Abstract
Zirconia’s superior mechanical properties and biocompatibility have made it a cornerstone of modern prosthodontics, yet achieving durable biomimetic bonding to tooth structure remains a challenge. This scoping review synthesizes evidence on bonding strategies for zirconia-based fixed dental prostheses (FDPs), evaluating surface treatments, cementation protocols, and long-term performance. Following PRISMA-ScR guidelines, 18 studies from PubMed, Scopus, Web of Science, and Embase were thoroughly analyzed. Key findings indicate that tribochemical silica coating (e.g., Rocatec™) combined with 10-methacryloyloxydecyl dihydrogen phosphate (MDP)-based primers (e.g., Panavia V5) is associated with the highest bond strengths (>40 MPa) and exceptional clinical survival rates (e.g., >95% at 15 years for resin-bonded FDPs). These combined mechanical–chemical strategies can be viewed as an attempt to create a biomimetic, hybrid interface akin to the natural enamel–dentin junction. Additively manufactured zirconia exhibits inferior bonding compared to milled counterparts, while ethyl cellulose coatings applied to the bonding surface effectively prevent contamination from saliva and moisture during intraoral try-in procedures. However, heterogeneous testing protocols and limited long-term clinical data highlight the need for standardized aging models and randomized trials. This review consolidates current evidence, offering clinically actionable recommendations through a biomimetic lens while identifying critical gaps for future research.
1. Introduction
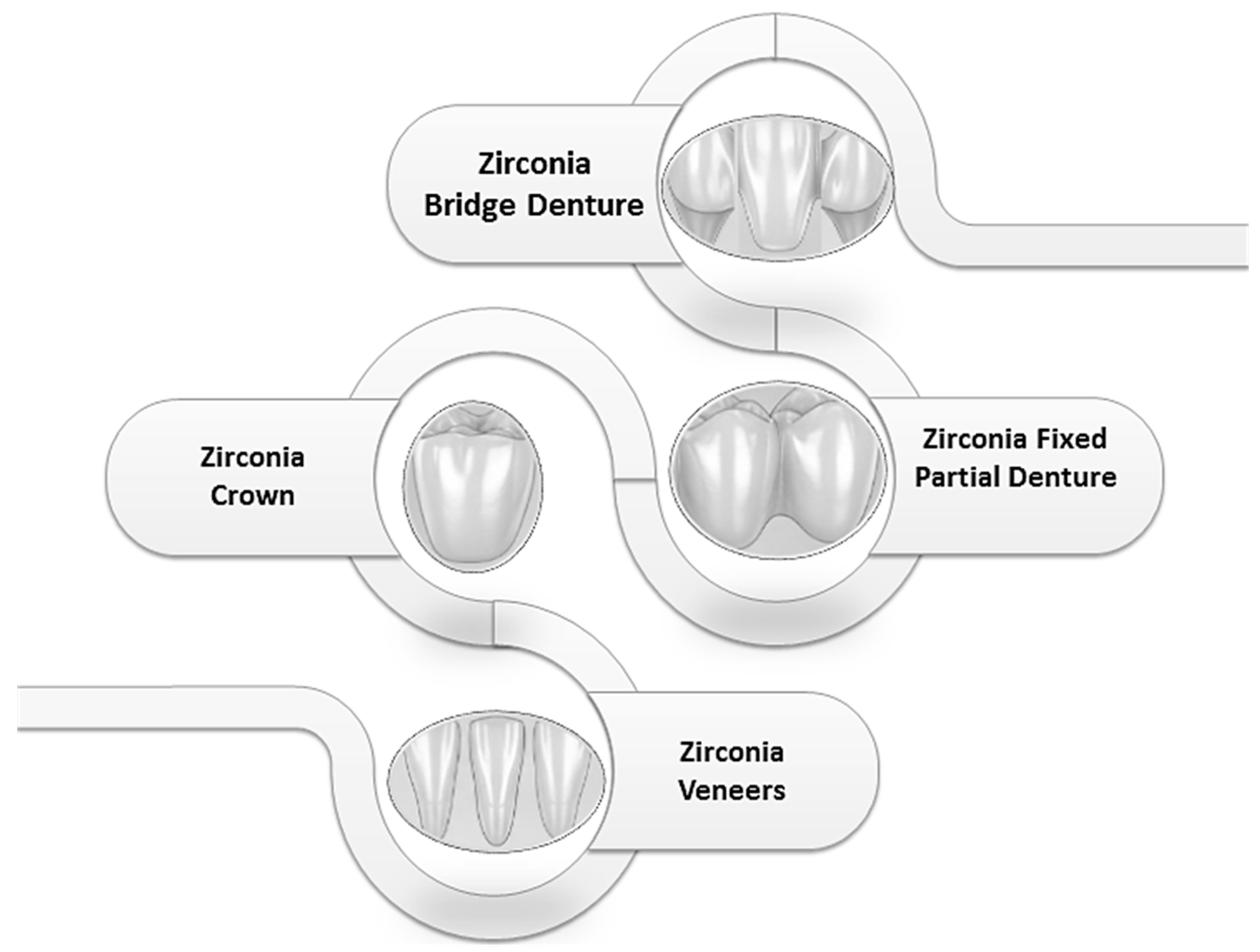
The rise in zirconia-based restorations marks a paradigm shift in modern prosthodontics, driven by their unparalleled biomechanical properties, biocompatibility, and esthetic potential [1,2,3,4,5,6]. As a polycrystalline ceramic devoid of a glassy phase, zirconia (ZrO2) derives its strength from transformation toughening, a mechanism that resists crack propagation, making it ideal for high-load applications such as crowns, fixed dental prostheses (FDPs), and resin-bonded restorations [7,8,9,10]. The figure below represents the main prosthodontic applications of zirconia in dental medicine: crowns, bridge, veneers, and fixed dentures (Figure 1).
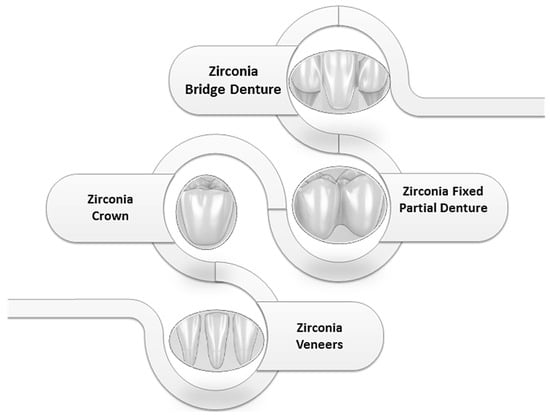
Figure 1.
Zirconia Applications in Prosthodontics.
However, its chemical inertness and absence of silica content challenge conventional adhesive protocols, which rely on micromechanical retention (e.g., acid etching) and chemical bonding (e.g., silane coupling agents) [11,12]. This inherent limitation has spurred extensive research into surface modifications, bioactive primers, and resin cements to achieve durable adhesion, yet debonding remains a leading cause of failure, with reported rates of 5–15% for resin-bonded FDPs over five years [13,14].
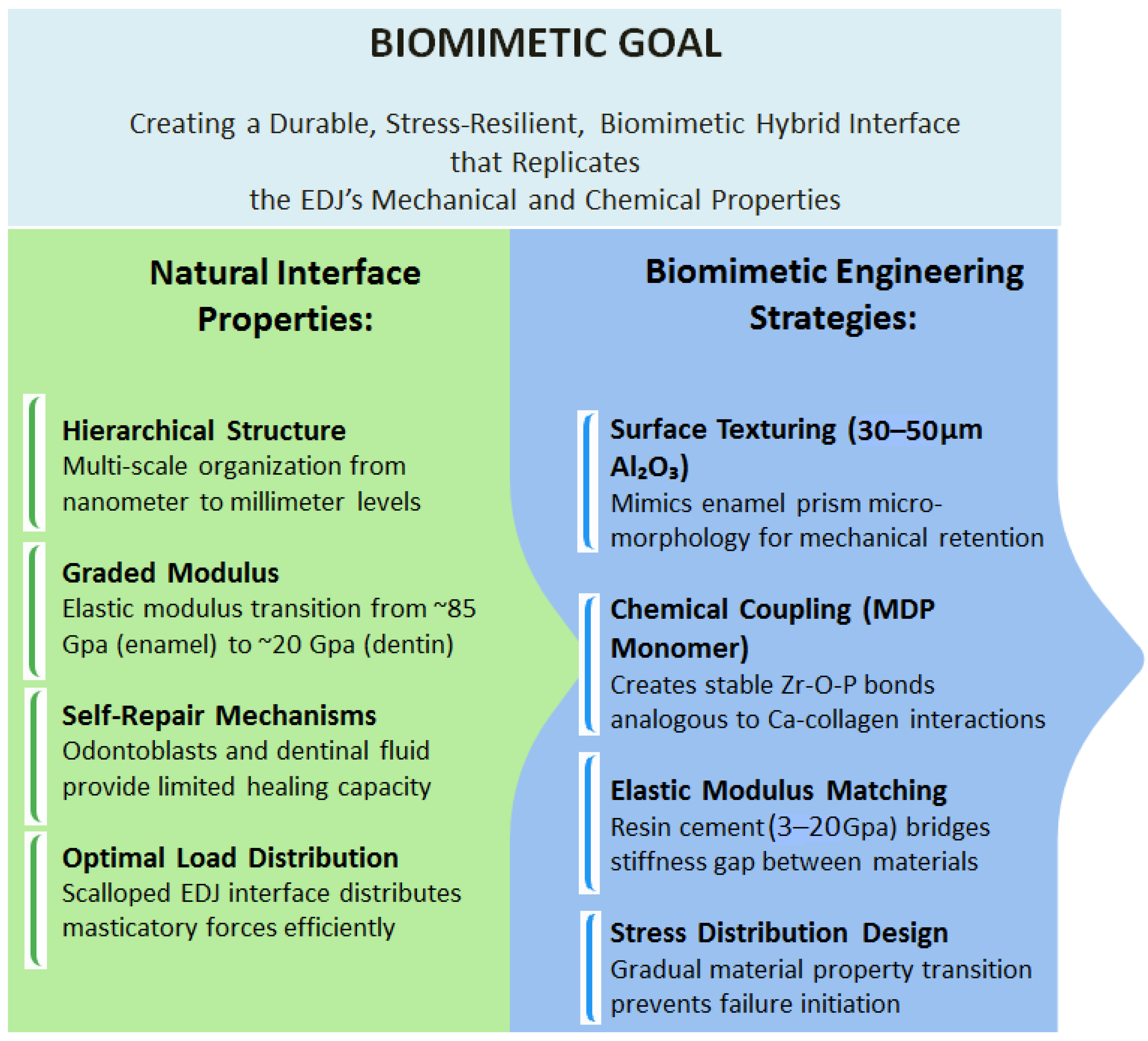
The evolution of zirconia bonding strategies reflects the convergence of material science and biomimetic principles [15]. The ultimate goal is to create a durable, stress-resilient tooth–restoration interface that mimics the biological excellence of the natural enamel–dentin junction (EDJ), a functionally graded zone that seamlessly integrates two dissimilar tissues [16,17]. Early approaches depended on macromechanical retention through retentive preparation designs, but the demand for minimally invasive prosthetics necessitated innovations in surface treatments and cement chemistry [18,19,20]. Surface roughening treatments, particularly airborne-particle abrasion (sandblasting), are a critically effective and widely validated method for enhancing the bond strength of zirconia-based dental restorations by increasing micromechanical retention and, in some cases, inducing beneficial compressive surface stresses, though the specific protocol must be optimized to avoid excessive surface damage that can compromise flexural strength [21,22,23,24,25,26,27]. The introduction of 10-methacryloyloxydecyl dihydrogen phosphate (MDP), a monomer capable of chemically bonding to zirconia’s oxide layer, revolutionized adhesion by complementing micromechanical retention with stable chemical interactions [28,29,30,31,32]. Despite this advancement, the proliferation of zirconia formulations (3Y-TZP, 4Y-PSZ, 5Y-PSZ) and manufacturing techniques (e.g., milling, additive manufacturing) has introduced new variables that influence bonding efficacy [33,34]. For instance, higher yttria content (5Y-PSZ) enhances translucency but reduces flexural strength, while subtractive manufacturing yields denser interfaces than 3D-printed zirconia, impacting resin infiltration and bond durability [35,36,37,38].
Contemporary bonding protocols now encompass three main dimensions:
- Surface pretreatments, such as tribochemical silica coating (e.g., Rocatec™), nanostructured alumina deposition, or laser ablation, which modify surface energy and topography, effectively creating a micro-rough, silica-rich surface that biomimics the retentive morphology of etched enamel [39,40];
- Primer and cement chemistry, including MDP-based primers and self-adhesive resins (e.g., Panavia V5), which optimize chemical adhesion, forming molecular bridges that emulate the organic–inorganic bonding of the hybrid layer in dentin [41,42];
- Aging resistance, where thermocycling and mechanical fatigue critically influence long-term performance [43,44,45].
- Yet clinical adoption remains inconsistent due to conflicting evidence, technique sensitivity, and a lack of consensus on optimal protocols [46]. For example, while airborne-particle abrasion with alumina enhances bond strength, excessive pressure may compromise the mechanical integrity of translucent zirconia [47,48,49,50]. Similarly, the efficacy of MDP primers varies with zirconia composition and surface treatment, underscoring the need for standardized guidelines [51,52,53,54,55].
This scoping review synthesizes a decade of evidence (2015–2025) to evaluate the interplay between zirconia material science, bonding protocols, and clinical outcomes. Specifically, it aims to map evidence on efficacy of bonding techniques for zirconia-based fixed dental prosthesis. The imperative for optimized bonding extends beyond preventing debonding; it is increasingly important to achieving a biomimetic restoration. A poor interface risks microleakage, secondary caries, pulpitis, and catastrophic failure, while overly aggressive surface treatments may compromise the material’s integrity. As zirconia continues to dominate restorative dentistry, this review maps current evidence, identifies knowledge gaps, and offers evidence-based recommendations to enhance the longevity and predictability of zirconia restorations through biomimetically informed strategies. The figure below represents an analogy of biomimetic bonding interface (Figure 2).
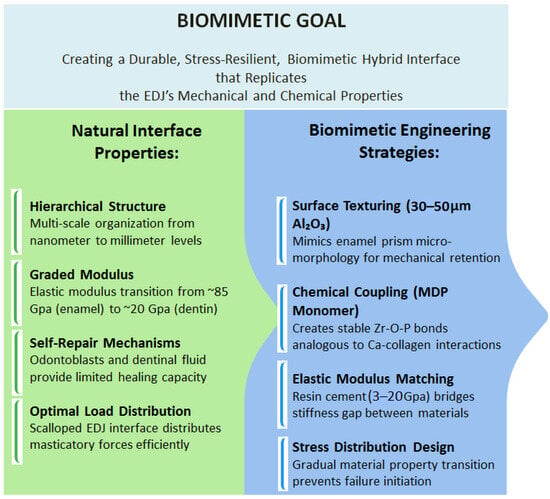
Figure 2.
Biomimetic bonding interface analogy.
2. Materials and Methods
2.1. PRISMA-ScR Compliance
This scoping review adhered to the guidelines outlined by Tricco et al., 2018, in the PRISMA Extension for Scoping Reviews methodology (PRISMA-ScR) [56]. The full checklist is listed in the Supplementary File S1.
2.2. Objective
This scoping review evaluated the evidence on optimal bonding strategies for zirconia fixed restorations, focusing on surface treatments, cementation protocols, and their long-term durability.
2.3. Search Strategy
To ensure methodological rigor while maintaining breadth, this scoping review systematically examined the literature from PubMed, Scopus, Web of Science, and Embase for zirconia, dental bonding, and fixed prostheses (full syntax provided in Supplementary File S2). Searches were conducted on July 2025, capturing advancements in zirconia bonding technologies. The search spanned January 2015–June 2025 and was limited to English-language studies.
The strategy prioritized evidence on adhesive performance while identifying gaps in long-term clinical validation. This systematic approach guaranteed that the review identified the most pertinent and credible evidence while maintaining transparency for reproducibility. By employing a broad yet focused search across major databases, this strategy effectively synthesizes existing knowledge and highlights gaps for future research.
2.4. Eligibility Criteria
This review focused on peer-reviewed studies published in English between 2015 and June 2025. It includes comparative investigations evaluating bonding strategies for zirconia restorations, encompassing both laboratory studies with standardized aging protocols and clinical studies with survival data. Systematic reviews were consulted for contextual background but excluded from primary analysis.
To ensure robust comparisons, selected studies had to report quantitative outcomes including
- Bond strength measurements (shear/microtensile in MPa);
- Clinical performance metrics (survival/debonding rates);
- Durability assessments (thermocycling, water storage, or chewing simulation results);
- Failure mode analyses (adhesive/cohesive/mixed fractures).
The scope specifically examined permanent zirconia restorations, including crowns, fixed dental prostheses, and resin-bonded bridges, while excluding temporary prostheses. Table 1 details the complete eligibility framework with scientific rationale.

Table 1.
Eligibility Criteria with Rationale.
2.5. Literature Screening and Prioritization
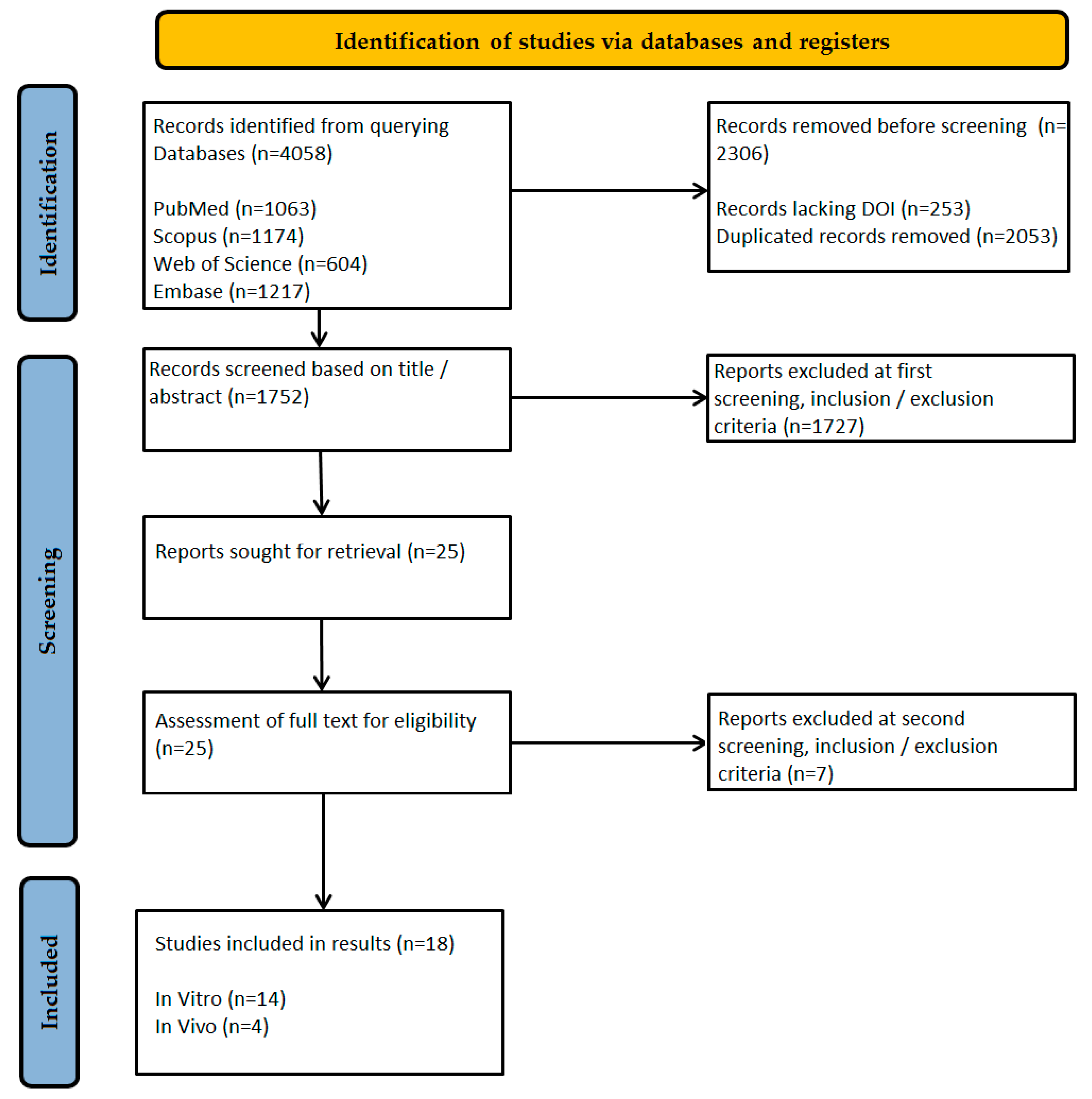
The literature selection was recorded following the PRISMA-ScR protocol flow diagram. To ensure thorough and methodically sound inclusion of relevant studies, this scoping review employed a structured, multi-step screening approach. The preliminary database searches retrieved 4058 records, reflecting widespread scientific interest in zirconia bonding methods for fixed dental prostheses. To streamline further screening, 253 records without a DOI were excluded, as they failed to meet fundamental eligibility criteria.
A thorough deduplication process was then conducted, eliminating 2053 duplicate records using a predefined method. This was executed in Microsoft Excel with a tailored formula to guarantee precise and accurate record handling.
Screening of the remaining 1752 records, based on titles and abstracts, was performed in accordance with the inclusion criteria. Exclusions (n = 1727) were made for studies that (1) examined non-zirconia materials or adhesion methods for dentures; (2) assessed pediatric crowns or lacked a clear bonding methodology (e.g., insufficient details on surface treatment or cementation); or (3) involved animal testing or were published in non-English languages. As a result, 25 studies remained for full-text evaluation.
The final 25 studies were subjected to a strict eligibility assessment. Two reviewers, A.M.D. and O.S., independently evaluated each study, with any disagreements resolved through discussion. Seven records were excluded due to the following reasons:
- Lack of bond strength measurements;
- Absence of an aging protocol;
- No comparison between MDP and the defined* silica-based approaches;
- Animal or in vitro studies lacking clinical applicability;
- Not focused on zirconia bonding;
- Review articles or editorials;
- No standardized bonding protocol.
* For the purposes of this review, “silica-based approaches” were defined as any surface treatment method that deposits or creates a silica layer on the zirconia surface to facilitate silane coupling. This includes, but is not limited to, tribochemical silica coating (e.g., CoJet, Rocatec), plasma spraying, glass fusing (sintering of porcelain layers), and internal coating or “Glaze-On” techniques.
2.6. Quality Assessment of References
Consistent with the objectives of a scoping review, a formal critical appraisal of individual sources of evidence was not conducted, as the goal was to map the available evidence irrespective of its methodological quality. Nevertheless, an extensive review of the data was conducted to fulfill the study’s purpose.
3. Results
3.1. Included Studies
The initial scoping search identified 4058 records across four databases. After deduplication and filtering, 1752 studies were screened based on their titles and abstracts. In accordance with PRISMA ScR guidelines, 25 full-text articles were evaluated for eligibility, with 18 ultimately meeting the inclusion criteria (see Figure 3).
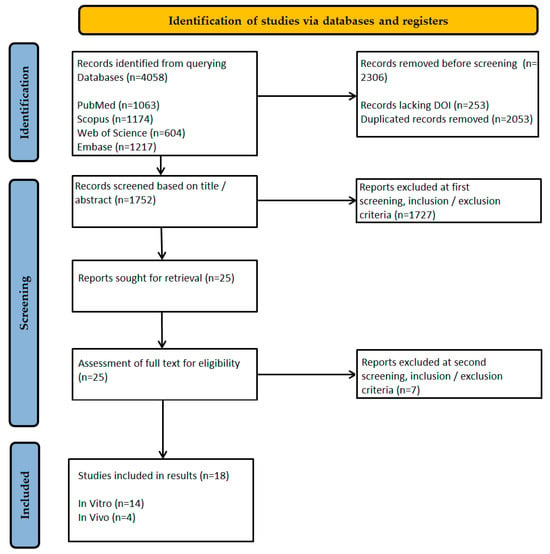
Figure 3.
Flow diagram of the study selection process according to PRISMA ScR guidelines.
3.2. Outline of Included Studies
Of the 18 studies included, 14 were in vitro investigations validated through laboratory bond strength tests (such as shear or push-out tests), while the remaining 4 were in vivo studies (including 2 prospective cohorts, 1 randomized controlled trial, and 1 retrospective study), featuring diverse experimental designs. Consequently, the final set of studies exhibited significant methodological heterogeneity (Table 2).

Table 2.
Incorporation of Different Research Designs.
Most of the evidence was derived from in vitro studies (n = 14), though the inclusion of such diverse experimental approaches provides a realistic view of this study’s goals. As opposed to systematic reviews that aim to address precise research questions, scoping reviews aim to map all available evidence broadly, incorporating various study designs. The key findings from the selected studies are extracted in Table 3.

Table 3.
Selected Literature with Key Findings.
3.3. Overview of Key Findings
The evidence from the included studies was synthesized and is presented herein according to the core objectives of this review: the efficacy of surface treatments, the performance of cementation protocols, and the long-term durability of the resulting bonds. Data on shear bond strength (SBS), failure modes, and clinical outcomes are integrated into this narrative.
It is important to note that the key evidence is based predominantly on in vitro findings, which represents a significant limitation as such studies cannot fully replicate the complex biochemical and biomechanical conditions of the oral environment. Furthermore, the widespread use of shear bond strength tests, while common, is criticized for generating uneven stress distribution at the bonding interface, which may limit the ability to evaluate the true adhesive performance and predict clinical behavior [75]. This issue is further addressed in the discussion section.
3.3.1. Surface Treatments
Surface pretreatment is a fundamental prerequisite for achieving reliable adhesion to zirconia. The evidence consistently demonstrates that micromechanical and chemomechanical interventions significantly outperform untreated surfaces. Air abrasion, particularly with silica-coated alumina particles (tribochemical silicatization) as exemplified by the Rocatec™ system, was found in some studies to increase SBS compared to non-abraded controls [59]. This process is intended to enhance surface roughness and energy, facilitating micromechanical interlocking and providing a silica-rich surface for chemical coupling.
The efficacy of air abrasion was further supported by clinical outcomes. Malgaj et al. reported that nanostructured alumina coating, an advanced air abrasion technique, achieved a clinical survival rate of 93.8% for resin-bonded fixed dental prostheses (RBFDPs), which was comparable to the 86.7% survival rate of conventional airborne-particle abrasion with 50-μm alumina, with no statistically significant difference between the two methods [61]. Beyond mechanical treatments, the critical issue of salivary contamination during clinical try-in procedures was effectively addressed by Kim et al., who demonstrated that a protective ethyl cellulose coating successfully prevented contamination and preserved bond strength, outperforming methods that involved cleaning after contamination had occurred [62].
3.3.2. Cementation Protocols
The choice of cementation protocol, specifically the use of chemical primers, is paramount to achieving high bond strength. Studies uniformly reported that unprimed zirconia yields low and highly variable bond strengths, with SBS values ranging from as low as 2.52 MPa to 33.15 MPa. The application of universal primers containing functional monomers dramatically and significantly improved these outcomes, elevating SBS values to a range of 21.80 to 57.20 MPa [67].
The most effective chemical agent identified across multiple studies was the monomer 10-methacryloyloxydecyl dihydrogen phosphate (MDP). Primers with MDP, such as Clearfil Ceramic Primer Plus, consistently yielded the highest and most durable bond strengths, maintaining efficacy after artificial aging through thermocycling, with reported SBS values exceeding 40 MPa [63]. The superiority of MDP-based primers was also confirmed in the context of endodontic posts, where Z-Prime Plus significantly increased the push-out bond strength of zirconia posts to root dentin [74]. Furthermore, the choice of resin cement itself influences outcomes; Clearfil SA Luting Cement outperformed Panavia F in one study [74], and RelyX Unicem 2 demonstrated significantly higher SBS than MaxCem Elite in another [59], highlighting that the primer–cement combination is a critical factor.
3.3.3. Long-Term Durability
The long-term performance of zirconia bonds is influenced by material composition, manufacturing techniques, and the ability to withstand aging. A key finding is that zirconia’s yttria content directly impacts resin bond stability. Hansson et al. found that 3Y-TZP exhibited the highest SBS after 6 months of water storage (28.98 MPa), which was significantly greater than the bond strengths observed for 4Y-PSZ and 5Y-PSZ (14.35 MPa and 16.05 MPa, respectively) [66]. This trend was corroborated by Suliman et al., who reported that higher yttria content facilitated easier debonding, with Er:YAG laser removal time for 5 mol% Y-TZP (4.03 min) being significantly shorter than for 3 mol% Y-TZP (12.46 min) [69].
The durability of the zirconia–veneer ceramic bond is also affected by manufacturing techniques. Zandinejad et al. determined that milled zirconia substrates provided a superior bond to porcelain (SBS 1.38 MPa) compared to additively manufactured zirconia (SBS 0.68 MPa), a difference that was further exacerbated by thermocycling [64]. While veneering techniques (heat-pressing vs. hand-layering) showed comparable bond strengths [65], the coloring process itself can be detrimental; Celik et al. reported that immersing zirconia in coloring liquid for extended durations (120 s) significantly reduced the SBS of veneering ceramic compared to precolored zirconia [58].
Clinically, the long-term durability of properly bonded zirconia prostheses is excellent. Kern et al. reported a 15-year survival rate of 97.3% for cantilever zirconia RBFDPs, with a retention rate of 82.3% despite some debonding events, the majority of which were successfully rebonded [71]. This outstanding performance is supported by shorter-term studies, such as Yazigi & Kern, who observed a 100% survival rate over a mean period of 53 months [60]. The clinical performance of zirconia RBFDPs was also found to be statistically equivalent to direct composite alternatives over a 3-year period [70].
3.4. Summary of Key Findings About Zirconia-Based FDP Restorations: Parameters and Performance
Table 4 summarizes key findings across major parameters, including primers, surface treatments, veneering techniques, porcelain-zirconia bonding, coloring zirconia, thermal cycling and firings, bioceramic cements, fatigue resistance, clinical RBFDP survival rates, and aging effects related to yttria content.

Table 4.
Summary of Key Findings about Zirconia-Based FDPs Restorations: Parameters and Performance.
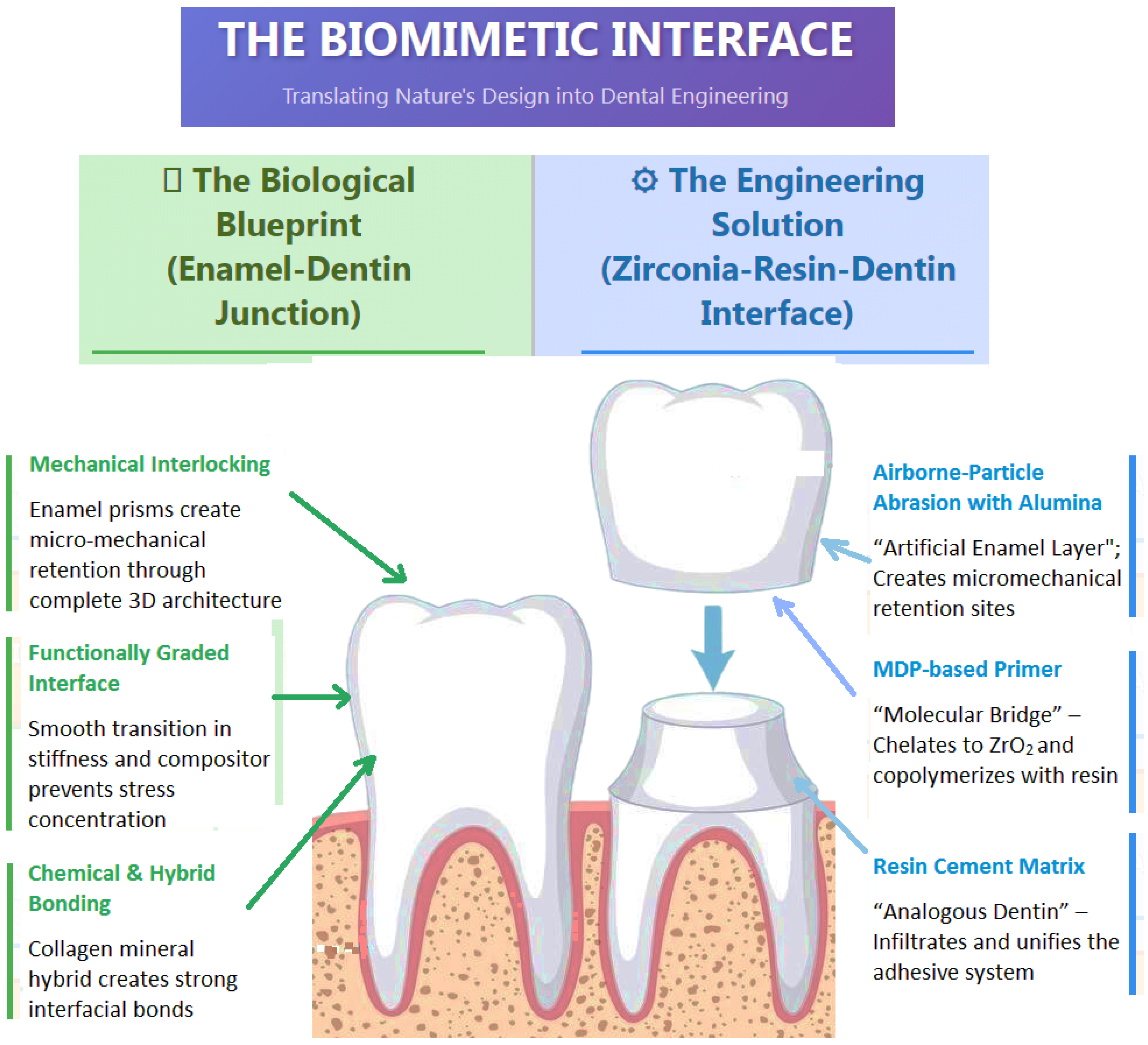
4. Discussion
This scoping review synthesizes evidence on zirconia bonding protocols, cementation strategies, manufacturing techniques, and clinical performance. The following discussion contextualizes key findings, addresses prevailing controversies, and highlights translational implications through a biomimetic lens. The figure below represents a conceptual diagram of analogous biomimetic bonding interfaces to visually articulate the conceptual framework of a “biomimetic lens” (Figure 4).
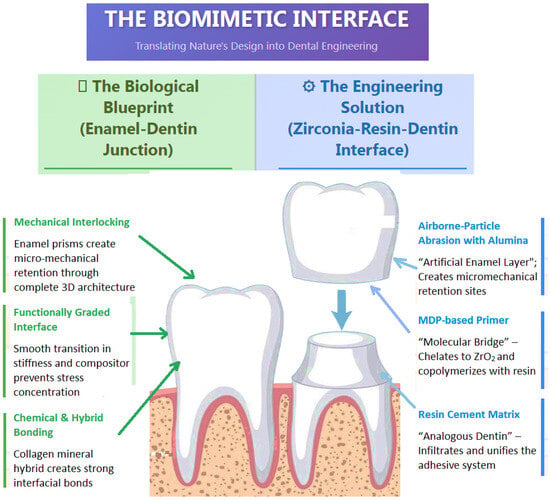
Figure 4.
Depiction of a Biomimetic Hybrid Interface.
4.1. Surface Pretreatments: Efficacy and Trade-Offs
Tribochemical Silica Coating (Rocatec™/CoJet)
Franz et al. (2021) demonstrated superior bond durability with tribochemical silica coating compared to alumina abrasion in their in vitro study, attributed to micromechanical retention and chemical bonding via silica deposition [59]. This process aims to create a biomimetic, silica-rich “artificial enamel” layer on the zirconia surface, making it amenable to conventional silane coupling, a strategy that successfully mimics the bonding protocol for natural silica-based ceramics. This aligns with Prochnow et al. (2025), who reported higher bond strength for 3Y-TZP after CoJet treatment, though translucent zirconias (4Y/5Y-PSZ) showed reduced performance post-aging [76]. Nevertheless, it is paramount to temper the interpretation of these findings. The claim of silica coating superiority often relies on in vitro evidence, and the clinical relevance of silica coating remains debated. Some authors argue that silica particles may not remain firmly embedded in the zirconia surface over the long term, questioning the method’s durability [77]. Furthermore, high clinical failure rates have been reported for resin-bonded FDPs using this method in some studies [78]. Unlike airborne-particle abrasion with alumina, which has been extensively evaluated in long-term clinical trials, robust clinical data for tribochemical silica coating are still lacking. Therefore, it should not be unequivocally stated as a superior method for everyday clinical practice. Quigley et al. (2021) caution that clinical data supporting tribochemical coatings over conventional abrasion remain limited, particularly for monolithic restorations [79].
Nanostructured Alumina Coating (NAC)
Malgaj et al. (2023) found comparable clinical retention between nanostructured alumina and airborne-particle abrasion for high-translucency zirconia (5Y-PSZ), mitigating strength degradation risks [61]. This is critical given Wang et al. (2024)’s emphasis on yttria content’s impact on zirconia’s mechanical properties [80]. However, McLaren et al. (2023) noted that nanostructured coatings may not universally enhance bond strength, as substrate composition (e.g., yttria-stabilized vs. cubic-phase zirconia) influences outcomes [81]. In contrast, Malgaj et al. (2021) reported statistically comparable bonding efficacy across 3Y, 4Y, and 5Y zirconia, helping to balance the perspective on the efficiency of NAC [82].
Ethyl Cellulose Coating
Kim et al. (2022) showed ethyl cellulose coatings effectively prevent salivary contamination, restoring bond strength to the baseline [62]. While promising for trial placements, Blatz et al. (2018) and Han et al. (2022) highlight that such coatings may complicate definitive cementation if not thoroughly removed, risking interfacial voids [83,84].
4.2. Cementation Chemistry: MDP’s Dominance and Alternatives
MDP-Based Primers/Resins
Yagawa et al. (2018) and Steiner et al. (2020) reported hydrolytic stability (>40 MPa) with MDP-containing systems (e.g., Panavia V5) [57,63]. The phosphate group in MDP chelates to zirconia’s surface oxides, while the methacrylate group co-polymerizes with the resin cement. This creates a “molecular bridge” or a synthetic protein-like tether, analogous to how collagen fibers in dentin form a hybrid layer with resin monomers, representing a form of molecular biomimicry [85,86,87]. Shokry et al. (2022) corroborate this, showing Panavia V5 outperformed Duo-Link Universal [88]. However, Guilardi et al. (2022) found that MDP’s efficacy depends on aging conditions, and thermocycling reduced bond strengths by 15–20%, suggesting long-term durability requires combined mechanical and chemical retention [89].
Bioceramic Cements
Dandoulaki et al. (2019) noted bioceramic cements underperformed versus glass ionomers (2.52–5.23 MPa vs. 4.20–6.61 MPa) [73]. Conversely, Aziz & El-Mowafy (2023) reported 100% 5-year survival with self-adhesive resins (RelyX Unicem 2, Panavia SA), questioning the need for bioactive cements in non-carious substrates [90].
4.3. Manufacturing and Veneering: Digital vs. Traditional
Milled vs. Additive-Manufactured (AM) Zirconia
Zandinejad et al. (2025) observed 2x higher porcelain bond strength in milled vs. AM zirconia, attributed to density variations in AM parts [64]. Huang et al. (2024) suggest AM process optimization (e.g., laser parameters) could bridge this gap, but current clinical data are lacking [3].
Digital Veneering
Sim et al. (2016) reported higher bond strength with digital veneering (28.29 MPa vs. 17.21 MPa), likely due to standardized ceramic application and reduced voids [72]. However, Utar et al. (2023) found conventional layering (e.g., IPS e.max Ceram) yielded superior flexural strength versus digitally veneered zirconia, highlighting a trade-off between precision and mechanical resilience [91].
4.4. Aging and Clinical Translation: Bench-to-Bedside Gaps
Yazigi & Kern (2022) correlated in vitro bond strengths >30 MPa with 5-year success rates >95% [60]. However, Elshiyab et al. (2017) noted that aqueous aging protocols often fail to replicate oral conditions (e.g., dynamic loading, pH cycling), potentially overestimating clinical performance [92].
4.5. Limitations of This Scoping Review
While this review maps the current evidence on bonding performance of zirconia-based FDPs restorations, its limitations must be acknowledged. The scope was restricted to English-language literature from the past decade, and the evidence base is predominantly derived from in vitro studies (14 of the 18 included studies), which inherently limits the direct extrapolation of findings to clinical outcomes due to the simulation rather than replication of aging, occlusal forces, and the intraoral environment. A significant constraint is the profound heterogeneity in testing protocols, where discrepancies between shear bond strength and microtensile tests complicate direct comparisons (e.g., Zandinejad et al. vs. Steiner et al.), underscoring an urgent need for standardized methodologies such as those outlined in ISO 29022 [57,64,93]. Furthermore, existing in vitro aging models are often incomplete; for instance, the work of Guilardi et al. (2022) demonstrates that fatigue cycling is a critical factor in resin-zirconia interface failure, a variable not consistently incorporated [89]. Most notably, a substantial gap exists in long-term clinical data, as evidenced by sparse evidence for monolithic zirconia crown survival beyond 10 years (Quigley et al., 2021), despite more robust 15-year data available for resin-bonded fixed dental prostheses (Kern et al., 2025) [71,79] These limitations primarily reflect gaps in the current primary literature rather than methodological flaws in the review itself, highlighting specific areas where future research must focus to strengthen clinical translation.
4.6. Future Directions
Research Priorities:
- Standardized aging protocols: Incorporate more rigorous aging protocols to better simulate long-term oral conditions, such as 37,500 thermocycles to simulate thermal stress, 150 days of water storage for hydrolysis, and 1.2 million load cycles to approximate five years of clinical service [94,95].
- AM zirconia optimization: Improve interfacial bonding through surface functionalization (e.g., laser patterning) [96,97,98].
- RCTs on novel primers/lasers: Compare zirconia primers (e.g., Z-Prime Plus) and Er:YAG debonding efficacy in clinical settings [99].
- Bio-inspired Interfacial Design: Future research should prioritize the development of truly biomimetic interfaces. This includes investigating functionally graded primers that create a stiffness gradient between zirconia and dentin, mimicking the EDJ. Furthermore, exploring bio-adhesive concepts, such as synthetic polymers inspired by mussel adhesive proteins (e.g., catechol-containing polymers), could lead to novel primers with superior binding to zirconia in the wet oral environment [100,101].
4.7. Clinical Recommendations
- For High-Strength Zirconia (3Y-TZP): According to large clinical studies, airborne-particle abrasion (APA) with alumina (e.g., 50-μm, at low pressure) combined with an MDP-based monomer (e.g., Panavia V5) remains the clinically validated gold standard due to its extensive long-term success data [77]. Tribochemical silica coating + MDP cement shows high bond strengths in vitro and can be considered a promising alternative, but its clinical validation is less robust, and it should not yet be viewed as a superior replacement for APA.
- For Translucent Zirconia (5Y-PSZ): Nanostructured alumina or low-pressure airborne abrasion to minimize strength loss [61,69] (Malgaj et al., 2023; Sulaiman et al., 2024).
- For AM Zirconia: Prioritize milled designs until AM process optimization is validated [3] (Huang et al., 2024).
5. Conclusions
While advancements in zirconia bonding are significant, translational challenges persist. Future research must standardize testing, incorporate multifactorial aging, and prioritize long-term clinical trials, particularly for monolithic and AM zirconia. This combined approach achieves the hybrid mechanical–chemical adhesion found in natural biological interfaces best.
- Clinical Recommendations: Airborne-particle abrasion with alumina + MDP-based resin cements remains the gold standard with the strongest clinical evidence. A tribochemical silica coating combined with MDP is a promising laboratory strategy but requires more robust long-term clinical validation before it can be universally recommended
- Research Gaps: Standardized aging protocols, bio-inspired interfacial designs, and RCTs comparing novel lasers/primers are needed.
Combined mechanical–chemical approaches yield the most durable bonds for zirconia restorations. Future studies should prioritize clinical validation, standardized testing, and learning from biological blueprints to create the next generation of adhesive interfaces.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/biomimetics10090632/s1: Supplementary File S1: Prisma ScR Checklist. Supplementary File S2: Search strategy.
Author Contributions
Conceptualization, I.-C.L., R.-I.V. and A.M.D.; methodology, M.S.T., I.-C.L., R.-I.V. and A.M.D.; software, A.M.D., R.-I.V. and A.M.V.; validation, I.-C.L., M.S.T., R.-I.V. and A.M.D.; formal analysis, R.-I.V., O.S. and A.M.D.; investigation, R.-I.V., A.M.D. and L.B.; resources, A.M.D., I.-C.L., A.M.V. and D.A.D.; data curation, L.B., O.S. and D.A.D.; writing—original draft preparation, I.-C.L., R.-I.V. and A.M.D.; writing—review and editing, R.-I.V., A.M.D., M.S.T. and A.M.V.; visualization, R.-I.V., A.M.D., M.S.T. and C.I.C.; supervision, R.-I.V., M.S.T. and A.M.D.; project administration, R.-I.V., A.M.D., D.A.D. and A.M.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
No new data were created.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| MDP | 10-methacryloyloxydecyl dihydrogen phosphate |
| ZrO2 | zirconia |
| MPa | megapascal |
| FDPs | fixed dental prostheses |
| EDJ | enamel–dentin junction |
| 3D | three-dimensional |
| FRC | fiber-reinforced composite |
| RBFDP | resin-Bonded Fixed Dental Prosthesis |
| AM | additively manufactured |
| 3Y-TZP | 3 mol% yttria-stabilized tetragonal zirconia polycrystal |
| 4Y-PSZ | 4 mol% Yttria-stabilized Partially Stabilized Zirconia |
| 5Y-PSZ | 5 mol% yttria-partially stabilized zirconia |
| NAC | nanostructured Alumina Coating |
References
- Aldhuwayhi, S. Zirconia in Dental Implantology: A Review of the Literature with Recent Updates. Bioengineering 2025, 12, 543. [Google Scholar] [CrossRef]
- Singh, P.V.; Reche, A.; Paul, P.; Agarwal, S.; Singh, P.V.; Reche, A.; Paul, P.; Agarwal, S. Zirconia Facts and Perspectives for Biomaterials in Dental Implantology. Cureus 2023, 15, e46828. [Google Scholar] [CrossRef]
- Huang, B.; Chen, M.; Wang, J.; Zhang, X. Advances in Zirconia-Based Dental Materials: Properties, Classification, Applications, and Future Prospects. J. Dent. 2024, 147, 105111. [Google Scholar] [CrossRef]
- Dhamande, M.M.; Beri, A.; Sathe, S.; Jaiswal, T.; Dubey, S.A. Transforming Smiles: A Case Study on Monolithic Zirconia Prosthetic Solutions. Cureus 2024, 16, e57889. [Google Scholar] [CrossRef]
- Hamza, T.A.; Sherif, R.M. Fracture Resistance of Monolithic Glass-Ceramics Versus Bilayered Zirconia-Based Restorations. J. Prosthodont. 2019, 28, e259–e264. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Ghulam, O.; Krsoum, M.; Binmahmoud, S.; Taher, H.; Elmalky, W.; Zafar, M.S. Revolution of Current Dental Zirconia: A Comprehensive Review. Molecules 2022, 27, 1699. [Google Scholar] [CrossRef]
- Gautam, C.; Joyner, J.; Gautam, A.; Rao, J.; Vajtai, R. Zirconia Based Dental Ceramics: Structure, Mechanical Properties, Biocompatibility and Applications. Dalton Trans. 2016, 45, 19194–19215. [Google Scholar] [CrossRef]
- Golriz, N.; Hosseinabadi, N. Additive Manufacturing of Ceria and Yttria Incorporated Toughened Monolithic Zirconia Dental Ceramic Crowns: In Vitro Simulated Aging Behavior. J. Prosthet. Dent. 2024, 132, 624.e1–624.e12. [Google Scholar] [CrossRef] [PubMed]
- Pyo, S.-W.; Park, K.; Daher, R.; Kwon, H.-B.; Han, J.-S.; Lee, J.-H. Comparison of the Clinical Outcomes of Resin-Modified Glass Ionomer and Self-Adhesive Resin Cementations for Full-Coverage Zirconia Restorations. J. Dent. 2023, 135, 104558. [Google Scholar] [CrossRef] [PubMed]
- Benalcázar-Jalkh, E.B.; Bergamo, E.T.P.; Campos, T.M.B.; Coelho, P.G.; Sailer, I.; Yamaguchi, S.; Alves, L.M.M.; Witek, L.; Tebcherani, S.M.; Bonfante, E.A. A Narrative Review on Polycrystalline Ceramics for Dental Applications and Proposed Update of a Classification System. Materials 2023, 16, 7541. [Google Scholar] [CrossRef] [PubMed]
- Thompson, J.Y.; Stoner, B.R.; Piascik, J.R.; Smith, R. Adhesion/Cementation to Zirconia and Other Non-Silicate Ceramics: Where Are We Now? Dent. Mater. 2011, 27, 71–82. [Google Scholar] [CrossRef] [PubMed]
- Scaminaci Russo, D.; Cinelli, F.; Sarti, C.; Giachetti, L. Adhesion to Zirconia: A Systematic Review of Current Conditioning Methods and Bonding Materials. Dent. J. 2019, 7, 74. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, N.; Ghosh, A. Current Scenario on Adhesion to Zirconia; Surface Pretreatments and Resin Cements: A Systematic Review. J. Indian Prosthodont. Soc. 2022, 22, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Cavalcanti, A.N.; Foxton, R.M.; Watson, T.F.; Oliveira, M.T.; Giannini, M.; Marchi, G.M. Bond Strength of Resin Cements to a Zirconia Ceramic with Different Surface Treatments. Oper. Dent. 2009, 34, 280–287. [Google Scholar] [CrossRef]
- Duplák, J.; Mikuláško, S.; Dupláková, D.; Yeromina, M.; Kaščák, R. Analysis of a Regression Model for Creating Surface Microgeometry after Machining Zirconia YML Used for Dental Application. Biomimetics 2024, 9, 473. [Google Scholar] [CrossRef]
- Xu, C.; Yao, X.; Walker, M.P.; Wang, Y. Chemical/Molecular Structure of the Dentin–Enamel Junction Is Dependent on the Intratooth Location. Calcif. Tissue Int. 2009, 84, 221–228. [Google Scholar] [CrossRef]
- Li, Q.; Liu, Y.; Zhao, D.; Yang, Y.; Liu, Q.; Zhang, Y.; Wu, J.; Dong, Z. Digital Light Printing of Zirconia/Resin Composite Material with Biomimetic Graded Design for Dental Application. Dent. Mater. 2025, 41, 16–27. [Google Scholar] [CrossRef]
- Maravic, T.; Mazzitelli, C.; Mayer-Santos, E.; Mancuso, E.; Gracis, S.; Breschi, L.; Fuzzi, M. Current Trends for Cementation in Prosthodontics: Part 1—The Substrate. Polymers 2025, 17, 566. [Google Scholar] [CrossRef]
- Barwacz, C.A.; Hernandez, M.; Husemann, R.H. Minimally Invasive Preparation and Design of a Cantilevered, All-Ceramic, Resin-Bonded, Fixed Partial Denture in the Esthetic Zone: A Case Report and Descriptive Review. J. Esthet. Restor. Dent. 2014, 26, 314–323. [Google Scholar] [CrossRef]
- Alomran, W.K.; Nizami, M.Z.I.; Xu, H.H.K.; Sun, J. Evolution of Dental Resin Adhesives—A Comprehensive Review. J. Funct. Biomater. 2025, 16, 104. [Google Scholar] [CrossRef]
- Roy, A.K.; Prasad, G.N.; Bhagat, T.V.; Chaturvedi, S.; Gurumurthy, V.; Vyas, R.; Vaddamanu, S.K.; Das, G. Analysis of Surface Conditioning Methods on Core-Veneer Bond Strength of CAD/CAM Zirconia Restorations. Technol. Health Care 2021, 29, 467–477. [Google Scholar] [CrossRef]
- Inokoshi, M.; Yoshihara, K.; Nagaoka, N.; Nakanishi, M.; De Munck, J.; Minakuchi, S.; Vanmeensel, K.; Zhang, F.; Yoshida, Y.; Vleugels, J.; et al. Structural and Chemical Analysis of the Zirconia–Veneering Ceramic Interface. J. Dent. Res. 2016, 95, 102–109. [Google Scholar] [CrossRef]
- Naji, G.A.-H.; Omar, R.A.; Yahya, R. Influence of Sodalite Zeolite Infiltration on the Coefficient of Thermal Expansion and Bond Strength of All-Ceramic Dental Prostheses. J. Mech. Behav. Biomed. Mater. 2017, 67, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Fornaini, C.; Poli, F.; Merigo, E.; Lutey, A.; Cucinotta, A.; Chevalier, M.; Mckee, S.; Brulat, N.; Rocca, J.-P.; Trevisi, G. Nanosecond Pulsed Fiber Laser Irradiation for Enhanced Zirconia Crown Adhesion: Morphological, Chemical, Thermal and Mechanical Analysis. J. Photochem. Photobiol. B Biol. 2021, 219, 112189. [Google Scholar] [CrossRef] [PubMed]
- Kurtulmus-Yilmaz, S.; Aktore, H. Effect of the Application of Surface Treatments before and after Sintering on the Flexural Strength, Phase Transformation and Surface Topography of Zirconia. J. Dent. 2018, 72, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Bergemann, C.; Duske, K.; Nebe, J.B.; Schöne, A.; Bulnheim, U.; Seitz, H.; Fischer, J. Microstructured Zirconia Surfaces Modulate Osteogenic Marker Genes in Human Primary Osteoblasts. J. Mater. Sci. Mater. Med. 2015, 26, 26. [Google Scholar] [CrossRef]
- Al-Amari, A.S.; Saleh, M.S.; Albadah, A.A.; Almousa, A.A.; Mahjoub, W.K.; Al-Otaibi, R.M.; Alanazi, E.M.; Alshammari, A.K.; Malki, A.T.; Alghelaiqah, K.F.; et al. A Comprehensive Review of Techniques for Enhancing Zirconia Bond Strength: Current Approaches and Emerging Innovations. Cureus 2024, 16, e70893. [Google Scholar] [CrossRef]
- Awad, M.M.; Alhalabi, F.; Alzahrani, K.M.; Almutiri, M.; Alqanawi, F.; Albdiri, L.; Alshehri, A.; Alrahlah, A.; Ahmed, M.H. 10-Methacryloyloxydecyl Dihydrogen Phosphate (10-MDP)-Containing Cleaner Improves Bond Strength to Contaminated Monolithic Zirconia: An In-Vitro Study. Materials 2022, 15, 1023. [Google Scholar] [CrossRef]
- Jo, E.-H.; Huh, Y.-H.; Ko, K.-H.; Park, C.-J.; Cho, L.-R. Effect of Liners and Primers on Tensile Bond Strength between Zirconia and Resin-Based Luting Agent. J. Adv. Prosthodont. 2018, 10, 374. [Google Scholar] [CrossRef]
- Llerena-Icochea, A.; Costa, R.; Borges, A.; Bombonatti, J.; Furuse, A. Bonding Polycrystalline Zirconia with 10-MDP–Containing Adhesives. Oper. Dent. 2017, 42, 335–341. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.; Kim, R.H.; Lee, S.C.; Lee, T.K.; Hayashi, M.; Yu, B.; Jo, D.-W. Evaluation of Tensile Bond Strength between Self-Adhesive Resin Cement and Surface-Pretreated Zirconia. Materials 2022, 15, 3089. [Google Scholar] [CrossRef]
- Koko, M.; Takagaki, T.; Abdou, A.; Wada, T.; Nikaido, T.; Tagami, J. Influence of 10-Methacryloyloxydecyl Dihydrogen Phosphate (MDP) Incorporated Experimental Cleaners on the Bonding Performance of Saliva-Contaminated Zirconia Ceramic. Clin. Oral Investig. 2022, 26, 1785–1795. [Google Scholar] [CrossRef] [PubMed]
- Ruggiero, M.M.; Souza, L.V.S.; Magno, M.B.; Song, X.; Maia, L.C.; Cury, A.A.D.B.; Zhang, Y. Is Additive Manufacturing of Dental Zirconia Comparable to Subtractive Methods When Considering Printing Orientation and Layer Thickness? A Systematic Review and Meta-Analysis. J. Esthet. Restor. Dent. 2025; early view. [Google Scholar] [CrossRef]
- Alageel, O.; Alfrisany, N.; Alshamrani, A.; Alsadon, O. The Impact of Additive and Subtractive Manufacturing on the Adhesion and Durability of Titanium–Zirconia Restorative Materials. J. Funct. Biomater. 2025, 16, 257. [Google Scholar] [CrossRef]
- Li, Q.-L.; Jiang, Y.-Y.; Wei, Y.-R.; Swain, M.V.; Yao, M.-F.; Li, D.-S.; Wei, T.; Jian, Y.-T.; Zhao, K.; Wang, X.-D. The Influence of Yttria Content on the Microstructure, Phase Stability and Mechanical Properties of Dental Zirconia. Ceram. Int. 2022, 48, 5361–5368. [Google Scholar] [CrossRef]
- da Silva, A.O.; Fiorin, L.; Faria, A.C.L.; Ribeiro, R.F.; Rodrigues, R.C.S. Translucency and Mechanical Behavior of Partially Stabilized Monolithic Zirconia after Staining, Finishing Procedures and Artificial Aging. Sci. Rep. 2022, 12, 16094. [Google Scholar] [CrossRef]
- Alghauli, M.A.; Alqutaibi, A.Y.; Wille, S.; Kern, M. The Physical-Mechanical Properties of 3D-Printed versus Conventional Milled Zirconia for Dental Clinical Applications: A Systematic Review with Meta-Analysis. J. Mech. Behav. Biomed. Mater. 2024, 156, 106601. [Google Scholar] [CrossRef] [PubMed]
- Moon, J.-M.; Jeong, C.-S.; Lee, H.-J.; Bae, J.-M.; Choi, E.-J.; Kim, S.-T.; Park, Y.-B.; Oh, S.-H. A Comparative Study of Additive and Subtractive Manufacturing Techniques for a Zirconia Dental Product: An Analysis of the Manufacturing Accuracy and the Bond Strength of Porcelain to Zirconia. Materials 2022, 15, 5398. [Google Scholar] [CrossRef]
- Conner, C.; Andretti, F.; Hernandez, A.I.; Rojas-Rueda, S.; Azpiazu-Flores, F.X.; Morrow, B.R.; Garcia-Godoy, F.; Jurado, C.A.; Alshabib, A. Surface Evaluation of a Novel Acid-Etching Solution for Zirconia and Lithium Disilicate. Materials 2025, 18, 2912. [Google Scholar] [CrossRef] [PubMed]
- Lima, R.B.W.; Leite, J.V.C.; Santos, J.V.D.N.; Barbosa, L.M.M.; Neto, H.N.M.; Da Silva, J.G.R.; Muniz, I.D.A.F.; Campos, D.E.S.; De Souza, G.M. Tribochemical Silica-Coating or Alumina Blasting for Zirconia Bonding? A Systematic Review of in Vitro Studies. Int. J. Adhes. Adhes. 2024, 129, 103554. [Google Scholar] [CrossRef]
- Wongkamhaeng, K.; Poomparnich, K.; Chitkraisorn, T.; Boonpitak, K.; Tosiriwatanapong, T. Effect of Combining Different 10-MDP-Containing Primers and Cement Systems on Shear Bond Strength between Resin Cement and Zirconia. BMC Oral Health 2025, 25, 206. [Google Scholar] [CrossRef]
- Li, X.; Liang, S.; Inokoshi, M.; Zhao, S.; Hong, G.; Yao, C.; Huang, C. Different Surface Treatments and Adhesive Monomers for Zirconia-Resin Bonds: A Systematic Review and Network Meta-Analysis. Jpn. Dent. Sci. Rev. 2024, 60, 175–189. [Google Scholar] [CrossRef]
- Prado, P.H.C.O.; Dapieve, K.S.; Campos, T.M.B.; Valandro, L.F.; Melo, R.M.D. Effect of Hydrothermal and Mechanical Aging on the Fatigue Performance of High-Translucency Zirconias. Dent. Mater. 2022, 38, 1060–1071. [Google Scholar] [CrossRef]
- Yang, Z.; Liu, H. Effects of Thermal Aging on the Cyclic Thermal Shock Behavior of Oxide/Oxide Ceramic Matrix Composites. Mater. Sci. Eng. A 2020, 769, 138494. [Google Scholar] [CrossRef]
- Unalan Degirmenci, B.; Degirmenci, A.; Seyfioglu Polat, Z. The Influence of Thermocycling and Ultraviolet Aging on Surface Characteristics and the Repair Bond Strength of CAD/CAM Resin Nanoceramics. J. Funct. Biomater. 2025, 16, 156. [Google Scholar] [CrossRef]
- Kyaw, O.; Inokoshi, M.; Kanazawa, M. Tribological Aspects of Enamel Wear Caused by Zirconia and Lithium Disilicate: A Meta-Narrative Review. Jpn. Dent. Sci. Rev. 2024, 60, 258–270. [Google Scholar] [CrossRef]
- Sanon, C.; Chevalier, J.; Douillard, T.; Cattani-Lorente, M.; Scherrer, S.S.; Gremillard, L. A New Testing Protocol for Zirconia Dental Implants. Dent. Mater. 2015, 31, 15–25. [Google Scholar] [CrossRef]
- Camposilvan, E.; Leone, R.; Gremillard, L.; Sorrentino, R.; Zarone, F.; Ferrari, M.; Chevalier, J. Aging Resistance, Mechanical Properties and Translucency of Different Yttria-Stabilized Zirconia Ceramics for Monolithic Dental Crown Applications. Dent. Mater. 2018, 34, 879–890. [Google Scholar] [CrossRef]
- Schepke, U.; Meijer, H.J.; Vermeulen, K.M.; Raghoebar, G.M.; Cune, M.S. Clinical Bonding of R Esin N Ano C Eramic Restorations to Zirconia Abutments: A Case Series Within a Randomized Clinical Trial. Clin. Implant Dent. Relat. Res. 2016, 18, 984–992. [Google Scholar] [CrossRef]
- Mazzoleni, S.; Stellini, E.; Ludovichetti, F.S.; Signoriello, A.G.; Positello, P.; Bertolini, R.; Pezzato, L.; Gracco, A.A. Paedodontic Preformed Crowns in Primary Teeth and Relative Degree of Dental Wear. Eur. J. Paediatr. Dent. 2024, 25, 1. [Google Scholar] [CrossRef]
- Özcan, M.; Jonasch, M. Effect of Cyclic Fatigue Tests on Aging and Their Translational Implications for Survival of All-Ceramic Tooth-Borne Single Crowns and Fixed Dental Prostheses. J. Prosthodont. 2018, 27, 364–375. [Google Scholar] [CrossRef]
- Jung, R.E.; Grohmann, P.; Sailer, I.; Steinhart, Y.; Fehér, A.; Hämmerle, C.; Strub, J.R.; Kohal, R. Evaluation of a One-piece Ceramic Implant Used for Single-tooth Replacement and Three-unit Fixed Partial Dentures: A Prospective Cohort Clinical Trial. Clin. Oral Implant Res. 2016, 27, 751–761. [Google Scholar] [CrossRef]
- Gunge, H.; Ogino, Y.; Kihara, M.; Tsukiyama, Y.; Koyano, K. Retrospective Clinical Evaluation of Posterior Monolithic Zirconia Restorations after 1 to 3.5 Years of Clinical Service. J. Oral Sci. 2018, 60, 154–158. [Google Scholar] [CrossRef]
- Pilo, R.; Harel, N.; Nissan, J.; Levartovsky, S. The Retentive Strength of Cemented Zirconium Oxide Crowns after Dentin Pretreatment with Desensitizing Paste Containing 8% Arginine and Calcium Carbonate. Int. J. Mol. Sci. 2016, 17, 426. [Google Scholar] [CrossRef]
- Rathmann, F.; Bömicke, W.; Rammelsberg, P.; Ohlmann, B. Veneered Zirconia Inlay-Retained Fixed Dental Prostheses: 10-Year Results from a Prospective Clinical Study. J. Dent. 2017, 64, 68–72. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Steiner, R.; Heiss-Kisielewsky, I.; Schwarz, V.; Schnabl, D.; Dumfahrt, H.; Laimer, J.; Steinmassl, O.; Steinmassl, P. Zirconia Primers Improve the Shear Bond Strength of Dental Zirconia. J. Prosthodont. 2020, 29, 62–68. [Google Scholar] [CrossRef]
- Celik, S.; Ucar, Y.; Ekren, O. Effect of Coloring Liquids on Color of Zirconia Frameworks and Bond Strength of Zirconia/Veneering Ceramic. J. Prosthet. Dent. 2020, 124, 110–115. [Google Scholar] [CrossRef]
- Franz, A.; Winkler, O.; Lettner, S.; Öppinger, S.; Hauser, A.; Haidar, M.; Moritz, A.; Watts, D.C.; Schedle, A. Optimizing the Fitting-Surface Preparation of Zirconia Restorations for Bonding to Dentin. Dent. Mater. 2021, 37, 464–476. [Google Scholar] [CrossRef] [PubMed]
- Yazigi, C.; Kern, M. Clinical Evaluation of Zirconia Cantilevered Single-Retainer Resin-Bonded Fixed Dental Prostheses Replacing Missing Canines and Posterior Teeth. J. Dent. 2022, 116, 103907. [Google Scholar] [CrossRef] [PubMed]
- Malgaj, T.; Abram, A.; Kocjan, A.; Jevnikar, P. Influence of Nanostructured Alumina Coating on the Clinical Performance of Zirconia Cantilevered Resin-Bonded Fixed Dental Prostheses: Up to 3-Year Results of a Prospective, Randomized, Controlled Clinical Trial. J. Prosthet. Dent. 2023, 129, 725–731. [Google Scholar] [CrossRef]
- Kim, H.-J.; Ferracane, J.L.; Park, M.; Choi, K.-K. Effect of Ethyl Cellulose Coating as an Evaluation Agent against Contamination on the Bond Strength of Zirconia Restorations: An in Vitro Study. J. Prosthet. Dent. 2022, 127, 766.e1–766.e9. [Google Scholar] [CrossRef]
- Yagawa, S.; Komine, F.; Fushiki, R.; Kubochi, K.; Kimura, F.; Matsumura, H. Effect of Priming Agents on Shear Bond Strengths of Resin-Based Luting Agents to a Translucent Zirconia Material. J. Prosthodont. Res. 2018, 62, 204–209. [Google Scholar] [CrossRef]
- Zandinejad, A.; Khanlar, L.N.; Barmak, A.B.; Ikeda, M.; Tagami, J.; Masri, R. Shear Bond Strength of Porcelain to Milled and Stereolithography Additively Manufactured Zirconia with and without Surface Treatment: An in Vitro Study. J. Prosthet. Dent. 2025, 133, 273–279. [Google Scholar] [CrossRef]
- Teng, W.S.; Yew, H.Z.; Jamadon, N.H.; Qamaruz Zaman, J.; Meor Ahmad, M.I.; Muchtar, A. Effect of Porcelain Veneering Technique in Bilayered Zirconia on Bond Strength and Residual Stress Distribution. J. Mech. Behav. Biomed. Mater. 2024, 151, 106361. [Google Scholar] [CrossRef] [PubMed]
- Hansson, M.; Ågren, M. Shear Bond Strength of Adhesive Cement to Zirconia: Effect of Added Proportion of Yttria for Stabilization. J. Prosthet. Dent. 2024, 131, 934.e1–934.e7. [Google Scholar] [CrossRef] [PubMed]
- Cadore-Rodrigues, A.C.; Machry, R.V.; Zucuni, C.P.; Pereira, G.K.R.; Valandro, L.F. Grinding and Polishing of the Inner Surface of Monolithic Simplified Restorations Made of Zirconia Polycrystals and Lithium Disilicate Glass-Ceramic: Effects on the Load-Bearing Capacity under Fatigue of the Bonded Restorations. J. Mech. Behav. Biomed. Mater. 2021, 124, 104833. [Google Scholar] [CrossRef]
- Hensel, J.; Reise, M.; Liebermann, A.; Buser, R.; Stawarczyk, B. Impact of Multiple Firings on Thermal Properties and Bond Strength of Veneered Zirconia Restorations. J. Mech. Behav. Biomed. Mater. 2022, 128, 105134. [Google Scholar] [CrossRef] [PubMed]
- Suliman, S.; Sulaiman, T.A.; Deeb, J.G.; Abdulmajeed, A.; Abdulmajeed, A.; Närhi, T. Er:YAG Laser Debonding of Zirconia and Lithium Disilicate Restorations. J. Prosthet. Dent. 2024, 131, 253.e1–253.e6. [Google Scholar] [CrossRef]
- Sato, T.; Hosaka, K.; Tagami, J.; Tashiro, H.; Miki, H.; Otani, K.; Nishimura, M.; Takahashi, M.; Shimada, Y.; Ikeda, M. Clinical Evaluation of Direct Composite versus Zirconia Resin-Bonded Fixed Dental Prostheses for a Single Missing Anterior Tooth: A Short-Term Multicenter Retrospective Study. J. Dent. 2024, 151, 105401. [Google Scholar] [CrossRef]
- Kern, M.; Türp, L.; Yazigi, C. Long-Term Outcome of Anterior Cantilever Zirconia Ceramic Resin-Bonded Fixed Dental Prostheses: Influence of the Pontic Location. J. Prosthet. Dent. 2025, 133, 1017–1023. [Google Scholar] [CrossRef]
- Sim, J.-Y.; Lee, W.-S.; Kim, J.-H.; Kim, H.-Y.; Kim, W.-C. Evaluation of Shear Bond Strength of Veneering Ceramics and Zirconia Fabricated by the Digital Veneering Method. J. Prosthodont. Res. 2016, 60, 106–113. [Google Scholar] [CrossRef]
- Dandoulaki, C.; Rigos, A.E.; Kontonasaki, E.; Karagiannis, V.; Kokoti, M.; Theodorou, G.S.; Papadopoulou, L.; Koidis, P. In Vitro Evaluation of the Shear Bond Strength and Bioactivity of a Bioceramic Cement for Bonding Monolithic Zirconia. J. Prosthet. Dent. 2019, 122, 167.e1–167.e10. [Google Scholar] [CrossRef]
- Torabi Ardakani, M.; Giti, R.; Taghva, M.; Javanmardi, S. Effect of a Zirconia Primer on the Push-out Bond Strength of Zirconia Ceramic Posts to Root Canal Dentin. J. Prosthet. Dent. 2015, 114, 398–402. [Google Scholar] [CrossRef]
- Kelly, J.R.; Benetti, P.; Rungruanganunt, P.; Bona, A.D. The Slippery Slope—Critical Perspectives on in Vitro Research Methodologies. Dent. Mater. 2012, 28, 41–51. [Google Scholar] [CrossRef]
- Prochnow, F.H.; Weber, K.R.; Rezende, C.E.; Kaizer, M.R.; Gonzaga, C.C. Air Abrasion vs. Tribochemical Silica Coating: Effect on Translucent Zirconia Bond Strength. Eur. J. Prosthodont. Restor. Dent. 2025, 33, 199. [Google Scholar] [CrossRef]
- Kern, M. Bonding to Oxide Ceramics—Laboratory Testing versus Clinical Outcome. Dent. Mater. 2015, 31, 8–14. [Google Scholar] [CrossRef]
- Ohlmann, B.; Rammelsberg, P.; Schmitter, M.; Schwarz, S.; Gabbert, O. All-Ceramic Inlay-Retained Fixed Partial Dentures: Preliminary Results from a Clinical Study. J. Dent. 2008, 36, 692–696. [Google Scholar] [CrossRef]
- Quigley, N.P.; Loo, D.S.S.; Choy, C.; Ha, W.N. Clinical Efficacy of Methods for Bonding to Zirconia: A Systematic Review. J. Prosthet. Dent. 2021, 125, 231–240. [Google Scholar] [CrossRef]
- Wang, L.; Wang, K.; Sheng, Y.; Hao, Z.; Tang, W.; Dou, R. The Effect of Phase Contents on the Properties of Yttria Stabilized Zirconia Dental Materials Fabricated by Stereolithography-Based Additive Manufacturing. J. Mech. Behav. Biomed. Mater. 2024, 150, 106313. [Google Scholar] [CrossRef]
- McLaren, E.A.; Maharishi, A.; White, S.N. Influence of Yttria Content and Surface Treatment on the Strength of Translucent Zirconia Materials. J. Prosthet. Dent. 2023, 129, 638–643. [Google Scholar] [CrossRef]
- Malgaj, T.; Mirt, T.; Kocjan, A.; Jevnikar, P. The Influence of Nanostructured Alumina Coating on Bonding and Optical Properties of Translucent Zirconia Ceramics: In Vitro Evaluation. Coatings 2021, 11, 1126. [Google Scholar] [CrossRef]
- Blatz, M.B.; Vonderheide, M.; Conejo, J. The Effect of Resin Bonding on Long-Term Success of High-Strength Ceramics. J. Dent. Res. 2018, 97, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Han, S.-H.; Shimada, Y.; Sadr, A.; Tagami, J.; Tabata, T.; Nakagawa, H.; Yang, S.-E. Effects of Material Thickness and Pretreatment on the Interfacial Gap of Translucent Zirconia Restorations with Self-Adhesive Resin Cement. Oper. Dent. 2022, 47, 535–548. [Google Scholar] [CrossRef]
- Nagaoka, N.; Yoshihara, K.; Feitosa, V.P.; Tamada, Y.; Irie, M.; Yoshida, Y.; Van Meerbeek, B.; Hayakawa, S. Chemical Interaction Mechanism of 10-MDP with Zirconia. Sci. Rep. 2017, 7, 45563. [Google Scholar] [CrossRef]
- Gungormus, M.; Tulumbaci, F. Peptide-Assisted Pre-Bonding Remineralization of Dentin to Improve Bonding. J. Mech. Behav. Biomed. Mater. 2021, 113, 104119. [Google Scholar] [CrossRef]
- Tanış, M.Ç.; Akay, C.; Karakış, D. Resin Cementation of Zirconia Ceramics with Different Bonding Agents. Biotechnol. Biotechnol. Equip. 2015, 29, 363–367. [Google Scholar] [CrossRef]
- Shokry, M.; Al-Zordk, W.; Ghazy, M. Retention Strength of Monolithic Zirconia Crowns Cemented with Different Primer-Cement Systems. BMC Oral Health 2022, 22, 187. [Google Scholar] [CrossRef]
- Guilardi, L.; Pereira, G.; Giordani, J.; Kleverlaan, C.; Valandro, L.; Rippe, M. Cement Choice and the Fatigue Performance of Monolithic Zirconia Restorations. Oper. Dent. 2022, 47, 461–472. [Google Scholar] [CrossRef]
- Aziz, A.M.; El-Mowafy, O. Clinical Evaluation of Zirconia Crowns Cemented with Two Different Resin Cements: A Retrospective Study. J. Oral Rehabil. 2023, 50, 1481–1486. [Google Scholar] [CrossRef]
- Utar, M.; Demirtağ, Z. Four-point Flexural Strength and Microtensile Bond Strength of Digitally and Conventionally Veneered Zirconia. Eur. J. Oral Sci. 2023, 131, e12926. [Google Scholar] [CrossRef]
- Elshiyab, S.H.; Nawafleh, N.; George, R. Survival and Testing Parameters of Zirconia-based Crowns under Cyclic Loading in an Aqueous Environment: A Systematic Review. J. Investig. Clin. Dent. 2017, 8, e12261. [Google Scholar] [CrossRef] [PubMed]
- ISO 29022:2013; Dentistry—Adhesion—Notched-Edge Shear Bond Strength Test. ISO: Geneva, Switzerland, 2013. Available online: https://www.iso.org/standard/45285.html (accessed on 2 July 2025).
- Behr, M.; Hindelang, U.; Rosentritt, M.; Lang, R.; Handel, G. Comparison of Failure Rates of Adhesive-Fixed Partial Dentures for in Vivo and in Vitro Studies. Clin. Oral Investig. 2000, 4, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Behr, M.; Leibrock, A.; Stich, W.; Rammelsberg, P.; Rosentritt, M.; Handel, G. Adhesive-Fixed Partial Dentures in Anterior and Posterior Areas. Clin. Oral Investig. 1998, 2, 31–35. [Google Scholar] [CrossRef]
- Sahoo, N.; Carvalho, O.; Özcan, M.; Silva, F.; Souza, J.C.M.; Lasagni, A.-F.; Henriques, B. Ultrashort Pulse Laser Patterning of Zirconia (3Y-TZP) for Enhanced Adhesion to Resin-Matrix Cements Used in Dentistry: An Integrative Review. J. Mech. Behav. Biomed. Mater. 2023, 143, 105943. [Google Scholar] [CrossRef]
- Cioloca Holban, C.; Tatarciuc, M.; Vitalariu, A.M.; Vasluianu, R.-I.; Antohe, M.; Diaconu, D.A.; Stamatin, O.; Dima, A.M. Three-Dimensional Printing and CAD/CAM Milling in Prosthodontics: A Scoping Review of Key Metrics Towards Future Perspectives. J. Clin. Med. 2025, 14, 4837. [Google Scholar] [CrossRef]
- Yoon, J.-Y. Improving Zirconia–Resin Cement Bonding Through Laser Surface Texturing: A Comparative Study. Prosthesis 2025, 7, 19. [Google Scholar] [CrossRef]
- Jiang, L.; Li, X.; Lu, Z.; Yang, S.; Chen, R.; Yu, H. Er:YAG Laser Settings for Debonding Zirconia Restorations: An in Vitro Study. J. Mech. Behav. Biomed. Mater. 2024, 151, 106331. [Google Scholar] [CrossRef]
- Du, J.; Niu, X.; Soboyejo, W. Bioinspired Design of Dental Functionally Graded Multilayer Structures. In Bioinspired Structures and Design; Soboyejo, W., Daniel, L., Eds.; Cambridge University Press: Cambridge, UK, 2020; pp. 140–166. ISBN 9781139058995. [Google Scholar]
- Yun, J.; Ge, R.; Tsoi, J.K.H.; Lu, Y.; Guo, S.; Guo, J.; Wang, Y. Design and Manufacturing of Bio-Inspired Functionally Graded Ceramic-Reinforced Resin Post-and-Core Restorations. Compos. Part A Appl. Sci. Manuf. 2025, 194, 108889. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).