Incorporation of Chitosan Nanoparticles into a Cold-Cure Orthodontic Acrylic Resin: Effects on Mechanical Properties
Abstract
1. Introduction
2. Materials and Methods
- Group 1: acrylic resin (control group)
- Group 2: acrylic resin with 0.5% chitosan NPs
- Group 3: acrylic resin with 1% chitosan NPs
- Group 4: acrylic resin with 2% chitosan NPs
- Group 5: acrylic resin with 4% chitosan NPs.
2.1. Preparation of Chitosan NPs
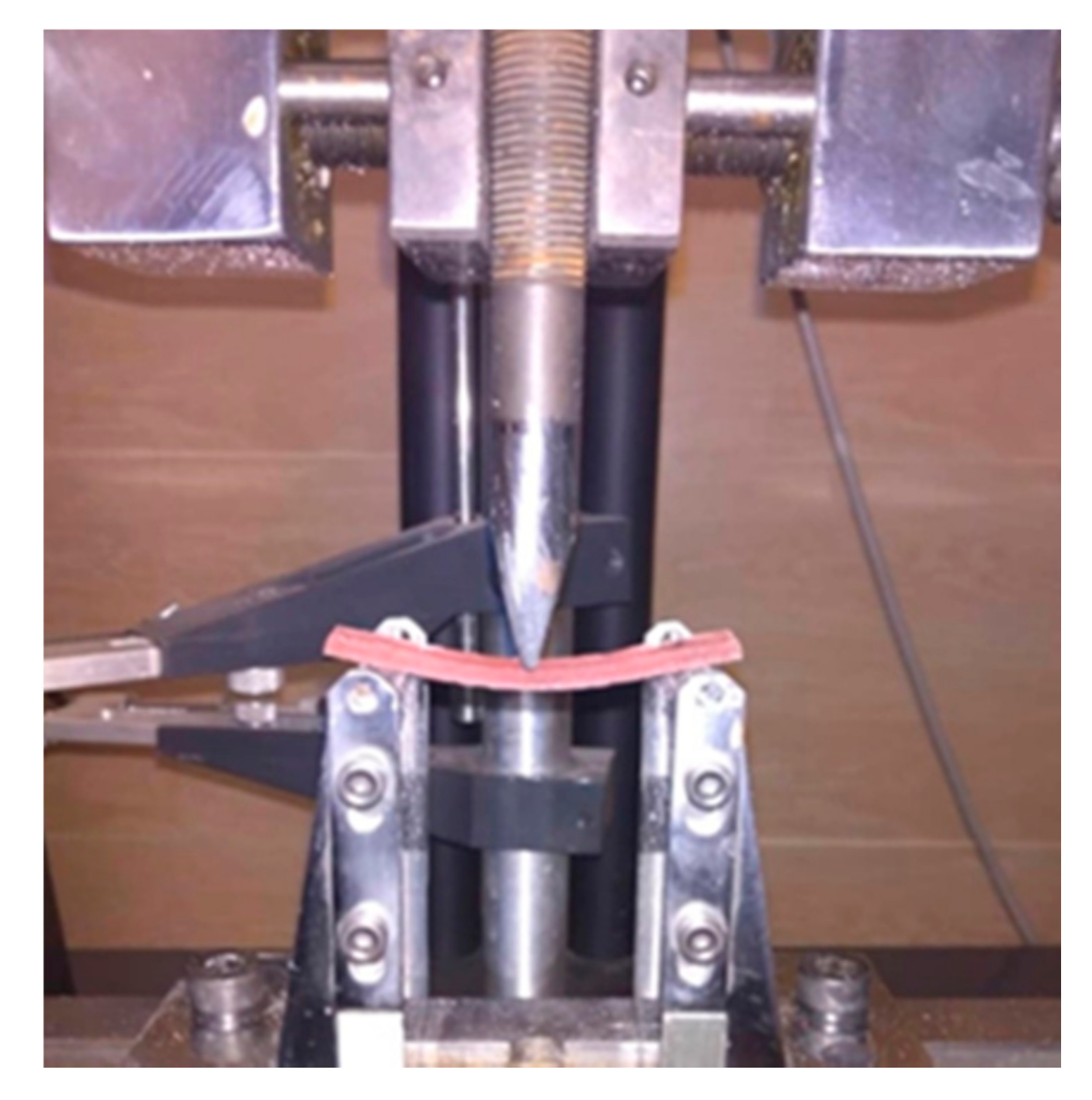
2.2. Flexural Strength
2.3. Compressive Strength
2.4. Microhardness
2.5. Impact Strength
3. Results
3.1. Flexural Strength
3.2. Compressive Strength
3.3. Microhardness
3.4. Impact Strength
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gong, S.-Q.; Epasinghe, J.; Rueggeberg, F.A.; Niu, L.-N.; Mettenberg, D.; Yiu, C.K.Y.; Blizzard, J.D.; Wu, C.D.; Mao, J.; Drisko, C.L.; et al. An ORMOSIL-Containing Orthodontic Acrylic Resin with Concomitant Improvements in Antimicrobial and Fracture Toughness Properties. PLoS ONE 2012, 7, e42355. [Google Scholar] [CrossRef] [PubMed]
- Morgan, T.; Wilson, M. The effects of surface roughness and type of denture acrylic on biofilm formation by Streptococcus oralis in a constant depth film fermentor. J. Appl. Microbiol. 2001, 91, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Shah, V.R.; Shah, D.N.; Chauhan, C.J.; Doshi, P.J.; Kumar, A. Evaluation of flexural strength and color stability of different denture base materials including flexible material after using different denture cleansers. J. Indian Prosthodont. Soc. 2015, 15, 367–373. [Google Scholar] [CrossRef]
- Porwal, A.; Khandelwal, M.; Punia, V.; Sharma, V. Effect of denture cleansers on color stability, surface roughness, and hardness of different denture base resins. J. Indian Prosthodont. Soc. 2017, 17, 61–67. [Google Scholar] [PubMed]
- Moussa, A.R.; Dehis, W.M.; Elboraey, A.N.; ElGabry, H.S. A Comparative Clinical Study of the Effect of Denture Cleansing on the Surface Roughness and Hardness of Two Denture Base Materials. Open Access Maced. J. Med Sci. 2016, 4, 476–481. [Google Scholar] [CrossRef]
- Neppelenbroek, K.H.; Pavarina, A.C.; Vergani, C.E.; Giampaolo, E.T. Hardness of heat-polymerized acrylic resins after disinfection and long-term water immersion. J. Prosthet. Dent. 2005, 93, 171–176. [Google Scholar] [CrossRef]
- Pavarina, A.C.; Vergani, C.E.; Machado, A.L.; Giampaolo, E.T.; Teraoka, M.T. The effect of disinfectant solutions on the hardness of acrylic resin denture teeth. J. Oral Rehabilitation 2003, 30, 749–752. [Google Scholar] [CrossRef]
- Bensel, T.; Bock, J.J.; Kebernik, A.; Arnold, C.; Mansour, S.; Boeckler, A.F. Effect of Disinfectants on Mechanical Properties of Orthodontic Acrylics. Int. J. Biomater. 2019, 2019, 1–10. [Google Scholar] [CrossRef]
- Da Silva, P.M.B.; Acosta, E.J.T.R.; Jacobina, M.; Pinto, L.D.R.; Porto, V.C. Effect of repeated immersion solution cycles on the color stability of denture tooth acrylic resins. J. Appl. Oral Sci. 2011, 19, 623–627. [Google Scholar] [CrossRef]
- Heravi, F.; Bagheri, H.; Rangrazi, A.; Zebarjad, S.M. An in vitro study on the retentive strength of orthodontic bands cemented with CPP-ACP-containing GIC. Mater. Res. Express 2016, 3, 125401. [Google Scholar] [CrossRef]
- Batra, P. Applications of Nanoparticles in Orthodontics. In Dental Applications of Nanotechnology; Springer Science and Business Media LLC: Berlin/Heidelberg, Germany, 2018; pp. 81–105. [Google Scholar]
- Toodehzaeim, M.H.; Zandi, H.; Meshkani, H.; Firouzabadi, A.H. The Effect of CuO Nanoparticles on Antimicrobial Effects and Shear Bond Strength of Orthodontic Adhesives. J. Dent. 2018, 19, 1–5. [Google Scholar]
- Sodagar, A.; Kassaee, M.Z.; Akhavan, A.; Javadi, N.; Arab, S.; Kharazifard, M.J. Effect of silver nano particles on flexural strength of acrylic resins. J. Prosthodont. Res. 2012, 56, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Sodagar, A.; Bahador, A.; Khalil, S.; Shahroudi, A.S.; Kassaee, M.Z. The effect of TiO2 and SiO2 nanoparticles on flexural strength of poly (methyl methacrylate) acrylic resins. J. Prosthodont. Res. 2013, 57, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Patil, S.R.; Reddy, A.K.; Kambalyal, P.B.; Vankhre, M.; Khan, M.Y.A.; Kumar, T.R. Comparative evaluation and influence on shear bond strength of incorporating silver, zinc oxide, and titanium dioxide nanoparticles in orthodontic adhesive. J. Orthod. Sci. 2016, 5, 127–131. [Google Scholar] [CrossRef]
- Cicciù, M.; Fiorillo, L.; Cervino, G. Chitosan Use in Dentistry: A Systematic Review of Recent Clinical Studies. Mar. Drugs 2019, 17, 417. [Google Scholar] [CrossRef]
- Rangrazi, A.; Bagheri, H.; Ghazvini, K.; Borouziniat, A.; Darroudi, M. Synthesis and antibacterial activity of colloidal selenium nanoparticles in chitosan solution: A new antibacterial agent. Mater. Res. Express 2020, 6, 1250h3. [Google Scholar] [CrossRef]
- Husain, S.; Al-Samadani, K.H.; Zafar, M.S.; Najeeb, S.; Khurshid, Z.; Zohaib, K.; Qasim, S.S.B. Chitosan Biomaterials for Current and Potential Dental Applications. Materials 2017, 10, 602. [Google Scholar] [CrossRef]
- Ghasempour, M.; Rajabnia, R.; Gharekhani, S.; Gholamhoseinnia, S.; Soroorhomayoon, S. Anti-Streptococcus mutans property of a chitosan: Containing resin sealant. J. Int. Soc. Prev. Community Dent. 2016, 6, 49–53. [Google Scholar] [CrossRef]
- Chandrasekaran, M.; Moussaoui, Y.; Chun, S.C. Antibacterial Activity of Chitosan Nanoparticles: A Review. Processes 2020, 8, 1173. [Google Scholar] [CrossRef]
- Retamoso, L.B.; Cunha, T.D.M.A.D.; Pithon, M.M.; Dos Santos, R.L.; Martins, F.O.; Romanos, M.T.V.; Tanaka, O.M. In vitro cytotoxicity of self-curing acrylic resins of different colors. Dent. Press J. Orthod. 2014, 19, 66–70. [Google Scholar] [CrossRef][Green Version]
- Soygun, K.; Bolayir, G.; Boztug, A. Mechanical and thermal properties of polyamide versus reinforced PMMA denture base materials. J. Adv. Prosthodont. 2013, 5, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Shibata, T.; Hamada, N.; Kimoto, K.; Sawada, T.; Sawada, T.; Kumada, H.; Umemoto, T.; Toyoda, M. Antifungal Effect of Acrylic Resin Containing Apatite-coated TiO2 Photocatalyst. Dent. Mater. J. 2007, 26, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Goiato, M.C.; Andreotti, A.M.; Moreno, A.; Nobrega, A.S.; Pesqueira, A.A.; Dos Santos, D.M. Influence of nanoparticles on color stability, microhardness, and flexural strength of acrylic resins specific for ocular prosthesis. Int. J. Nanomed. 2014, 9, 5779–5787. [Google Scholar] [CrossRef]
- Moslehifard, E.; Anaraki, M.R.; Shirkavand, S. Effect of adding TiO2 nanoparticles on the SEM morphology and mechanical properties of conventional heat-cured acrylic resin. J. Dent. Res. Dent. Clin. Dent. Prospects 2019, 13, 234. [Google Scholar] [CrossRef] [PubMed]
- Ellakwa, A.; Morsy, M.A.; El-Sheikh, A.M. Effect of Aluminum Oxide Addition on the Flexural Strength and Thermal Diffusivity of Heat-Polymerized Acrylic Resin. J. Prosthodont. 2008, 17, 439–444. [Google Scholar] [CrossRef]
- Alhareb, A.O.; Ahmad, Z.A. Effect of Al2O3/ZrO2 reinforcement on the mechanical properties of PMMA denture base. J. Reinf. Plast. Compos. 2010, 30, 86–93. [Google Scholar] [CrossRef]
- Al-Harbi, F.A.; Abdel-Halim, M.S.; Gad, M.M.; Fouda, S.M.; Baba, N.Z.; Alrumaih, H.S.; Akhtar, S. Effect of Nanodiamond Addition on Flexural Strength, Impact Strength, and Surface Roughness of PMMA Denture Base. J. Prosthodont. 2018, 28, e417–e425. [Google Scholar] [CrossRef]
- Hamedi-Rad, F.; Ghaffari, T.; Rezaii, F.; Ramazani, A. Effect of Nanosilver on Thermal and Mechanical Properties of Acrylic Base Complete Dentures. J. Dent. 2014, 11, 495–505. [Google Scholar]
- Ghaffari, T.; Hamedi-Rad, F.; Ezzati, B. In Vitro Comparison of Compressive and Tensile Strengths ofAcrylic Resins Reinforced by Silver Nanoparticles at 2% and 0.2% Concentrations. J. Dent. Res. Dent. Clin. Dent. Prospect. 2014, 8, 204–209. [Google Scholar]
- Abdulridha, W.M.; Almusawi, R.M.; Al-Jubouri, O.M.; Wally, Z.J.; Zidan, S.; Haider, J.; Al-Quraine, N.T. Sudying the effect of adding Titanium Dioxide (TiO2) nanoparticles on the compressive strength of chemical and heat-activated acrylic denture base resins. J. Mater. Process Technol. 2020, 1–13. [Google Scholar] [CrossRef]
- Farina, A.P.; Cecchin, D.; Soares, R.G.; Botelho, A.L.; Takahashi, J.M.F.K.; Mazzetto, M.O.; Mesquita, M.F. Evaluation of Vickers hardness of different types of acrylic denture base resins with and without glass fibre reinforcement. Gerodontology 2012, 29, e155–e160. [Google Scholar] [CrossRef] [PubMed]
- Vojdani, M.; Bagheri, R.; Khaledi, A.A.R. Effects of aluminum oxide addition on the flexural strength, surface hardness, and roughness of heat-polymerized acrylic resin. J. Dent. Sci. 2012, 7, 238–244. [Google Scholar] [CrossRef]
- Ghahremani, L.; Shirkavand, S.; Akbari, F.; Sabzikari, N. Tensile strength and impact strength of color modified acrylic resin reinforced with titanium dioxide nanoparticles. J. Clin. Exp. Dent. 2017, 9, e661–e665. [Google Scholar] [CrossRef] [PubMed]



| Groups | n | Mean (MPa) | Standard Deviation (MPa) |
|---|---|---|---|
| Acrylic resin(control) | 10 | 64.1 | 12.41 |
| Acrylic resin + 0.5% chitosan NPs | 10 | 60.4 | 7.04 |
| Acrylic resin + 1% chitosan NPs | 10 | 52.6 | 12.29 |
| Acrylic resin + 2% chitosan NPs | 10 | 46.9 | 11.25 |
| Acrylic resin + 4% chitosan NPs | 10 | 39.3 | 9.14 |
| (I) Group | (J) Group | p-Value |
|---|---|---|
| Group 1 (Control) | Group 2 | 0.939 |
| Group 3 | 0.140 | |
| Group 4 | 0.008 | |
| Group 5 | 0.000 | |
| Group 2 | Group 3 | 0.497 |
| Group 4 | 0.056 | |
| Group 5 | 0.001 | |
| Group 3 | Group 4 | 0.763 |
| Group 5 | 0.051 | |
| Group 4 | Group 5 | 0.472 |
| Groups | n | Mean (MPa) | Standard Deviation (MPa) |
|---|---|---|---|
| Acrylic resin(control) | 23 | 92.61 | 22.86 |
| Acrylic resin + 0.5% chitosan NPs | 23 | 88.78 | 14.79 |
| Acrylic resin + 1% chitosan NPs | 23 | 83.74 | 12.48 |
| Acrylic resin + 2% chitosan NPs | 23 | 79.04 | 14.93 |
| Acrylic resin + 4% chitosan NPs | 23 | 71.35 | 15.71 |
| (I) Group | (J) Group | p-Value |
|---|---|---|
| Group 1 (Control) | Group 2 | 0.935 |
| Group 3 | 0.368 | |
| Group 4 | 0.040 | |
| Group 5 | 0.000 | |
| Group 2 | Group 3 | 0.839 |
| Group 4 | 0.274 | |
| Group 5 | 0.005 | |
| Group 3 | Group 4 | 0.871 |
| Group 5 | 0.089 | |
| Group 4 | Group 5 | 0.515 |
| Groups | n | Mean (VHN) | Standard Deviation (VHN) |
|---|---|---|---|
| Acrylic resin(control) | 20 | 17.50 | 2.19 |
| Acrylic resin + 0.5% chitosan NPs | 20 | 17.37 | 1.17 |
| Acrylic resin + 1% chitosan NPs | 20 | 16.93 | 1.18 |
| Acrylic resin + 2% chitosan NPs | 20 | 16.76 | 1.30 |
| Acrylic resin+ 4% chitosan NPs | 20 | 15.91 | 2.67 |
| Groups | n | Mean (J/m2) | Standard Deviation (J/m2) |
|---|---|---|---|
| Acrylic resin(control) | 6 | 2875 | 487 |
| Acrylic resin + 0.5% chitosan NPs | 6 | 2769 | 749 |
| Acrylic resin + 1% chitosan NPs | 6 | 2644 | 596 |
| Acrylic resin + 2% chitosan NPs | 6 | 2531 | 380 |
| Acrylic resin + 4% chitosan NPs | 6 | 2389 | 122 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahabi, M.; Movahedi Fazel, S.; Rangrazi, A. Incorporation of Chitosan Nanoparticles into a Cold-Cure Orthodontic Acrylic Resin: Effects on Mechanical Properties. Biomimetics 2021, 6, 7. https://doi.org/10.3390/biomimetics6010007
Shahabi M, Movahedi Fazel S, Rangrazi A. Incorporation of Chitosan Nanoparticles into a Cold-Cure Orthodontic Acrylic Resin: Effects on Mechanical Properties. Biomimetics. 2021; 6(1):7. https://doi.org/10.3390/biomimetics6010007
Chicago/Turabian StyleShahabi, Mostafa, Sorour Movahedi Fazel, and Abdolrasoul Rangrazi. 2021. "Incorporation of Chitosan Nanoparticles into a Cold-Cure Orthodontic Acrylic Resin: Effects on Mechanical Properties" Biomimetics 6, no. 1: 7. https://doi.org/10.3390/biomimetics6010007
APA StyleShahabi, M., Movahedi Fazel, S., & Rangrazi, A. (2021). Incorporation of Chitosan Nanoparticles into a Cold-Cure Orthodontic Acrylic Resin: Effects on Mechanical Properties. Biomimetics, 6(1), 7. https://doi.org/10.3390/biomimetics6010007





