Athlete’s Heart in Elite Biathlon, Nordic Cross—Country and Ski-Mountaineering Athletes: Cardiac Adaptions Determined Using Echocardiographic Data
Abstract
1. Introduction
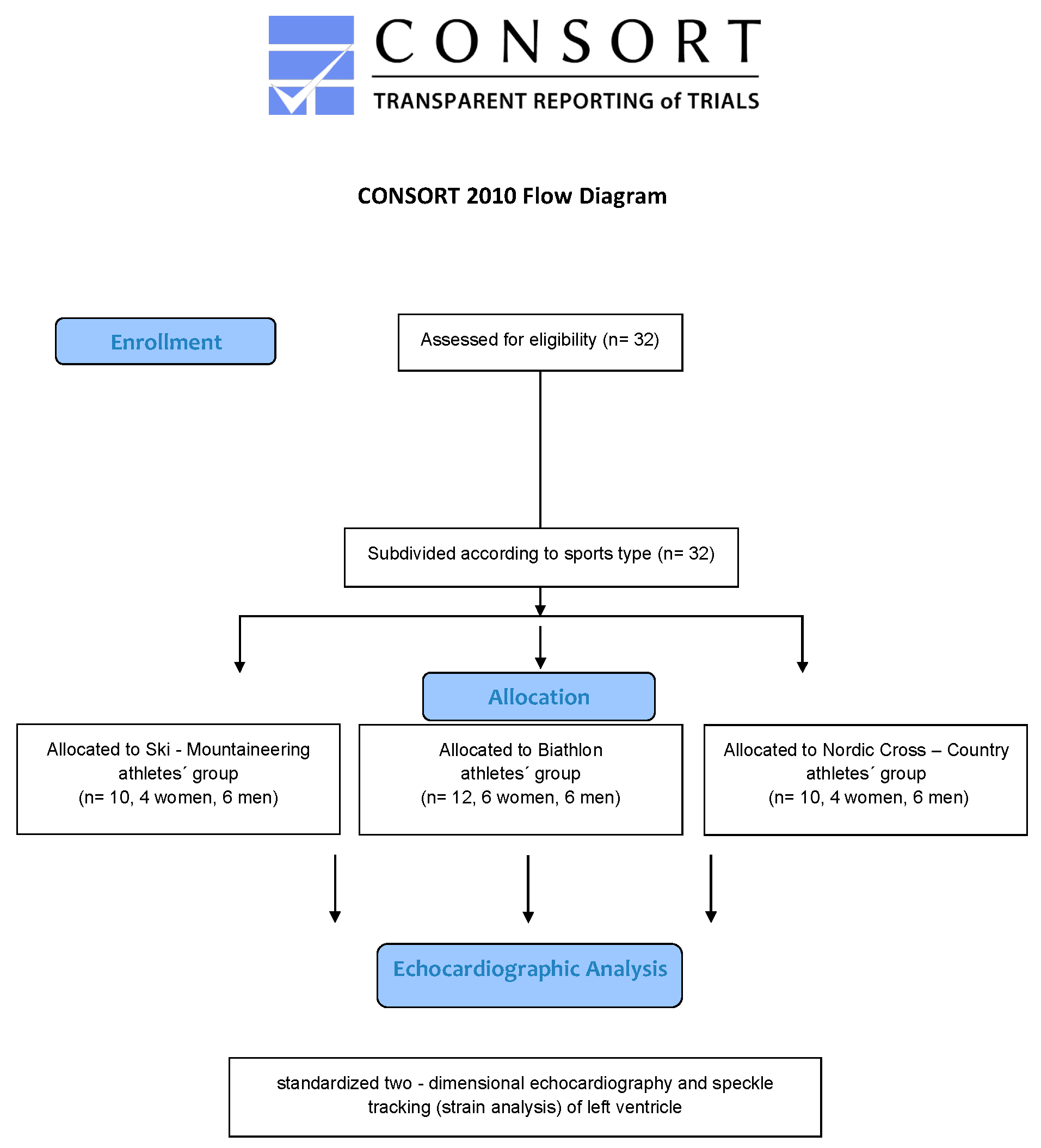
2. Materials and Methods
2.1. Study Population
2.2. Participants Visit
2.3. Statistical Analyses
3. Results
3.1. Baseline Characterictics and Echocardiographic Assessment
3.2. Morpholgical and Functional Cardiac Remodeling
4. Discussion
4.1. Impact of Two Dimensional Echocardiography on Morpholgical and Functional Cardiac Remodeling of the Athlete’s Left Heart
4.2. Global Longitudinal Strain (GLS) Analysis of the Athlete’s Left Ventricle in Winter Sport Professionals
4.3. Impact of Two Dimensional Echocardiography on Morpholgical and Functional Cardiac Remodeling of the Athlete’s Right Heart
4.4. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Buskirk, E.R.; Kollias, J.; Akers, R.F.; Prokop, E.K.; Reategui, E.P. Maximal performance at altitude and on return from altitude in conditioned runners. J. Appl. Physiol. 1967, 23, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Duc, S.; Cassirame, J.; Durand, F. Physiology of Ski Mountaineering Racing. Int. J. Sports Med. 2011, 32, 856–863. [Google Scholar] [CrossRef]
- Menz, V.; Niedermeier, M.; Stehle, R.; Mugele, H.; Faulhaber, M. Assessment of Maximal Aerobic Capacity in Ski Mountaineering: A Laboratory-Based Study. Int. J. Environ. Res. Public Health 2021, 18, 7002. [Google Scholar] [CrossRef]
- Tosi, P.; Leonardi, A.; Schena, L. The energy cost of ski mountaineering: Effects of speed and ankle loading. J. Sport Med. Phys. Fit. 2009, 49, 25–29. [Google Scholar]
- Armstrong, R.B.; Laughlin, M.H.; Rome, L.; Taylor, C.R. Metabolism of rats running up and down an incline. J. Appl. Physiol. 1983, 55, 518–521. [Google Scholar] [CrossRef]
- Balducci, P.; Clémençon, M.; Morel, B.; Quiniou, G.; Saboul, D.; Hautier, C.A. Comparison of Level and Graded Treadmill Tests to Evaluate Endurance Mountain Runners. J. Sports Sci. Med. 2016, 15, 239–246. [Google Scholar] [PubMed]
- Jonsson Kårström, M.; McGawley, K.; Laaksonen, M.S. Physiological Responses to Rifle Carriage during Roller-Skiing in Elite Biathletes. Front. Physiol. 2019, 10, 1519. [Google Scholar] [CrossRef]
- Laaksonen, M.S.; Andersson, E.; Jonsson Kårström, M.; Lindblom, H.; McGawley, K. Laboratory-Based Factors Predicting Skiing Performance in Female and Male Biathletes. Front. Sports Act. Living 2020, 2, 99. [Google Scholar] [CrossRef] [PubMed]
- Karlstedt, E.; Chelvanathan, A.; da Silva, M.; Cleverley, K.; Kumar, K.; Bhullar, N.; Lytwyn, M.; Bohonis, S.; Oomah, S.; Nepomuceno, R.; et al. The impact of repeated marathon running on cardiovascular function in the aging population. J. Cardiovasc. Magn. Reson. 2012, 14, 58. [Google Scholar] [CrossRef]
- Galderisi, M.; Cosyns, B.; Edvardsen, T.; Cardim, N.; Delgado, V.; di Salvo, G.; Donal, E.; Sade, L.E.; Ernande, L.; Garbi, M.; et al. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: An expert consensus document of the European Association of Cardiovascular Imaging. Eur. Heart J.-Cardiovasc. Imaging 2017, 18, 1301–1310. [Google Scholar] [CrossRef]
- Stefani, L.; Toncelli, L.; di Tante, V.; Vono, M.C.R.; Cappelli, B.; Pedrizzetti, G.; Galanti, G. Supernormal functional reserve of apical segments in elite soccer players: An ultrasound speckle tracking handgrip stress study. Cardiovasc. Ultrasound 2008, 6, 14. [Google Scholar] [CrossRef]
- Chandra, N.; Bastiaenen, R.; Papadakis, M.; Sharma, S. Sudden Cardiac Death in Young Athletes. J. Am. Coll. Cardiol. 2013, 61, 1027–1040. [Google Scholar] [CrossRef] [PubMed]
- Stefani, L.; Toncelli, L.; Gianassi, M.; Manetti, P.; di Tante, V.; Vono, M.R.C.; Moretti, A.; Cappelli, B.; Pedrizzetti, G.; Galanti, G. Two-dimensional tracking and TDI are consistent methods for evaluating myocardial longitudinal peak strain in left and right ventricle basal segments in athletes. Cardiovasc. Ultrasound 2007, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Szauder, I.; Kovács, A.; Pavlik, G. Comparison of left ventricular mechanics in runners versus bodybuilders using speckle tracking echocardiography. Cardiovasc. Ultrasound 2015, 13, 7. [Google Scholar] [CrossRef] [PubMed]
- Utomi, V.; Oxborough, D.; Whyte, G.P.; Somauroo, J.; Sharma, S.; Shave, R.; Atkinson, G.; George, K. Systematic review and meta-analysis of training mode, imaging modality and body size influences on the morphology and function of the male athlete’s heart. Heart 2013, 99, 1727–1733. [Google Scholar] [CrossRef]
- Pelliccia, A.; Maron, B.J.; Spataro, A.; Proschan, M.A.; Spirito, P. The Upper Limit of Physiologic Cardiac Hypertrophy in Highly Trained Elite Athletes. N. Engl. J. Med. 1991, 324, 295–301. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Merghani, A.; Mont, L. Exercise and the heart: The good, the bad, and the ugly. Eur. Heart J. 2015, 36, 1445–1453. [Google Scholar] [CrossRef]
- Galanti, G.; Toncelli, L.; Tosi, B.; Orlandi, M.; Giannelli, C.; Stefani, L.; Mascherini, G.; Modesti, P.A. Evaluation of left ventricular remodelling in young Afro-Caribbean athletes. Cardiovasc. Ultrasound 2019, 17, 20. [Google Scholar] [CrossRef]
- Maron, B.J. Structural features of the athlete heart as defined by echocardiography. J. Am. Coll. Cardiol. 1986, 7, 190–203. [Google Scholar] [CrossRef]
- Maron, B.J.; Doerer, J.J.; Haas, T.S.; Tierney, D.M.; Mueller, F.O. Sudden Deaths in Young Competitive Athletes. Circulation. 2009, 119, 1085–1092. [Google Scholar] [CrossRef]
- Maron, B.J.; Epstein, S.E.; Roberts, W.C. Causes of sudden death in competitive athletes. J. Am. Coll. Cardiol. 1986, 7, 204–214. [Google Scholar] [CrossRef]
- Maron, B.J.; Haas, T.S.; Ahluwalia, A.; Rutten-Ramos, S.C. Incidence of cardiovascular sudden deaths in Minnesota high school athletes. Heart Rhythm 2013, 10, 374–377. [Google Scholar] [CrossRef]
- Galanti, G.; Stefani, L.; Mascherini, G.; di Tante, V.; Toncelli, L. Left ventricular remodeling and the athlete’s heart, irrespective of quality load training. Cardiovasc. Ultrasound 2016, 14, 46. [Google Scholar] [CrossRef] [PubMed]
- Guasch, E.; Benito, B.; Qi, X.; Cifelli, C.; Naud, P.; Shi, Y.; Mighiu, A.; Tardif, J.-C.; Tadevosyan, A.; Chen, Y.; et al. Atrial Fibrillation Promotion by Endurance Exercise. J. Am. Coll. Cardiol. 2013, 62, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Wilhelm, M. Atrial fibrillation in endurance athletes. Eur. J. Prev. Cardiol. 2014, 21, 1040–1048. [Google Scholar] [CrossRef] [PubMed]
- Stefani, L.; Pedrizzetti, G.; de Luca, A.; Mercuri, R.; Innocenti, G.; Galanti, G. Real-time evaluation of longitudinal peak systolic strain (speckle tracking measurement) in left and right ventricles of athletes. Cardiovasc. Ultrasound 2009, 7, 17. [Google Scholar] [CrossRef]
- Beaumont, A.; Grace, F.; Richards, J.; Hough, J.; Oxborough, D.; Sculthorpe, N. Left Ventricular Speckle Tracking-Derived Cardiac Strain and Cardiac Twist Mechanics in Athletes: A Systematic Review and Meta-Analysis of Controlled Studies. Sports Med. 2017, 47, 1145–1170. [Google Scholar] [CrossRef]
- Caselli, S.; Montesanti, D.; Autore, C.; di Paolo, F.M.; Pisicchio, C.; Squeo, M.R.; Musumeci, B.; Spataro, A.; Pandian, N.G.; Pelliccia, A. Patterns of Left Ventricular Longitudinal Strain and Strain Rate in Olympic Athletes. J. Am. Soc. Echocardiogr. 2015, 28, 245–253. [Google Scholar] [CrossRef]
- Charfeddine, S.; Mallek, S.; Triki, F.; Hammami, R.; Abid, D.; Abid, L.; Kammoun, S. Echocardiographic analysis of the left ventricular function in young athletes: A focus on speckle tracking imaging. Pan Afr. Med. J. 2016, 25, 171. [Google Scholar] [CrossRef]
- D’Ascenzi, F.; Caselli, S.; Solari, M.; Pelliccia, A.; Cameli, M.; Focardi, M.; Padeletti, M.; Corrado, D.; Bonifazi, M.; Mondillo, S. Novel echocardiographic techniques for the evaluation of athletes’ heart: A focus on speckle-tracking echocardiography. Eur. J. Prev. Cardiol. 2016, 23, 437–446. [Google Scholar] [CrossRef]
- Maufrais, C.; Schuster, I.; Doucende, G.; Vitiello, D.; Rupp, T.; Dauzat, M.; Obert, P.; Nottin, S. Endurance Training Minimizes Age-Related Changes of Left Ventricular Twist-Untwist Mechanics. J. Am. Soc. Echocardiogr. 2014, 27, 1208–1215. [Google Scholar] [CrossRef]
- Santoro, A.; Alvino, F.; Antonelli, G.; Caputo, M.; Padeletti, M.; Lisi, M.; Mondillo, S. Endurance and Strength Athlete’s Heart: Analysis of Myocardial Deformation by Speckle Tracking Echocardiography. J. Cardiovasc. Ultrasound 2014, 22, 196–204. [Google Scholar] [CrossRef]
- Tokodi, M.; Lakatos, B.K.; Ruppert, M.; Fábián, A.; Oláh, A.; Sayour, A.A.; Ladányi, Z.; Soós, A.; Merkely, B.; Sengupta, P.P.; et al. Left Ventricular Pressure-Strain-Volume Loops for the Noninvasive Assessment of Volume Overload-Induced Myocardial Dysfunction. JACC Cardiovasc. Imaging 2021, 14, 1868–1871. [Google Scholar] [CrossRef]
- Zacher, J.; Blome, I.; Schenk, A.; Gorr, E. Cardiac adaptations in elite female football- and volleyball-athletes do not impact left ventricular global strain values: A speckle tracking echocardiography study. Int. J. Cardiovasc. Imaging 2020, 36, 1085–1096. [Google Scholar] [CrossRef]
- Harriss, D.J.; MacSween, A.; Atkinson, G. Ethical Standards in Sport and Exercise Science Research: 2020 Update. Int. J. Sports Med. 2019, 40, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Evangelista, A.; Flachskampf, F.; Lancellotti, P.; Badano, L.; Aguilar, R.; Monaghan, M.; Zamorano, J.; Nihoyannopoulos, P. European Association of Echocardiography recommendations for standardization of performance, digital storage and reporting of echocardiographic studies. Eur. J. Echocardiogr. 2008, 9, 438–448. [Google Scholar] [CrossRef]
- Lang, R.; Bierig, M.; Devereux, R.; Flachskampf, F.; Foster, E.; Pellikka, P.; Picard, M.; Roman, M.; Seward, J.; Shanewise, J. Recommendations for chamber quantification. Eur. J. Echocardiogr. 2006, 7, 1–39. [Google Scholar] [CrossRef] [PubMed]
- Hagendorff, A.; Fehske, W.; Flachskampf, F.A.; Helfen, A.; Kreidel, F.; Kruck, S.; la Rosée, K.; Tiemann, K.; Voigt, J.-U.; von Bardeleben, R.S.; et al. Manual zur Indikation und Durchführung der Echokardiographie—Update 2020 der Deutschen Gesellschaft für Kardiologie. Kardiologe 2020, 14, 396–431. [Google Scholar] [CrossRef]
- Hashem, M.-S.; Kalashyan, H.; Choy, J.; Chiew, S.K.; Shawki, A.-H.; Dawood, A.H.; Becher, H. Left Ventricular Relative Wall Thickness Versus Left Ventricular Mass Index in Non-Cardioembolic Stroke Patients. Medicine 2015, 94, e872. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39. [Google Scholar] [CrossRef]
- Mitchell, J.H.; Haskell, W.; Snell, P.; van Camp, S.P. Task Force 8: Classification of sports. J. Am. Coll. Cardiol. 2005, 45, 1364–1367. [Google Scholar] [CrossRef] [PubMed]
- Pavlik, G.; Major, Z.; Varga-Pintér, B.; Jeserich, M.; Kneffel, Z. The athlete’s heart Part I (Review). Acta Physiol. Hung. 2010, 97, 337–353. [Google Scholar] [CrossRef] [PubMed]
- Pluim, B.M.; Zwinderman, A.H.; van der Laarse, A.; van der Wall, E.E. The Athlete’s Heart. Circulation 2010, 101, 336–344. [Google Scholar] [CrossRef] [PubMed]
- Fagard, R. Athlete’s heart. Heart 2003, 89, 1455–1461. [Google Scholar] [CrossRef] [PubMed]
- Naylor, L.H.; George, K.; O’Driscoll, G.; Green, D.J. The Athlete’s Heart. Sports Med. 2008, 38, 69–90. [Google Scholar] [CrossRef]
- Iskandar, A.; Mujtaba, M.T.; Thompson, P.D. Left Atrium Size in Elite Athletes. JACC Cardiovasc. Imaging 2015, 8, 753–762. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, P.; Lutter, C. Haemodynamic effects of paroxysmal supraventricular tachycardia in an endurance athlete during exercise testing. BMJ Case Rep. 2019, 12, e231659. [Google Scholar] [CrossRef]
- Kasikcioglu, E.; Oflaz, H.; Akhan, H.; Kayserilioglu, A.; Umman, B.; Bugra, Z.; Erzengin, F. Left Atrial Geometric and Functional Remodeling in Athletes. Int. J. Sports Med. 2006, 27, 267–271. [Google Scholar] [CrossRef]
- Klasnja, A.V.; Jakovljevic, D.G.; Barak, O.F.; Popadic Gacesa, J.Z.; Lukac, D.D.; Grujic, N.G. Cardiac power output and its response to exercise in athletes and non-athletes. Clin. Physiol. Funct. Imaging 2013, 33, 201–205. [Google Scholar] [CrossRef]
- Major, Z.; Csajági, E.; Kneffel, Z.; Kováts, T.; Szauder, I.; Sidó, Z.; Pavlik, G. Comparison of left and right ventricular adaptation in endurance-trained male athletes. Acta Physiol. Hung. 2015, 102, 23–33. [Google Scholar] [CrossRef]
- D’Andrea, A.; Limongelli, G.; Caso, P.; Sarubbi, B.; della Pietra, A.; Brancaccio, P.; Cice, G.; Scherillo, M.; Limongelli, F.; Calabrò, R. Association between left ventricular structure and cardiac performance during effort in two morphological forms of athlete’s heart. Int. J. Cardiol. 2002, 86, 177–184. [Google Scholar] [CrossRef]
- Angelini, P.; Cheong, B.Y.; Lenge de Rosen, V.V.; Lopez, J.A.; Uribe, C.; Masso, A.H.; Ali, S.W.; Davis, B.R.; Muthupillai, R.; Willerson, J.T. Magnetic Resonance Imaging–Based Screening Study in a General Population of Adolescents. J. Am. Coll. Cardiol. 2018, 71, 579–580. [Google Scholar] [CrossRef]
- Eckart, R.E.; Scoville, S.L.; Campbell, C.L.; Shry, E.A.; Stajduhar, K.C.; Potter, R.N.; Pearse, L.A.; Virmani, R. Sudden Death in Young Adults: A 25-Year Review of Autopsies in Military Recruits. Ann. Intern. Med. 2004, 141, 829. [Google Scholar] [CrossRef]
- Angelini, P.; Vidovich, M.I.; Lawless, C.E.; Elayda, M.A.; Lopez, J.A.; Wolf, D.; Willerson, J.T. Preventing sudden cardiac death in athletes: In search of evidence-based, cost effective screening. Tex. Heart Inst. J. 2013, 40, 148–155. [Google Scholar] [PubMed]
- Mandraffino, G.; Imbalzano, E.; lo Gullo, A.; Zito, C.; Morace, C.; Cinquegrani, M.; Savarino, F.; Oreto, L.; Giuffrida, C.; Carerj, S.; et al. Abnormal left ventricular global strain during exercise-test in young healthy smokers. Sci. Rep. 2020, 10, 5700. [Google Scholar] [CrossRef] [PubMed]
- Pagourelias, E.D.; Mirea, O.; Duchenne, J.; van Cleemput, J.; Delforge, M.; Bogaert, J.; Kuznetsova, T.; Voigt, J.-U. Echo Parameters for Differential Diagnosis in Cardiac Amyloidosis. Circ. Cardiovasc. Imaging 2017, 10, e005588. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Ma, C.S.; Fan, L.; Su, B.; Wang, Y.X.; Jiang, G.D.; Zhou, B.Y. The value of left ventricular longitudinal strain in the diagnosis and differential diagnosis of myocardial amyloidosis. Zhonghua Yi Xue Za Zhi 2020, 100, 3431–3436. [Google Scholar]
- D’Ascenzi, F.; Pelliccia, A.; Solari, M.; Piu, P.; Loiacono, F.; Anselmi, F.; Caselli, S.; Focardi, M.; Bonifazi, M.; Mondillo, S. Normative Reference Values of Right Heart in Competitive Athletes: A Systematic Review and Meta-Analysis. J. Am. Soc. Echocardiogr. 2017, 30, 845–858. [Google Scholar] [CrossRef]
- D’Andrea, A.; Riegler, L.; Golia, E.; Cocchia, R.; Scarafile, R.; Salerno, G.; Pezzullo, E.; Nunziata, L.; Citro, R.; Cuomo, S.; et al. Range of right heart measurements in top-level athletes: The training impact. Int. J. Cardiol. 2013, 164, 48–57. [Google Scholar] [CrossRef] [PubMed]
- D’Ascenzi, F.; Pelliccia, A.; Corrado, D.; Cameli, M.; Curci, V.; Alvino, F.; Natali, B.M.; Focardi, M.; Bonifazi, M.; Mondillo, S. Right ventricular remodelling induced by exercise training in competitive athletes. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Sitges, M.; Merino, B.; Butakoff, C.; de la Garza, M.S.; Paré, C.; Montserrat, S.; Vidal, B.; Azqueta, M.; Sarquella, G.; Gutierrez, J.A.; et al. Characterizing the spectrum of right ventricular remodelling in response to chronic training. Int. J. Cardiovasc. Imaging 2017, 33, 331–339. [Google Scholar] [CrossRef] [PubMed]
- Pagourelias, E.D.; Kouidi, E.; Efthimiadis, G.K.; Deligiannis, A.; Geleris, P.; Vassilikos, V. Right Atrial and Ventricular Adaptations to Training in Male Caucasian Athletes: An Echocardiographic Study. J. Am. Soc. Echocardiogr. 2013, 26, 1344–1352. [Google Scholar] [CrossRef] [PubMed]
- Sandbakk, Ø.; Hegge, A.M.; Losnegard, T.; Skattebo, Ø.; Tønnessen, E.; Holmberg, H.-C. The Physiological Capacity of the World’s Highest Ranked Female Cross-country Skiers. Med. Sci. Sports Exerc. 2016, 48, 1091–1100. [Google Scholar] [CrossRef] [PubMed]



| Ski–Mo n = 10 | NCC n = 10 | Biathletes n = 12 | ||||
|---|---|---|---|---|---|---|
| Male n = 6 | Female n = 4 | Male n = 6 | Female n = 4 | Male n = 6 | Female n = 6 | |
| Age (y) | 21.2 ± 1.9 | 20.8 ± 2.4 | 26.3 ± 4.1 | 25.5 ± 0.5 | 27.3 ± 3.6 | 29.0 ± 3.2 |
| Height (cm) | 178.4 ± 3.7 | 163.5 ± 8.8 | 181.3 ± 4.7 | 171.2 ± 5.8 | 180.9 ± 5.1 | 172.8 ± 3.7 |
| Weight (kg) | 67.5 ± 0.5 | 53.2 ± 6.5 | 72.0 ± 3.0 | 63.4 ± 5.9 | 77.1 ± 3.7 | 62.5 ± 4.1 |
| BMI (kg/m2) | 18.9 ± 1.7 | 19.8 ± 0.4 | 22.0 ± 1.1 | 21.6 ± 1.2 | 23.6 ± 0.9 | 20.9 ± 1.0 |
| Resting Blood Pressure Systolic/Diastolic (mmHg) | 120 ± 5.6 82 ± 3.5 | 100 ± 8.2 72 ± 1.5 | 125 ± 8.3 78 ± 2.9 | 105 ± 7.2 71 ± 3.8 | 117 ± 7.6 77 ± 2.2 | 108 ± 6.2 70 ± 3.3 |
| Resting Heart Rate (bpm) | 40 ± 5.6 | 44 ± 4.5 | 42 ± 3.6 | 46 ± 5.1 | 41 ± 4.2 | 45 ± 5.1 |
| BSA (body surface area m2) | 1.75 ± 0.08 | 1.61 ± 0.12 | 1.88 ± 0.04 | 1.81 ±0.07 | 1.92 ± 0.04 | 1.77 ± 0.05 |
| Ski-Mo (I) n = 10 | NCC (II) n = 10 | Biathletes (III) n = 12 | p-Value | ||||
|---|---|---|---|---|---|---|---|
| Male n = 6 | Female n = 4 | Male n = 6 | Female n = 4 | Male n = 6 | Female n = 6 | ||
| LV edd (mm) | 50.83 ± 4.22 | 45.25 ± 5.96 | 55.50 ± 3.83 | 50.75 ± 3.50 | 55.50 ± 5.24 | 49.50 ± 1.52 | ns |
| 48.6 ± 5.48 | 53.6 ± 4.27 | 52.5 ± 4.83 | |||||
| LV Mass Index (g/m2) | 97.2 ± 25.2 | 76.3 ± 26.7 | 130.7 ± 16.5 | 106 ± 16.4 | 133.5 ± 20.6 | 102.3 ± 14.8 | 0.0078 * |
| 88.8 ± 26.6 * | 120.8 ± 20.1 * | 117.9 ± 23.6 * | |||||
| Relative Wall Thickness RWT | 0.38 ± 0.03 | 0.34 ± 0.06 | 0.40 ± 0.04 | 0.41 ± 0.04 | 0.40 ± 0.04 | 0.42 ± 0.04 | Ski-Mo vs. NCC 0.0230 * Ski-Mo vs. Bia 0.0230 * |
| 0.37 ± 0.05 | 0.41 ± 0.03 | 0.41 ± 0.04 | |||||
| IVSd (mm) | 8.67 ± 1.97 | 8.25 ± 2.50 | 11.00 ± 0.63 | 10.50 ± 0.58 | 10.83 ± 0.98 | 9.67 ± 1.37 | Ski-Mo vs. NCC 0.0266 *, Ski-Mo vs. Bia 0.0337 * |
| 8.5 ± 2.07 | 10.4 ± 1.17 | 10.3 ± 1.29 | |||||
| LVPWs (mm) | 9.97 ± 1.03 | 7.75 ± 1.50 | 11.17 ± 0.41 | 10.50 ± 0.58 | 12.33 ± 2.07 | 10.17 ± 1.17 | Ski-Mo vs. NCC 0.0161 * Ski-Mo vs. Bia 0.0030 * |
| 8.9 ± 1.52 | 10.9 ± 0.57 | 11.3 ± 1.96 | |||||
| E/A | 2.18 ± 0.58 | 1.98 ± 0.17 | 2.48 ± 0.26 | 2.40 ± 0.77 | 1.97 ± 0.52 | 1.75 ± 0.40 | NCC vs. Bia 0.0166 * |
| 2.1 ± 0.45 | 2.5 ± 0.49 | 1.9 ± 0.46 | |||||
| E/E′ | 6.75 ± 1.71 | 7 ± 1.79 | 6.80 ± 0.86 | 6.13 ± 1.22 | 7 ± 0.86 | 6.37 ± 1.04 | ns |
| 6.9 ± 1.66 | 6.4 ± 1.09 | 6.7 ± 0.97 | |||||
| LAVI (mL/m2) | 51.83 ± 12.1 | 46.25 ± 11.1 | 150 ± 84.58 | 89.3 ± 45.7 | 117.5 ± 37.7 | 72.8 ± 19.6 | 0.0052 * |
| 49.6 ± 11.4 | 125.7 ± 75.2 | 95.2 ± 36.9 | |||||
| RA (cm2) | 19.17 ± 3.87 | 16.75 ± 2.87 | 24.83 ± 3.73 | 18.28 ± 4.72 | 20.78 ± 3.64 | 15.50 ± 2.40 | ns |
| 18.2 ± 3.55 | 22.2 ± 5.16 | 18.1 ± 4.03 | |||||
| LV–EF | 60,33 ± 4.08 | 58.00 ± 5.60 | 61.17 ± 4.96 | 59.50 ± 4.80 | 65.83 ± 5.38 | 73.00 ± 4.34 | 0.0001 * |
| 59.4 ± 4.60 | 60.5 ± 4.70 | 69.4 ± 5.98 | |||||
| GLS | −18.26 ± 2.21 | −18.83 ± 2.93 | −21.21 ± 1.99 | −23.25 ± 3.23 | −22.62 ± 1.26 | −22.34 ± 1.42 | 0.0003 * |
| −18.5 ± 2.38 | −22.0 ± 2.61 | −22.5±1.29 | |||||
| Parameter | OUR Study Data | Reference Value Male | Reference Value Female | |
|---|---|---|---|---|
| Total Male (n = 18) | Total Female (n = 14) | |||
| LV edd (mm) | 53.9 ± 4.8 | 48.6 ± 4.1 | 42–58 | 38–52 |
| LV-EF (%) | 62.4 ± 5.2 | 64.9 ± 8.6 | 52–72 | 54–74 |
| LV Mass Index (g/m2) | 120.4 ± 26.1 | 95.9 ± 21.9 | 49–115 | 43–95 |
| IVSd (mm) | 10.2 ± 1.7 | 9.2 ± 1.7 | 6–10 | 6–9 |
| LVPWd (mm) | 11.1 ± 1.7 | 9.6 ± 1.6 | 6–10 | 6–9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zimmermann, P.; Moser, O.; Eckstein, M.L.; Wüstenfeld, J.; Schöffl, V.; Zimmermann, L.; Braun, M.; Schöffl, I. Athlete’s Heart in Elite Biathlon, Nordic Cross—Country and Ski-Mountaineering Athletes: Cardiac Adaptions Determined Using Echocardiographic Data. J. Cardiovasc. Dev. Dis. 2022, 9, 8. https://doi.org/10.3390/jcdd9010008
Zimmermann P, Moser O, Eckstein ML, Wüstenfeld J, Schöffl V, Zimmermann L, Braun M, Schöffl I. Athlete’s Heart in Elite Biathlon, Nordic Cross—Country and Ski-Mountaineering Athletes: Cardiac Adaptions Determined Using Echocardiographic Data. Journal of Cardiovascular Development and Disease. 2022; 9(1):8. https://doi.org/10.3390/jcdd9010008
Chicago/Turabian StyleZimmermann, Paul, Othmar Moser, Max L. Eckstein, Jan Wüstenfeld, Volker Schöffl, Lukas Zimmermann, Martin Braun, and Isabelle Schöffl. 2022. "Athlete’s Heart in Elite Biathlon, Nordic Cross—Country and Ski-Mountaineering Athletes: Cardiac Adaptions Determined Using Echocardiographic Data" Journal of Cardiovascular Development and Disease 9, no. 1: 8. https://doi.org/10.3390/jcdd9010008
APA StyleZimmermann, P., Moser, O., Eckstein, M. L., Wüstenfeld, J., Schöffl, V., Zimmermann, L., Braun, M., & Schöffl, I. (2022). Athlete’s Heart in Elite Biathlon, Nordic Cross—Country and Ski-Mountaineering Athletes: Cardiac Adaptions Determined Using Echocardiographic Data. Journal of Cardiovascular Development and Disease, 9(1), 8. https://doi.org/10.3390/jcdd9010008






