the Pulmonary Artery and Aorta Beyond the Ventriculo-Arterial Junction. Pacing. Clin. Electrophysiol. 2007, 30, 534–539. [Google Scholar] [CrossRef]
- Ho, S.Y.; Cabrera, J.A.; Tran, V.H.; Farré, J.; Anderson, R.H.; Sánchez-Quintana, D. Architecture of the Pulmonary Veins: Relevance to Radiofrequency Ablation. Heart 2001, 86, 265–270. [Google Scholar] [CrossRef] [Green Version]
- Yamada, T.; Litovsky, S.H.; Kay, G.N. The Left Ventricular Ostium: An Anatomic Concept Relevant to Idiopathic Ventricular Arrhythmias. Circ. Arrhythm. Electrophysiol. 2008, 1, 396–404. [Google Scholar] [CrossRef] [Green Version]
- Hlivák, P.; Peichl, P.; Cihák, R.; Wichterle, D.; Kautzner, J. Catheter Ablation of Idiopathic Ventricular Tachycardia Originating from Myocardial Extensions into a Noncoronary Aortic Cusp. J. Cardiovasc. Electrophysiol. 2012, 23, 98–101. [Google Scholar] [CrossRef]
- Gard, J.J.; Asirvatham, S.J. Outflow Tract Ventricular Tachycardia. Tex. Heart. Inst. J. 2012, 39, 526–5288. [Google Scholar] [PubMed]
- Asirvatham, S.J. Correlative Anatomy for the Invasive Electrophysiologist: Outflow Tract and Supravalvar Arrhythmia. J. Cardiovasc. Electrophysiol. 2009, 20, 955–968. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.; Dagum, P.; Miller, D.C. Aortic Root Dynamics and Surgery: From Craft to Science. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 2007, 362, 1407–1419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brecker, S.J.; Jin, X.Y.; Yacoub, M.H. Anatomical Definition of Aortic Root Abscesses by Transesophageal Echocardiography: Planning a Surgical Strategy Using Homograft Valves. Clin. Cardiol. 1995, 18, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Oh, H.K.; Kim, N.Y.; Kang, M.W.; Kang, S.K.; Yu, J.H.; Lim, S.P.; Choi, J.S.; Na, M.H. Aortic Periannular Abscess Invading into the Central Fibrous Body, Mitral Valve, and Tricuspid Valve. Korean J. Thorac. Cardiovasc. Surg. 2014, 47, 283–286. [Google Scholar] [CrossRef] [Green Version]
- Parish, L.M.; Liu, L.; Woo, Y.J. Endocarditis with Massive Aortic Root Abscess and Atrioventricular Septal Destruction. Interact. Cardiovasc. Thorac. Surg. 2009, 8, 280–282. [Google Scholar] [CrossRef] [PubMed]
- Vipparthy, S.C.; Ravi, V.; Avula, S.; Kambhatla, S.; Mahmood, M.; Kabour, A.; Ali, S.S.; Barzallo, M.; Mungee, S. Meta-Analysis of Transcatheter Aortic Valve Implantation Versus Surgical Aortic Valve Replacement in Patients with Low Surgical Risk. Am. J. Cardiol. 2020, 125, 459–468. [Google Scholar] [CrossRef]
- Kawashima, T.; Sato, F. Visualizing Anatomical Evidences on Atrioventricular Conduction System for TAVI. Int. J. Cardiol. 2014, 174, 1–6. [Google Scholar] [CrossRef]
- Jilaihawi, H.; Zhao, Z.; Du, R.; Staniloae, C.; Saric, M.; Neuburger, P.J.; Querijero, M.; Vainrib, A.; Hisamoto, K.; Ibrahim, H.; et al. Minimizing Permanent Pacemaker Following Repositionable Self-Expanding Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2019, 12, 1796–1807. [Google Scholar] [CrossRef]
- Kappetein, A.P.; Head, S.J.; Généreux, P.; Piazza, N.; van Mieghem, N.M.; Blackstone, E.H.; Brott, T.G.; Cohen, D.J.; Cutlip, D.E.; van Es, G.A.; et al. Updated Standardized Endpoint Definitions for Transcatheter Aortic Valve Implantation: The Valve Academic Research Consortium-2 Consensus Document. J. Am. Coll. Cardiol. 2012, 60, 1438–1454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pontone, G.; Andreini, D.; Bartorelli, A.L.; Bertella, E.; Cortinovis, S.; Mushtaq, S.; Annoni, A.; Formenti, A.; Baggiano, A.; Conte, E.; et al. Aortic Annulus Area Assessment by Multidetector Computed Tomography for Predicting Paravalvular Regurgitation in Patients Undergoing Balloon-Expandable Transcatheter Aortic Valve Implantation: A Comparison with Transthoracic and Transesophageal Echocardiography. Am. Heart. J. 2012, 164, 576–584. [Google Scholar]
- Tamborini, G.; Fusini, L.; Muratori, M.; Cefalù, C.; Gripari, P.; Ali, S.G.; Pontone, G.; Andreini, D.; Bartorelli, A.L.; Alamanni, F.; et al. Feasibility and Accuracy of Three-Dimensional Transthoracic Echocardiography vs. Multidetector Computed Tomography in the Evaluation of Aortic Valve Annulus in Patient Candidates to Transcatheter Aortic Valve Implantation. Eur. Heart J. Cardiovasc. Imaging. 2014, 15, 1316–1323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.H.; Kim, H.J.; Kim, J.B.; Jung, S.H.; Choo, S.J.; Chung, C.H.; Lee, J.W. Supra-Annular Versus Intra-Annular Prostheses in Aortic Valve Replacement: Impact on Haemodynamics and Clinical Outcomes. Interact. Cardiovasc. Thorac. Surg. 2019, 28, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Suchá, D.; Tuncay, V.; Prakken, N.H.; Leiner, T.; van Ooijen, P.M.; Oudkerk, M.; Budde, R.P. Does the Aortic Annulus Undergo Conformational Change Throughout the Cardiac Cycle? A Systematic Review. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 1307–1317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sutton, J.P.; Ho, S.Y.; Anderson, R.H. The Forgotten Interleaflet Triangles: A Review of Surgical Anatomy of the Aortic Valve. Ann. Thorac. Surg. 1995, 59, 419–427. [Google Scholar] [CrossRef]
- Sá, M.P.B.O.; Zhigalov, K.; Cavalcanti, L.R.P.; Escorel Neto, A.C.; Rayol, S.C.; Weymann, A.; Ruhparwar, A.; Lima, R.C. Impact of Aortic Annulus Enlargement on the Outcomes of Aortic Valve Replacement: A Meta-Analysis. Semin. Thorac. Cardiovasc. Surg. 2020. [Google Scholar] [CrossRef] [PubMed]
- Katayama, S.; Umetani, N.; Sugiura, S.; Hisada, T. The Sinus of Valsalva Relieves Abnormal Stress on Aortic Valve Leaflets by Facilitating Smooth Closure. J. Thorac. Cardiovasc. Surg. 2008, 136, 1528–1535.e1. [Google Scholar] [CrossRef] [Green Version]
- Pisani, G.; Scaffa, R.; Ieropoli, O.; Dell’Amico, E.M.; Maselli, D.; Morbiducci, U.; De Paulis, R. Role of the Sinuses of Valsalva on the Opening of the Aortic Valve. J. Thorac. Cardiovasc. Surg. 2013, 145, 999–1003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Robicsek, F.; Thubrikar, M.J.; Fokin, A.A. Cause of Degenerative Disease of the Trileaflet Aortic Valve: Review of Subject and Presentation of a New Theory. Ann. Thorac. Surg. 2002, 73, 1346–1354. [Google Scholar] [CrossRef]
- Underwood, M.J.; El Khoury, G.; Deronck, D.; Glineur, D.; Dion, R. The Aortic Root: Structure, Function, and Surgical Reconstruction. Heart 2000, 83, 376–380. [Google Scholar] [CrossRef]
- Thubrikar, M.J.; Nolan, S.P.; Aouad, J.; Deck, J.D. Stress Sharing between the Sinus and Leaflets of Canine Aortic Valve. Ann. Thorac. Surg. 1986, 42, 434–440. [Google Scholar] [CrossRef]
- Tzemos, N.; Therrien, J.; Yip, J.; Thanassoulis, G.; Tremblay, S.; Jamorski, M.T.; Webb, G.D.; Siu, S.C. Outcomes in Adults with Bicuspid Aortic Valves. JAMA 2008, 300, 1317–1325. [Google Scholar] [CrossRef] [Green Version]
- Ammannaya, G.K.K. Lambl’s Excrescences: Current Diagnosis and Management. Cardiol. Res. 2019, 10, 207–210. [Google Scholar] [CrossRef] [Green Version]
- Nighoghossian, N.; Trouillas, P.; Perinetti, M.; Barthelet, M.; Ninet, J.; Loire, R. Excroissance de Lambl: Une Cause Inhabituelle D’embolie Cérébrale [Lambl’s Excrescence: An Uncommon Cause of Cerebral Embolism]. Rev. Neurol. 1995, 51, 583–585. [Google Scholar]
- Roldan, C.A.; Shively, B.K.; Crawford, M.H. Valve excrescences: Prevalence, Evolution and Risk for Cardioembolism. J. Am. Coll. Cardiol. 1997, 30, 1308–1314. [Google Scholar] [CrossRef] [Green Version]
- Kalavakunta, J.K.; Peddi, P.; Bantu, V.; Tokala, H.; Kodenchery, M. Lambl’s Excrescences: A Rare Cause of Stroke. J. Heart Valve. Dis. 2010, 19, 669–670. [Google Scholar] [PubMed]
- Schoen, F.J. Evolving Concepts of Cardiac Valve Dynamics: The Continuum of Development, Functional Structure, Pathobiology, and Tissue Engineering. Circulation 2008, 118, 1864–1880. [Google Scholar] [CrossRef] [PubMed]
- Muriago, M.; Sheppard, M.N.; Ho, S.Y.; Anderson, R.H. Location of the Coronary Arterial Orifices in The Normal Heart. Clin. Anat. 1997, 10, 297–302. [Google Scholar] [CrossRef]
- Mariani, S.; Peek, G.J. Coronary Reimplantation in Aortic Root Surgery: The Trapdoor Technique for Adults. Ann. Thorac. Surg. 2015, 99, 1833–1834. [Google Scholar] [CrossRef]
- Tatsuishi, W.; Nakano, K.L.; Kubota, S.; Asano, R.; Kataoka, G. Identification of Coronary Artery Orifice to Prevent Coronary Complications in Bioprosthetic and Transcatheter Aortic Valve Replacement. Circ. J. 2015, 79, 2157–2161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khatri, P.J.; Webb, J.G.; Rodés-Cabau, J.; Fremes, S.E.; Ruel, M.; Lau, K.; Guo, H.; Wijeysundera, H.C.; Ko, D.T. Adverse Effects Associated with Transcatheter Aortic Valve Implantation: A Meta-Analysis of Contemporary Studies. Ann. Intern. Med. 2013, 158, 35–46. [Google Scholar] [CrossRef]
- Dvir, D.; Webb, J.; Brecker, S.; Bleiziffer, S.; Hildick-Smith, D.; Colombo, A.; Descoutures, F.; Hengstenberg, C.; Moat, N.E.; Bekeredjian, R.; et al. Transcatheter Aortic Valve Replacement for Degenerative Bioprosthetic Surgical Valves: Results from the Global Valve-In-Valve Registry. Circulation 2012, 126, 2335–2344. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, H.B.; Webb, J.G.; Makkar, R.R.; Cohen, M.G.; Kapadia, S.R.; Kodali, S.; Tamburino, C.; Barbanti, M.; Chakravarty, T.; Jilaihawi, H.; et al. Predictive Factors, Management, and Clinical Outcomes of Coronary Obstruction Following Transcatheter Aortic Valve Implantation: Insights from a Large Multicenter Registry. J. Am. Coll. Cardiol. 2013, 62, 1552–1562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tops, L.F.; Wood, D.A.; Delgado, V.; Schuijf, J.D.; Mayo, J.R.; Pasupati, S.; Lamers, F.P.; van der Wall, E.E.; Schalij, M.J.; Webb, J.G.; et al. Noninvasive Evaluation of the Aortic Root with Multislice Computed Tomography Implications for Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Imaging 2008, 1, 321–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tamborini, G.; Fusini, L.; Gripari, P.; Muratori, M.; Cefalù, C.; Maffessanti, F.; Alamanni, F.; Bartorelli, A.; Pontone, G.; Andreini, D.; et al. Feasibility and Accuracy of 3DTEE Versus CT for the Evaluation of Aortic Valve Annulus to Left Main Ostium Distance before Transcatheter Aortic Valve Implantation. JACC Cardiovasc. Imaging 2012, 5, 579–588. [Google Scholar] [CrossRef] [PubMed] [Green Version]








| Name | Meaning | |
|---|---|---|
| Ventricular–arterial junction | The term ventricular–arterial junction describes the border between the ventricular myocardium and the fibroelastic structure of the aortic root. Contrary to the right AV junction, where the pulmonary root is entirely supported by the muscular infundibulum, only the left and the right coronary sinuses are partially supported by the myocardium (see text), being the remaining extent of the aortic root supported by fibrous tissue (MS = membranous septum; see text and references [12,13]). |  |
| Cusps, leaflets | The term “cusps” refers to the moving parts of the aortic root. When seen in closed position from the ventricular perspective, this component is similar to the surface of a molar tooth (called cusp). The term is used to describe the structure of the valve (i.e., unicuspidal, bicuspid, and tri-cuspid). Literally the term indicates a pointed end where two curves meet. In the aortic root, it indicates an intact interleaflet triangle with its apex reaching the sinutubular junction. The term leaflet means “small leaf”, which describes a thin, pliable layer. This term perfectly fits the leaflet aspect. N = non-coronary, L = left coronary, R = right coronary leaflets/cusps. |  |
| Commissures | In the anatomy of the aortic root this term refers to the most distal area where the insertions of the leaflets on the aortic wall join each other. |  |
| Aortic annulus | The aortic annulus is the three-dimensional line that follows the hinge line of the leaflets on the aortic wall. This line of dense connective tissue has a crown-shaped appearance (white dotted line). |  |
| Virtual or “echocardiographic” annulus | This term refers to a circumference that joins the lowest points of the leaflet insertion. Although neither anatomically or histologically recognizable, this term has become relevant in the TAVI era. Measurements of this virtual basal plane are used for the sizing of the valve in tricuspid valves. This virtual annuls does not have an anatomic counterpart. |  |
| Surgical annulus | Surgeons fix the prosthetic valves on a circular area lying between the nadirs of the sinuses and midway to the commissures (the aortic prostheses have a flat sewing ring). The term “surgical annulus” refers to this “ring area” and provides a precise reference point when the prosthesis is sutured on “supra” annular position. |  |
| Functions of Aortic Root |
|---|
| Allowing the transit of a significant amount of blood with a minimum gradient between the left ventricle and the aorta |
| nsuring a wide flow variation (up to 5 times) |
| Preventing significant back flow, having, at the same time, a robust structural integrity to withstand the aortic pressure |
| Enabling an optimal coronary perfusion |
| Preserving leaflet integrity |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Paiocchi, V.L.; Faletra, F.F.; Ferrari, E.; Schlossbauer, S.A.; Leo, L.A.; Maisano, F. Multimodality Imaging of the Anatomy of the Aortic Root. J. Cardiovasc. Dev. Dis. 2021, 8, 51. https://doi.org/10.3390/jcdd8050051
Paiocchi VL, Faletra FF, Ferrari E, Schlossbauer SA, Leo LA, Maisano F. Multimodality Imaging of the Anatomy of the Aortic Root. Journal of Cardiovascular Development and Disease. 2021; 8(5):51. https://doi.org/10.3390/jcdd8050051
Chicago/Turabian StylePaiocchi, Vera Lucia, Francesco F. Faletra, Enrico Ferrari, Susanne Anna Schlossbauer, Laura Anna Leo, and Francesco Maisano. 2021. "Multimodality Imaging of the Anatomy of the Aortic Root" Journal of Cardiovascular Development and Disease 8, no. 5: 51. https://doi.org/10.3390/jcdd8050051
APA StylePaiocchi, V. L., Faletra, F. F., Ferrari, E., Schlossbauer, S. A., Leo, L. A., & Maisano, F. (2021). Multimodality Imaging of the Anatomy of the Aortic Root. Journal of Cardiovascular Development and Disease, 8(5), 51. https://doi.org/10.3390/jcdd8050051







