Fabrication of Ethosomes Containing Tocopherol Acetate to Enhance Transdermal Permeation: In Vitro and Ex Vivo Characterizations
Abstract
:1. Introduction
2. Materials and Methods
2.1. Reagents
2.2. Instruments
2.3. Preparation of Ethosomal NPs
2.4. Preparation of Ethosomal Gels
2.5. Physicochemical Characterizations of Ethosomal Dispersions
2.5.1. Zeta Potential (ZP) and Particle Size (PS)
2.5.2. Drug Entrapment Efficiency (% EE)
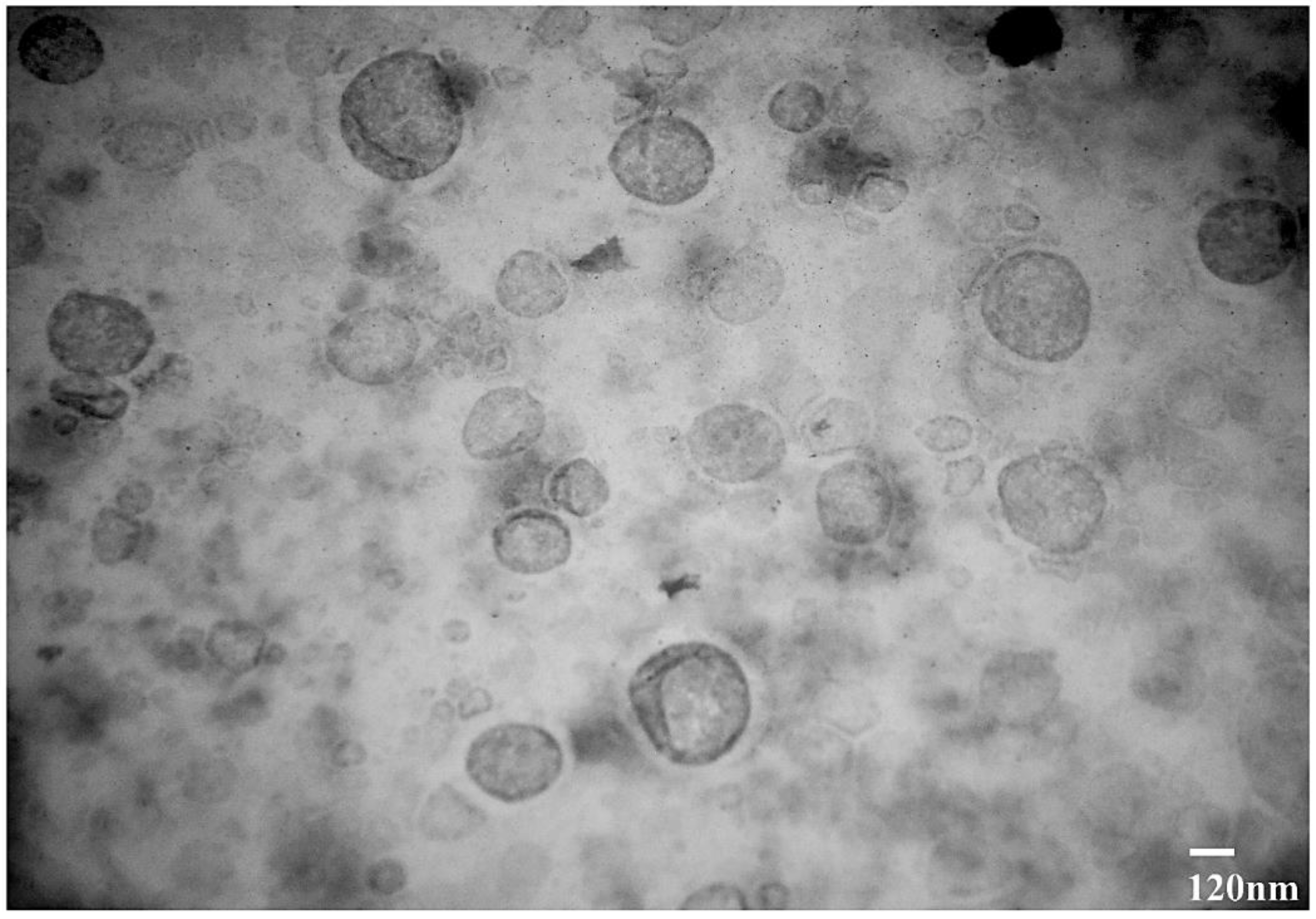
2.5.3. Transmission Electron Microscopy (TEM)
2.5.4. Organoleptic, PH, Conductivity, and Spreadability Assessments
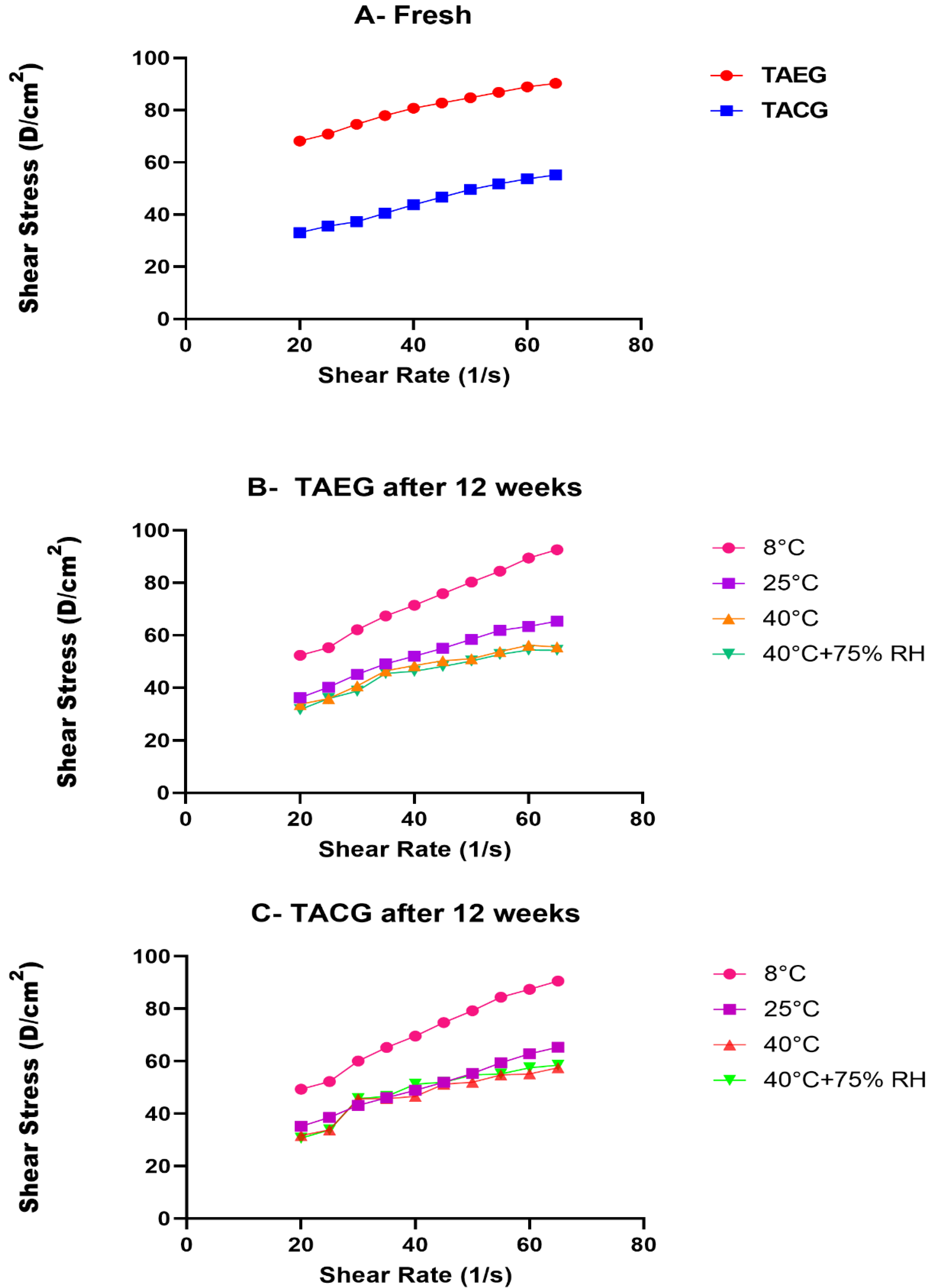
2.5.5. Rheological Analysis
2.6. Ex Vivo Permeation Studies
2.7. Statistical Analysis
3. Results and Discussion
3.1. Fabrication and Optimization of TAEG Formulations
3.2. Physicochemical Characterizations of TA-Loaded Ethosomes
3.2.1. TEM Analysis
3.2.2. PS Analysis
3.2.3. PDI Analysis
3.2.4. ZP Analysis
| # | Formulation Code | Ethanol (%) | Phospholipid (%) | PS (nm) | PDI | ZP (mV) |
|---|---|---|---|---|---|---|
| 1 | TA-1 | 25 | 5 | 235 | 0.475 | −18.9 |
| 2 | TA-2 | 25 | 2.5 | 159 | 0.377 | −21.7 |
| 3 | TA-3 | 25 | 0.5 | 144.4 | 0.312 | −19.2 |
| 4 | TA-4 | 30 | 5 | 289 | 0.389 | −20.6 |
| 5 | TA-5 | 30 | 2.5 | 200.6 | 0.465 | −18.6 |
| 6 | TA-6 | 30 | 0.5 | 156 | 0.277 | −16.8 |
| 7 | TA-7 | 40 | 5 | 231.2 | 0.361 | −28.4 |
| 8 | TA-8 | 40 | 2.5 | 207.6 | 0.348 | −20.3 |
| 9 | TA-9 | 40 | 0.5 | 153.7 | 0.214 | −17.9 |
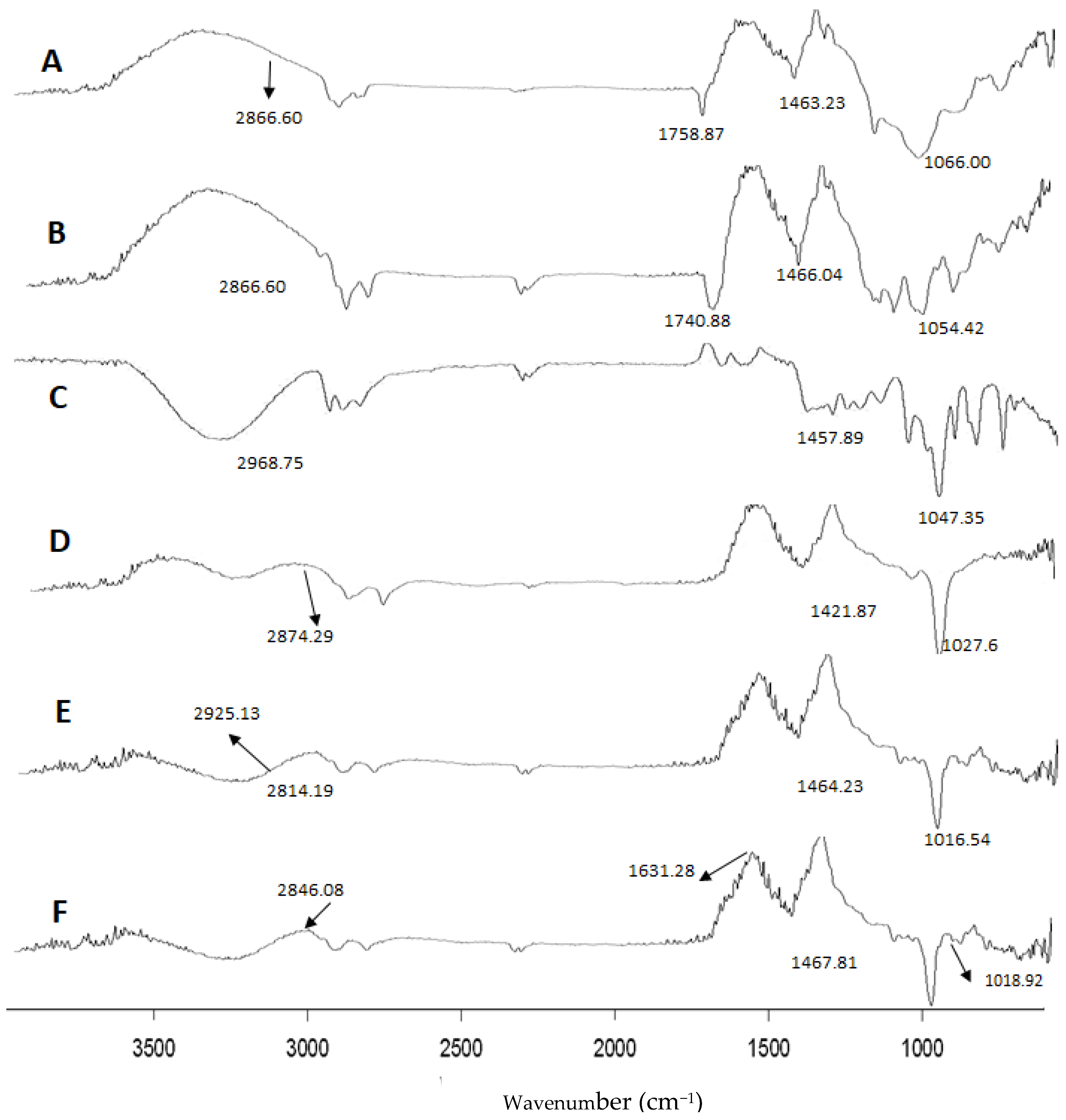
3.2.5. FT-IR Analysis
3.2.6. Thermostability, and Organoleptic Analysis
3.2.7. pH, Conductivity, and Viscosity Analyses
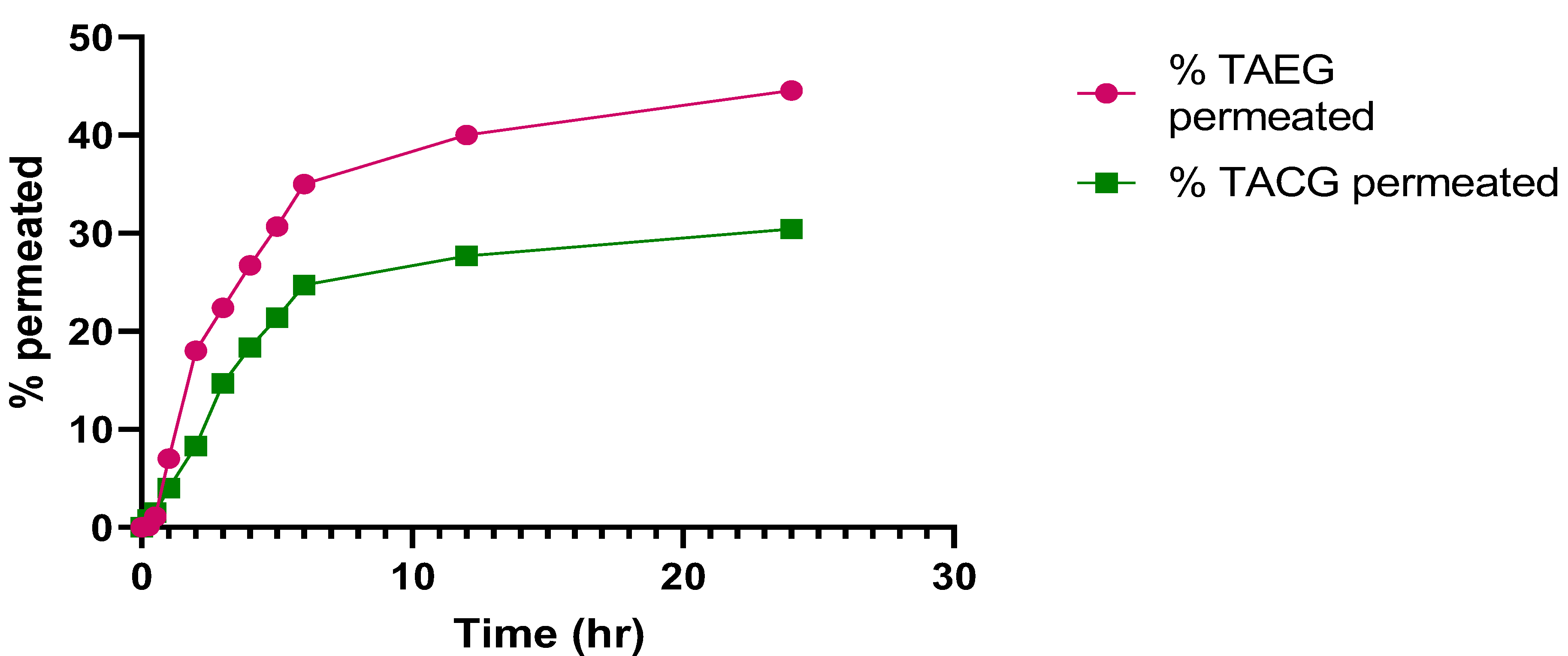
3.3. Ex Vivo Permeation Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Khan, M.K.; Khan, B.A.; Uzair, B.; Niaz, S.I.; Khan, H.; Hosny, K.M.; Menaa, F. Development of Chitosan-Based Nanoemulsion Gel Containing Microbial Secondary Metabolite with Effective Antifungal Activity: In vitro and in vivo Characterizations. Int. J. Nanomed. 2021, 16, 8203. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.A.; Mahmood, T.; Menaa, F.; Shahzad, Y.; Yousaf, A.M.; Hussain, T.; Ray, S.D. New Perspectives on the Efficacy of Gallic Acid in Cosmetics and Nanocosmeceuticals. Curr. Pharm. Des. 2018, 24, 5181–5187. [Google Scholar] [CrossRef] [PubMed]
- Khan, B.A.; Akhtar, N.; Menaa, A.; Menaa, F. A novel Cassia fistula (L.)-based emulsion elicits skin anti-aging benefits in humans. Cosmetics 2015, 2, 368–383. [Google Scholar] [CrossRef] [Green Version]
- Koufaki, M. Vitamin E derivatives: A patent review (2010–2015). Expert Opin. Ther. Pat. 2016, 26, 35–47. [Google Scholar] [CrossRef]
- Duhem, N.; Danhier, F.; Préat, V. Vitamin E-based nanomedicines for anti-cancer drug delivery. J. Control. Release 2014, 182, 33–44. [Google Scholar] [CrossRef]
- Brigelius-Flohé, R. Bioactivity of vitamin E. Nutr. Res. Rev. 2006, 19, 174–186. [Google Scholar] [CrossRef] [Green Version]
- Saez, V.; Souza, I.; Mansur, C. Lipid nanoparticles (SLN & NLC) for delivery of vitamin E: A comprehensive review. Int. J. Cosmet. Sci. 2018, 40, 103–116. [Google Scholar]
- Chen, W.; Barthelman, M.; Martinez, J.; Alberts, D.; Gensler, H.L. Inhibition of cyclobutane pyrimidine dimer formation in epidermal p53 gene of UV-irradiated mice by α-tocopherol. Nutr. Cancer 1997, 29, 205–211. [Google Scholar] [CrossRef]
- Nada, A.H.; Zaghloul, A.A.; Hedaya, M.M.; Khattab, I.S. Development of novel formulations to enhance in vivo transdermal permeation of tocopherol. Acta Pharm. 2014, 64, 299–309. [Google Scholar] [CrossRef] [Green Version]
- McVean, M.; Liebler, D.C. Prevention of DNA photodamage by vitamin E compounds and sunscreens: Roles of ultraviolet absorbance and cellular uptake. Mol. Carcinog. Publ. Coop. Univ. Tex. MD Anderson Cancer Cent. 1999, 24, 169–176. [Google Scholar] [CrossRef]
- Lippman, S.M.; Klein, E.A.; Goodman, P.J.; Lucia, M.S.; Thompson, I.M.; Ford, L.G.; Parnes, H.L.; Minasian, L.M.; Gaziano, J.M.; Hartline, J.A. Effect of selenium and vitamin E on risk of prostate cancer and other cancers: The Selenium and Vitamin E Cancer Prevention Trial (select). JAMA 2009, 301, 39–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thiele, J.; Schroeter, C.; Hsieh, S.; Podda, M.; Packer, L. The antioxidant network of the stratum corneum. Curr. Probl. Dermatol. 2001, 29, 26–42. [Google Scholar] [PubMed]
- Ijaz, M.; Akhtar, N. Fatty acids based α-Tocopherol loaded nanostructured lipid carrier gel: In vitro and in vivo evaluation for moisturizing and anti-aging effects. J. Cosmet. Dermatol. 2020, 19, 3067–3076. [Google Scholar] [CrossRef] [PubMed]
- Fahr, A.; Liu, X. Drug delivery strategies for poorly water-soluble drugs. Expert Opin. Drug Deliv. 2007, 4, 403–416. [Google Scholar] [CrossRef]
- Mustacich, D.J.; Vo, A.T.; Elias, V.D.; Payne, K.; Sullivan, L.; Leonard, S.W.; Traber, M.G. Regulatory mechanisms to control tissue α-tocopherol. Free Radic. Biol. Med. 2007, 43, 610–618. [Google Scholar] [CrossRef] [Green Version]
- Niki, E. Antioxidant Defense Network and Vitamin E. In Vitamin E; RSC Publishing: London, UK, 2019; pp. 134–150. [Google Scholar]
- Rangarajan, M.; Zatz, J.L. Effect of formulation on the delivery and metabolism of a-tocopheryl acetate. J. Cosmet. Sci 2001, 52, 225–236. [Google Scholar]
- Menaa, F. When pharma meets nano or the emerging era of nanopharmaceuticals. Pharm. Anal. Acta 2013, 4, 223. [Google Scholar] [CrossRef] [Green Version]
- Jun-Bo, T.; Zhuang-Qun, Y.; Xi-Jing, H.; Ying, X.; Yong, S.; Zhe, X.; Tao, C. Effect of ethosomal minoxidil on dermal delivery and hair cycle of C57BL/6 mice. J. Dermatol. Sci. 2007, 45, 135–137. [Google Scholar] [CrossRef]
- Touitou, E.; Dayan, N.; Bergelson, L.; Godin, B.; Eliaz, M. Ethosomes—Novel vesicular carriers for enhanced delivery: Characterization and skin penetration properties. J. Control. Release 2000, 65, 403–418. [Google Scholar] [CrossRef]
- Jain, S.; Umamaheshwari, R.; Bhadra, D.; Jain, N. Ethosomes: A novel vesicular carrier for enhanced transdermal delivery of an antiHIV agent. Indian J. Pharm. Sci. 2004, 66, 72. [Google Scholar]
- Sharma, A.; Kuhad, A.; Bhandari, R. Novel nanotechnological approaches for treatment of skin-aging. J. Tissue Viability 2022. in press. [Google Scholar] [CrossRef] [PubMed]
- Akhtar, N.; Akhtar, N. Development of stable tocopherol succinate-loaded ethosomes to enhance transdermal permeation: In vitro and in vivo characterizations. J. Cosmet. Dermatol. 2022. in press. [Google Scholar] [CrossRef] [PubMed]
- Rakesh, R.; Anoop, K. Formulation and optimization of nano-sized ethosomes for enhanced transdermal delivery of cromolyn sodium. J. Pharm. Bioallied Sci. 2012, 4, 333. [Google Scholar] [PubMed]
- Ascenso, A.; Raposo, S.; Batista, C.; Cardoso, P.; Mendes, T.; Praça, F.G.; Bentley, M.V.L.B.; Simões, S. Development, characterization, and skin delivery studies of related ultradeformable vesicles: Transfersomes, ethosomes, and transethosomes. Int. J. Nanomed. 2015, 10, 5837. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mao, Y.-T.; Hua, H.-Y.; Zhang, X.-G.; Zhu, D.-X.; Li, F.; Gui, Z.-H.; Zhao, Y.-X. Ethosomes as delivery system for transdermal administration of vinpocetine. Die Pharm. Int. J. Pharm. Sci. 2013, 68, 381–382. [Google Scholar]
- Andleeb, M.; Shoaib Khan, H.M.; Daniyal, M. Development, Characterization and Stability Evaluation of Topical Gel Loaded With Ethosomes Containing Achillea millefolium L. Extract. Front. Pharmacol. 2021, 12, 336. [Google Scholar] [CrossRef]
- Fathalla, D.; Youssef, E.M.; Soliman, G.M. Liposomal and ethosomal gels for the topical delivery of anthralin: Preparation, comparative evaluation and clinical assessment in psoriatic patients. Pharmaceutics 2020, 12, 446. [Google Scholar] [CrossRef]
- Reis, C.P.; Neufeld, R.J.; Ribeiro, A.J.; Veiga, F.; Nanoencapsulation, I. Methods for preparation of drug-loaded polymeric nanoparticles. Nanomed. Nanotechnol. Biol. Med. 2006, 2, 8–21. [Google Scholar] [CrossRef] [Green Version]
- Sharif, A.; Akhtar, N. Fabrication of niosomes containing N-acetyl glucosamine: In-vitro and ex-vivo characterizations. Pak. J. Pharm. Sci. 2020, 33, 1321–1326. [Google Scholar]
- Castro, N.R.; Cristal dos Santos, C.P.; de Campos, V.E.B.; Cardoso, V.; Vermelho, A.B.; dos Santos, E.P.; Mansur, C.R.E. Development of hybrid vesicular nanosystems composed of lipids and chitosan for octyl methoxycinnamate encapsulation. Colloids Surf. A Physicochem. Eng. Asp. 2021, 608, 125476. [Google Scholar] [CrossRef]
- Shumilov, M.; Bercovich, R.; Duchi, S.; Ainbinder, D.; Touitou, E. Ibuprofen transdermal ethosomal gel: Characterization and efficiency in animal models. J. Biomed. Nanotechnol. 2010, 6, 569–576. [Google Scholar] [CrossRef] [PubMed]
- Campos, E.V.; Proença, P.L.; da Costa, T.G.; de Lima, R.; Fraceto, L.F.; de Araujo, D.R. Using Chitosan-Coated Polymeric Nanoparticles-Thermosensitive Hydrogels in association with Limonene as Skin Drug Delivery Strategy. BioMed Res. Int. 2022, 2022, 9165443. [Google Scholar] [CrossRef] [PubMed]
- Khan, Z.U.; Razzaq, A.; Khan, A.; Rehman, N.U.; Khan, H.; Khan, T.; Khan, A.U.; Althobaiti, N.A.; Menaa, F.; Iqbal, H. Physicochemical Characterizations and Pharmacokinetic Evaluation of Pentazocine Solid Lipid Nanoparticles against Inflammatory Pain Model. Pharmaceutics 2022, 14, 409. [Google Scholar] [CrossRef]
- Pereira, T.A.; Guerreiro, C.M.; Maruno, M.; Ferrari, M.; Rocha-Filho, P.A. Exotic vegetable oils for cosmetic o/w nanoemulsions: In vivo evaluation. Molecules 2016, 21, 248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khalil, R.M.; Abdelbary, G.A.; Basha, M.; Awad, G.E.; El-Hashemy, H.A. Design and evaluation of proniosomes as a carrier for ocular delivery of lomefloxacin HCl. J. Liposome Res. 2017, 27, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Apolinario, A.C.; Hauschke, L.; Nunes, J.R.; Lopes, L.B. Towards nanoformulations for skin delivery of poorly soluble API: What does indeed matter? J. Drug Deliv. Sci. Technol. 2020, 60, 102045. [Google Scholar] [CrossRef]
- Sah, E.; Sah, H. Recent trends in preparation of poly (lactide-co-glycolide) nanoparticles by mixing polymeric organic solution with antisolvent. J. Nanomater. 2015, 16, 61. [Google Scholar] [CrossRef] [Green Version]
- Ibrahim, T.M.; Abdallah, M.H.; El-Megrab, N.A.; El-Nahas, H.M. Transdermal ethosomal gel nanocarriers; a promising strategy for enhancement of anti-hypertensive effect of carvedilol. J. Liposome Res. 2019, 29, 215–228. [Google Scholar] [CrossRef]
- Jain, S.; Patel, N.; Madan, P.; Lin, S. Quality by design approach for formulation, evaluation and statistical optimization of diclofenac-loaded ethosomes via transdermal route. Pharm. Dev. Technol. 2015, 20, 473–489. [Google Scholar] [CrossRef]
- Basiri, L.; Rajabzadeh, G.; Bostan, A. Physicochemical properties and release behavior of Span 60/Tween 60 niosomes as vehicle for α-Tocopherol delivery. LWT 2017, 84, 471–478. [Google Scholar] [CrossRef]
- Junyaprasert, V.B.; Singhsa, P.; Suksiriworapong, J.; Chantasart, D. Physicochemical properties and skin permeation of Span 60/Tween 60 niosomes of ellagic acid. Int. J. Pharm. 2012, 423, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Shi, Y.; Wang, H.; Zhao, X.; Sun, Q.; Huang, Y.; Qi, T.; Lin, G. Ethosomal Gel for Improving Transdermal Delivery of Thymosin β-4. Int. J. Nanomed. 2019, 14, 9275–9284. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pyrz, W.D.; Buttrey, D.J. Particle size determination using TEM: A discussion of image acquisition and analysis for the novice microscopist. Langmuir 2008, 24, 11350–11360. [Google Scholar] [CrossRef] [PubMed]
- Chourasia, M.K.; Kang, L.; Chan, S.Y. Nanosized ethosomes bearing ketoprofen for improved transdermal delivery. Results Pharma Sci. 2011, 1, 60–67. [Google Scholar] [CrossRef] [Green Version]
- Iyer, S.S.; Barr, W.H.; Karnes, H.T. Profiling in vitro drug release from subcutaneous implants: A review of current status and potential implications on drug product development. Biopharm. Drug Dispos. 2006, 27, 157–170. [Google Scholar] [CrossRef]
- Nair, R.; Arun Kumar, K.; Vishnu Priya, K.; Sevukarajan, M. Recent advances in solid lipid nanoparticle based drug delivery systems. J. Biomed. Sci. Res 2011, 3, 368–384. [Google Scholar]
- Shatalebi, M.; Mostafavi, S.; Moghaddas, A. Niosome as a drug carrier for topical delivery of N-acetyl glucosamine. Res. Pharm. Sci. 2010, 5, 107. [Google Scholar]
- Natsheh, H.; Touitou, E. Phospholipid vesicles for dermal/transdermal and nasal administration of active molecules: The effect of surfactants and alcohols on the fluidity of their lipid bilayers and penetration enhancement properties. Molecules 2020, 25, 2959. [Google Scholar] [CrossRef]
- He, J.; Shi, H.; Huang, S.; Han, L.; Zhang, W.; Zhong, Q. Core-shell nanoencapsulation of α-tocopherol by blending sodium oleate and rebaudioside A: Preparation, characterization, and antioxidant activity. Molecules 2018, 23, 3183. [Google Scholar] [CrossRef] [Green Version]
- Thang, L.; Hanh, N.; Duong, D. Study on cause-effect relations and optimization of exemestane-loaded nanostructured lipid carriers. Int. J. Pharm. Pharm. Sci. 2017, 9, 68–74. [Google Scholar] [CrossRef] [Green Version]
- Sargam, Y.; Wang, K.; Tsyrenova, A.; Liu, F.; Jiang, S. Effects of anionic and nonionic surfactants on the dispersion and stability of nanoSiO2 in aqueous and cement pore solutions. Cem. Concr. Res. 2021, 144, 106417. [Google Scholar] [CrossRef]
- Abd El-Alim, S.; Kassem, A.; Basha, M. Proniosomes as a novel drug carrier system for buccal delivery of benzocaine. J. Drug Deliv. Sci. Technol. 2014, 24, 452–458. [Google Scholar] [CrossRef]
- Shirsand, S.; Para, M.; Nagendrakumar, D.; Kanani, K.; Keerthy, D. Formulation and evaluation of Ketoconazole niosomal gel drug delivery system. Int. J. Pharm. Investig. 2012, 2, 201. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elsayed, M.M.; Abdallah, O.Y.; Naggar, V.F.; Khalafallah, N.M. Deformable liposomes and ethosomes: Mechanism of enhanced skin delivery. Int. J. Pharm. 2006, 322, 60–66. [Google Scholar] [CrossRef]
- Budhiraja, A.; Dhingra, G. Development and characterization of a novel antiacne niosomal gel of rosmarinic acid. Drug Deliv. 2015, 22, 723–730. [Google Scholar] [CrossRef] [Green Version]
- Abdulbaqi, I.M.; Darwis, Y.; Khan, N.A.K.; Abou Assi, R.; Khan, A.A. Ethosomal nanocarriers: The impact of constituents and formulation techniques on ethosomal properties, in vivo studies, and clinical trials. Int. J. Nanomed. 2016, 11, 2279. [Google Scholar] [CrossRef] [Green Version]
- Arora, D.; Nanda, S. Quality by design driven development of resveratrol loaded ethosomal hydrogel for improved dermatological benefits via enhanced skin permeation and retention. Int. J. Pharm. 2019, 567, 118448. [Google Scholar] [CrossRef]




| Code | Drug (%) | Propylene Glycol (%) | Phospholipid (%) | Ethanol (%) | Water (%) | E.E (%) |
|---|---|---|---|---|---|---|
| TA-1 | 0.25 | 10 | 5 | 25 | q.s | 91.80 |
| TA-2 | 0.25 | 10 | 2.5 | 25 | q.s | 92.03 |
| TA-3 | 0.25 | 10 | 0.5 | 25 | q.s | 96.37 |
| TA-4 | 0.25 | 10 | 5 | 30 | q.s | 99.2 |
| TA-5 | 0.25 | 10 | 2.5 | 30 | q.s | 99.71 |
| TA-6 | 0.25 | 10 | 0.5 | 30 | q.s | 97.89 |
| TA-7 | 0.25 | 10 | 5 | 40 | q.s | 93.04 |
| TA-8 | 0.25 | 10 | 2.5 | 40 | q.s | 95.78 |
| TA-9 | 0.25 | 10 | 0.5 | 40 | q.s | 97.73 |
| Observed Parameters | Temp. | Fresh | After 48 h | After 72 h | After 7 days | After 21 days | After 30 days | After 60 days | After 90 days | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C | E | C | E | C | E | C | E | C | E | C | E | C | E | C | E | ||
| Color | 8 °C | W | W | W | W | W | W | W | W | W | W | W | W | W | W | W | W |
| 25 °C | W | W | W | W | W | W | W | W | W | W | W | W | W | W | W | W | |
| 40 °C | W | W | W | W | W | W | W | W | W | W | OW | W | LY | LY | Y | LY | |
| 40 °C ± 75% RH | W | W | W | W | W | W | W | W | W | W | OW | W | LY | LY | Y | LY | |
| Odor | 8 °C | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 25 °C | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| 40 °C | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| 40 °C ± 75% RH | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Look | 8 °C | T | M | T | M | T | M | T | M | T | M | T | M | T | M | T | M |
| 25 °C | T | M | T | M | T | M | T | M | T | M | T | M | T | M | T | M | |
| 40 °C | T | M | T | M | T | M | T | M | T | M | T | M | T | M | T | M | |
| 40 °C ± 75% RH | T | M | T | M | T | M | T | M | T | M | T | M | T | M | T | M | |
| Liquefaction | 8 °C | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
| 25 °C | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| 40 °C | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| 40 °C ± 75% RH | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |
| Formulations | pH 5.5 | ER of TAEG | TE of TAEG | ||
|---|---|---|---|---|---|
| Flux (µg/cm².h) | Papp (cm/h) | % Drug Permeated | |||
| TAEG | 23.75 | 0.0095 | 44.55 ± 0.01% | 1.173 | 2.15 |
| TACG | 20.25 | 0.0081 | 30.44 ± 0.01% | ||
| pH 7.4 | |||||
| TAEG | 3.43 | 0.0014 | 36.18 ± 0.01% | 0.441 | 1.30 |
| TACG | 7.72 | 0.0031 | 14.76 ± 0.01% | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akhtar, N.; Akhtar, N.; Menaa, F.; Alharbi, W.; Alaryani, F.S.S.; Alqahtani, A.M.; Ahmad, F. Fabrication of Ethosomes Containing Tocopherol Acetate to Enhance Transdermal Permeation: In Vitro and Ex Vivo Characterizations. Gels 2022, 8, 335. https://doi.org/10.3390/gels8060335
Akhtar N, Akhtar N, Menaa F, Alharbi W, Alaryani FSS, Alqahtani AM, Ahmad F. Fabrication of Ethosomes Containing Tocopherol Acetate to Enhance Transdermal Permeation: In Vitro and Ex Vivo Characterizations. Gels. 2022; 8(6):335. https://doi.org/10.3390/gels8060335
Chicago/Turabian StyleAkhtar, Naheed, Naveed Akhtar, Farid Menaa, Walaa Alharbi, Fatima Saad Salem Alaryani, Ali Musfer Alqahtani, and Faizan Ahmad. 2022. "Fabrication of Ethosomes Containing Tocopherol Acetate to Enhance Transdermal Permeation: In Vitro and Ex Vivo Characterizations" Gels 8, no. 6: 335. https://doi.org/10.3390/gels8060335
APA StyleAkhtar, N., Akhtar, N., Menaa, F., Alharbi, W., Alaryani, F. S. S., Alqahtani, A. M., & Ahmad, F. (2022). Fabrication of Ethosomes Containing Tocopherol Acetate to Enhance Transdermal Permeation: In Vitro and Ex Vivo Characterizations. Gels, 8(6), 335. https://doi.org/10.3390/gels8060335







