Identification of Gait-Cycle Phases for Prosthesis Control
Abstract
:1. Introduction
- -
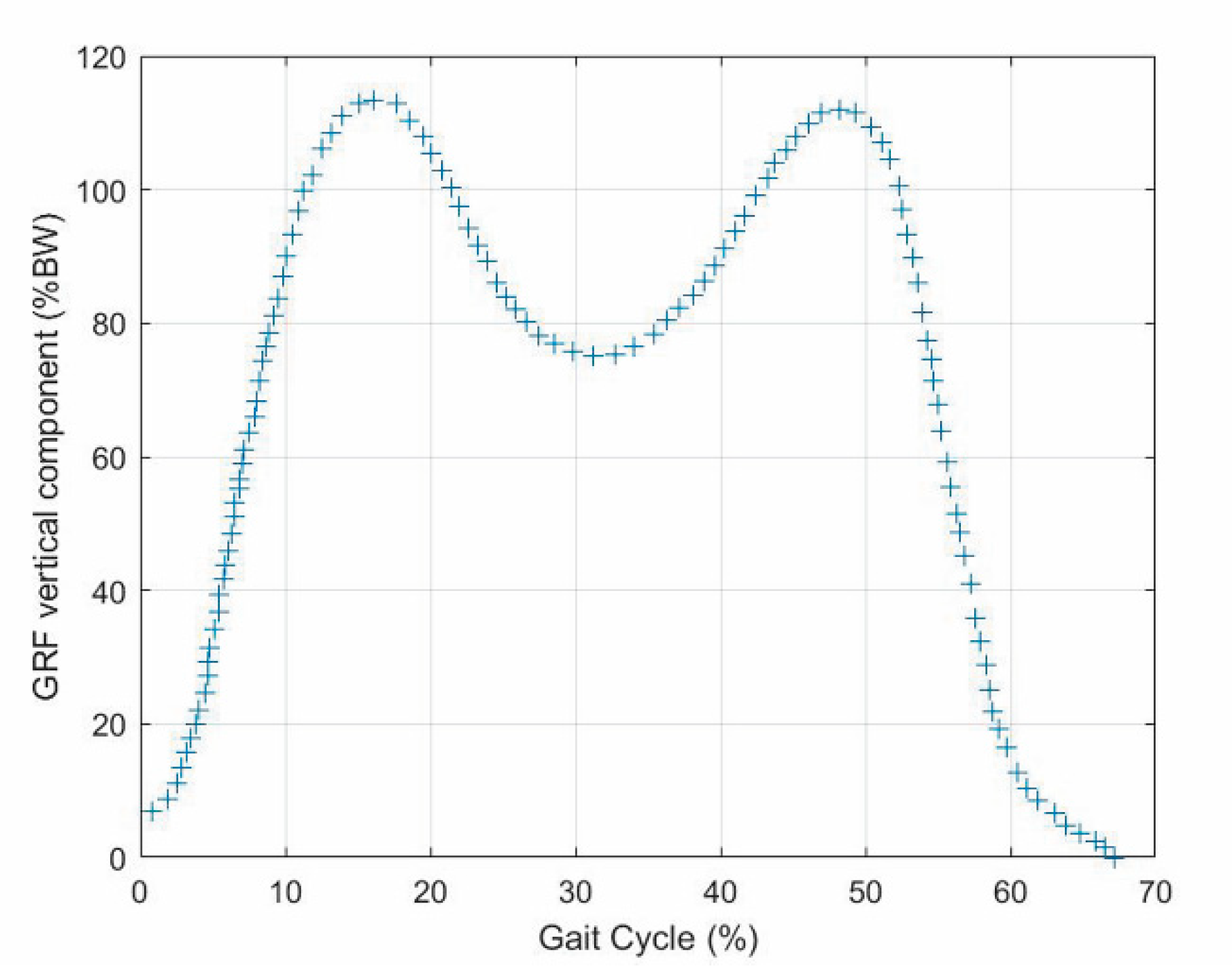
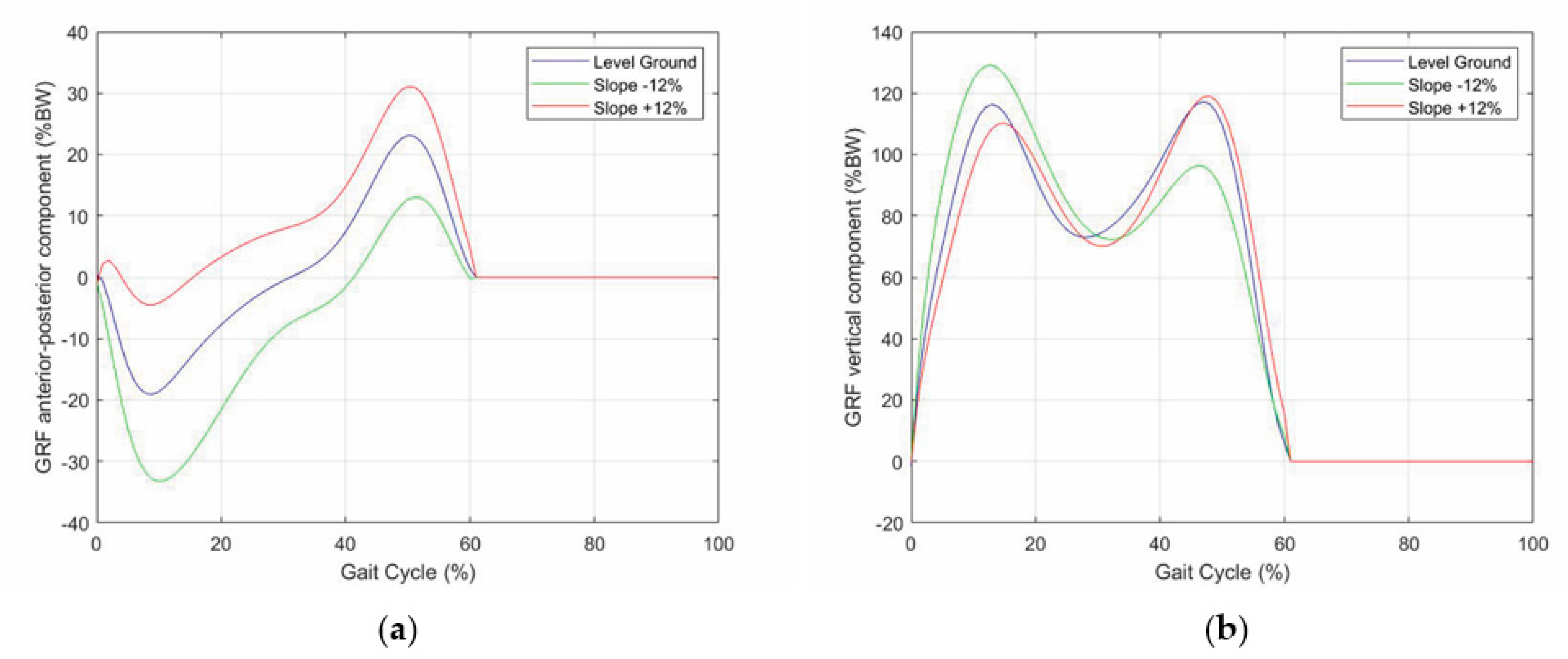
- The vertical force has two peaks of about 120% of the body weight (BW) that occur approximately at the end of the initial double-support period (i.e., 10% of gait-cycle completion (Figure 1)) and earlier than the beginning of the terminal double-support period (i.e., 45–50% of gait-cycle completion (Figure 1)) with a minimum of about 80% BW in the middle (i.e., 30% of gait-cycle completion (Figure 1));
- -
- The anterior–posterior shear has two peaks with opposite signs of about 20% BW, which approximately occur when the vertical force has two peaks and vanish in the middle of the stance phase (i.e., 30% of gait-cycle completion (Figure 1));
- -
- The medial–lateral shear is much smaller than the other two components. It has no sharp peaks, and it is comprised in the range [−5, +5]%BW
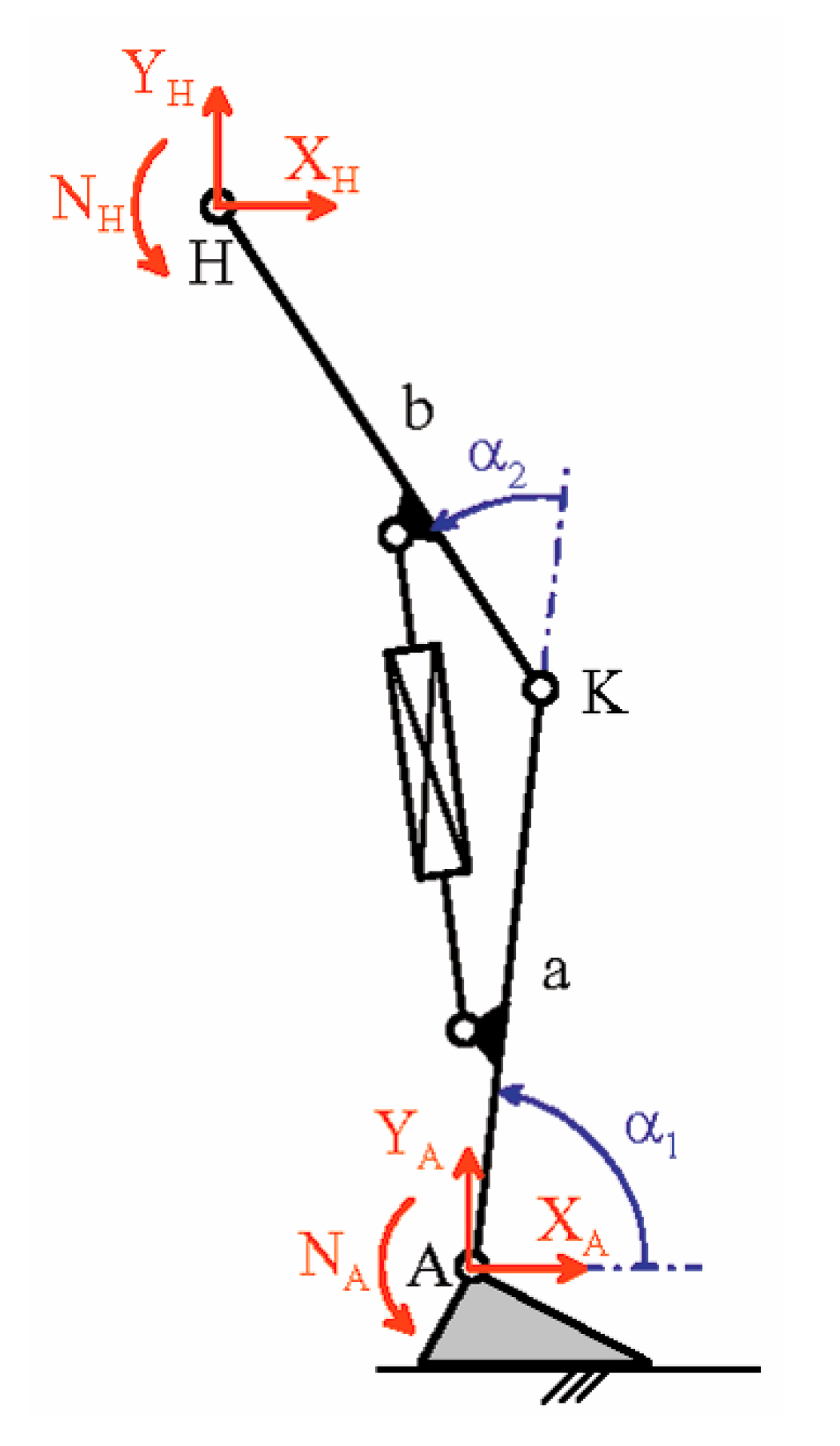
2. Materials and Methods
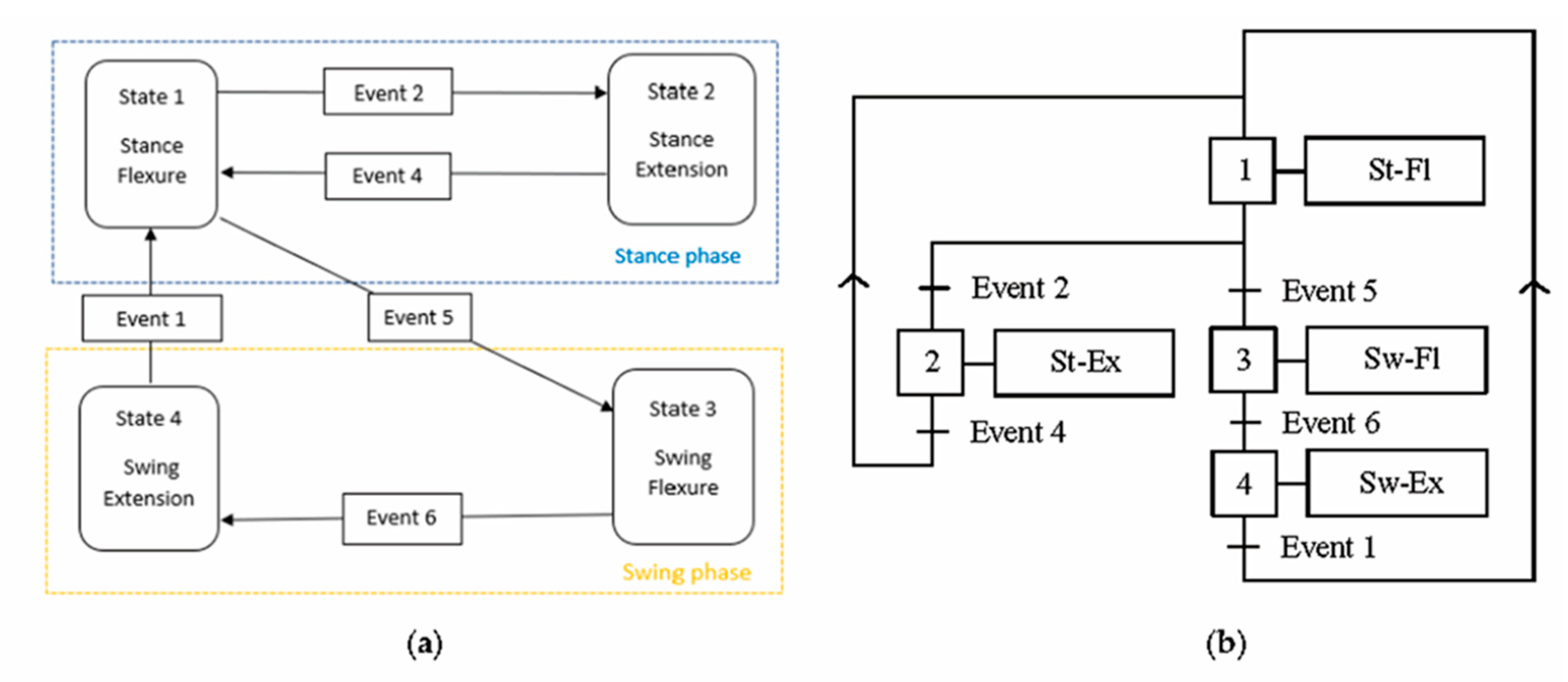
2.1. Detection of Gait-Cycle Events
- -
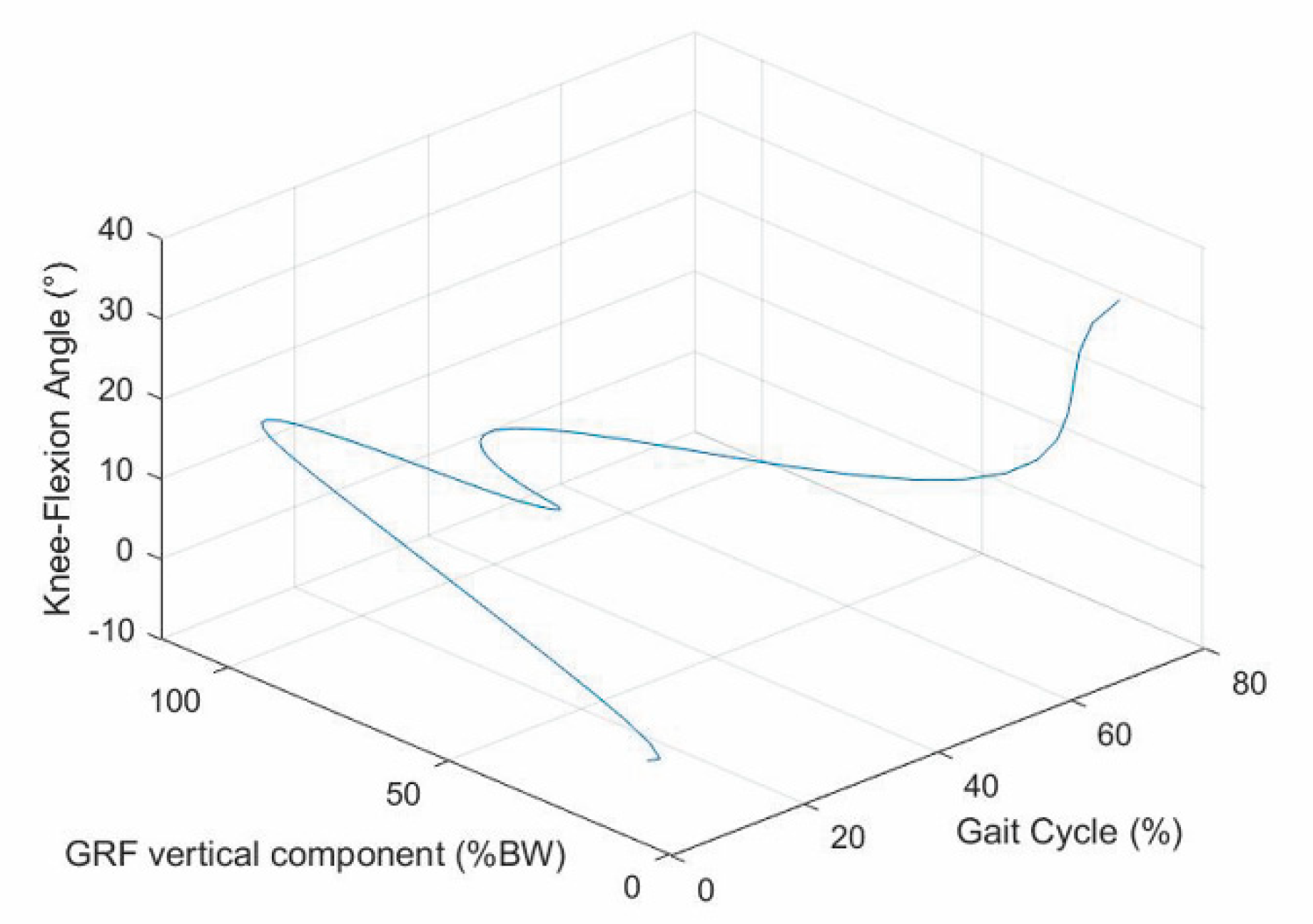
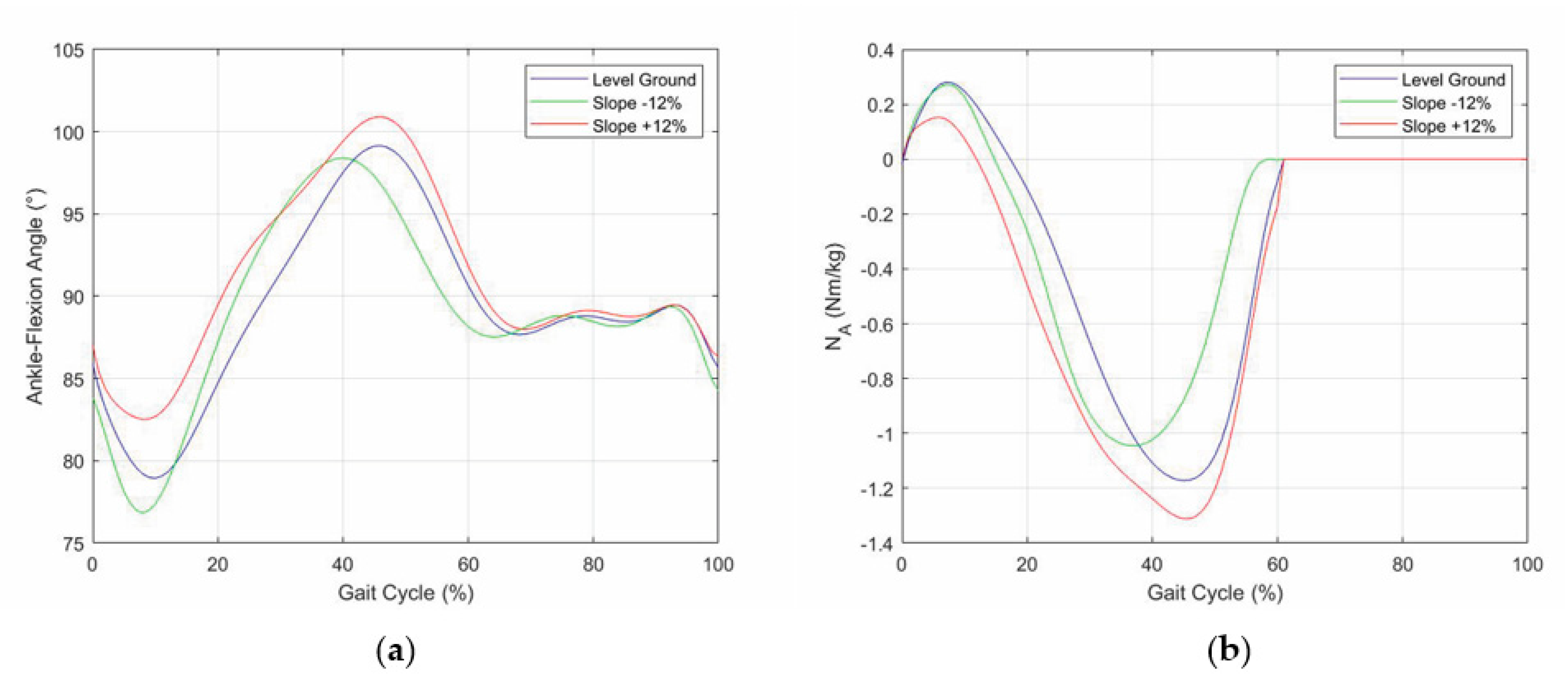
- A first flexion of the knee starts at the IC event (1st event), which is easily identified by the transition of the GRF vertical component from zero to a positive value, increases with the GRF increase and reaches its maximum a bit earlier than the 1st peak of the GRF vertical component (2nd event). This is because the knee flexion somehow compensates for the shock of the sudden appearance of a non-null GRF and gives a smooth transition from the swing phase to the stance phase.
- -
- The first knee flexion is followed by a complete knee extension that has its middle configuration at the minimum of the GRF vertical component (3rd event) and approximately terminates when the GRF vertical component reaches its 2nd GRF peak (4th event), which is at the beginning of the second double-support period.
- -
- A second knee flexion then starts, which accompanies the decrease of the GRF vertical component until the TO event (5th event), easily identified by the transition of the GRF vertical component from a positive value to zero, and continues during the swing phase until the reaching of a maximum flexion angle that occurs nearly at the middle of the swing phase (6th event).
- -
- The second knee flexion is followed by a second knee extension that terminates at the next IC event (1st event of the next cycle).
2.2. Detection of the Longitudinal Slope
- -
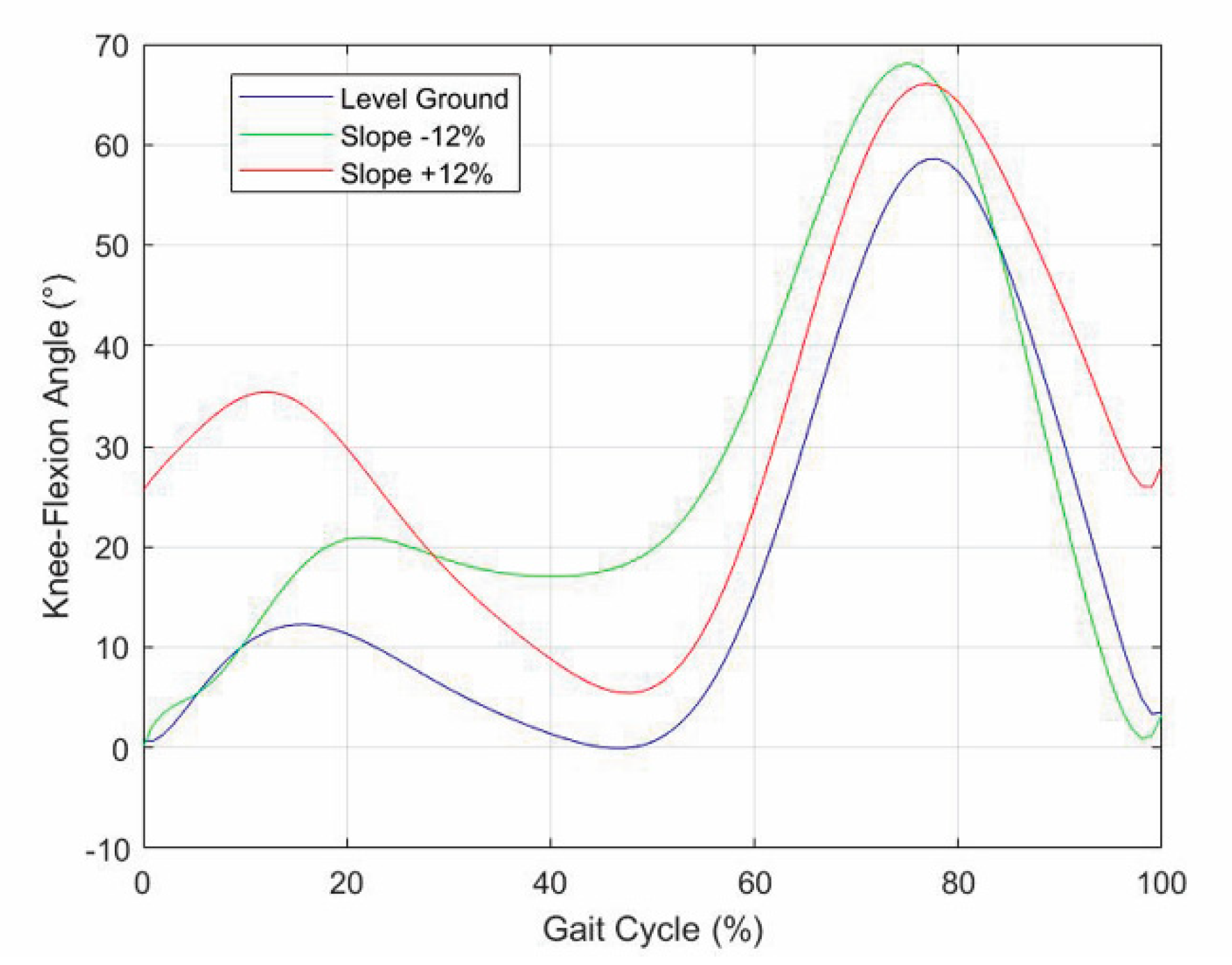
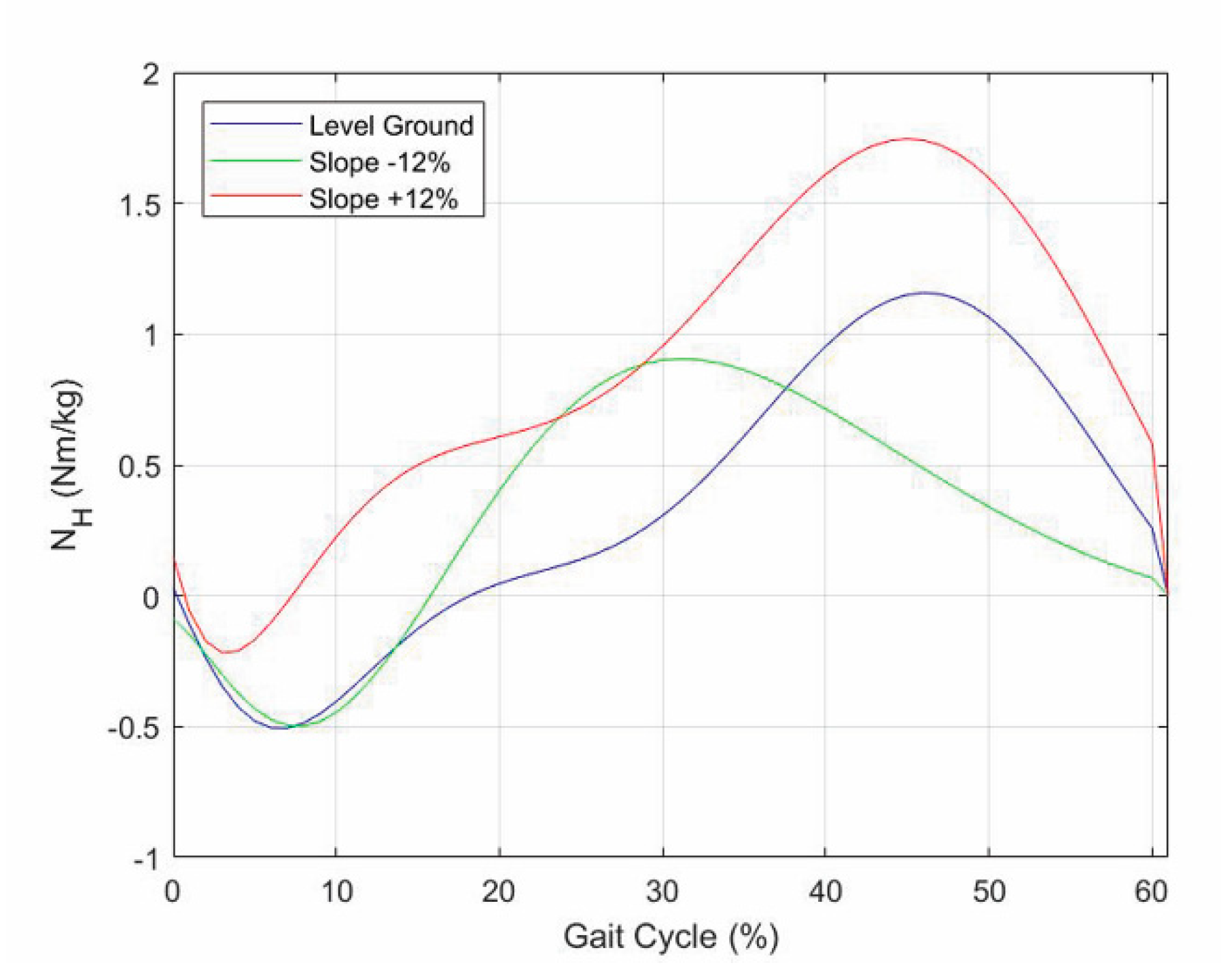
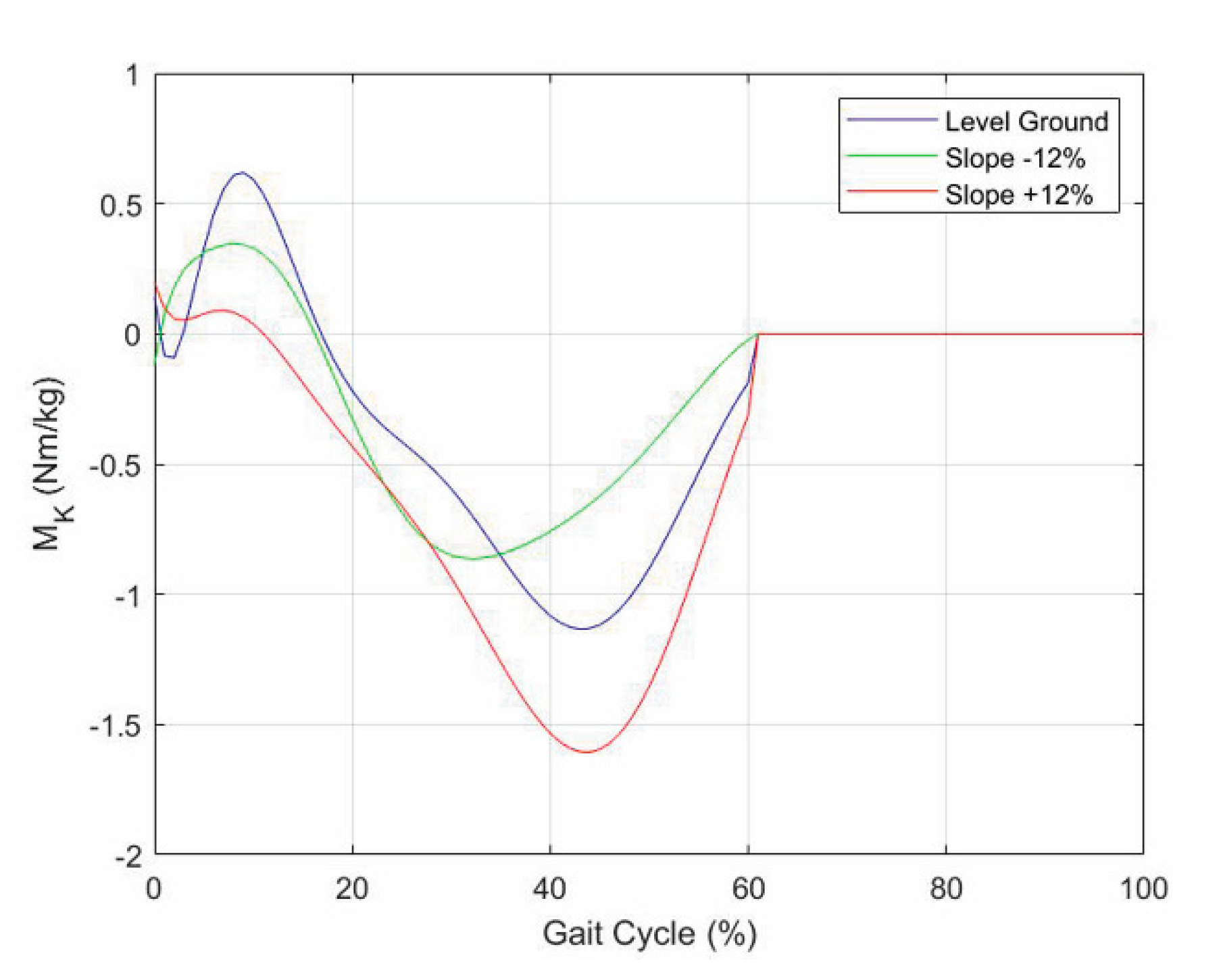
- In uphill walking, the GRF vertical component still has two peaks, but the 2nd peak is higher than the 1st, and the difference increases with the slope, whereas the knee-flexion angle still has two flexions and two extensions, but the knee flexion at the IC increases with the slope;
- -
- In downhill walking, the GRF vertical component still has two peaks, but the 1st peak is higher than the 2nd, and the difference increases with the slope, whereas the knee-flexion angle keeps the same IC value, but all the intermediate values are amplified with an amplification factor that increases with the slope;
- -
- Both in uphill and in downhill walking the minimum value between the two peaks does not change appreciably.
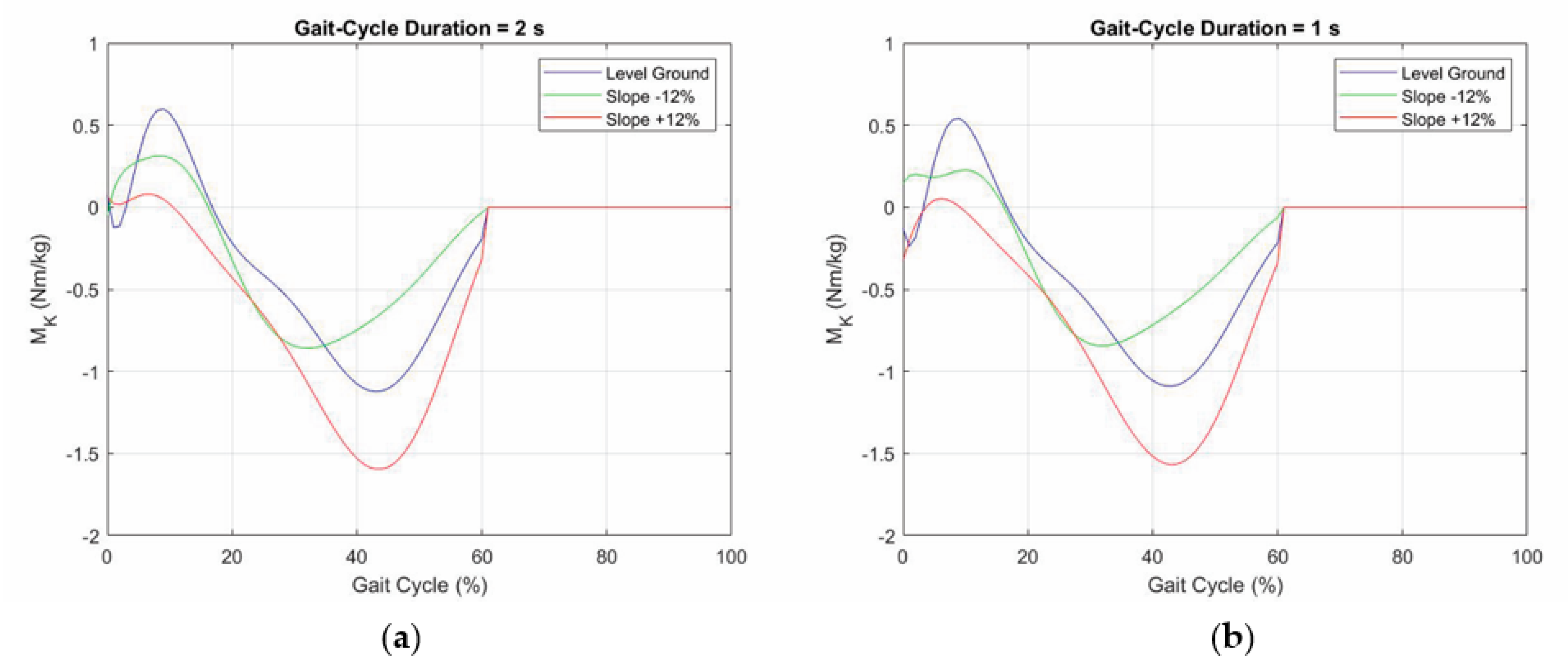
2.3. Effects of Cadence
- (i)
- The “normal” walking cadence of the patient is determined as the one at which the two GRF peaks are about equal;
- (ii)
- The reference peak difference ΔF0, the maximum knee-flexion angle, etc. at each cadence are determined (e.g., through a regression on a finite number of measures on the patient);
- (iii)
- The parameter ΔF that appears in Table 2 for identifying a possible slope is redefined as follows
2.4. Control Algorithm
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Villa, C. Analyse de la Marche des Personnes Amputées de Membre Inférieur en Situations Contraignantes de la vie Courante. Ph.D. Thesis, Biomécanique [physics.med-ph]. Ecole Nationale Supérieure d’Arts et Métiers—ENSAM, Paris, France, 2014. In French (NNT: 2014ENAM0002), (pastel-01064361). Available online: https://pastel.archives-ouvertes.fr/pastel-01064361/ (accessed on 23 January 2021).
- Hayot, C. Analyse Biomécanique 3D de la Marche Humaine: Comparaison des Modèles Mécaniques. Ph.D. Thesis, University of Poitiers, Poitiers, France, 2010. Available online: https://www.theses.fr/2010POIT2342 (accessed on 23 January 2021).
- Fusco, N. Analyse, Modélisation et Simulation de la Marche Pathologique. Ph.D. Thesis, Sciences du Vivant [q-bio], Université Rennes 2, Rennes, France, 2008. In French (tel-00293627v2). Available online: https://tel.archives-ouvertes.fr/tel-00293627/ (accessed on 23 January 2021).
- Sutherland, D.H. The evolution of clinical gait analysis part I: Kinesiological EMG. Gait Posture 2001, 14, 61–70. [Google Scholar] [CrossRef]
- Sutherland, D.H. The evolution of clinical gait analysis part II: Kinematics. Gait Posture 2002, 16, 159–179. [Google Scholar] [CrossRef]
- Sutherland, D.H. The evolution of clinical gait analysis part III: Kinetics and energy assessment. Gait Posture 2005, 21, 447–461. [Google Scholar] [CrossRef] [PubMed]
- Duhamel, A.; Bourriez, J.; Devos, P.; Krystkowiak, P.; Destée, A.; Derambure, P.; Defebvre, L. Statistical tools for clinical gait analysis. Gait Posture 2004, 20, 204–212. [Google Scholar] [CrossRef] [PubMed]
- Rueterbories, J.; Spaich, E.G.; Larsen, B.; Andersen, O.K. Methods for gait event detection and analysis in ambulatory systems. Med. Eng. Phys. 2010, 32, 545–552. [Google Scholar] [CrossRef]
- Wren, T.A.; Gorton, G.E.; Õunpuu, S.; Tucker, C.A. Efficacy of clinical gait analysis: A systematic review. Gait Posture 2011, 34, 149–153. [Google Scholar] [CrossRef] [PubMed]
- Cimolin, V.; Galli, M. Summary measures for clinical gait analysis: A literature review. Gait Posture 2014, 39, 1005–1010. [Google Scholar] [CrossRef] [PubMed]
- Caldas, R.; Mundt, M.; Potthast, W.; de Lima Neto, F.B.; Markert, B. A systematic review of gait analysis methods based on inertial sensors and adaptive algorithms. Gait Posture 2017, 57, 204–210. [Google Scholar] [CrossRef]
- Roberts, M.; Mongeon, D.; Prince, F. Biomechanical parameters for gait analysis: A systematic review of healthy human gait. Phys. Ther. Rehabil. 2017, 4, 6. [Google Scholar] [CrossRef]
- Alharthi, A.S.; Yunas, S.U.; Ozanyan, K.B. Deep Learning for Monitoring of Human Gait: A Review. IEEE Sens. J. 2019, 19, 9575–9591. [Google Scholar] [CrossRef] [Green Version]
- Papagiannis, G.I.; Triantafyllou, A.I.; Roumpelakis, I.M.; Zampeli, F.; Eleni, P.G.; Koulouvaris, P.; Papadopoulos, E.C.; Papagelopoulos, P.J.; Babis, G.C. Methodology of surface electromyography in gait analysis: Review of the literature. J. Med. Eng. Technol. 2019, 43, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Fakoorian, S.; Roshanineshat, A.; Khalaf, P.; Azimi, V.; Simon, D.; Hardin, E. An Extensive Set of Kinematic and Kinetic Data for Individuals with Intact Limbs and Transfemoral Prosthesis Users. Appl. Bionics Biomech. 2020, 2020, 8864854. [Google Scholar] [CrossRef] [PubMed]
- Goujon, H. Gait Analysis of Transfemoral Amputee. Ph.D. Thesis, Engineering Sciences [Physics], Arts et Métiers ParisTech, Paris, France, 2006. (NNT: 2006ENAM0042), (pastel-00002067). Available online: https://hal.archives-ouvertes.fr/pastel-00002067 (accessed on 23 January 2021).
- Whittle, M.W. Gait Analysis: An Introduction, 4th ed.; Elsevier: Philadelphia, PA, USA, 2007; ISBN 978-0750688833. [Google Scholar]
- Kirtley, C. Clinical Gait Analysis: Theory and Practic; Elsevier: Philadelphia, PA, USA, 2006; ISBN 978-0443100093. [Google Scholar]
- Simoneau, G.G. Kinesiology of Walking. In Kinesiology of the Musculoskeletal System: Foundations for Physical Rehabilitation, 2nd ed.; Neumann, D.A., Ed.; Mosby: St. Louis, MO, USA, 2010; pp. 627–681. [Google Scholar]
- Lafortune, M.A.; Cavanagh, P.R.; Sommer, H.J., III; Kalenak, A. Three-dimensional kinematics of the human knee during walking. J. Biomech. 1992, 25, 347–357. [Google Scholar] [CrossRef]
- Giakas, G.; Baltzopoulos, V. Time and frequency domain analysis of ground reaction forces during walking: An investigation of variability and symmetry. Gait Posture 1997, 5, 189–197. [Google Scholar] [CrossRef]
- Damavandi, M.; Dixon, P.C.; Pearsall, D.J. Ground reaction force adaptations during cross-slope walking and running. Hum. Mov. Sci. 2012, 31, 182–189. [Google Scholar] [CrossRef]
- Dauriac, B. Contribution à la Mise en Oeuvre et L’évaluation de Technologies Embarquées Pour L’appareillage de Personnes Amputées du Membre Inférieur. Ph.D. Thesis, Ecole Nationale Supérieure d’Arts et Métiers—ENSAM, Paris, France, 2018. In French (NNT: 2018ENAM0017). (tel-01936168). Available online: https://pastel.archives-ouvertes.fr/tel-01936168 (accessed on 13 February 2021).
- Collins, D.M.; Karmarkar, A.; Relich, R.; Pasquina, P.F.; Cooper, R.A. Review of research on prosthetic devices for lower extremity amputation. Crit. Rev. Biomed. Eng. 2006, 34, 379–438. [Google Scholar] [CrossRef]
- Torrealba, R.R.; Fernández-López, G.; Grieco, J.C. Towards the development of knee prostheses: Review of current researches. Kybernetes 2008, 37, 1561–1576. [Google Scholar] [CrossRef]
- Hafner, B.J.; Willingham, L.L.; Buell, N.C.; Allyn, K.J.; Smith, D.G. Evaluation of Function, Performance, and Preference as Transfemoral Amputees Transition from Mechanical to Microprocessor Control of the Prosthetic Knee. Arch. Phys. Med. Rehabil. 2007, 88, 207–217. [Google Scholar] [CrossRef]
- Versluys, R.; Desomer, A.; Lenaerts, G.; Beyl, P.; Van Damme, M.; VanderBorght, B.; Vanderniepen, I.; Van Der Perre, G.; Lefeber, D. From conventional prosthetic feet to bionic feet: A review study. In Proceedings of the 2008 2nd IEEE RAS & EMBS International Conference on Biomedical Robotics and Biomechatronics, Scottsdale, AZ, USA, 19–22 October 2008; pp. 49–54. [Google Scholar] [CrossRef]
- Bogue, R. Exoskeletons and robotic prosthetics: A review of recent developments. Ind. Robot. Int. J. 2009, 36, 421–427. [Google Scholar] [CrossRef]
- Martin, J.; Pollock, A.; Hettinger, J. Microprocessor Lower Limb Prosthetics: Review of Current State of the Art. JPO J. Prosthet. Orthot. 2010, 22, 183–193. [Google Scholar] [CrossRef]
- Sawers, A.B.; Hafner, B.J. Outcomes associated with the use of microprocessor-controlled prosthetic knees among individuals with unilateral transfemoral limb loss: A systematic review. J. Rehabil. Res. Dev. 2013, 50, 273–314. [Google Scholar] [CrossRef]
- Grimmer, M.; Seyfarth, A. Mimicking Human-Like Leg Function in Prosthetic Limbs. In Neuro-Robotics; Trends in Augmentation of Human Performance; Artemiadis, P., Ed.; Springer: Dordrecht, The Netherlands, 2014; Volume 2, pp. 105–155. [Google Scholar] [CrossRef]
- Windrich, M.; Grimmer, M.; Christ, O.; Rinderknecht, S.; Beckerle, P. Active lower limb prosthetics: A systematic review of design issues and solutions. Biomed. Eng. Online 2016, 15, 140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mattogno, F.; Rosellini, G.; Di Stanislao, E.; Denza, G.; Cova, M. Dispositivi Ortopedici: Manuale; ITOP S.p.A. Officine Ortopediche: Palestrina, Italy, 2020; pp. 208–233. Available online: https://www.itop.it/wp-content/uploads/2017/07/manuale_dispositivi_ortopedici_ITOP.pdf (accessed on 6 March 2021).
- Willems, P.-A.; Schepens, B.; Detrembleur, C. Marche normale. In EMC-Kinésithérapie-Médecine Physique-Réadaptation; Elsevier Masson SAS: Paris, France, 2012; 26-007-B-75. [Google Scholar] [CrossRef]
- McIntosh, A.S.; Beatty, K.T.; Dwan, L.N.; Vickers, D.R. Gait dynamics on an inclined walkway. J. Biomech. 2006, 39, 2491–2502. [Google Scholar] [CrossRef]
- Oberg, T.; Karsznia, A.; Oberg, K. Basic gait parameters: Reference data for normal subjects, 10–79 years of age. J. Rehabil. Res. Dev. 1993, 30, 210–223. [Google Scholar] [PubMed]
- Stansfield, B.W.; Hillman, S.J.; Hazlewood, M.E.; Lawson, A.A.; Mann, A.M.; Loudon, I.R.; Robb, J.E. Normalized Speed, Not Age, Characterizes Ground Reaction Force Patterns in 5- to 12-Year-Old Children Walking at Self-Selected Speeds. J. Pediatr. Orthop. 2001, 21, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Stoquart, G.; Detrembleur, C.; Lejeune, T. Effect of speed on kinematic, kinetic, electromyographic and energetic reference values during treadmill walking. Neurophysiol. Clin. Neurophysiol. 2008, 38, 105–116. [Google Scholar] [CrossRef]
- Pillet, H.; Drevelle, X.; Bonnet, X.; Villa, C.; Martinet, N.; Sauret, C.; Bascou, J.; Loiret, I.; Djian, F.; Rapin, N.; et al. APSIC: Training and fitting amputees during situations of daily living. IRBM 2014, 35, 60–65. [Google Scholar] [CrossRef]
- Smith, J.D.; Ferris, A.E.; Heise, G.D.; Hinrichs, R.N.; Martin, P.E. Oscillation and Reaction Board Techniques for Estimating Inertial Properties of a Below-knee Prosthesis. J. Vis. Exp. 2014, 87, e50977. [Google Scholar] [CrossRef] [Green Version]
| 1 | According to ([19], p. 632), the reference data for “normal” walking are 1.37 m/s for the walking speed, 1.87 steps/s (110 steps/min) of step rate (cadence), and 0.72 m of step length. |
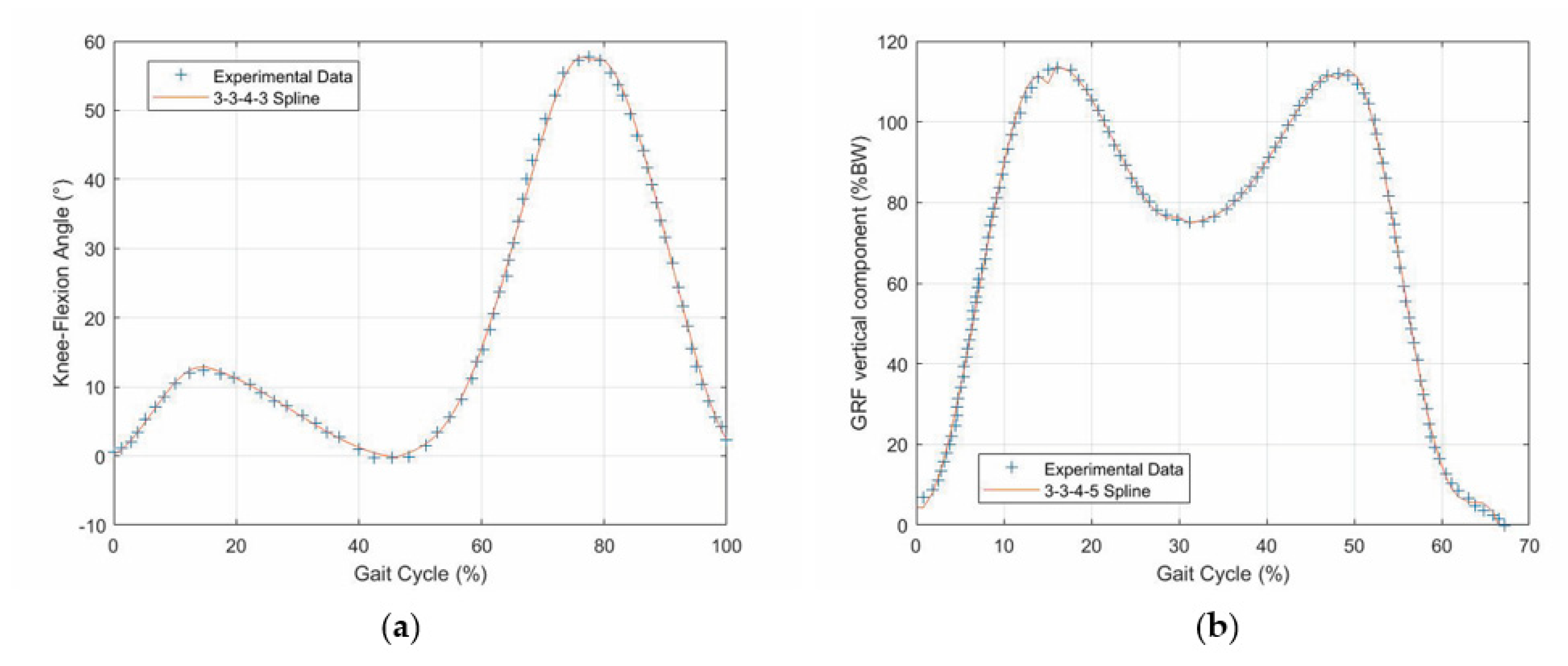
| 2 | The first between the IC event and the 1st peak occurrence, the second between the 1st peak occurrence and the central minimum, the third between the central minimum and the 2nd peak occurrence, and the fourth between the 2nd peak occurrence and the next IC event. |
| 3 | The numbers separated by the hyphens indicate the degrees of the polynomials that compose the spline. |
| 4 | The first between the IC event and the 1st peak occurrence, the second between the 1st peak occurrence and the central minimum, the third between the central minimum and the 2nd peak occurrence, and the fourth between the 2nd peak occurrence and the TO event. |


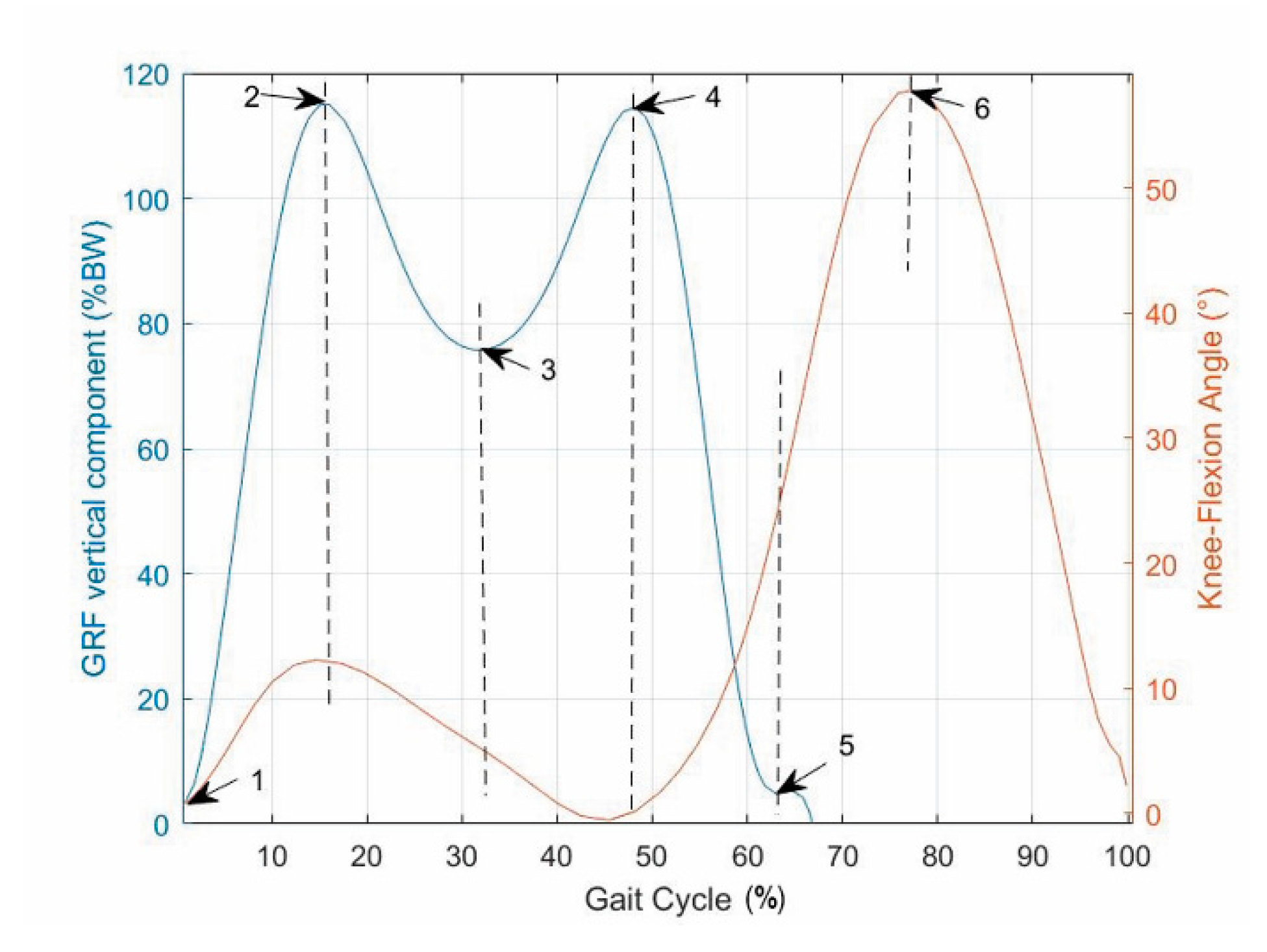

| Detected Condition (t = Time Instant) | Event (Number/Name) | Gait-Cycle Percentage (%) |
|---|---|---|
| GRF(t − dt) = 0 & GRF(t) > 0 | 1/IC | 0 |
| GRF (t − dt) < GRF(t) > GRF(t + dt) | 2/1st GRF peak | 15 |
| GRF(t − dt) > GRF(t) < GRF(t + dt) | 3/heel rise | 32 |
| GRF(t − dt) < GRF(t) > GRF(t + dt) | 4/2nd GRF peak | 47 |
| GRF(t) > 0 & GRF(t + dt) = 0 | 5/TO | 64 |
| Limit Switch Reached | 6/max knee flexion | 78 |
| Detected Condition (i = Cycle Index) | Event (Number) | Slope Variation (Sign) |
|---|---|---|
| ΔFi > ΔFi+1 | 7 | Negative |
| ΔFi+1 > ΔFi | 8 | Positive |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Gregorio, R.; Vocenas, L. Identification of Gait-Cycle Phases for Prosthesis Control. Biomimetics 2021, 6, 22. https://doi.org/10.3390/biomimetics6020022
Di Gregorio R, Vocenas L. Identification of Gait-Cycle Phases for Prosthesis Control. Biomimetics. 2021; 6(2):22. https://doi.org/10.3390/biomimetics6020022
Chicago/Turabian StyleDi Gregorio, Raffaele, and Lucas Vocenas. 2021. "Identification of Gait-Cycle Phases for Prosthesis Control" Biomimetics 6, no. 2: 22. https://doi.org/10.3390/biomimetics6020022
APA StyleDi Gregorio, R., & Vocenas, L. (2021). Identification of Gait-Cycle Phases for Prosthesis Control. Biomimetics, 6(2), 22. https://doi.org/10.3390/biomimetics6020022







