Minimally Invasive Surgical Repair of a Partial Atrioventricular Canal Defect in a 20-Year-Old Patient—A Case Report and Review of Literature
Abstract
:1. Introduction
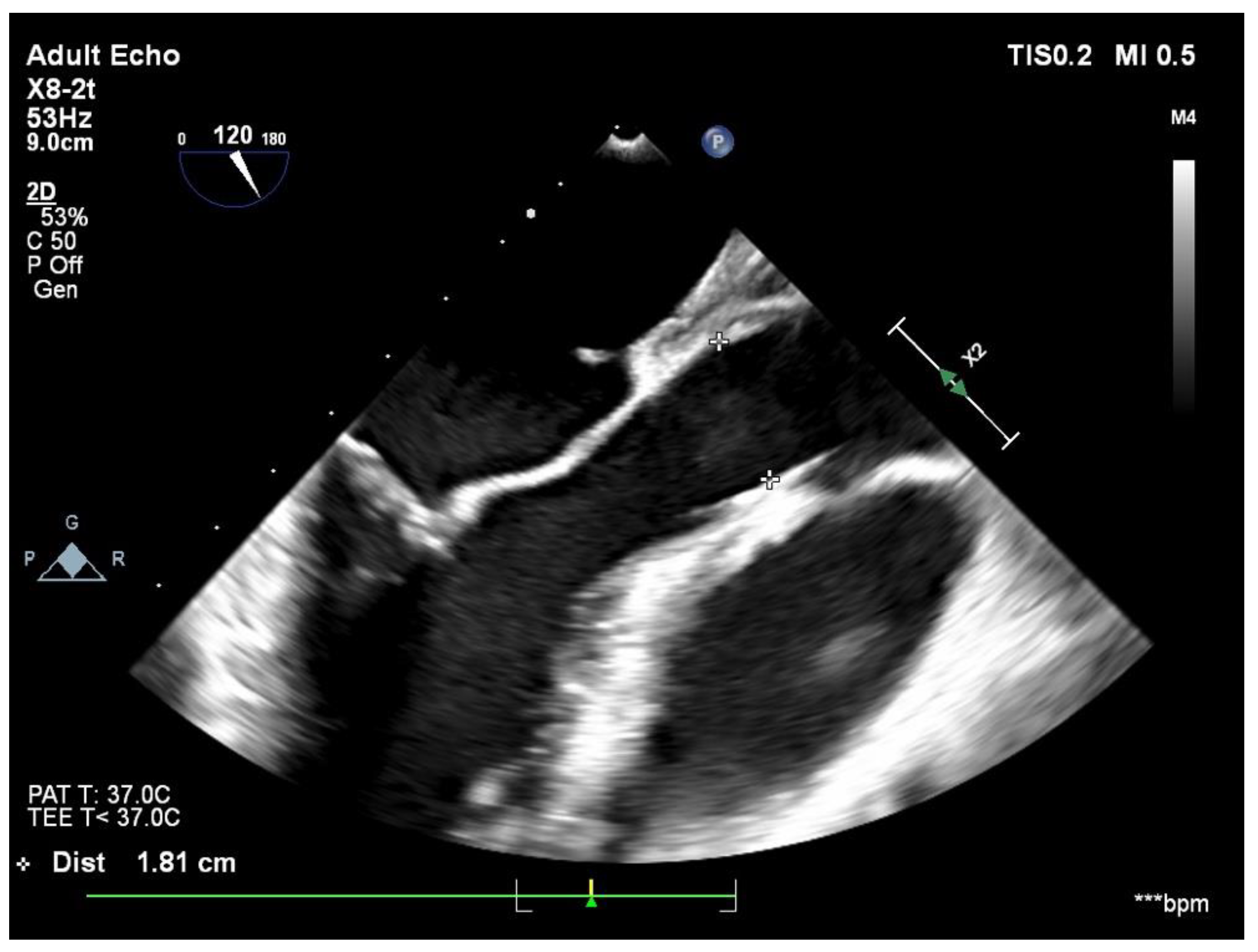
2. Case Report
3. Discussions
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Geva, T.; Martins, J.D.; Wald, R.M. Atrial septal defects. Lancet 2014, 383, 1921–1932. [Google Scholar] [CrossRef]
- Costache, V.S.; Moldovan, H.; Arsenescu, C.; Costache, A. Aortic valve surgery of the 21st century: Sutureless AVR versus TAVI. Minerva Cardioangiol. 2018, 66, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Carpentier, A. Surgical anatomy and management of the mitral component of atrioventricular canal defects. In Pediatric Cardiology; Churchill Livingstone: London, UK, 1978; pp. 477–486. [Google Scholar]
- Iliuta, L.; Rac-Albu, M. Predictors and late incidence of persistent or recurrent heart failure after aortic valve replacement for aortic stenosis compared with aortic regurgitation. Eur. Heart J. 2014, 35, 58. [Google Scholar]
- Dobritoiu, F.; Moldovan, H.; Oncica, R.; Vasile, G.; Nechifor, E.; Copaescu, C. Giant Cavernous Hemangioma of the Right Atrium—A Rare Case and Literature Review. Chirurgia 2020, 115, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Molnar, A.; Sacui, D.; Oprea, A.; Trifan, C.; Moldovan, H. Native Valve Infective Endocarditis - the Postoperative Results and Role of the Endocarditis Team. A Single Center Experience. Chirurgia 2021, 116, 75–88. [Google Scholar] [CrossRef]
- Iliuta, L.; Savulescu, C.; Moldovan, H.; Gherghiceanu, D.P.; Vasile, R.; Filipescu, D.; Macarie, C.; Candea, V. Diastolic versus systolic left ventricular dysfunction as independent predictors for unfavourable postoperative evolution in patients with aortic stenosis undergoing aortic valve replacement. Eur. Heart J. 2005, 26, 193. [Google Scholar]
- Pacifico, A.D.; Ricchi, A.; Bargeron, L.; Colvin, E.; Kirklin, J. Corrective repair of complete atrioventricular canal defects and major associated cardiac anomalies. Ann. Thorac. Surg. 1998, 46, 645–651. [Google Scholar] [CrossRef]
- Filipescu, D.; Calugareanu, A.; Luchian, M.; Marinica, I.; Ghenu, O.; Marin, S.; Moldovan, H.; Deleanu, D. Fatal myocardial infarction secondary to thyrotoxicosis. Case report. Acta Endocrinol.-Buchar. 2009, 5, 275–281. [Google Scholar] [CrossRef]
- Socoteanu, I. Tratat de Patologie Chirurgicala Cardiovasculara; Medicala: București, Romania, 2007; Volume I, pp. 621–631. ISBN 6422573000364. [Google Scholar]
- Goh, E.; Mohammed, H.; Salmasi, M.Y.; Ho, S.; Benedetto, U.; Caputo, M.; Angelini, G.; Vohra, H.A. Minimally invasive versus transcatheter closure of secundum atrial septal defects: A systematic review and meta-analysis. Perfusion 2021, 37, 2676591211021935. [Google Scholar]
- Yanagisawa, J.; Maekawa, A.; Sawaki, S.; Tokoro, M.; Ozeki, T.; Orii, M.; Saiga, T.; Ito, T. Three-port totally endoscopic repair vs conventional median sternotomy for atrial septal defect. Surg. Today 2019, 49, 118–123. [Google Scholar] [CrossRef]
- Zhu, J.; Zhang, Y.; Bao, C.; Ding, F.; Mei, J. Individualized strategy of minimally invasive cardiac surgery in congenital cardiac septal defects. J. Cardiothorac. Surg. 2022, 17, 5. [Google Scholar] [CrossRef]
- Moldovan, H.; Sibișan, A.M.; Țigănașu, R.; Popescu, B.Ș.; Vasile, G.; Gheorghiță, D.; Zaharia, O.; Costache, V.S.; Guță, A.; Molnar, A. Superior Sinus Venosus Atrial Septal Defect with Partial Anomalous Pulmonary Venous Drainage-Minimally Invasive Approach-Case Report. Medicina 2021, 57, 984. [Google Scholar] [CrossRef] [PubMed]
- Mylonas, K.S.; Ziogas, I.A.; Evangeliou, A.; Hemmati, P.; Schizas, D.; Sfyridis, P.G.; Economopoulos, K.P.; Bakoyiannis, C.; Kapelouzou, A.; Tzifa, A.; et al. Minimally Invasive Surgery vs Device Closure for Atrial Septal Defects: A Systematic Review and Meta-analysis. Pediatr. Cardiol. 2020, 41, 853–861. [Google Scholar] [CrossRef] [PubMed]
- Sabzi, F.; Faraji, R.; Kazeminasab, M. Minimal Invasive Technique in Atrial Septal Defect Surgery. Cardiol. Res. 2018, 9, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Mishra, S.; Tomar, M.; Malhotra, R.; Radhakrishnan, S.; Mishra, Y.; Iyer, K.S.; Shrivastava, S.; Trehan, N. Comparison between transcatheter closure and minimally invasive surgery for fossa ovalis atrial septal defect: A single institutional experience. Indian Heart J. 2008, 60, 125–132. [Google Scholar] [PubMed]
- Liava’a, M.; Kalfa, D. Surgical closure of atrial septal defects. J. Thorac. Dis. 2018, 10 (Suppl. S24), S2931–S2939. [Google Scholar] [CrossRef] [PubMed]
- Zheng, X.X.; Wang, Z.Y.; Ma, L.Y.; Liu, H.; Liu, H.; Qin, J.W.; Shao, Y.F. Triport periareolar thoracoscopic surgery versus right minithoracotomy for repairing atrial septal defect in adults. Interact. Cardiovasc. Thorac. Surg. 2021, 32, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Barbero, C.; Marchetto, G.; Pace Napoleone, C.; Calia, C.; Cura Stura, E.; Pocar, M.; Rinaldi, M.; Boffini, M. Right mini-thoracotomy approach for grown-up congenital heart disease. J. Card. Surg. 2021, 36, 1917–1921. [Google Scholar] [CrossRef] [PubMed]
- Myers, P.; Sologashvili, T.; Prêtre, R. Non-visible scar surgery: Right axillary thoracotomy approach for partial atrioventricular canal repair. Multimed. Man. Cardiothorac. Surg. 2019, 2019, 31872984. [Google Scholar]
- Robu, M.; Marian, D.R.; Lazăr, E.; Radu, R.; Boroș, C.; Sibișan, A.; Voica, C.; Broască, M.; Gheorghiță, D.; Moldovan, H.; et al. Open Coronary Endarterectomy of Left Anterior Descending Artery—Case Report and Review of Literature. J. Cardiovasc. Dev. Dis. 2022, 9, 83. [Google Scholar] [CrossRef] [PubMed]
- Müller, L.; Höfer, D.; Holfeld, J.; Hangler, H.; Bonaros, N.; Grimm, M. Indications and contra-indications for minimally invasive mitral valve surgery. J. Vis. Surg. 2018, 4, 255. [Google Scholar] [CrossRef]
- Byrne, J.G.; Adams, D.H.; Mitchell, M.E.; Cohn, L.H. Minimally invasive direct access for repair of atrial septal defect in adults. Am. J. Cardiol. 1999, 84, 919–922. [Google Scholar] [CrossRef]
- Kharouf, R.; Luxenberg, D.M.; Khalid, O.; Abdulla, R. Atrial septal defect: Spectrum of care. Pediatr. Cardiol. 2008, 29, 271–280. [Google Scholar] [CrossRef]
- Bakar, S.N.; Burns, D.J.P.; Diamantouros, P.; Sridhar, K.; Kiaii, B.; Chu, M.W.A. Clinical outcomes of a combined transcatheter and minimally invasive atrial septal defect repair program using a ‘Heart Team’ approach. J. Cardiothorac. Surg. 2018, 13, 11. [Google Scholar] [CrossRef] [PubMed]
- Chu, M.W.; Losenno, K.L.; Fox, S.A.; Adams, C.; Al-Habib, H.; Guo, R.; Menkis, A.H.; Kiaii, B. Clinical outcomes of minimally invasive endoscopic and conventional sternotomy approaches for atrial septal defect repair. Can. J. Surg. 2014, 57, E75–E81. [Google Scholar] [CrossRef]
- Buzatu, M.; Geantă, V.; Ştefănoiu, R.; Buţu, M.; Petrescu, M.I.; Buzatu, M.; Antoniac, I.; Iacob, G.; Niculescu, F.; Ghica, Ş.I.; et al. Investigations into Ti-15Mo-W Alloys Developed for Medical Applications. Materials 2019, 12, 147. [Google Scholar] [CrossRef] [Green Version]
- Chowdhury, U.K.; Airan, B.; Malhotra, A.; Bisoi, A.K.; Kalaivani, M.; Govindappa, R.M.; Venugopal, P. Specific issues after surgical repair of partial atrioventricular septal defect: Actuarial survival, freedom from reoperation, fate of the left atrioventricular valve, prevalence of left ventricular outflow tract obstruction, and other events. J. Thorac. Cardiovasc. Surg. 2009, 137, 548–555.e2. [Google Scholar] [CrossRef] [Green Version]
- Jurcut, R.; Savu, O.; Popescu, B.A.; Florian, A.; Herlea, V.; Moldovan, H.; Ginghina, C. Primary cardiac leiomyoma when valvular disease becomes a vascular surgical emergency. Circulation 2010, 121, e415–e418. [Google Scholar] [CrossRef]
- Rusu, E.L.E.N.A.; Sarbu, I.; Cristescu, C.; Coculescu, B.I.; Moldovan, H.; Petrut, S.; Muresan, A.; Vassu, T.; Pelinescu, D. Highlighting the Antimicrobial Activity of Organic Componds Isolated from some strains of lacticacid bacteria. Rev. Chim. 2016, 67, 2417–2421. [Google Scholar]
- Evseev, E.P.; Golovina, V.I.; Ivanov, V.A.; Belov, Y.V. Plastika sinus septum defekta s korrektsieĭ chastichnogo anomal’nogo drenazha legochnykh ven iz minitorakotomnogo dostupa [Sinus septal defect closure with correction of partial anomalous pulmonary vein drainage through mini-thoracotomy]. Khirurgiia 2020, 1, 85–88. [Google Scholar]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moldovan, H.; Bulescu, C.; Cacoveanu, M.; Voica, C.; Safta, S.; Goicea, M.; Dobra, I.; Antoniac, I.; Gheorghiță, D.; Zaharia, O. Minimally Invasive Surgical Repair of a Partial Atrioventricular Canal Defect in a 20-Year-Old Patient—A Case Report and Review of Literature. J. Cardiovasc. Dev. Dis. 2022, 9, 352. https://doi.org/10.3390/jcdd9100352
Moldovan H, Bulescu C, Cacoveanu M, Voica C, Safta S, Goicea M, Dobra I, Antoniac I, Gheorghiță D, Zaharia O. Minimally Invasive Surgical Repair of a Partial Atrioventricular Canal Defect in a 20-Year-Old Patient—A Case Report and Review of Literature. Journal of Cardiovascular Development and Disease. 2022; 9(10):352. https://doi.org/10.3390/jcdd9100352
Chicago/Turabian StyleMoldovan, Horațiu, Cristian Bulescu, Mihai Cacoveanu, Cristian Voica, Sabina Safta, Mihai Goicea, Irina Dobra, Iulian Antoniac, Daniela Gheorghiță, and Ondin Zaharia. 2022. "Minimally Invasive Surgical Repair of a Partial Atrioventricular Canal Defect in a 20-Year-Old Patient—A Case Report and Review of Literature" Journal of Cardiovascular Development and Disease 9, no. 10: 352. https://doi.org/10.3390/jcdd9100352
APA StyleMoldovan, H., Bulescu, C., Cacoveanu, M., Voica, C., Safta, S., Goicea, M., Dobra, I., Antoniac, I., Gheorghiță, D., & Zaharia, O. (2022). Minimally Invasive Surgical Repair of a Partial Atrioventricular Canal Defect in a 20-Year-Old Patient—A Case Report and Review of Literature. Journal of Cardiovascular Development and Disease, 9(10), 352. https://doi.org/10.3390/jcdd9100352






