1. Introduction
Clozapine is the most effective antipsychotic for treatment-resistant schizophrenia [
1]. It is, however, associated with many peripheral adverse drug reactions (ADRs), including cardiac (myocarditis, cardiomyopathy and postural hypotension), metabolic (metabolic syndrome, obesity and diabetes), hypersalivation and gastrointestinal (constipation and ileus) [
2,
3]. Nose-to-brain (N2B) drug delivery offers a promising approach to the delivery of antipsychotics to the central nervous system (CNS) in the management of schizophrenia. This route bypasses the blood–brain barrier (BBB) and hepatic first-pass metabolism, which may increase the CNS drug availability and reduce peripheral ADRs [
4]. In order to deliver therapeutic doses of clozapine to the olfactory region, the antipsychotic drug needs to penetrate the hydrophilic mucus layer, while avoiding mucin adsorption, before permeating the olfactory membrane [
5]. Due to the small volume of the nasal cavity, only small volumes (100–250 µL [
6]) of therapeutic doses can be administered intranasally. It is, therefore, crucial for the antipsychotic drug to be solubilized before administration in order to increase the transmucosal nasal absorption and avoid the rapid mucociliary clearance from the nasal cavity [
4].
Well-reported methods to enhance drug solubility include the use of surfactants and solubilizers [
7,
8,
9]. Polysorbates are hydrophilic, non-ionic surfactants that are frequently used as an emulsifying and solubilizing agent in foods, cosmetics and pharmaceutical formulations [
10]. Polysorbate 20 (PS20) and polysorbate 80 (PS80) are approved by the U.S. Food and Drug Administration (FDA) for intranasal administration, and are often used to solubilize hydrophobic drugs, such as clozapine. In recent years, poloxamer hydrogels have received interest as in situ drug delivery vehicles due to their thermoreversibility. Poloxamer 407 (P407) is among the most commonly used poloxamers, as it remains a solution at room temperature but forms an in situ gel at physiological temperatures and at low concentrations. It is a versatile excipient that is widely used in pharmaceutical formulations due to its low toxicity. Traditional surfactants have a low molecular weight, whereas P407 is made of triblock copolymers of poly(ethylene oxide)-
b-poly(propylene oxide)-
b-poly(ethylene oxide; PEO-PPO-PEO). The high hydrophobic PPO fraction of P407, along with the polymer molecular weight compared to other types of poloxamers, has the capacity to increase the drug loading of water-insoluble drugs through direct solubilization [
11].
Designing the most suitable sol–gel formulation for the intranasal delivery of clozapine involves balancing a variety of parameters, including the micellarized drug, particle size, lipophilicity, formulation pH and molecular interactions between the drug and other excipients. Herein, we report on the development of clozapine-encapsulated binary polysorbate/poloxamer mixed micelles formulated into a thermosensitive sol–gel, intended for N2B delivery to reduce peripheral ADRs, increase CNS drug bioavailability and improve patient compliance. Accordingly, the aim of the present study was to investigate the feasibility of the optimized formulations to transport clozapine across nasal mucosa tissues in a controlled manner for a sustained therapeutic effect.
3. Conclusions
The addition of PS20 or PS80 markedly improved the drug loading, micellar packing, increased stabilization and mechanical strength of the P407-based sol–gel formulations. Formulation F4 was found to be more elastic than F3 at the nasal temperature due to the higher synergism of binary PS80-P407 mixed micelles, producing more thermodynamically stable and rigid micellar sol–gels than PS20-P407. The variations in encapsulation, drug release and drug permeation recorded between F3 and F4 did not consider the particle size, PDI and zeta potential, as they were not significantly different. Using the Korsmeyer–Peppas model, our results showed a non-Fickian, anomalous behavior release of clozapine from the sol–gel at 34 °C, which involved a combination of mechanisms, including polymer swelling and drug diffusion. The permeation of clozapine in F3 through the nasal mucosa tissue was shown to be better, with more of the drug retained within the tissue post-administration of F4. Therefore, binary PS20-P407 mixed micelles in a sol–gel system may be a preferable carrier system for intranasal clozapine delivery to the brain compared to binary PS80-P407 mixed micelles.
4. Materials and Methods
Clozapine (>98% purity) was purchased from Adooq Bioscience (Irvine, CA, USA). P407, hydroxypropyl methyl cellulose (HPMC E4M) and glycerin were purchased from Sigma-Aldrich (Castle Hill, NSW, Australia). PS20, PS80 and carbopol 934 NF were purchased from PCCA (Matraville, NSW, Australia). Hydrochloric acid (HCl), sodium hydroxide (NaOH), potassium chloride (KCl), calcium chloride dihydrate (CaCl2·2H2O), sodium chloride (NaCl) and methanol were of analytical grade and purchased from Sigma-Aldrich (Castle Hill, NSW, Australia). Orthophosphoric acid was purchased from Thermo Fisher Scientific (Brisbane, QLD, Australia) and potassium dihydrogen orthophosphate anhydrous was purchased from Chem-Supply (Gillman, SA, Australia). Milli-Q water was used as a formulation vehicle.
4.1. Sol–Gel Preparation
The sol–gels were prepared using the cold method [
43] as described by Pandey et al. [
44] with slight modifications. Briefly, 15.5%
w/
w P407 and 0.5%
w/
w HPMC were dry mixed before sufficient volume of Milli-Q water was added to hydrate the mixture. Separately, a stock solution of 1%
v/
v carbopol in Milli-Q water was prepared. Then, 3%
w/
w glycerin and 0.1%
w/
w of the carbopol solution were added to the mixture, and stirred thoroughly (400 rpm) for 6 h at 2–8 °C. At the same time, 0.1%
w/
w clozapine was stirred in 1%, 3% or 5%
w/
w PS20 or PS80 at room temperature before being mixed with the polymer solution, and the final weight of the formulation was made up to 10 g with Milli-Q water and stirred thoroughly (400 rpm) overnight at 2–8 °C. The final sol–gel mixture was adjusted to pH 5.5 ± 0.2 with 0.1 M HCl or 0.1 N NaOH.
4.2. Determination of Clozapine Saturation Solubility in ‘Sol’ form of 15.5% w/w P407
An excess amount of clozapine was added to 15.5%
w/
w P407 and stirred overnight (400 rpm) at 2–8 °C. Samples were centrifuged at 12,000 rpm at 4 °C for 45 min using a refrigerated centrifuge (Eppendorf Centrifuge 5804 R, Hamburg, Germany). The supernatant liquid was collected and filtered using a 0.45 µm, 25 mm PTFE Syringe Membrane Filter (PhaseSep Pty Ltd., Doncaster East, VIC, Australia), and the concentration of clozapine was measured using HPLC [
45,
46].
4.3. Preparation of Simulated Nasal Fluid (SNF)
SNF was prepared by dissolving KCl 1.29 mg/mL, NaCl 7.45 mg/mL and CaCl
2·2H
2O 0.32 mg/mL with Milli-Q water, and was adjusted to pH 5.5 ± 0.1 with 0.1 M HCl and 0.1 N NaOH [
47,
48].
4.4. Rheology Studies
Rheological evaluations of all sol–gel formulations were performed using a Discovery Hybrid Rheometer HR-3 (TA Instruments, New Castle, DE, USA) with a 40 mm parallel plate geometry and a sample gap of 200 μm. The gelation temperature (Tsol/gel), G’ modulus, G’’ modulus and loss tangent (tan δ) of the sol–gels were evaluated using oscillatory measurements, with a temperature ramp between 8 °C to 40 °C and ramp rate of 5 °C/min at 1.0 Pa (stress) and 1.0 Hz (frequency). The dynamic viscosity of the sol–gels was measured using flow measurements, with a temperature ramp between 8 °C to 40 °C and ramp rate of 5 °C/min at 2.0 rad/s (angular velocity). The flow behavior of the sol–gels was evaluated at 4 °C (storage temperature) and 34 °C (nasal temperature), with a flow ramp between 10 s−1 to 1000 s−1. The strength of the gels at nasal temperature was recorded using the G’ modulus as a measurement of stiffness. All measurements were carried out in triplicate and the resultant curves were generated directly from the manufacturer’s computer TRIOS software (TA Instruments, New Castle, DE, USA).
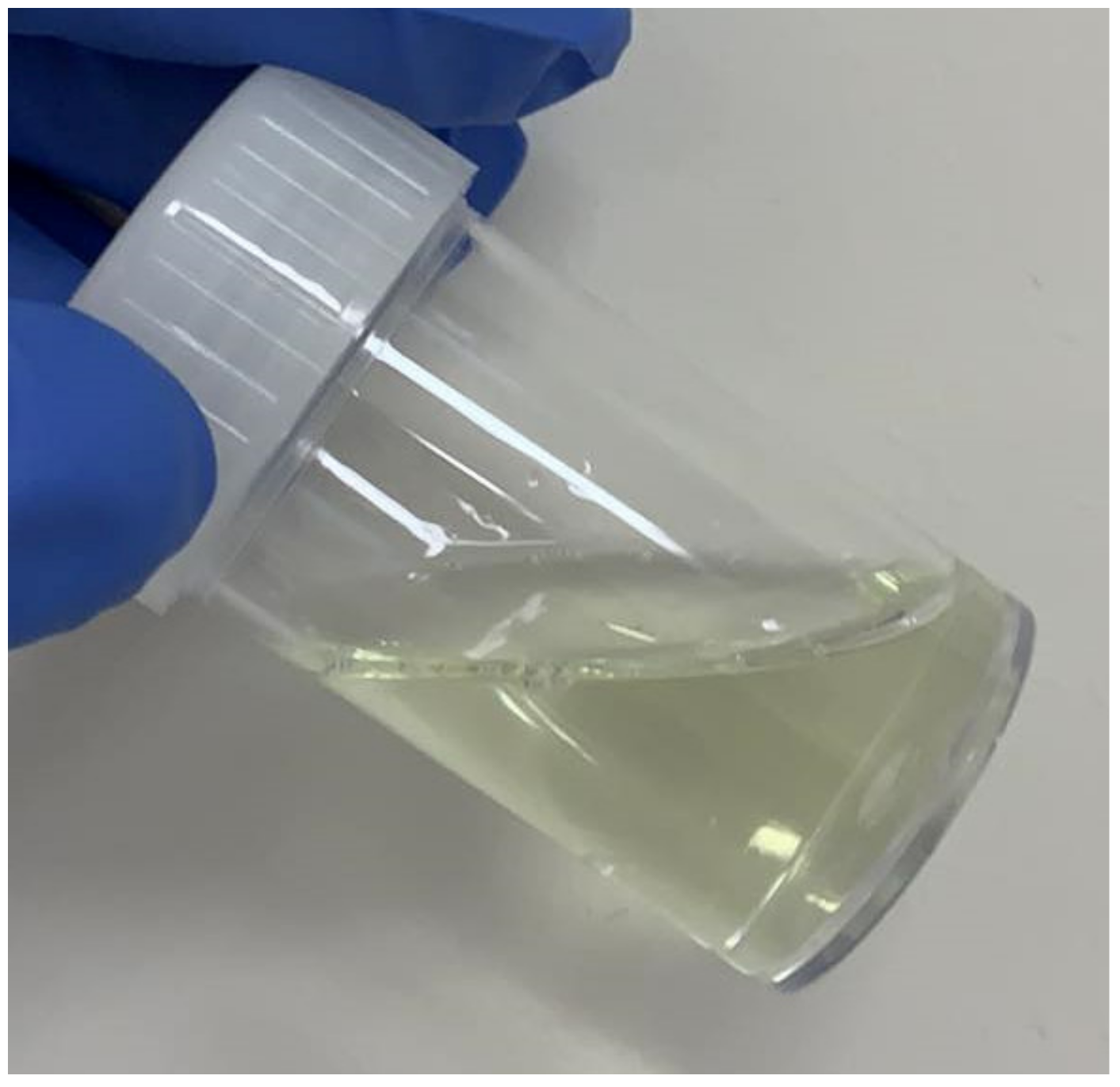
4.5. Determination of Turbidity
The turbidity of the sol–gels when in liquid form was performed using a Hach TU5200 EPA Turbidimeter (Hach Company, Loveland, COL, USA) measuring in nephelometric turbidity units (NTU) with a Class 2 laser product and 650 nm (EPA 0.43 mW) optical light source. The sol–gels were left at room temperature and any air bubbles were removed before evaluation. The scattered light was collected at a 90° angle to the incident light and 360° around the sample vial. The turbidity sensor was calibrated using three Stablcal® turbidity standards (10, 20, 600 NTU). The relative clarity of the sol–gels was measured in triplicate.
4.6. Particle Size, PDI and Zeta Potential
The hydrodynamic particle diameter, PDI, and zeta potential of clozapine in the binary polysorbate/poloxamer mixed micelles were measured using dynamic light scattering (DLS) with Zetasizer Nano ZS (Malvern Instruments, Malvern, UK). Diluted samples (1:10) were pipetted into disposable cuvettes for particle size and PDI measurements, and disposable DTS1070 folded zeta cells (Malvern Instruments, Malvern, UK) for zeta potential measurements. The detection scattering angle was set at 173° (25 °C) with equilibration time at 60 s. Measurements were carried out in triplicate and recorded as the mean ± SD of three independent runs.
4.7. High Performance Liquid Chromatography (HPLC) Analysis and Quantitation of Clozapine
The concentration of clozapine was analyzed using a RP-HPLC equipment (Shimadzu Nexera-i LC-2040C, Kyoto, Japan) equipped with a low pressure quaternary gradient pump, along with a dual wavelength UV detector (at 234 nm), auto sampler (10 μL injection volume) and column oven (maintained at 25 °C). The chromatographic data were processed using LC solution 1.24 SP1 software. The quantification analysis was performed under isocratic conditions with a C18 column (Phenomenex Gemini C18 150 × 2 mm, 3 μm). The mobile phase consisted of methanol and phosphate buffer (3.4 mM potassium dihydrogen orthophosphate buffer, pH 2.0 adjusted with 10% v/v o-phosphoric acid) in the ratio of 65:35 (v/v). The flow rate was 0.2 mL/min and the retention time of clozapine was found to be 3.3 min. The concentration of clozapine was calculated using a standard calibration curve (R2: 0.9998) over the concentration range of 1–50 μg/mL. The lower limit of detection (LOD) was 0.03 μg/mL and the lower limit of quantification (LOQ) was 0.1 μg/mL.
4.8. Differential Scanning Calorimetry (DSC) and Thermogravimetric Analysis (TGA)
The sol–gels were frozen with liquid nitrogen for an hour and then lyophilized using a VirTis BenchTop Pro with Omnitronics™ freeze dryer (SP Industries, Warminster, PA, USA) at −102 °C (50 Hz) and ≤20 mT for 24 h. The powdered sol–gels of approximately 4–5 mg were transferred into aluminum crucibles and the thermal analysis of the sol–gels was carried out using a Mettler Toledo TGA/DSC 2 equipment (Mettler Toledo, Columbus, OH, USA). Heating runs were performed under compressed air, with a heating rate of 10 °C/min over 25–600 °C (49). STARe software was used to generate the thermal curves by measuring heat output (DSC) and mass loss (TGA) as temperature is increased.
4.9. X-ray Power Diffraction (XRD) Analysis
X-ray diffraction was carried out to identify phases in the powdered sample, with data collected using a Bruker D8 Advance MKII XRD X-ray diffractometer (Bruker, Billerica, MA, USA) equipped with a Cu source, a LynxEye detector and operated at 40 kV and 40 mA. Diffraction patterns were recorded by continuous scans from 5 to 45° 2Ɵ, with a step size of 0.04° and 15 rpm rotation at a scan rate of 0.4° s per step. The resulting patterns were imported into Diffrac EVA version 5.1, where phases were identified using the PDF-4 2020 ICDD database [
49].
4.10. In Vitro Drug Release Study
In vitro drug release studies were performed using a Logan DHC-6T vertical Franz diffusion apparatus (Logan instruments, Somerset, NJ, USA). Clozapine solution (0.1% w/w) was used as control, prepared in 1 mL 0.1 M HCl and made up to 10 g with Milli-Q water (adjusted to pH 5.5 with 0.1 N NaOH). The donor compartment was filled with 1.5 mL of the optimized sol–gel or clozapine solution, and the receiver compartment was filled with 12 mL of SNF. Snake skin dialysis membranes (Thermo Fisher Scientific, Brisbane, QLD, Australia) with a 3.5 kDa MWCO were soaked in SNF for 15 min prior to experimentation. Membranes having effective areas of 1.5 × 1.5 cm2 exposed to the test formulations/solutions were then mounted between the donor cap and receiver body. The temperature of the chamber was kept at 34 ± 1 °C with standard stirring speed. Samples of 0.5 mL were collected from the receiver compartment at 0, 0.5, 1, 2, 4, 8, 12, 24, 48 and 72 h, and replaced with fresh SNF of equal volume after each sampling. The samples were placed in a −80 °C refrigerator until analysis using HPLC. The release study experiments were performed in triplicate.
4.11. Ex Vivo Drug Permeation Study
Ex vivo drug permeation of the optimized sol–gels was carried out using Franz diffusion apparatus using excised sheep nasal mucosal tissues [
31,
50], which were obtained from The University of Queensland (UQ)’s School of Veterinary Science (Gatton, QLD, Australia) following a process supervised by veterinary officials in accordance with the Ethics Committee of Animal Experimentation at UQ (Ethics Approval No. 2021/AE000143). The mucosal specimens, with effective surface area of 1.5 × 1.5 cm
2, were mounted onto the Franz diffusion apparatus, with the mucosal surface facing the donor compartment and serosal side facing the receptor compartment. The donor compartment was filled with 500 μL of the optimized sol–gels or clozapine solution (as described above), and the receiver compartment was filled with 12 mL of SNF to ensure sink conditions. The temperature of the chamber was kept at 34 ± 1 °C with standard stirring speed. The tissues were allowed to stabilize for 30 min prior to loading of the optimized sol–gels. Sample aliquots of 0.5 mL were collected from the receiver compartment at 0, 1, 2, 4, 6, 8 h and replaced with fresh SNF of equal volume after each sampling. The samples were placed in a −80 °C refrigerator until analysis using HPLC. The experiments were carried out in triplicate and the data were fitted into Fick’s second law of diffusion equation to determine the permeability parameters of clozapine in the sol–gels across the sheep nasal mucosa, where C
t is the cumulative drug permeated at time
t,
Cd is concentration of clozapine in the donor chamber (0.5 mg),
K is the partition coefficient (log P) of clozapine,
L is the diffusion path length and
D is the diffusion constant, which was calculated using Equation (3) [
31,
51].
The apparent permeability coefficient,
Papp, was calculated using Equation (4), and the steady state flux,
Jss, was calculated using Equation (5), where
S represents the cross-sectional area of flow.
4.12. Mathematical Modelling of In Vitro and Ex Vivo Drug Release Kinetics
The in vitro and ex vivo drug release data were fitted to mathematical models, including zero-order, first-order, Hixson–Crowell and Korsmeyer–Peppas, to predict the kinetics and release mechanism of clozapine from the sol–gel polymer matrix [
30]. For zero-order kinetics, the release of clozapine can be described using Equation (6), where
C0 is the initial concentration of clozapine released (usually,
C0 = 0) and
K0 is the zero-order constant.
For first-order kinetics, Equation (7) was used to describe the release of clozapine from the polymer gel matrix, where
K1 is the first-order constant.
Equation (8) illustrates the release of clozapine using the Hixson–Crowell model, where
KHC is the Hixson–Crowell constant.
For Korsmeyer–Peppas kinetics, drug release can be described using Equation (9), where
F represents the fraction of drug released at time
t,
Mt is the amount of drug released at time
t,
M∞ is the amount of drug released at infinity,
Km is the Korsmeyer–Peppas constant and
n is the diffusion or release component [
31]. In this model, if
n = 0.5 (Fickian Case I), the drug release is driven by diffusion, and when
n = 1 (non-Fickian Case II), the drug release is governed by polymer swelling or relaxation of polymeric chains. When 0.5 <
n < 1 (non-Fickian anomalous), the drug release process is indicated by both diffusion and swelling of the polymer matrix. If
n > 1 (non-Fickian Super Case II), the drug release is said to be due to the tension and breaking of the polymer [
30].
The obtained regression (R2) values were used to verify the release of clozapine from the sol–gel formulations, and the highest correlation coefficient was considered to be the best model.
4.13. Nasal Mucosal Tissue Deposition of Optimized Sol–Gels
The mucosal tissues were then collected at 2, 4, 6 and 8 h following exposure of the optimized sol–gels or control solution. The collected tissues were washed with Milli-Q water, blotted with filter paper, wrapped in aluminum foil and stored at −80 °C until analysis. On the day of analysis, the tissues were thawed and dried with filter paper. They were then frozen with liquid nitrogen and grinded using a mortar and pestle. Acetonitrile was added to the powdered tissues to make 100 mg/mL of tissue homogenate. The samples were vortexed for 10 s and centrifuged at 10,000 rpm for 5 min. The supernatant was collected for HPLC analysis to determine the concentration of clozapine deposited in the nasal tissues [
44].
4.14. Drug Stability Study
The optimized sol–gel formulations were subjected to drug stability study for a period of three months at low temperature (2–8 °C), room temperature (25 °C) and elevated temperature (40 °C). Phase separation was determined after refrigerated centrifugation (12,000 rpm for 30 min at 4 °C) at one, two and three months for each temperature to observe for time-dependent changes in drug content [
30,
52].
4.15. Data Analysis
The data analysis was measured using t-test to determine statistical differences between individual means. In all analyses, a two-tailed p-value < 0.05 denotes significance. All analyses were performed using GraphPad Prism v9.