An Evaluation of the Performance of Low-Cost Resin Printers in Orthodontics
Abstract
1. Introduction
2. Materials and Methods
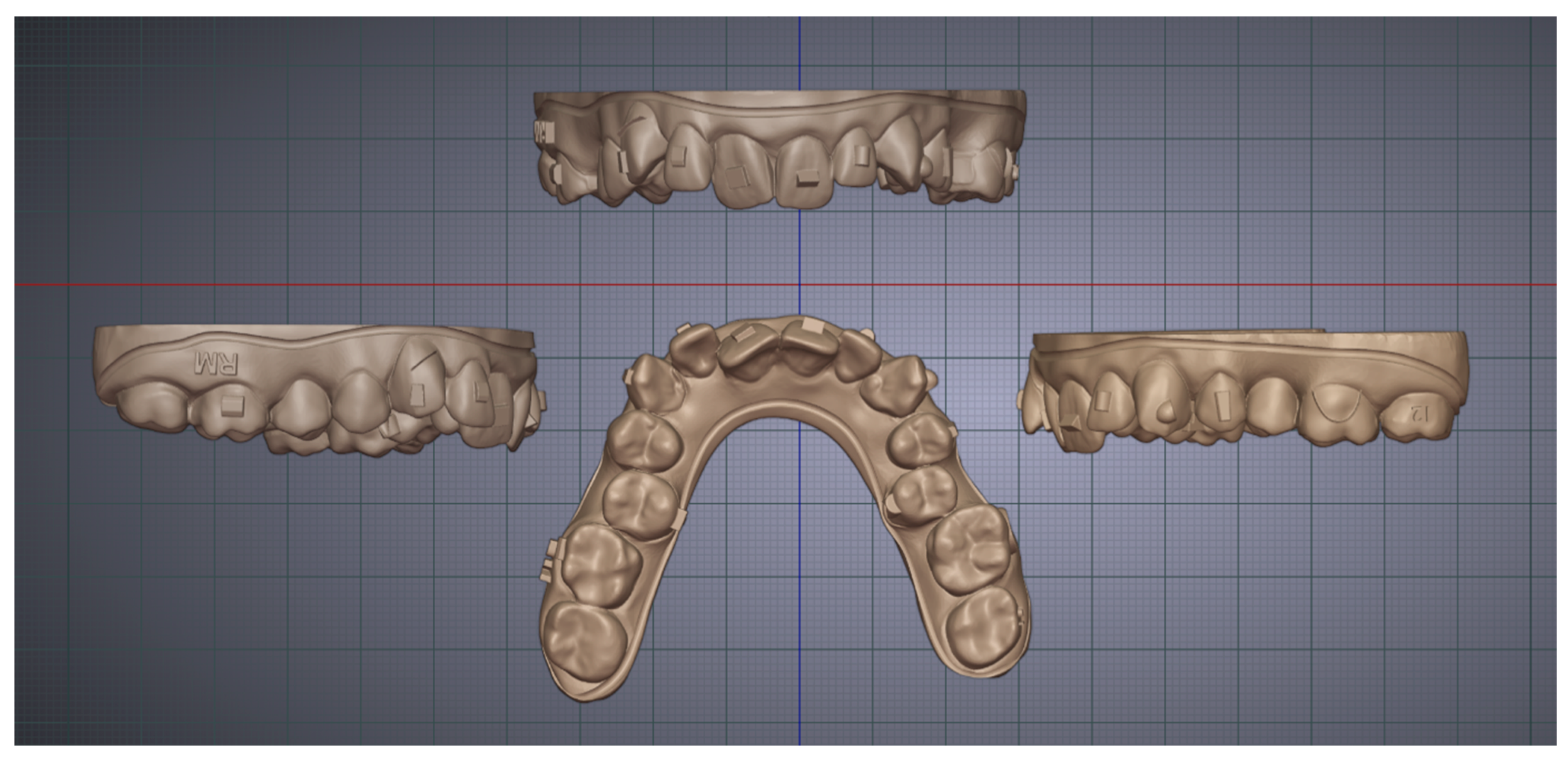
2.1. Model Design
2.2. Printing Material
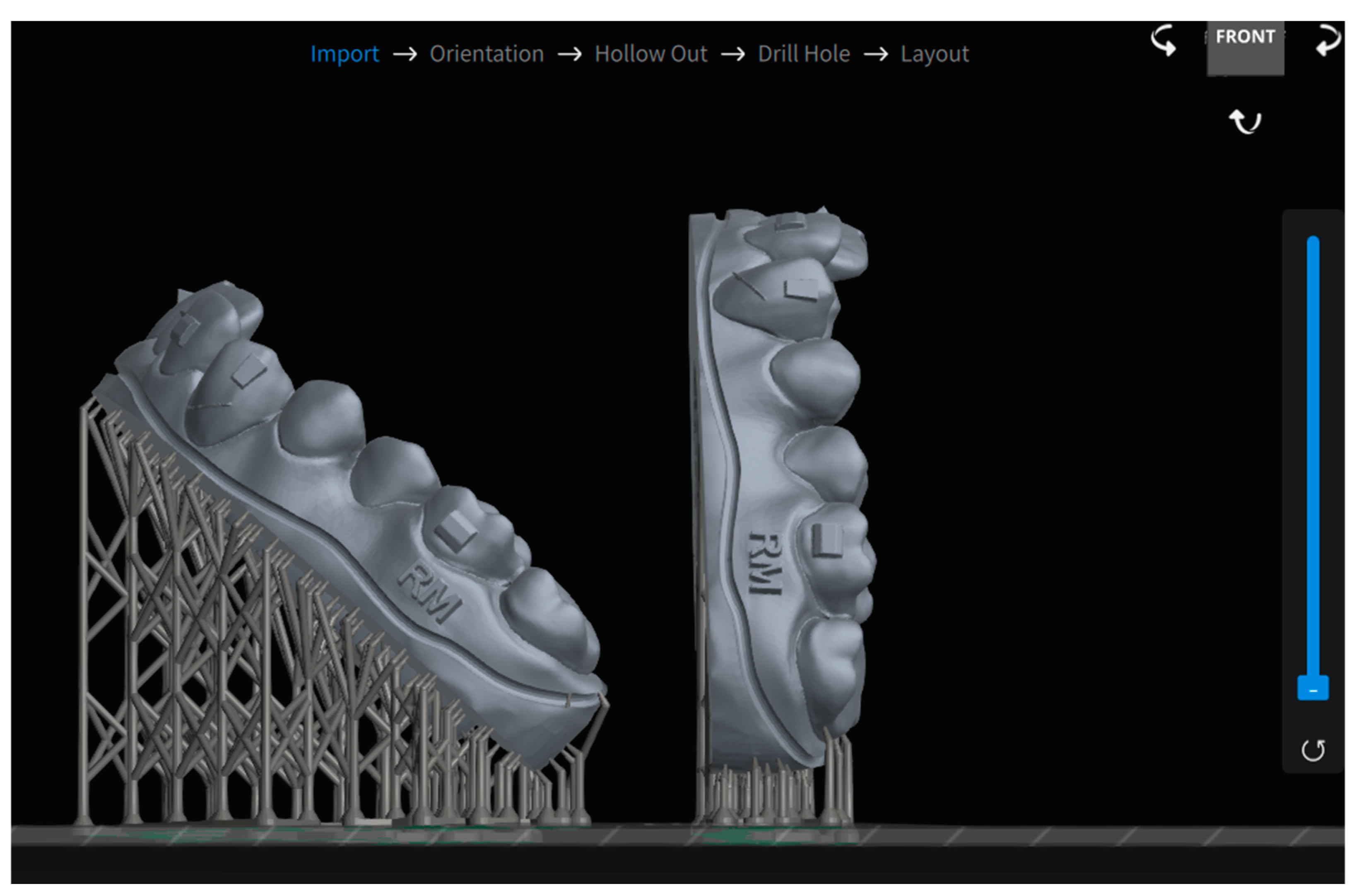
2.3. Printing Process
2.4. Post-Processing
2.5. Scanning
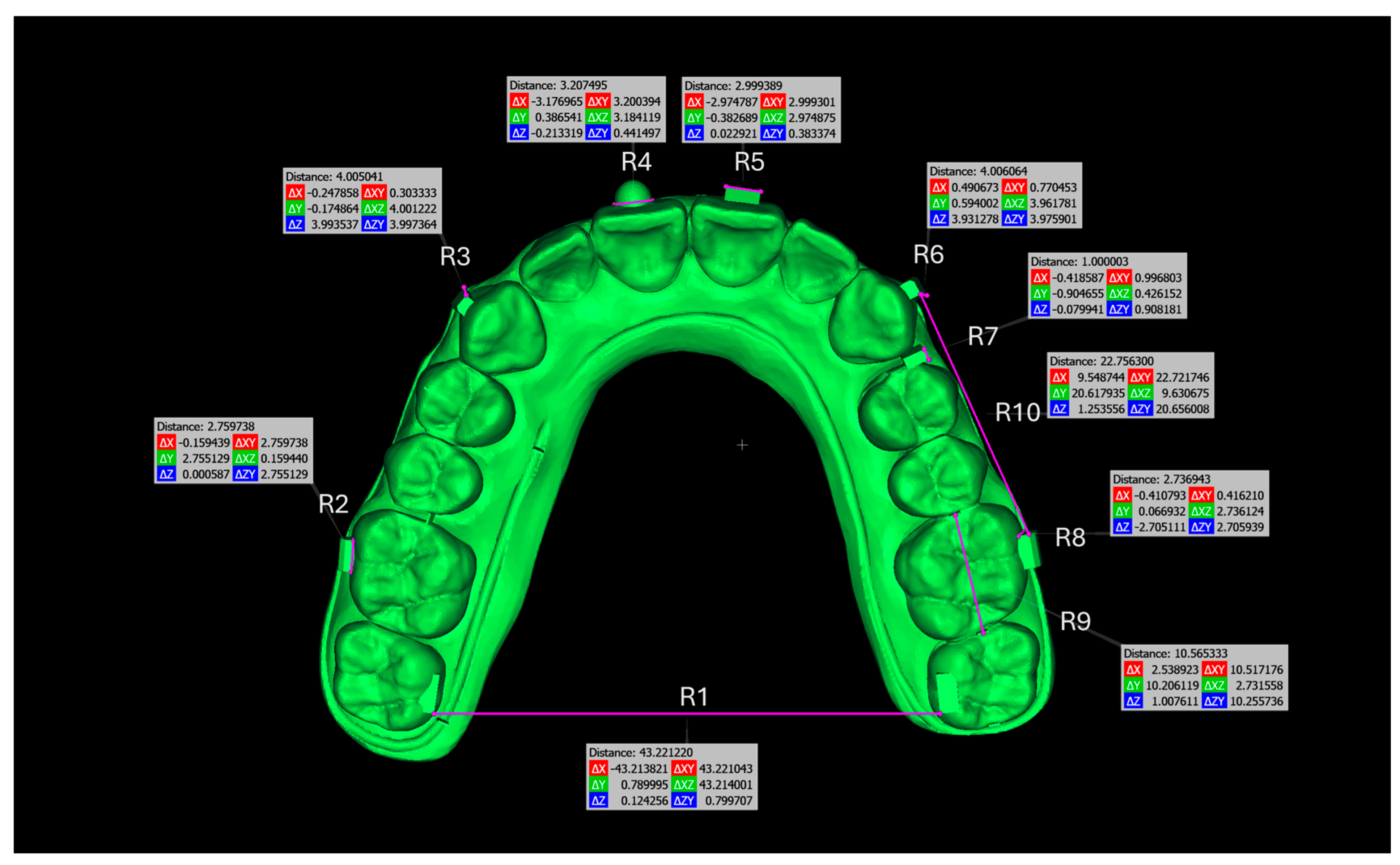
2.6. Comparison and Evaluation
2.7. Statistical Analysis
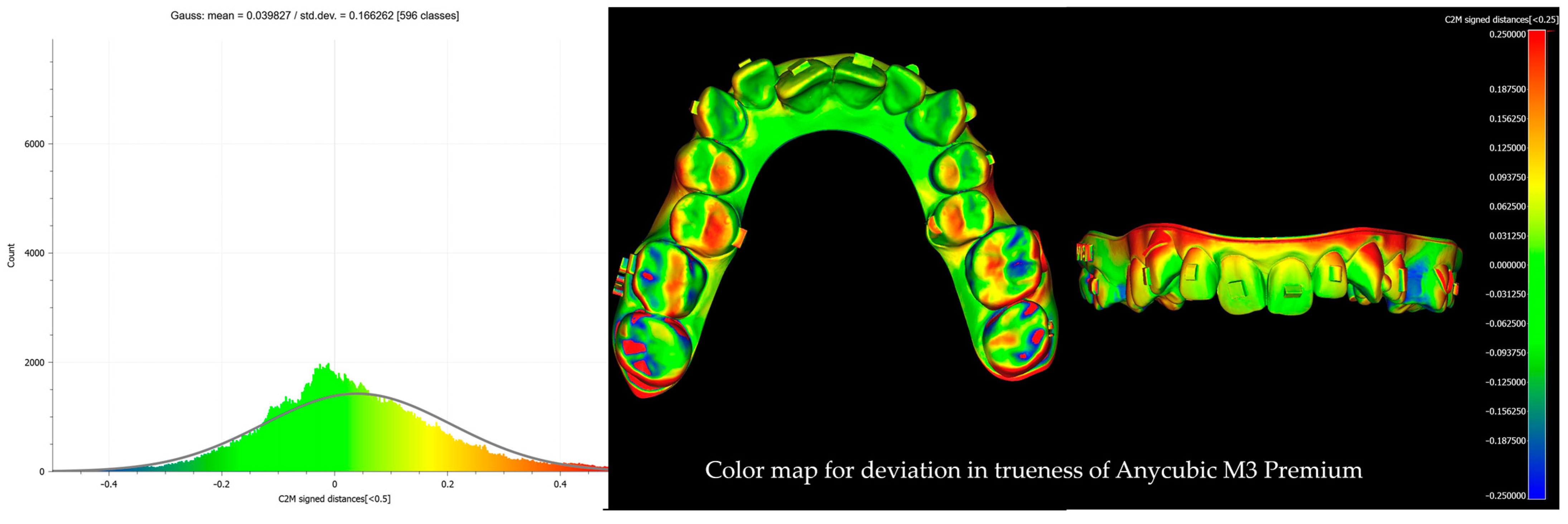
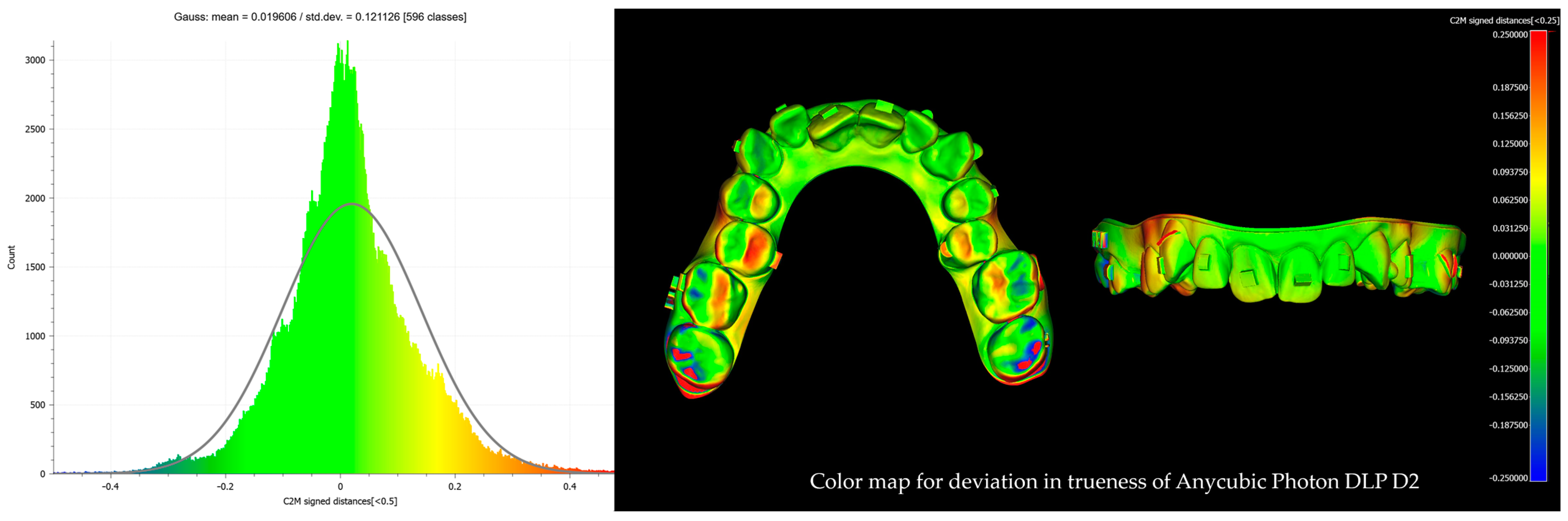
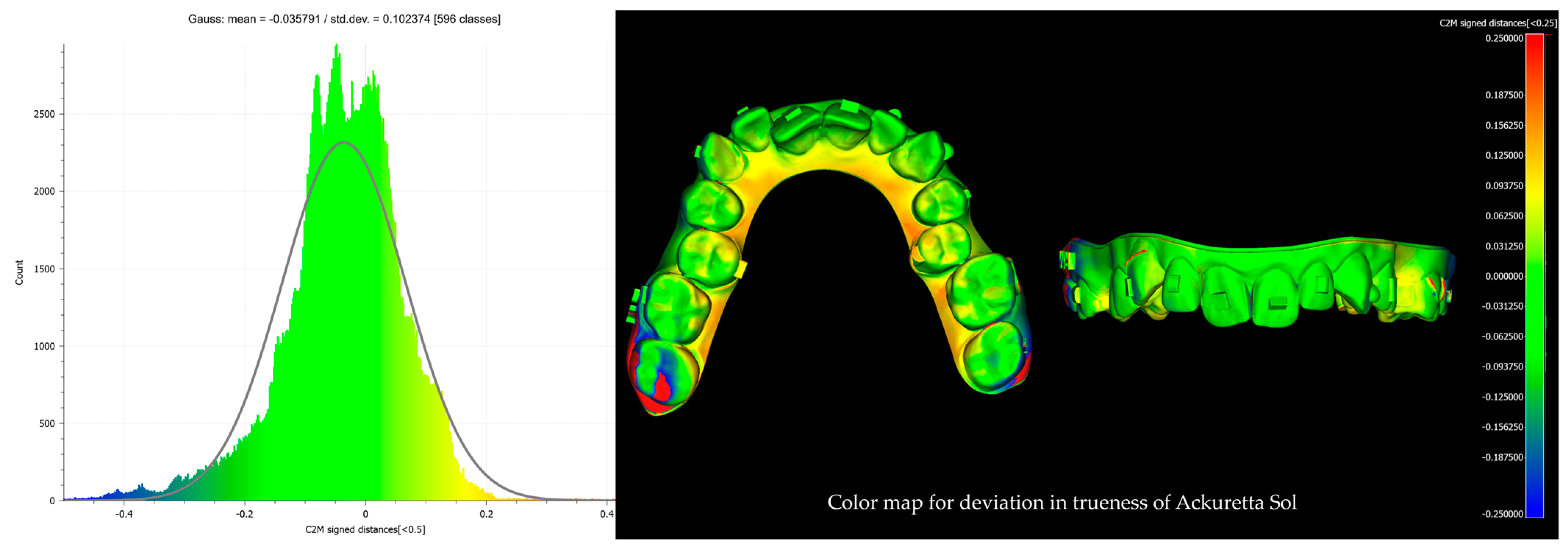
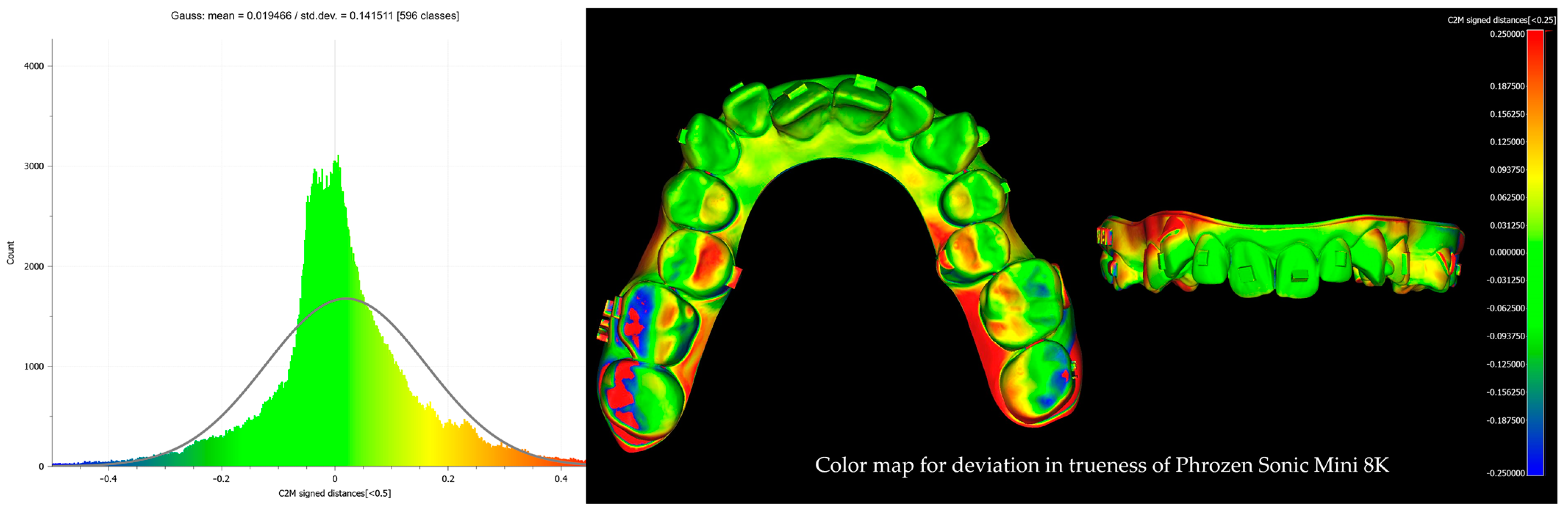
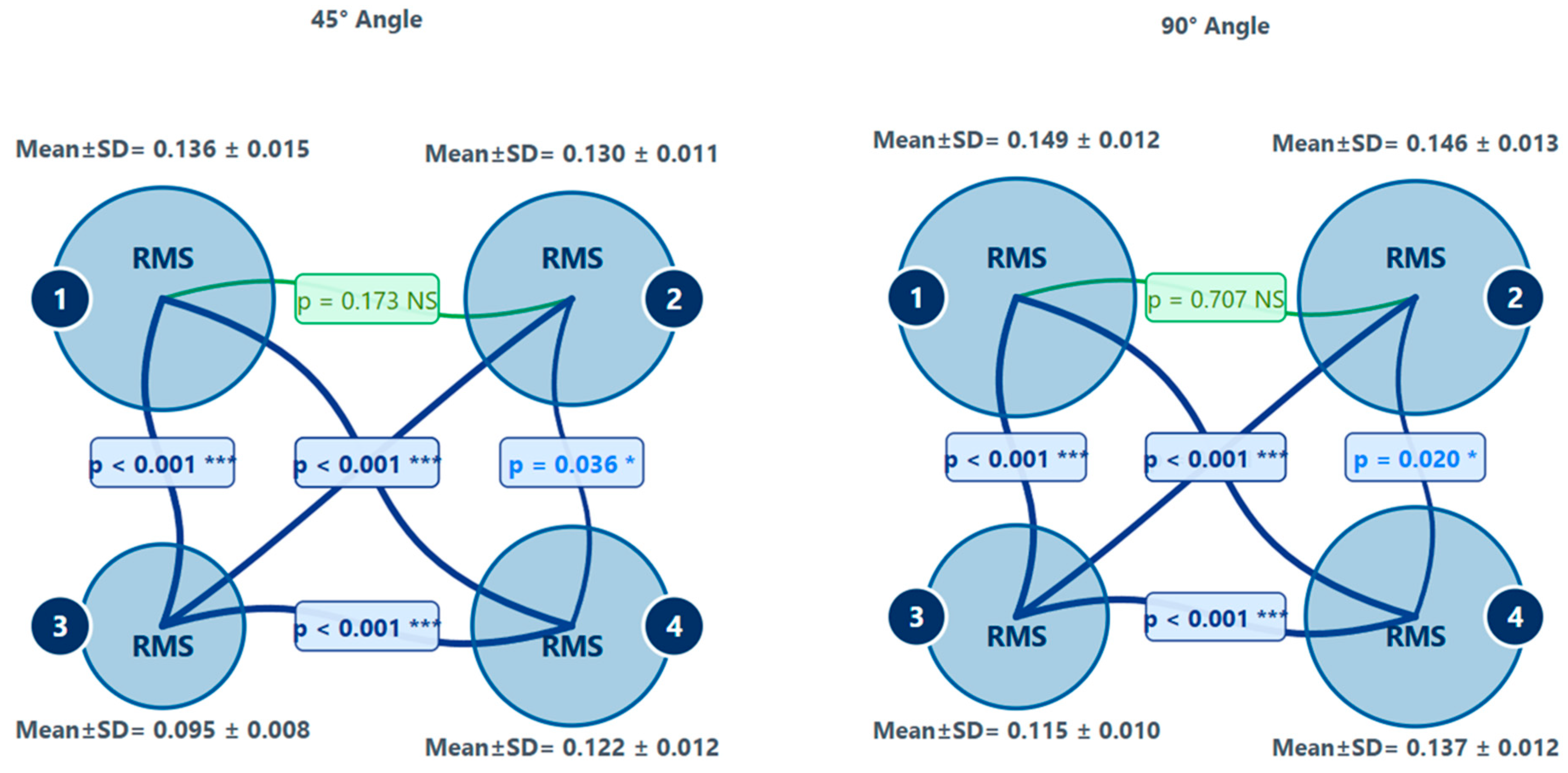
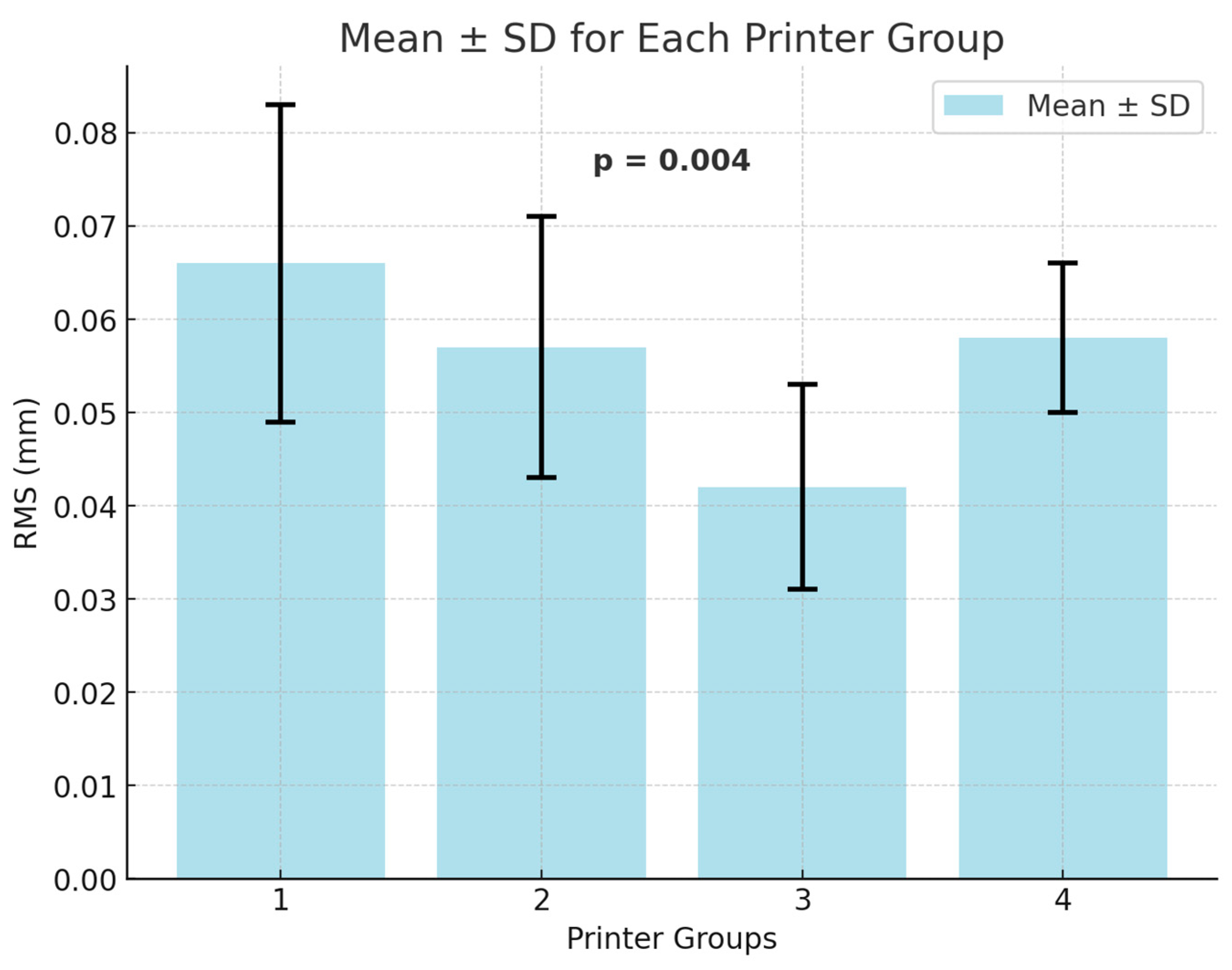
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cole, D.; Bencharit, S.; Carrico, C.K.; Arias, A.; Tüfekçi, E. Evaluation of fit for 3D-printed retainers compared with thermoform retainers. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 592–599. [Google Scholar] [CrossRef] [PubMed]
- Tay, Y.W.; Panda, B.; Paul, S.C.; Tan, M.J.; Qian, S.; Leong, K.F.; Chua, C.K. Processing and properties of construction materials for 3D printing. Mater. Sci. Forum. 2016, 861, 177–181. [Google Scholar] [CrossRef]
- Wang, X.; Shujaat, S.; Jacobs, R. Accuracy of desktop versus professional 3D printers for maxillofacial model production. A systematic review and meta-analysis. J. Dent. 2021, 112, 103741. [Google Scholar] [CrossRef]
- Guo, N.; Leu, M.C. Additive manufacturing: Technology, applications and research needs. Front. Mech. Eng. 2013, 8, 215–243. [Google Scholar] [CrossRef]
- Prendergast, M.E.; Burdick, J.A. Recent advances in enabling technologies in 3D printing for precision medicine. Adv. Mater. 2020, 32, 1902516. [Google Scholar] [CrossRef]
- Guzzi, E.A.; Tibbitt, M.W. Additive manufacturing of precision biomaterials. Adv. Mater. 2020, 32, 1901994. [Google Scholar] [CrossRef]
- Dawood, A.; Marti, B.M.; Sauret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Jindal, P.; Juneja, M.; Siena, F.L.; Bajaj, D.; Breedon, P. Mechanical and geometric properties of thermoformed and 3D printed clear dental aligners. Am. J. Orthod. Dentofacial Orthop. 2019, 156, 694–701. [Google Scholar] [CrossRef]
- Caminiti, M.; Lou, T. Clear aligner orthognathic splints. J. Oral Maxillofac. Surg. 2019, 77, 1071.e1–1071.e8. [Google Scholar] [CrossRef]
- Cassetta, M.; Altieri, F.; Giorgio, R.D.; Barbato, E. Palatal orthodontic miniscrew insertion using a CAD-CAM surgical guide: Description of a technique. Int. J. Oral Maxillofac. Surg. 2018, 47, 1195–1198. [Google Scholar] [CrossRef]
- Grassia, V.; Ronsivalle, V.; Isola, G.; Nucci, L.; Leonardi, R.; Lo Giudice, A. Accuracy (trueness and precision) of 3D printed orthodontic models finalized to clear aligners production, testing crowded and spaced dentition. BMC Oral Health 2023, 23, 352. [Google Scholar] [CrossRef] [PubMed]
- Schittecatte, L.; Geertsen, V.; Bonamy, D.; Nguyen, T.; Guenoun, P. From resin formulation and process parameters to the final mechanical properties of 3D printed acrylate materials. MRS Commun. 2023, 13, 357–377. [Google Scholar] [CrossRef]
- Alifui-Segbaya, F. Biomedical photopolymers in 3D printing. Rapid Prototyp. J. 2020, 26, 437–444. [Google Scholar] [CrossRef]
- Ligon, S.C.; Liska, R.; Stampfl, J.; Gurr, M.; Mülhaumpt, R. Polymers for 3D printing and customized additive manufacturing. Chem. Rev. 2017, 117, 10212–10290. [Google Scholar] [CrossRef]
- Chang, D.G.; Li, S.; An, C.F. The influence analysis of globular indexing cam mechanism size parameters on transmission performance. Adv. Mater. Res. 2012, 426, 163–167. [Google Scholar] [CrossRef]
- Yu, C.; Schimelman, J.; Wang, P.; Miller, K.L.; Ma, X.; You, S.; Guan, J.; Sun, B.; Zhu, W.; Chen, S. Photopolymerizable biomaterials and light-based 3D printing strategies for biomedical applications. Chem. Rev. 2020, 120, 10695–10743. [Google Scholar] [CrossRef]
- Mohamed, M.G.; Kumar, H.; Wang, Z.; Martin, N.; Mills, B.; Kim, K. Rapid and inexpensive fabrication of multi-depth microfluidic device using high-resolution LCD stereolithographic 3D printing. J. Manuf. Mater. Process. 2019, 3, 26. [Google Scholar] [CrossRef]
- Shan, W.; Chen, Y.; Hu, M.; Qin, S.; Peng, L. 4D printing of shape memory polymer via liquid crystal display (LCD) stereolithographic 3D printing. Mater. Res. Express 2020, 7, 105305. [Google Scholar] [CrossRef]
- Quan, H.; Zhang, T.; Xu, H.; Luo, S.; Nie, J.; Zhu, X. Photo-curing 3D printing technique and its challenges. Bioact. Mater. 2020, 5, 110–115. [Google Scholar] [CrossRef]
- Brown, G.B.; Currier, G.F.; Kadioglu, O.; Kierl, J.P. Accuracy of 3-dimensional printed dental models reconstructed from digital intraoral impressions. Am. J. Orthod. Dentofac. Orthop. 2018, 154, 733–739. [Google Scholar] [CrossRef]
- ISO 12836; Dentistry—Digitizing Devices for CAD/CAM Systems for Indirect Dental Restorations—Test Methods for Assessing Accuracy (2nd Ed.). International Organization for Standardization: Geneva, Switzerland, 2015.
- Koenig, N.; Choi, J.Y.; McCray, J.; Hayes, A.; Schneider, P.; Kim, K.B. Comparison of dimensional accuracy between direct-printed and thermoformed aligners. Korean J. Orthod. 2022, 52, 249–257. [Google Scholar] [CrossRef] [PubMed]
- Kessler, A.; Hickel, R.; Reymus, M. 3D printing in dentistry—State of the art. Oper. Dent. 2020, 45, 30–40. [Google Scholar] [CrossRef] [PubMed]
- ElShebiny, T.; Matthaios, S.; Menezes, L.M.; Tsolakis, I.A.; Palomo, J.M. Effect of printing technology, layer height, and orientation on assessment of 3D-printed models. J. World Fed. Orthod. 2024, 13, 169–174. [Google Scholar] [CrossRef]
- Ko, J.; Bloomstein, R.D.; Briss, D.; Holland, J.N.; Morsy, H.M.; Kasper, F.K.; Huang, W. Effect of build angle and layer height on the accuracy of 3-dimensional printed dental models. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 451–458.e2. [Google Scholar] [CrossRef]
- Favero, C.S.; English, J.D.; Cozad, B.E.; Wirthlin, J.O.; Short, M.M.; Kasper, F.K. Effect of print layer height and printer type on the accuracy of 3-dimensional printed orthodontic models. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 557–565. [Google Scholar] [CrossRef]
- Venezia, P.; Ronsivalle, V.; Rustico, L.; Barbato, E.; Leonardi, R.; Giudice, A.L. Accuracy of orthodontic models prototyped for clear aligners therapy: A 3D imaging analysis comparing different market segment 3D printing protocols. J. Dent. 2022, 124, 104212. [Google Scholar] [CrossRef]
- Tsolakis, I.A.; Papaioannou, W.; Papadopoulou, E.; Dalampira, M.; Tsolakis, A.I. Comparison in terms of accuracy between DLP and LCD printing technology for dental model printing. Dent. J. 2022, 10, 181. [Google Scholar] [CrossRef]
- Nulty, A. A comparison of trueness and precision of 12 3D printers used in dentistry. BDJ Open 2022, 8, 14. [Google Scholar] [CrossRef]
- Lo Giudice, A.; Ronsivalle, V.; Rustico, L.; Aboulazm, K.; Isola, G.; Palazzo, G. Evaluation of the accuracy of orthodontic models prototyped with entry-level LCD-based 3D printers: A study using surface-based superimposition and deviation analysis. Clin. Oral Investig. 2022, 6, 303–312. [Google Scholar] [CrossRef]
- Lohfeld, S.; Belnap, B.; Retrouvey, J.M.; Walker, M.P. Effect of model body type and print angle on the accuracy of 3D-printed orthodontic models. Biomimetics 2024, 9, 217. [Google Scholar] [CrossRef]
- Hassan, W.N.W.; Yusoff, Y.; Mardi, N.A. Comparison of reconstructed rapid prototyping models produced by 3D printing and conventional stone models with different degrees of crowding. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 209–218. [Google Scholar] [CrossRef] [PubMed]
- Hazeveld, A.; Slater, J.J.H.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Vlaskalic, V.; Boyd, R. Orthodontic treatment of a mildly crowded malocclusion using the Invisalign System. Aust. Orthod. J. 2001, 17, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Jaber, S.T.; Hajeer, M.Y.; Khattab, T.Z.; Mahaini, L. Evaluation of the fused deposition modeling and the digital light processing techniques in terms of dimensional accuracy of printing dental models used for the fabrication of clear aligners. Clin. Exp. Dent. Res. 2021, 7, 591–600. [Google Scholar] [CrossRef]
| Feature | Anycubic Photon M3 Premium (Printer 1) | Anycubic Photon DLP D2 (Printer 2) | Ackuretta SOL (Printer 3) | Phrozen Sonic Mini 8K (Printer 4) |
|---|---|---|---|---|
| 3D Printing Technology | Monochrome LCD | DLP (Digital Light Processing) | Monochrome LCD | Monochrome LCD |
| Screen/Projector | 7680 × 4320 pixels (8K) | 2560 × 1440 pixels (2K) DLP Projector | Unspecified | 7500 × 3240 pixels (8K) |
| XY Resolution | 28.5 µm | 51 µm | 49 µm | 22 µm |
| Layer Thickness (Adjustable) | 50–150 µm | 50–150 µm | 50–150 µm | 22–150 µm |
| Price | USD 650–400 | USD 680–400 | USD 9750 | USD 509.99 |
| Screen Lifespan | 2000 h | 20000 h | 10000 h | 2000 h |
| Printer | (45° vs. 90°) | t-Value | p-Value |
|---|---|---|---|
| 1 | 45° vs. 90° | −4.044 | <0.001 *** |
| 2 | 45° vs. 90° | −4.713 | <0.001 *** |
| 3 | 45° vs. 90° | −8.912 | <0.001 *** |
| 4 | 45° vs. 90° | −5.905 | <0.001 *** |
| Variable | Test | p-Value | Post Hoc | Printer 1 | Printer 2 | Printer 3 | Printer 4 | Group Differences |
|---|---|---|---|---|---|---|---|---|
| R1 | ANOVA | <0.05 | Tukey HSD | 0.533 ± 0.067 | 0.294 ± 0.049 | 0.204 ± 0.043 | 0.318 ± 0.066 | All groups significantly different |
| R2 | ANOVA | <0.05 | Tamhane T2 | 0.035 ± 0.039 | 0.021 ± 0.020 | 0.013 ± 0.024 | 0.043 ± 0.041 | Only 3–4 different |
| R3 | Kruskal–Wallis | <0.001 | Dunn’s | 0.04 (−0.04–0.12) | 0.02 (−0.04–0.05) | 0.01 (−0.04–0.03) | 0.02 (−0.03–0.06) | 1–2, 1–3 different |
| R4 | Kruskal–Wallis | 0.108 | None | 0.04 (−0.05–0.10) | 0.03 (−0.05–0.05) | 0.02 (0.00–0.07) | 0.02 (0.01–0.04) | No significant differences |
| R5 | Kruskal–Wallis | 0.849 | None | 0.02 (−0.04–0.05) | 0.02 (−0.04–0.05) | 0.02 (−0.02–0.04) | 0.02 (−0.04–0.04) | No significant differences |
| R6 | Kruskal–Wallis | 0.036 | Dunn’s | 0.02 (−0.03–0.05) | 0.01 (−0.03–0.03) | 0.01 (0.00–0.02) | 0.01 (−0.03–0.04) | Only 1–3 different |
| R7 | Kruskal–Wallis | 0.594 | None | 0.01 (−0.03–0.02) | 0.01 (−0.01–0.02) | 0.01 (−0.01–0.03) | 0.01 (−0.01–0.03) | No significant differences |
| R8 | Kruskal–Wallis | 0.088 | None | 0.03 (−0.04–0.07) | 0.03 (−0.04–0.05) | 0.01 (−0.05–0.03) | 0.02 (−0.04–0.05) | No significant differences |
| R9 | Kruskal–Wallis | <0.001 | Dunn’s | 0.11 (−0.11–0.18) | 0.12 (0.07–0.16) | 0.04 (0.01–0.07) | 0.04 (0.01–0.11) | 1–2, 1–3, 1–4, 2–4 different |
| R10 | ANOVA | <0.05 | Tamhane T2 | 0.151 ± 0.038 | 0.167 ± 0.032 | 0.087 ± 0.042 | 0.127 ± 0.022 | 1–3, 2–3, 3–4 different |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oğuz, F.; Bor, S. An Evaluation of the Performance of Low-Cost Resin Printers in Orthodontics. Biomimetics 2025, 10, 249. https://doi.org/10.3390/biomimetics10040249
Oğuz F, Bor S. An Evaluation of the Performance of Low-Cost Resin Printers in Orthodontics. Biomimetics. 2025; 10(4):249. https://doi.org/10.3390/biomimetics10040249
Chicago/Turabian StyleOğuz, Fırat, and Sabahattin Bor. 2025. "An Evaluation of the Performance of Low-Cost Resin Printers in Orthodontics" Biomimetics 10, no. 4: 249. https://doi.org/10.3390/biomimetics10040249
APA StyleOğuz, F., & Bor, S. (2025). An Evaluation of the Performance of Low-Cost Resin Printers in Orthodontics. Biomimetics, 10(4), 249. https://doi.org/10.3390/biomimetics10040249








