Prognostic Relevance of Cardiopulmonary Exercise Testing for Patients with Chronic Thromboembolic Pulmonary Hypertension
Abstract
1. Background
2. Study Design and Methods
2.1. Patients
2.2. Lung Function and CPET
2.3. Right Heart Catheterization and Echocardiography
2.4. Follow-Up
2.5. Statistics
3. Results
3.1. Patient Characteristics
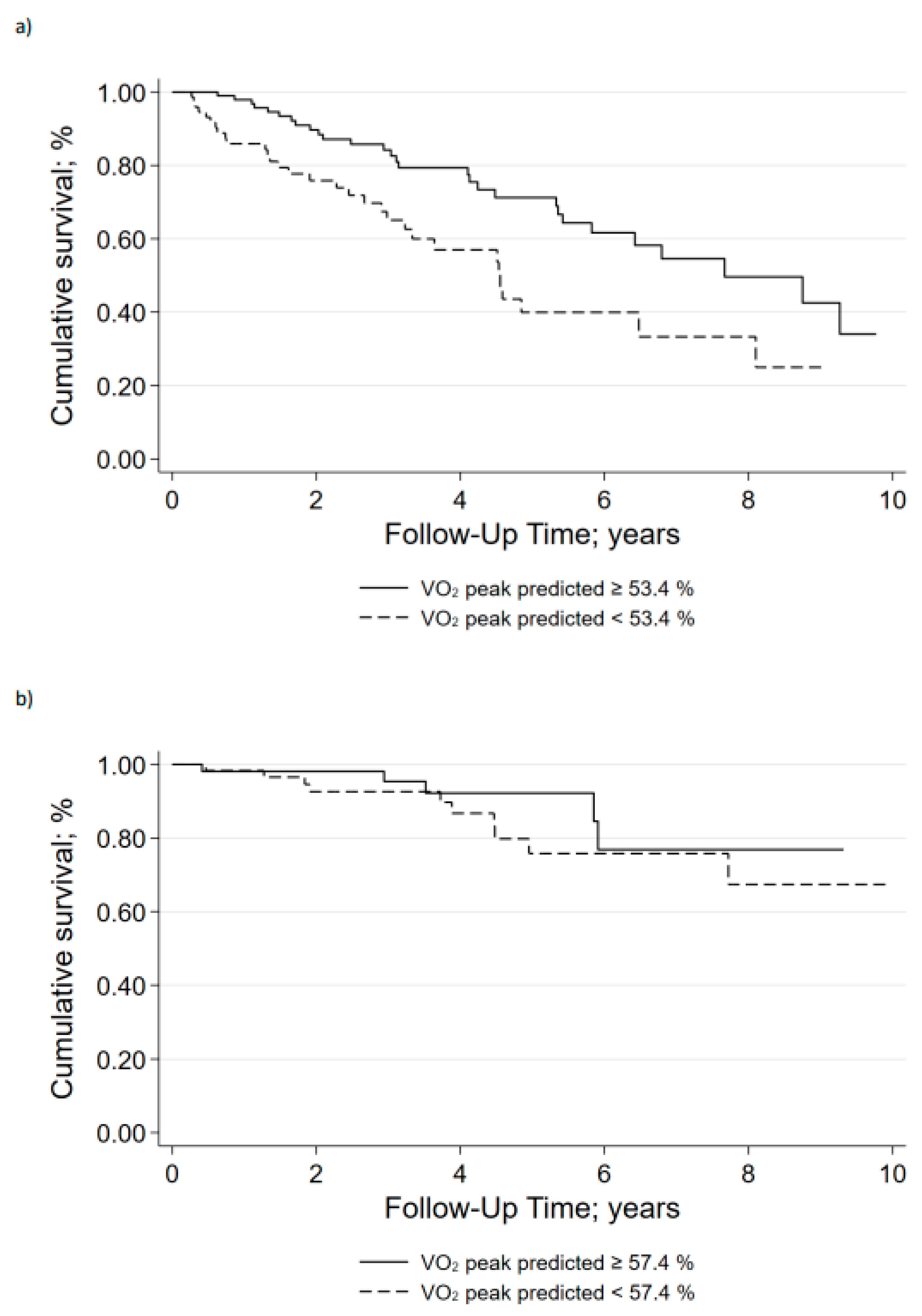
3.2. Survival
3.3. Determinants of Prognosis
4. Discussion
5. Interpretation
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Sista, A.K.; Miller, L.E.; Kahn, S.R.; Kline, J.A. Persistent right ventricular dysfunction, functional capacity limitation, exercise intolerance, and quality of life impairment following pulmonary embolism: Systematic review with meta-analysis. Vasc. Med. 2017, 22, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Klok, F.A.; van der Hulle, T.; den Exter, P.L.; Lankeit, M.; Huisman, M.V.; Konstantinides, S. The post-PE syndrome: A new concept for chronic complications of pulmonary embolism. Blood Rev. 2014, 28, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Sista, A.K.; Klok, F.A. Late outcomes of pulmonary embolism: The post-PE syndrome. Thromb. Res. 2018, 164, 157–162. [Google Scholar] [CrossRef]
- Ghofrani, H.A.; Sanchez, M.A.G.; Humbert, M.; Pittrow, D.; Simonneau, G.; Gall, H.; Grünig, E.; Klose, H.; Halank, M.; Langleben, D.; et al. Riociguat treatment in patients with chronic thromboembolic pulmonary hypertension: Final safety data from the EXPERT registry. Respir. Med. 2021, 178, 106220. [Google Scholar] [CrossRef]
- Gall, H.; Hoeper, M.M.; Richter, M.J.; Cacheris, W.; Hinzmann, B.; Mayer, E. An epidemiological analysis of the burden of chronic thromboembolic pulmonary hypertension in the USA, Europe and Japan. Eur. Respir. Rev. 2017, 26, 160121. [Google Scholar] [CrossRef] [PubMed]
- Sharma, M.; Levine, D.J. Revisiting a Distinct Entity in Pulmonary Vascular Disease: Chronic Thromboembolic Pulmonary Hypertension (CTEPH). Medicina 2021, 57, 355. [Google Scholar] [CrossRef] [PubMed]
- Held, M.; Kolb, P.; Grün, M.; Jany, B.; Hübner, G.; Grgic, A.; Holl, R.; Schaefers, H.J.; Wilkens, H. Functional Characterization of Patients with Chronic Thromboembolic Disease. Respiration 2016, 91, 503–509. [Google Scholar] [CrossRef]
- Fedullo, P.F.; Auger, W.R.; Kerr, K.M.; Rubin, L.J. Chronic thromboembolic pulmonary hypertension. Eur. Respir. J. 2019, 53, 1801915. [Google Scholar]
- Held, M.; Grün, M.; Holl, R.; Hübner, G.; Kaiser, R.; Karl, S.; Kolb, M.; Schäfers, H.J.; Wilkens, H.; Jany, B. Cardiopulmonary exercise testing to detect chronic thromboembolic pulmonary hypertension in patients with normal echocardiography. Respiration 2014, 87, 379–387. [Google Scholar] [CrossRef]
- Weatherald, J.; Philipenko, B.; Montani, D.; Laveneziana, P. Ventilatory efficiency in pulmonary vascular diseases. Eur. Respir. Rev. 2021, 30, 200214. [Google Scholar] [CrossRef]
- Wilkens, H.; Konstantinides, S.; Lang, I.M.; Bunck, A.C.; Gerges, M.; Gerhardt, F.; Grgic, A.; Grohé, C.; Guth, S.; Held, M.; et al. Chronic thromboembolic pulmonary hypertension (CTEPH): Updated Recommendations from the Cologne Consensus Conference 2018. Int. J. Cardiol. 2018, 272, 69–78. [Google Scholar] [CrossRef]
- Zhao, Q.H.; Wang, L.; Pudasaini, B.; Jiang, R.; Yuan, P.; Gong, S.G.; Guo, J.; Xiao, Q.; Liu, H.; Wu, C.; et al. Cardiopulmonary exercise testing improves diagnostic specificity in patients with echocardiography-suspected pulmonary hypertension. Clin. Cardiol. 2017, 40, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Scheidl, S.J.; Englisch, C.; Kovacs, G.; Reichenberger, F.; Schulz, R.; Breithecker, A.; Ghofrani, H.A.; Seeger, W.; Olschewski, H. Diagnosis of CTEPH versus IPAH using capillary to end-tidal carbon dioxide gradients. Eur. Respir. J. 2012, 39, 119–124. [Google Scholar] [CrossRef]
- Zhai, Z.; Murphy, K.; Tighe, H.; Wang, C.; Wilkins, M.R.; Gibbs, J.S.R.; Howard, L.S. Differences in ventilatory inefficiency between pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Chest 2011, 140, 1284–1291. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Sun, X.; Cao, Y.; Pudasaini, B.; Yang, W.; Liu, J.; Guo, J. Cardiopulmonary exercise testing and pulmonary function testing for predicting the severity of CTEPH. BMC Pulm. Med. 2021, 21, 324. [Google Scholar] [CrossRef]
- Gopalan, D.; Delcroix, M.; Held, M. Diagnosis of chronic thromboembolic pulmonary hypertension. Eur. Respir. Rev. 2017, 26, 160108. [Google Scholar] [CrossRef]
- Delcroix, M.; Torbicki, A.; Gopalan, D.; Sitbon, O.; Klok, F.A.; Lang, I.; Jenkins, D.; Kim, N.H.; Humbert, M.; Jais, X.; et al. ERS statement on chronic thromboembolic pulmonary hypertension. Eur. Respir. J. 2021, 57, 2002828. [Google Scholar] [CrossRef] [PubMed]
- Schwaiblmair, M.; Faul, C.; von Scheidt, W.; Berghaus, T.M. Ventilatory efficiency testing as prognostic value in patients with pulmonary hypertension. BMC Pulm. Med. 2012, 12, 23. [Google Scholar] [CrossRef] [PubMed]
- Groepenhoff, H.; Vonk-Noordegraaf, A.; Boonstra, A.; Spreeuwenberg, M.D.; Postmus, P.E.; Bogaard, H.J. Exercise testing to estimate survival in pulmonary hypertension. Med. Sci. Sports Exerc. 2008, 40, 1725–1732. [Google Scholar] [CrossRef]
- Galiè, N.; Humbert, M.; Vachiery, J.L.; Gibbs, S.; Lang, I.; Torbicki, A.; Simonneau, G.; Peacock, A.; Vonk Noordegraaf, A.; Beghetti, M.; et al. 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur. Respir. J. 2015, 46, 903–975. [Google Scholar]
- Cotes, J.E.; Chinn, D.J.; Quanjer, P.H.; Roca, J.; Yernault, J.C. Standardization of the measurement of transfer factor (diffusing capacity). Eur. Respir. J. 1993, 6 (Suppl. 16), 41–52. [Google Scholar] [CrossRef]
- Criee, C.P.; Berdel, D.; Heise, D.; Kardos, P.; Köhler, D.; Leupold, W.; Magnussen, H.; Marek, W.; Merget, R.; Mitfessel, H.; et al. Recommendations on spirometry by Deutsche Atemwegsliga. Pneumologie 2006, 60, 576–584. [Google Scholar] [CrossRef]
- Crièe, C.P.; Berdel, D.; Heise, D.; Kardos, P.; Köhler, D.; Leupold, W.; Magnussen, H.; Marek, W.; Merget, R.; Mitfessel, H. Empfehlungen der Deutschen Atemwegsliga und der Deutschen Gesellschaft für Pneumologie und Beatmungsmedizin. In Empfehlungen zur Ganzkörperplethysmographie (Bodyplethysmographie); Dustri-Verlag Dr. Karl Feistle: Munich, Germany; Orlando, FL, USA, 2009. [Google Scholar]
- Meyer, F.J.; Borst, M.M.; Buschmann, H.C.; Claussen, M.; Dumitrescu, D.; Ewert, R.; Friedmann-Bette, B.; Glaeser, S.; Gloeckl, R.; Haring, K.; et al. Exercise Testing in Respiratory Medicine—DGP Recommendations. Pneumologie 2018, 72, 687–731. [Google Scholar]
- Westhoff, M.; Rühle, K.H.; Greiwing, A.; Schomaker, R.; Eschenbacher, H.; Siepmann, M.; Lehnigk, B. Positional paper of the German working group "cardiopulmonary exercise testing" to ventilatory and metabolic (lactate) thresholds. Dtsch. Med. Wochenschr. 2013, 138, 275–280. [Google Scholar] [PubMed]
- Gläser, S.; Ittermann, T.; Schäper, C.; Obst, A.; Dörr, M.; Spielhagen, T.; Felix, S.B.; Völzke, H.; Bollmann, T.; Opitz, C.F.; et al. The Study of Health in Pomerania (SHIP) reference values for cardiopulmonary exercise testing. Pneumologie 2013, 67, 58–63. [Google Scholar]
- Rosenkranz, S.; Behr, J.; Ewert, R.; Ghofrani, H.A.; Gr, E.; Halank, M.; Hoeper, M.M.; Leuchte, H.H.; Olschewski, H.; Schmeisser, A.; et al. Right heart catheterization in pulmonary hypertension. Dtsch. Med. Wochenschr. 2011, 136, 2601–2616; quiz 2617–2620. [Google Scholar] [PubMed]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–270. [Google Scholar] [CrossRef]
- Weihs, W. Die standardisierte Echokardiographie: Durchführung, Archivierung und Befunderstellung inklusive Evaluierung der systolischen Linksventrikelfunktion. Aust. J. Cardiol. 2014, 21, 8–13. [Google Scholar]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 2015, 28, 1–39.e14. [Google Scholar] [CrossRef]
- McCabe, C.; Deboeck, G.; Harvey, I.; Ross, R.M.; Gopalan, D.; Screaton, N.; Pepke-Zaba, J. Inefficient exercise gas exchange identifies pulmonary hypertension in chronic thromboembolic obstruction following pulmonary embolism. Thromb. Res. 2013, 132, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Habedank, D.; Opitz, C.; Karhausen, T.; Kung, T.; Steinke, I.; Ewert, R. Predictive Capability of Cardiopulmonary and Exercise Parameters From Day 1 to 6 Months After Acute Pulmonary Embolism. Clin. Med. Insights Circ. Respir. Pulm. Med. 2018, 12, 1179548418794155. [Google Scholar] [CrossRef] [PubMed]
- Laveneziana, P.; Di Paolo, M.; Palange, P. The clinical value of cardiopulmonary exercise testing in the modern era. Eur. Respir. Rev. 2021, 30, 200187. [Google Scholar] [CrossRef] [PubMed]
- Lewczuk, J.; Piszko, P.; Jagas, J.; Porada, A.; Sobkowicz, B.; Wrabec, K.; Wójciak, S. Prognostic factors in medically treated patients with chronic pulmonary embolism. Chest 2001, 119, 818–823. [Google Scholar] [CrossRef]
- Wensel, R.; Francis, D.P.; Meyer, F.J.; Opitz, C.F.; Bruch, L.; Halank, M.; Winkler, J.; Seyfarth, H.J.; Gläser, S.; Blumberg, F.; et al. Incremental prognostic value of cardiopulmonary exercise testing and resting haemodynamics in pulmonary arterial hypertension. Int. J. Cardiol. 2013, 167, 1193–1198. [Google Scholar] [CrossRef]
- Wensel, R.; Opitz, C.F.; Anker, S.D.; Winkler, J.; Höffken, G.; Kleber, F.X.; Sharma, R.; Hummel, M.; Hetzer, R.; Ewert, R. Assessment of survival in patients with primary pulmonary hypertension: Importance of cardiopulmonary exercise testing. Circulation 2002, 106, 319–324. [Google Scholar] [CrossRef]
- Malhotra, R.; Bakken, K.; D’Elia, E.; Lewis, G.D. Cardiopulmonary Exercise Testing in Heart Failure. JACC Heart Fail. 2016, 4, 607–616. [Google Scholar] [CrossRef]
- Tromeur, C.; Jaïs, X.; Mercier, O.; Couturaud, F.; Montani, D.; Savale, L.; Jevnikar, M.; Weatherald, J.; Sitbon, O.; Parent, F.; et al. Factors predicting outcome after pulmonary endarterectomy. PLoS ONE 2018, 13, e0198198. [Google Scholar] [CrossRef]
- Korsholm, K.; Andersen, A.; Mellemkjær, S.; Nielsen, D.V.; Klaaborg, K.E.; Ilkjær, L.B.; Nielsen-Kudsk, J.E. Results from more than 20 years of surgical pulmonary endarterectomy for chronic thromboembolic pulmonary hypertension in Denmark. Eur. J. Cardiothorac. Surg. 2017, 52, 704–709. [Google Scholar] [CrossRef]
- Kallonen, J.; Glaser, N.; Bredin, F.; Corbascio, M.; Sartipy, U. Life expectancy after pulmonary endarterectomy for chronic thromboembolic pulmonary hypertension: A Swedish single-center study. Pulm. Circ. 2020, 10, 2045894020918520. [Google Scholar] [CrossRef] [PubMed]
- Kopeć, G.; Dzikowska-Diduch, O.; Mroczek, E.; Mularek-Kubzdela, T.; Chrzanowski, Ł.; Skoczylas, I.; Tomaszewski, M.; Peregud-Pogorzelska, M.; Karasek, D.; Lewicka, E.; et al. Characteristics and outcomes of patients with chronic thromboembolic pulmonary hypertension in the era of modern therapeutic approaches: Data from the Polish multicenter registry (BNP-PL). Ther. Adv. Chronic Dis. 2021, 12, 20406223211002961. [Google Scholar] [CrossRef]
- Delcroix, M.; Staehler, G.; Gall, H.; Grünig, E.; Held, M.; Halank, M.; Klose, H.; Vonk-Noordegraaf, A.; Rosenkranz, S.; Pepke-Zaba, J.; et al. Risk assessment in medically treated chronic thromboembolic pulmonary hypertension patients. Eur. Respir. J. 2018, 52, 1800248. [Google Scholar] [CrossRef] [PubMed]
- Delcroix, M.; Lang, I.; Pepke-Zaba, J.; Jansa, P.; D’Armini, A.M.; Snijder, R.; Bresser, P.; Torbicki, A.; Mellemkjaer, S.; Lewczuk, J.; et al. Long-Term Outcome of Patients With Chronic Thromboembolic Pulmonary Hypertension: Results From an International Prospective Registry. Circulation 2016, 133, 859–871. [Google Scholar] [CrossRef] [PubMed]
- Brenot, P.; Jaïs, X.; Taniguchi, Y.; Alonso, C.G.; Gerardin, B.; Mussot, S.; Mercier, O.; Fabre, D.; Parent, F.; Jevnikar, M.; et al. French experience of balloon pulmonary angioplasty for chronic thromboembolic pulmonary hypertension. Eur. Respir. J. 2019, 53, 1802095. [Google Scholar] [CrossRef] [PubMed]
- Madani, M.M.; Auger, W.R.; Pretorius, V.; Sakakibara, N.; Kerr, K.M.; Kim, N.H.; Fedullo, P.F.; Jamieson, S.W. Pulmonary endarterectomy: Recent changes in a single institution’s experience of more than 2700 patients. Ann. Thorac. Surg. 2012, 94, 97–103; discussion 103. [Google Scholar] [CrossRef]
- Mayer, E.; Jenkins, D.; Lindner, J.; D’armini, A.; Kloek, J.; Meyns, B.; Ilkjaer, L.B.; Klepetko, W.; Delcroix, M.; Lang, I.; et al. Surgical management and outcome of patients with chronic thromboembolic pulmonary hypertension: Results from an international prospective registry. J. Thorac. Cardiovasc. Surg. 2011, 141, 702–710. [Google Scholar] [CrossRef]
- Richter, M.J.; Sommer, N.; Gall, H.; Voswinckel, R.; Seeger, W.; Mayer, E.; Wiedenroth, C.B.; Rieth, A.; Grimminger, F.; Guth, S.; et al. Pulmonary Hemodynamic Response to Exercise in Chronic Thromboembolic Pulmonary Hypertension before and after Pulmonary Endarterectomy. Respiration 2015, 90, 63–73. [Google Scholar] [CrossRef]
- Radtke, T.; Crook, S.; Kaltsakas, G.; Louvaris, Z.; Berton, D.; Urquhart, D.S.; Kampouras, A.; Rabinovich, R.A.; Verges, S.; Kontopidis, D.; et al. ERS statement on standardisation of cardiopulmonary exercise testing in chronic lung diseases. Eur. Respir. Rev. 2019, 28, 180101. [Google Scholar] [CrossRef]
- Benzo, R.P.; Paramesh, S.; Patel, S.A.; Slivka, W.A.; Sciurba, F.C. Optimal protocol selection for cardiopulmonary exercise testing in severe COPD. Chest 2007, 132, 1500–1505. [Google Scholar] [CrossRef]
- Ewert, R.; Gläser, S.; Winkler, J.; Schrader, H.; Trümper, B.G.; Haase, P.U.; Obst, A.; Hoheisel, G. Cardiopulmonary Exercise Testing (CPET) in severe COPD--a multicentre comparison of two test protocols. Pneumologie 2012, 66, 402–407. [Google Scholar]


| Parameter | Non-Surgical Treatment (n = 207) | Surgical Treatment (n = 138) | p | ||
|---|---|---|---|---|---|
| n | Mean ± SD or n (%) | n | Mean ± SD or n (%) | ||
| Age (years) | 207 | 69 ± 12 | 138 | 61 ± 12 | <0.001 |
| Sex (female) | 207 | 101 (48.8) | 138 | 61 (44.2) | 0.403 |
| Body mass index (kg/m2) | 204 | 28.7 ± 5.5 | 137 | 28.3 ± 4.9 | 0.675 |
| Comorbidities | |||||
| Hypertension | 194 | 131 (67.5) | 124 | 66 (53.2) | 0.010 |
| Venous thromboembolism | 122 | 75 (61.5) | 86 | 59 (68.6) | 0.290 |
| Atrial fibrillation | 169 | 54 (32.0) | 112 | 11 (9.8) | <0.001 |
| Chronic renal failure | 193 | 60 (31.1) | 124 | 37 (29.8) | 0.814 |
| Diabetes mellitus | 192 | 37 (19.3) | 124 | 12 (9.7) | 0.021 |
| Coronary artery disease | 193 | 37 (19.2) | 124 | 24 (19.4) | 0.968 |
| COPD/asthma | 139 | 26 (18.7) | 79 | 12 (15.2) | 0.511 |
| Malignancy | 160 | 29 (18.1) | 112 | 16 (14.3) | 0.402 |
| Peripheral artery disease | 92 | 6 (6.5) | 78 | 0 (0.0) | 0.022 |
| Interstitial lung disease | 185 | 11 (6.0) | 122 | 1 (0.8) | 0.023 |
| Parameter | Non-Surgical Treatment (n = 207) | Surgical Treatment (n = 138) | p | ||
|---|---|---|---|---|---|
| n | Mean ± SD or n (%) | n | Mean ± SD or n (%) | ||
| WHO functional class | 190 | 121 | |||
| I | 5 (2.6) | 9 (7.4) | 0.071 | ||
| II | 48 (25.3) | 39 (32.2) | |||
| III | 126 (66.3) | 69 (57.0) | |||
| IV | 11 (5.8) | 4 (3.3) | |||
| Six-minute walk distance (m) | 107 | 336 ± 115 | 75 | 390 ± 122 | 0.001 |
| Echocardiography | |||||
| LVEF (%) | 147 | 59.9 ± 7.4 | 95 | 61.2 ± 10.2 | 0.031 |
| TAPSE (mm) | 151 | 19.9 ± 5.6 | 102 | 19.0 ± 5.7 | 0.040 |
| Estimated RVSP (mm Hg) | 138 | 59.1 ± 27.1 | 94 | 62.4 ± 28.1 | 0.239 |
| Right heart catheterization | |||||
| RAPm (mm Hg) | 189 | 8.3 ± 5.0 | 126 | 7.9 ± 5.1 | 0.407 |
| PAPm (mm Hg) | 207 | 41.0 ± 11.1 | 138 | 42.2 ± 10.8 | 0.481 |
| PVR (Wood Units) | 179 | 7.7 ± 4.3 | 113 | 7.9 ± 4.2 | 0.280 |
| TPR (Wood Units) | 183 | 9.9 ± 4.7 | 111 | 9.4 ± 3.8 | 0.321 |
| Cardiac index (L/min/m2) | 183 | 2.5 ± 0.8 | 111 | 2.4 ± 0.5 | 0.547 |
| SvO2 (%) | 140 | 64.0 ± 8.6 | 103 | 63.2 ± 9.3 | 0.316 |
| Parameter | Non-Surgical Treatment (n = 207) | Surgical Treatment (n = 138) | p | ||
|---|---|---|---|---|---|
| n | Mean ± SD | n | Mean ± SD | ||
| Pulmonary function | |||||
| TLC (% pred.) | 178 | 95.6 ± 17.3 | 125 | 101.4 ± 14.4 | 0.003 |
| FVC (% pred.) | 183 | 86.0 ± 19.8 | 129 | 93.8 ± 17.8 | 0.032 |
| FEV1 (% pred.) | 185 | 80.4 ± 20.3 | 131 | 86.5 ± 18.3 | 0.123 |
| FEV1/FVC (%) | 183 | 72.7 ± 10.4 | 129 | 73.8 ± 7.8 | 0.647 |
| RV (% pred.) | 176 | 114 ± 35 | 126 | 120.3 ± 29.4 | 0.004 |
| RV/TLC (% pred.) | 166 | 47.7 ± 11.7 | 123 | 43.0 ± 10.7 | 0.001 |
| DLCO (% pred.) | 105 | 59.6 ± 18.9 | 71 | 64.6 ± 14.7 | 0.091 |
| KCO (% pred.) | 155 | 74.5 ± 19.9 | 116 | 76.1 ± 15.5 | 0.766 |
| Cardiopulmonary exercise test | |||||
| Max. power (% pred.) | 200 | 62.2 ± 36.5 | 129 | 72.6 ± 42.3 | 0.159 |
| VO2peak (mL/min/kg) | 192 | 12.9 ± 4.2 | 133 | 13.2 ± 3.8 | 0.311 |
| VO2peak (% pred.) | 192 | 59.8 ± 19.8 | 133 | 57.9 ± 19.7 | 0.498 |
| VO2/heart rate max. (mL/beat) | 191 | 8.8 ± 3.0 | 132 | 8.7 ± 2.7 | 0.857 |
| VE/VCO2 slope | 164 | 50.4 ± 16.2 | 111 | 53.9 ± 18.1 | 0.336 |
| VE/VCO2 at rest | 175 | 44.6 ± 9.2 | 111 | 47.0 ± 9.3 | 0.026 |
| VE/VCO2 at VT1 | 150 | 45.0 ± 10.9 | 100 | 48.3 ± 12.0 | 0.352 |
| PETCO2 at rest (mm Hg) | 173 | 26.1 ± 5.5 | 109 | 24.1 ± 4.5 | 0.010 |
| PETCO2 at VT1 (mm Hg) | 147 | 26.4 ± 6.7 | 102 | 24.1 ± 5.9 | 0.065 |
| P(A-a)O2 max. (mm Hg) | 100 | 47.8 ± 14.7 | 75 | 51.7 ± 14.5 | 0.150 |
| P(a-ET)CO2 peak (mm Hg) | 101 | 8.3 ± 4.3 | 74 | 9.6 ± 4.2 | 0.057 |
| VE/MVV (%) | 163 | 83.7 ± 29.8 | 123 | 103.9 ± 34.7 | <0.001 |
| PaO2 at rest (mm Hg) | 166 | 65.6 ± 12.8 | 102 | 75.6 ± 78.8 | 0.196 |
| PaO2 max. (mm Hg) | 144 | 61.9 ± 13.9 | 101 | 62.1 ± 11.0 | 0.855 |
| PaCO2 at rest (mm Hg) | 166 | 35.0 ± 5.2 | 100 | 32.9 ± 3.8 | 0.027 |
| PaCO2 max. (mm Hg) | 100 | 34.0 ± 6.9 | 72 | 31.6 ± 5.1 | 0.625 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ewert, R.; Ittermann, T.; Schmitt, D.; Pfeuffer-Jovic, E.; Stucke, J.; Tausche, K.; Halank, M.; Winkler, J.; Hoheisel, A.; Stubbe, B.; et al. Prognostic Relevance of Cardiopulmonary Exercise Testing for Patients with Chronic Thromboembolic Pulmonary Hypertension. J. Cardiovasc. Dev. Dis. 2022, 9, 333. https://doi.org/10.3390/jcdd9100333
Ewert R, Ittermann T, Schmitt D, Pfeuffer-Jovic E, Stucke J, Tausche K, Halank M, Winkler J, Hoheisel A, Stubbe B, et al. Prognostic Relevance of Cardiopulmonary Exercise Testing for Patients with Chronic Thromboembolic Pulmonary Hypertension. Journal of Cardiovascular Development and Disease. 2022; 9(10):333. https://doi.org/10.3390/jcdd9100333
Chicago/Turabian StyleEwert, Ralf, Till Ittermann, Delia Schmitt, Elena Pfeuffer-Jovic, Johannes Stucke, Kristin Tausche, Michael Halank, Jörg Winkler, Andreas Hoheisel, Beate Stubbe, and et al. 2022. "Prognostic Relevance of Cardiopulmonary Exercise Testing for Patients with Chronic Thromboembolic Pulmonary Hypertension" Journal of Cardiovascular Development and Disease 9, no. 10: 333. https://doi.org/10.3390/jcdd9100333
APA StyleEwert, R., Ittermann, T., Schmitt, D., Pfeuffer-Jovic, E., Stucke, J., Tausche, K., Halank, M., Winkler, J., Hoheisel, A., Stubbe, B., Heine, A., Seyfarth, H.-J., Opitz, C., Habedank, D., Wensel, R., & Held, M. (2022). Prognostic Relevance of Cardiopulmonary Exercise Testing for Patients with Chronic Thromboembolic Pulmonary Hypertension. Journal of Cardiovascular Development and Disease, 9(10), 333. https://doi.org/10.3390/jcdd9100333








