Comparison of Different Laboratory Tests to Identify “Aspirin Resistance” and Risk of Vascular Events among Ischaemic Stroke Patients: A Double-Blind Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subject Selection
2.2. Laboratory Tests
2.2.1. Light Transmission Aggregometry (LTA)
2.2.2. Whole Blood Turbidimetric-Based Aggregometry (VerifyNow® System, Accumetrics, San Diego, CA, USA)
2.2.3. Whole Blood Multiple Electrode Impedance Aggregometry (Multiplate® Platelet Function Analyzer, Dynabyte Medical, Munich, through Dyamed Biotech, Singapore)
2.3. Definition of Aspirin Resistance (AR)
2.4. Subject Follow-Up
2.5. Statistical Analysis
3. Results
3.1. Participant Characteristics
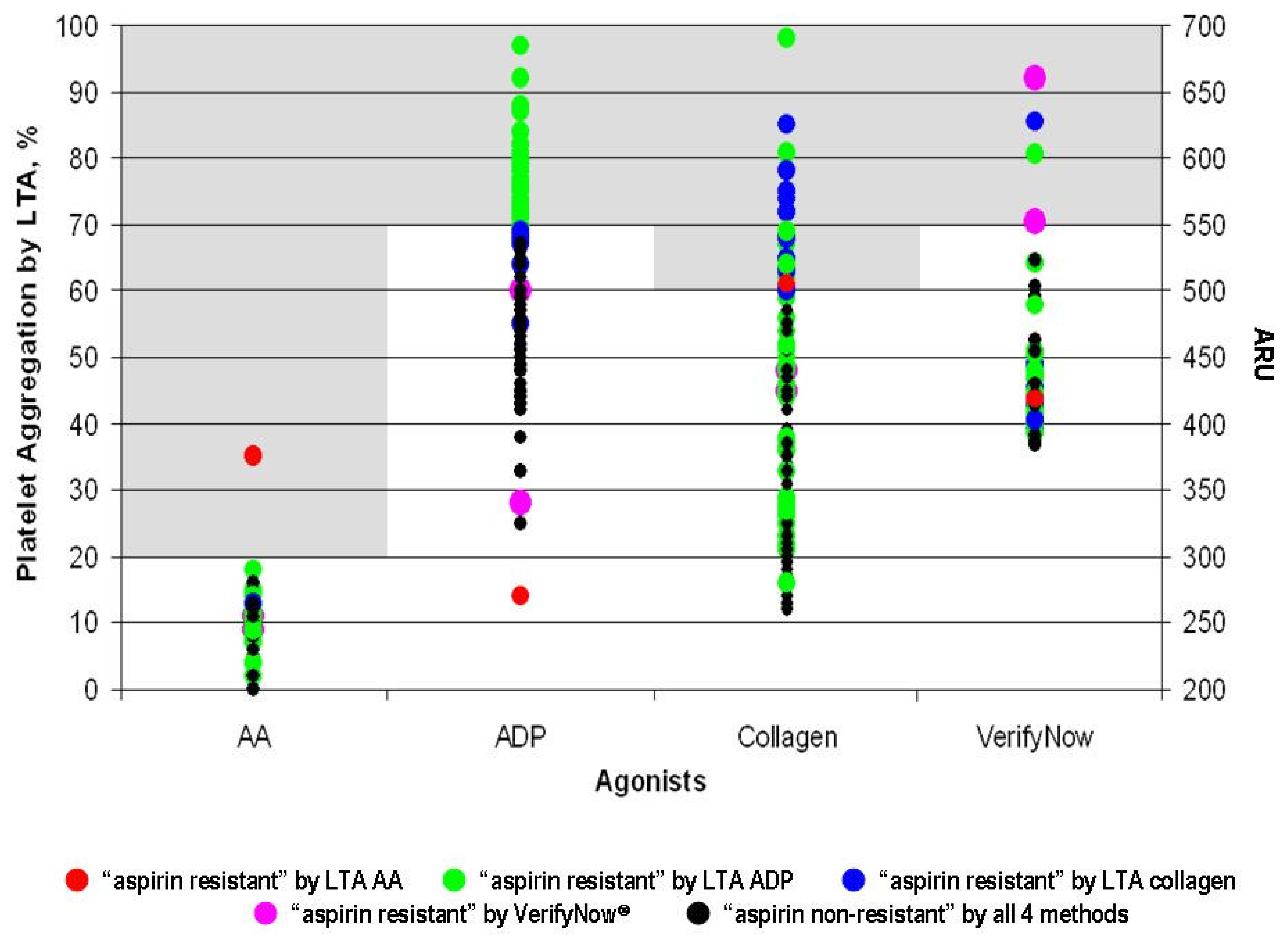
3.2. Aspirin Resistance
3.3. Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Niu, P.P.; Guo, Z.N.; Jin, H.; Xing, Y.Q.; Yang, Y. Antiplatelet regimens in the long-term secondary prevention of transient ischaemic attack and ischaemic stroke: An updated network meta-analysis. BMJ Open 2016, 6, e009013. [Google Scholar] [CrossRef] [PubMed]
- Del Giovane, C.; Boncoraglio, G.B.; Bertù, L.; Banzi, R.; Tramacere, I. Antiplatelet drugs for secondary prevention in patients with ischemic stroke or transient ischemic attack: A systematic review and network meta-analysis. BMC Neurol. 2021, 21, 319. [Google Scholar] [CrossRef] [PubMed]
- Greer, D.M. Aspirin and antiplatelet agent resistance: Implications for prevention of secondary stroke. CNS Drugs 2010, 24, 1027–1040. [Google Scholar] [CrossRef] [PubMed]
- Kuzniatsova, N.; Shantsila, E.; Blann, A.; Lip, G.Y. A contemporary viewpoint on ‘aspirin resistance’. Ann. Med. 2012, 44, 773–783. [Google Scholar] [CrossRef] [PubMed]
- Gorelick, P.B.; Farooq, M.U. Advances in Our Understanding of “Resistance” to Antiplatelet Agents for Prevention of Ischemic Stroke. Stroke Res. Treat. 2013, 2013, 727842. [Google Scholar] [CrossRef] [PubMed]
- Hankey, G.J.; Eikelboom, J.W. Aspirin resistance. Lancet 2006, 367, 606–617. [Google Scholar] [CrossRef]
- Sztriha, L.K.; Sas, K.; Vécsei, L. Aspirin resistance in stroke: 2004. J. Neurol. Sci. 2005, 229–230, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.T.; Thijs, V.; Murphy, S.J.X.; Fernandez-Cadenas, I.; Montaner, J.; Offiah, C.; Marquardt, L.; Kelly, P.J.; Bath, P.M.; Lim, S.-Y.; et al. Platelet function/reactivity testing and prediction of risk of recurrent vascular events and outcomes after TIA or ischaemic stroke: Systematic review and meta-analysis. J. Neurol. 2020, 267, 3021–3037. [Google Scholar] [CrossRef]
- Dretzke, J.; Riley, R.D.; Lordkipanidze, M.; Jowett, S.; O’Donnell, J.; Ensor, J.; Moloney, E.; Price, M.; Raichand, S.; Hodgkinson, J.; et al. The prognostic utility of tests of platelet function for the detection of ‘aspirin resistance’ in patients with established cardiovascular or cerebrovascular disease: A systematic review and economic evaluation. Health Technol. Assess. 2015, 19, 1–366. [Google Scholar] [CrossRef]
- Kleindorfer, D.O.; Towfighi, A.; Chaturvedi, S.; Cockroft, K.M.; Gutierrez, J.; Lombardi-Hill, D.; Kamel, H.; Kernan, W.N.; Kittner, S.J.; Leira, E.C.; et al. 2021 Guideline for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke 2021, 52, e364–e467. [Google Scholar] [CrossRef]
- Alberts, M.J. Platelet function testing for aspirin resistance is reasonable to do: Yes! Stroke 2010, 41, 2400–2401. [Google Scholar] [CrossRef] [Green Version]
- Adams, H.P., Jr.; Bendixen, B.H.; Kappelle, L.J.; Biller, J.; Love, B.B.; Gordon, D.L.; Marsh, E.E., 3rd. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 1993, 24, 35–41. [Google Scholar] [CrossRef] [Green Version]
- GUSTO Investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N. Engl. J. Med. 1993, 329, 673–682. [Google Scholar] [CrossRef] [Green Version]
- Lv, H.; Yang, Z.; Wu, H.; Liu, M.; Mao, X.; Liu, X.; Ding, H.; Shi, Z.; Zhou, Y.; Liu, Q.; et al. High On-Treatment Platelet Reactivity as Predictor of Long-term Clinical Outcomes in Stroke Patients with Antiplatelet Agents. Transl. Stroke Res. 2022, 13, 391–398. [Google Scholar] [CrossRef]
- Jing, Y.; Yue, X.; Yang, S.; Li, S. Association of Aspirin Resistance with Increased Mortality in Ischemic Stroke. J. Nutr. Heath Aging 2019, 23, 266–270. [Google Scholar] [CrossRef]
- Wang, C.-W.; Su, L.-L.; Hua, Q.-J.; He, Y.; Fan, Y.-N.; Xi, T.-T.; Yuan, B.; Liu, Y.-X.; Ji, S.-B. Aspirin resistance predicts unfavorable functional outcome in acute ischemic stroke patients. Brain Res. Bull. 2018, 142, 176–182. [Google Scholar] [CrossRef]
- Zhang, N.; Wang, Z.; Zhou, L. Aspirin resistance are associated with long-term recurrent stroke events after ischaemic stroke. Brain Res. Bull. 2017, 134, 205–210. [Google Scholar] [CrossRef]
- Yi, X.; Zhou, Q.; Lin, J.; Chi, L. Aspirin Resistance in Chinese Stroke Patients Increased the Rate of Recurrent Stroke and other Vascular Events. Int. J. Stroke 2013, 8, 535–539. [Google Scholar] [CrossRef]
- Patel, S.; Arya, V.; Saraf, A.; Bhargava, M.; Agrawal, C.S. Aspirin and Clopidogrel Resistance in Indian Patients with Ischemic Stroke and its Associations with Gene Polymorphisms: A Pilot Study. Ann. Indian Acad. Neurol. 2019, 22, 147–152. [Google Scholar] [CrossRef]
- Azmin, S.; Sahathevan, R.; Rabani, R.; Nafisah, W.Y.; Tan, H.J.; Raymond, A.A.; Hamidon, B.B.; Shamsu, A.S.; Norlinah, M.I. Biochemical aspirin resistance in stroke patients—A cross-sectional single centre study. EXCLI J. 2013, 12, 907–915. [Google Scholar] [CrossRef]
- Gan, R.; Teleg, R.A.; Florento, L.; Bitanga, E.S. Effect of increasing doses of aspirin on platelet aggregation among stroke patients. Cerebrovasc. Dis. 2002, 14, 252–255. [Google Scholar] [CrossRef]
- Tohgi, H.; Konno, S.; Tamura, K.; Kimura, B.; Kawano, K. Effects of low-to-high doses of aspirin on platelet aggregability and metabolites of thromboxane A2 and prostacyclin. Stroke 1992, 23, 1400–1403. [Google Scholar] [CrossRef] [Green Version]
- Venketasubramanian, N.; Pwee, K.H.; Chen, C.P.L. Singapore ministry of health clinical practice guidelines on stroke and transient ischemic attacks. Int. J. Stroke 2011, 6, 251–258. [Google Scholar] [CrossRef]
- Harrison, P.; Segal, H.; Blasbery, K.; Furtado, C.; Silver, L.; Rothwell, P.M. Screening for aspirin responsiveness after transient ischemic attack and stroke: Comparison of 2 point-of-care platelet function tests with optical aggregometry. Stroke 2005, 36, 1001–1005. [Google Scholar] [CrossRef] [Green Version]
- Dharmasaroja, P.A.; Sae-Lim, S. Comparison of aspirin response measured by urinary 11-dehydrothromboxane B2 and VerifyNow aspirin assay in patients with ischemic stroke. J. Stroke Cerebrovasc. Dis. 2014, 23, 953–957. [Google Scholar] [CrossRef]
- Shao, T.; Cheng, Y.; Jin, J.; Huang, L.; Yang, D.; Luo, C.; Han, Z.; Wang, Z.; Ge, W.; Xu, Y. A comparison of three platelet function tests in ischemic stroke patients with antiplatelet therapy. J. Clin. Neurosci. 2020, 78, 91–96. [Google Scholar] [CrossRef]
- Ma, L.; Chen, W.; Pan, Y.; Yan, H.; Li, H.; Meng, X.; Wang, Y.; Wang, Y. Comparison of VerifyNow, thromboelastography, and PL-12 in patients with minor ischemic stroke or transient ischemic attack. Aging 2021, 13, 8396–8407. [Google Scholar] [CrossRef]
- Lordkipanidze, M.; Pharand, C.; Schampaert, E.; Turgeon, J.; Palisaitis, D.A.; Diodati, J.G. A comparison of six major platelet function tests to determine the prevalence of aspirin resistance in patients with stable coronary artery disease. Eur. Heart J. 2007, 28, 1702–1708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hankey, G.J.; Eikelboom, J.W. Aspirin resistance. BMJ 2004, 328, 477–479. [Google Scholar] [CrossRef] [PubMed]
- Jefferson, B.K.; Foster, J.; McCarthy, J.J.; Ginsburg, G.; Parker, A.; Kottke-Marchant, K.; Topol, E. Aspirin resistance and a single gene. Am. J. Cardiol. 2005, 95, 805–808. [Google Scholar] [CrossRef] [PubMed]
- Altman, R.; Scazziota, A.; Funes, J.C. Why single daily dose of aspirin may not prevent platelet aggregation. Thromb. Res. 1988, 51, 259–266. [Google Scholar] [CrossRef]
- Bongiovanni, D.; Han, J.; Klug, M.; Kirmes, K.; Viggiani, G.; von Scheidt, M.; Schreiner, N.; Condorelli, G.; Laugwitz, K.-L.; Bernlochner, I. Role of Reticulated Platelets in Cardiovascular Disease. Arterioscler. Thromb. Vasc. Biol. 2022, 42, 527–539. [Google Scholar] [CrossRef]
- Mainoli, B.; Duarte, G.S.; Costa, J.; Ferreira, J.; Caldeira, D. Once- versus Twice-Daily Aspirin in Patients at High Risk of Thrombotic Events: Systematic Review and Meta-Analysis. Am. J. Cardiovasc. Drugs 2021, 21, 63–71. [Google Scholar] [CrossRef]
- Helgason, C.M.; Bolin, K.M.; Hoff, J.A.; Winkler, S.R.; Mangat, A.; Tortorice, K.L.; Brace, L.D. Development of aspirin resistance in persons with previous ischemic stroke. Stroke 1994, 25, 2331–2336. [Google Scholar] [CrossRef] [Green Version]
- Pulcinelli, F.M.; Pignatelli, P.; Celestini, A.; Riondino, S.; Gazzaniga, P.P.; Violi, F. Inhibition of platelet aggregation by aspirin progressively decreases in long-term treated patients. J. Am. Coll. Cardiol. 2004, 43, 979–984. [Google Scholar] [CrossRef] [Green Version]

| First Stroke (F) (n = 61) | Recurrent Stroke (R) (n = 52) | Control (C) (n = 30) | p-Value | |||
|---|---|---|---|---|---|---|
| Age, mean ± SD (years) * | 64 ± 8 | 67 ± 8 | 57 ± 4 | F vs. R 0.18 | F vs. C 0.0004 | R vs. C <0.0001 |
| Female, n (%) | 31 (51%) | 22 (42%) | 15 (50%) | 0.37 | 0.94 | 0.50 |
| Ethnicity, n (%) | ||||||
| Chinese | 54 (89%) | 43 (83%) | 30 (100%) | 0.38 | 0.05 | 0.02 |
| Malay | 3 (5%) | 8 (15%) | 0 (0%) | 0.06 | 0.55 | 0.02 |
| Indian | 4 (7 %) | 0 (0%) | 0 (0%) | 0.06 | 0.15 | 1 |
| Other | 0 (0%) | 1 (2%) | 0 (0%) | 1 | 1 | 1 |
| Risk factors, n (%) | ||||||
| No risk factor | 0 (0%) | 0 (0%) | 10 (33%) | 1 | <0.0001 | <0.0001 |
| Hypertension | 45 (74%) | 44 (85%) | 11 (37%) | 0.16 | 0.0006 | <0.0001 |
| Diabetes mellitus | 31 (51%) | 32 (62%) | 8 (27%) | 0.25 | 0.03 | 0.002 |
| Hyperlipidemia | 56 (92%) | 47 (90%) | 11 (37%) | 0.79 | <0.0001 | <0.0001 |
| Coronary artery disease | 2 (3%) | 4 (8%) | 0 (0%) | 0.30 | 0.55 | 0.12 |
| Smoking | 6 (10%) | 8 (15%) | 2 (7%) | 0.37 | 0.62 | 0.25 |
| Alcohol | 0 (0%) | 0 (0%) | 2 (7%) | 1 | 0.11 | 0.13 |
| Stroke subtype, n (%) ** | ||||||
| Atherosclerotic (extracranial) | 6 (10%) | 5 (10%) | n/a | 0.97 | ||
| Atherosclerotic (intracranial) | 14 (23%) | 33 (63%) | n/a | <0.001 | ||
| Lacunar/small vessel disease | 32 (52%) | 13 (25%) | n/a | 0.003 | ||
| Cryptogenic | 9 (15%) | 1 (2%) | n/a | 0.02 | ||
| Concomitant medications, n (%) | ||||||
| Blood pressure lowering | 26 (43%) | 24 (46%) | 11 (37%) | 0.71 | 0.59 | 0.41 |
| Lipid lowering | 56 (92%) | 49 (94%) | 10 (33%) | 0.62 | <0.0001 | <0.0001 |
| Hypoglycemic | 26 (43%) | 25 (48%) | 6 (20%) | 0.56 | 0.03 | 0.01 |
| Supplements in past 2 weeks, n (%) | ||||||
| Glucosamine tablets | 1 (2%) | 1 (2%) | 3 (10%) | 1 | 0.07 | 0.10 |
| Calcium tablets | 0 (0%) | 0 (0%) | 5 (17%) | 1 | 0.001 | 0.002 |
| Red wine | 0 (0%) | 1 (2%) | 8 (27%) | 1 | <0.0001 | 0.0006 |
| Grape juice | 0 (0%) | 1 (2%) | 2 (7%) | 1 | 0.11 | 0.27 |
| Vitamin E | 1 (2%) | 0 (0%) | 4 (13%) | 1 | 0.02 | 0.007 |
| Gingko | 1 (2%) | 1 (2%) | 3 (10%) | 1 | 0.07 | 0.10 |
| Ginseng | 4 (7%) | 1 (2%) | 2 (7%) | 0.23 | 0.98 | 0.27 |
| Garlic tablets | 3 (5%) | 0 (0%) | 2 (7%) | 0.11 | 0.73 | 0.13 |
| Traditional Chinese medicine | 6 (10%) | 6 (12%) | 2 (7%) | 0.77 | 0.62 | 0.13 |
| Laboratory Test | Post-Stroke Patients | Control (n = 30) | ||
|---|---|---|---|---|
| All (n = 113) | First (n = 61) | Recurrent (n = 52) | ||
| Light transmission aggregometry | n = 113 | n = 61 | n = 52 | n = 30 |
| Arachidonic acid 0.5 mM | ||||
| Mean ± SD, % | 12 ± 4 | 10 ± 3 | 13 ± 4 | 91 ± 6 |
| ≥20% aggregation *, n (%) | 1 (1%) | 0 (0%) | 1 (2%) | 30 (100%) |
| ADP 10 µM | ||||
| Mean ± SD, % | 62 ± 15 | 62 ± 18 | 63 ± 11 | 83 ± 12 |
| ≥70% aggregation *, n (%) | 36 (32%) | 24 (39%) | 12 (23%) | 26 (87%) |
| Collagen 2 ug/ml | ||||
| Mean ± SD, % | 41 ± 19 | 38 ± 19 | 44 ± 18 | 88 ± 8 |
| ≥60% aggregation *, n (%) | 22 (19%) | 9 (15%) | 13 (25%) | 30 (100%) |
| VerifyNow® | n = 112 | n = 61 | n = 51 | n = 30 |
| Mean ± SD, ARU | 426 ± 45 | 427 ± 54 | 425 ± 30 | 637 ± 29 |
| ≥550 ARU *, n (%) | 4 (4%) | 4 (7%) | 0 (0%) | 30 (100%) |
| Multiplate® | n = 113 | n = 61 | n = 52 | n = 30 |
| ASPItest, Mean ± SD, AUC | 97 ± 76 | 96 ± 82 | 98 ± 70 | 369 ± 153 |
| ADPtest, Mean ± SD, AUC | 337 ± 150 | 348 ± 164 | 325 ± 132 | 339 ± 128 |
| COLtest, Mean ± SD, AUC | 192 ± 105 | 215 ± 114 | 164 ± 87 | 455 ± 130 |
| Study ID No. | Outcome | Days from Index Stroke to Outcome | Platelet Aggregation Test | |||
|---|---|---|---|---|---|---|
| LTA AA (%) | LTA ADP (%) | LTA Collagen (%) | VerifyNow® (ARU) | |||
| 33 | Death | 260 | 15 | 50 | 21 | 427 |
| 44 | Heart attack | 1068 | 15 | 97 * | 50 | 412 |
| 61 | Recurrent stroke | 837 | 9 | 74 * | 26 | 422 |
| 99 | Amputation | 738 | 7 | 92 * | 64 * | 421 |
| 103 | Recurrent stroke | 44 | 12 | 75 * | 22 | 405 |
| 111 | Death | 355 | 15 | 58 | 21 | 504 |
| 116 | Recurrent stroke | 611 | 14 | 71 * | 45 | 440 |
| 129 | Death | 484 | 9 | 77 * | 69 * | 489 |
| 135 | Heart attack | 71 | 16 | 57 | 12 | 419 |
| 145 | Recurrent stroke | 155 | 11 | 62 | 31 | 414 |
| Mean ± SD | 462 ± 347 | 12 ± 3 | 71 ± 15 | 36 ± 20 | 435 ± 34 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Venketasubramanian, N.; Agustin, S.J.; Padilla, J.L.; Yumul, M.P.; Sum, C.; Lee, S.H.; Ponnudurai, K.; Gan, R.N. Comparison of Different Laboratory Tests to Identify “Aspirin Resistance” and Risk of Vascular Events among Ischaemic Stroke Patients: A Double-Blind Study. J. Cardiovasc. Dev. Dis. 2022, 9, 156. https://doi.org/10.3390/jcdd9050156
Venketasubramanian N, Agustin SJ, Padilla JL, Yumul MP, Sum C, Lee SH, Ponnudurai K, Gan RN. Comparison of Different Laboratory Tests to Identify “Aspirin Resistance” and Risk of Vascular Events among Ischaemic Stroke Patients: A Double-Blind Study. Journal of Cardiovascular Development and Disease. 2022; 9(5):156. https://doi.org/10.3390/jcdd9050156
Chicago/Turabian StyleVenketasubramanian, Narayanaswamy, Sherwin Joy Agustin, Jorge L. Padilla, Maricar P. Yumul, Christina Sum, Sze Haur Lee, Kuperan Ponnudurai, and Robert N. Gan. 2022. "Comparison of Different Laboratory Tests to Identify “Aspirin Resistance” and Risk of Vascular Events among Ischaemic Stroke Patients: A Double-Blind Study" Journal of Cardiovascular Development and Disease 9, no. 5: 156. https://doi.org/10.3390/jcdd9050156
APA StyleVenketasubramanian, N., Agustin, S. J., Padilla, J. L., Yumul, M. P., Sum, C., Lee, S. H., Ponnudurai, K., & Gan, R. N. (2022). Comparison of Different Laboratory Tests to Identify “Aspirin Resistance” and Risk of Vascular Events among Ischaemic Stroke Patients: A Double-Blind Study. Journal of Cardiovascular Development and Disease, 9(5), 156. https://doi.org/10.3390/jcdd9050156







