Effects of Accelerated Aging on Color Stability and Surface Roughness of a Biomimetic Composite: An In Vitro Study
Abstract
:1. Introduction
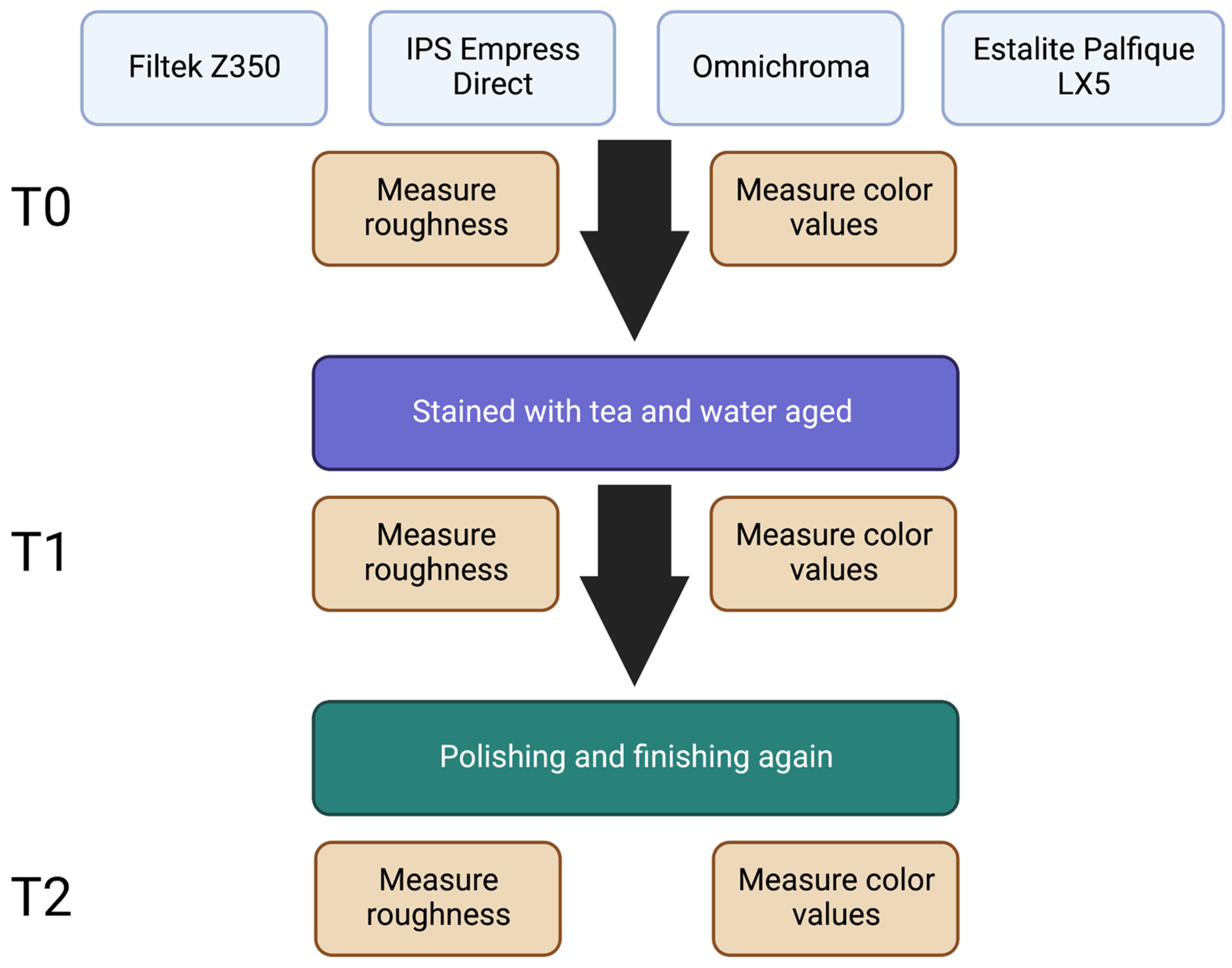
2. Materials and Methods
2.1. Sample Preparation
2.2. Staining Process
2.3. Aging Process
2.4. Finishing and Polishing
2.5. Color Testing
2.6. Surface Roughness
2.7. Statistical Analysis
3. Results
3.1. Overall Color Measurement
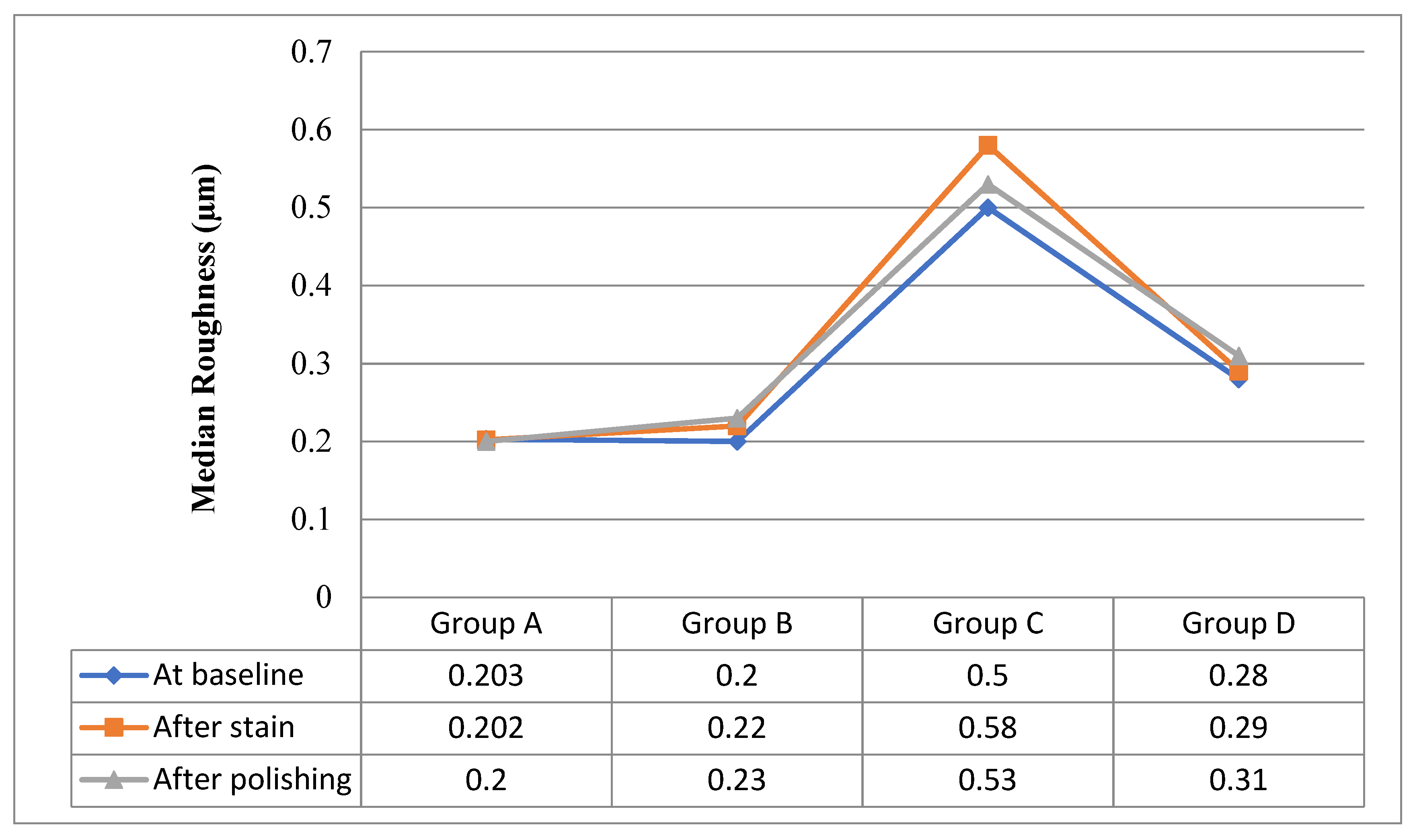
3.2. Surface Roughness Measurement
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Dutta, S.; Maria, R. The effect of various polishing systems on surface roughness of nano and microhybrid composite restoratives: An in vitro surface profilometric study. Indian J. Appl. Med. Res. 2012, 3, 214–220. [Google Scholar]
- Lal, S.M.; Jagadish, S. Direct composite veneering technique producing a smile design with a customized matrix. J. Conserv. Dent. 2006, 9, 87–92. [Google Scholar] [CrossRef]
- Backes, C.N.; FranÇa, F.M.G.; Turssi, C.P.; Amaral, F.L.B.D.; Basting, R.T. Color stability of a bulk-fill composite resin light-cured at different distances. Braz. Oral Res. 2020, 34, e119. [Google Scholar] [CrossRef] [PubMed]
- Fontes, S.T.; Fernandez, M.R.; De Moura, C.M.; Meireles, S.S. Color stability of a nanofill composite: Effect of different immersion media. J. Appl. Oral Sci. 2009, 17, 388–391. [Google Scholar] [CrossRef]
- Villalta, P.; Lu, H.; Okte, Z.; Garcia-Godoy, F.; Powers, J.M. Effects of staining and bleaching on color change of dental composite resins. J. Prosthet. Dent. 2006, 95, 137–142. [Google Scholar] [CrossRef]
- Patel, S.B.; Gordan, V.V.; Barrett, A.A.; Shen, C. The effect of surface finishing and storage solutions on the color stability of resin-based composites. J. Am. Dent. Assoc. 2004, 135, 587–594. [Google Scholar] [CrossRef]
- Bagheri, R.; Burrow, M.F.; Tyas, M. Influence of food-simulating solutions and surface finish on susceptibility to staining of aesthetic restorative materials. J. Dent. 2005, 33, 389–398. [Google Scholar] [CrossRef]
- Bollen, C.M.L.; Lambrechts, P.; Quirynen, M. Comparison of surface roughness of oral hard materials to the threshold surface roughness for bacterial plaque retention: A review of the literature. Dent. Mater. 1997, 13, 258–269. [Google Scholar] [CrossRef]
- Beltrami, R.; Ceci, M.; De Pani, G.; Vialba, L.; Federico, R.; Poggio, C.; Colombo, M. Effect of different surface finishing/polishing procedures on color stability of esthetic restorative materials: A spectrophotometric evaluation. Eur. J. Dent. 2018, 12, 49–56. [Google Scholar] [CrossRef]
- Pettini, F.; Corsalini, M.; Savino, M.G.; Stefanachi, G.; Di Venere, D.; Pappalettere, C.; Monno, G.; Boccaccio, A. Roughness Analysis on Composite Materials (Microfilled, Nanofilled and Silorane) after Different Finishing and Polishing Procedures. Open Dent. J. 2015, 9, 357–367. [Google Scholar] [CrossRef] [Green Version]
- Jurado, C.A.; Tsujimoto, A.; Watanabe, H.; Fischer, N.G.; Hasslen, J.A.; Tomeh, H.; Baruth, A.G.; Barkmeier, W.W.; Garcia-Godoy, F. Evaluation of Polishing Systems for CAD/CAM Polymer-Infiltrated Ceramic-Network Restorations. Oper. Dent. 2021, 46, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Kocaagaoglu, H.; Aslan, T.; Gürbulak, A.; Albayrak, H.; Taşdemir, Z.; Gumus, H. Efficacy of polishing kits on the surface roughness and color stability of different composite resins. Niger. J. Clin. Pract. 2017, 20, 557–565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Madhyastha, P.S.; Hegde, S.; Srikant, N.; Kotian, R.; Iyer, S.S. Effect of finishing/polishing techniques and time on surface roughness of esthetic restorative materials. Dent. Res. J. 2017, 14, 326–330. [Google Scholar] [CrossRef]
- Bertoldo, C.; Miranda, D.; Junior, E.; Aguiar, F.; Lima, D. Evaluation of surface roughness and color stability of direct resin composites after different polishing protocols. Dent. Clin. N. Am. 2011, 3, 4–7. [Google Scholar]
- Kevin, B. How to match any composite restoration shade: Tokuyama’s OMNICHROMA Uses Smart Chromatic Technology to Match a Wider Range of Natural Teeth Colors. Dent. Prod. Rep. 2019, 53, 36. [Google Scholar]
- Sampath, S. Survival times of restorative parameters vis-à-vis material combinations. J. Res. Dent. 2015, 3, 14–20. [Google Scholar] [CrossRef]
- Abzal, M.S.; Rathakrishnan, M.; Prakash, V.; Vivekanandhan, P.; Subbiya, A.; Sukumaran, V.G. Evaluation of surface roughness of three different composite resins with three different polishing systems. J. Conserv. Dent. 2016, 19, 171–174. [Google Scholar]
- Freitas, F.; Pinheiro de Melo, T.; Delgado, A.H.; Monteiro, P.; Rua, J.; Proença, L.; Caldeira, J.; Mano Azul, A.; Mendes, J.J. Varying the Polishing Protocol Influences the Color Stability and Surface Roughness of Bulk-Fill Resin-Based Composites. J. Funct. Biomater. 2021, 12, 1. [Google Scholar] [CrossRef]
- Paolone, G.; Mazzitelli, C.; Josic, U.; Scotti, N.; Gherlone, E.; Cantatore, G.; Breschi, L. Modeling Liquids and Resin-Based Dental Composite Materials—A Scoping Review. Materials 2022, 15, 3759. [Google Scholar] [CrossRef]
- Jaramillo-Cartagena, R.; López-Galeano, E.J.; Latorre-Correa, F.; Agudelo-Suárez, A.A. Effect of Polishing Systems on the Surface Roughness of Nano-Hybrid and Nano-Filling Composite Resins: A Systematic Review. Dent. J. 2021, 9, 95. [Google Scholar] [CrossRef]
- Lehmann, A.; Nijakowski, K.; Potempa, N.; Sieradzki, P.; Król, M.; Czyż, O.; Radziszewska, A.; Surdacka, A. Press-On Force Effect on the Efficiency of Composite Restorations Final Polishing—Preliminary In Vitro Study. Coatings 2021, 11, 705. [Google Scholar] [CrossRef]
- Barakah, H.; Taher, N. Effect of polishing systems on stain susceptibility and surface roughness of nanocomposite resin material. J. Prosthet. Dent. 2014, 112, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Polli, M.; Arossi, G. Effect of finishing and polishing on the color stability of a composite resin immersed in staining solutions. J. Dent. Res. Rev. 2015, 2, 120–126. [Google Scholar]
- Sensi, L.; Winkler, C.; Geraldeli, S. Accelerated Aging Effects on Color Stability of Potentially Color Adjusting Resin-based Composites. Oper. Dent. 2021, 46, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Rueggeberg, F.A.; Margeson, D.H. The Effect of Oxygen Inhibition on an Unfilled/Filled Composite System. J. Dent. Res. 1990, 69, 1652–1658. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.A.; Dunn, K.; Afutu, R.; Tran, D.; Ghanem, J.; Perry, R.; Kugel, G. Shade-Matching Capacity of Omnichroma in Anterior Restorations. J. Dent. Sci. 2020, 5, 1–7. [Google Scholar]
- Hamadamin, D.I.; Saeed, D.H. The Impact of Energy Drinks on Surface Roughness, Hardness, and Color Stability of Three Types of Composite Restorations. J. Hunan Univ. Nat. Sci. 2021, 48, 335–348. [Google Scholar]
- Alghamdi, A.; Algarni, A.; Eskandrani, R.M.; Alazmi, K.F. Influence of Energy and Soft Drinks on the Surface and Mechanical Properties of Nanofilled Composite Resin. Int. J. Dent. Sci. Res. 2019, 7, 44–48. [Google Scholar]
- Aldharrab, A. Effect of Energy Drinks on the Color Stability of Nanofilled Composite Resin. J. Contemp. Dent. Pract. 2013, 14, 704–711. [Google Scholar] [CrossRef]
- Chowdhury, D.; Mazumdar, P.; Desai, P.; Datta, P. Comparative evaluation of surface roughness and color stability of nanohybrid composite resin after periodic exposure to tea, coffee, and Coca-cola—An in vitro profilometric and image analysis study. J. Conserv. Dent. 2020, 23, 395–401. [Google Scholar] [CrossRef]
- Kumari, R.V.; Nagaraj, H.; Siddaraju, K.; Poluri, R.K. Evaluation of the Effect of Surface Polishing, Oral Beverages and Food Colorants on Color Stability and Surface Roughness of Nanocomposite Resins. J. Int. Oral Health 2015, 7, 63–70. [Google Scholar] [PubMed]
- Dhananjaya, K.M.; Vadavadagi, S.V.; Almalki, S.A.; Verma, T.; Arora, S.; Kumar, N.N. In Vitro Analysis of Different Polishing Systems on the Color Stability and Surface Roughness of Nanocomposite Resins. J. Contemp. Dent. Pract. 2019, 20, 1335–1338. [Google Scholar] [PubMed]
- Yadav, R.D.; Raisingani, D.; Jindal, D.; Mathur, R. A Comparative Analysis of Different Finishing and Polishing Devices on Nanofilled, Microfilled, and Hybrid Composite: A Scanning Electron Microscopy and Profilometric Study. Int. J. Clin. Pediatr. Dent. 2016, 9, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Robertson, L.; Phaneuf, M.; Haimeur, A.; Pesun, I.; França, R. Degree of conversion and oxygen-inhibited layer effect of three dental adhesives. Dent. J. 2016, 4, 37. [Google Scholar] [CrossRef] [Green Version]
- Alkhadim, Y.K.; Hulbah, M.J.; Nassar, H.M. Color Shift, Color Stability, and Post-Polishing Surface Roughness of Esthetic Resin Composites. Materials 2020, 13, 1376. [Google Scholar] [CrossRef] [Green Version]
- AlSheikh, R. Color stability of Lucirin-photo-activated resin composite after immersion in different staining solutions: A spectrophotometric study. Clin. Cosmet. Investig. Dent. 2019, 11, 297–311. [Google Scholar] [CrossRef] [Green Version]
- Piccoli, Y.B.; Lima, V.P.; Basso, G.R.; Salgado, V.E.; Lima, G.S.; Moraes, R.R. Optical Stability of High-translucency Resin-based Composites. Oper. Dent. 2019, 44, 536–544. [Google Scholar] [CrossRef]
- Yazdi, H.K.; Nasoohi, N.; Benvidi, M. In Vitro Efficacy of Listerine Whitening Mouthwash for Color Recovery of Two Discolored Composite Resins. Front. Dent. 2019, 16, 181–186. [Google Scholar] [CrossRef]
- Abdulwahhab, Z.S.; Alkhalidi, E.F. Effect of Staining and Bleaching on Surface Roughness of Different Nano Hybrid Resin Composite Materials. Al-Rafidain Dent. J. 2021, 21, 42–50. [Google Scholar] [CrossRef]
- Aydın, N.; Karaoğlanoğlu, S.; Oktay, E.A.; Ersöz, B. Investigation of Single Shade Composite Resin Surface Roughness and Color Stability. Atatürk Üniversitesi Diş Hekim. Fakültesi Derg. 2021, 31, 207–214. [Google Scholar] [CrossRef]
- Carrillo-Marcos, A.; Salazar-Correa, G.; Castro-Ramirez, L.; Ladera-Castañeda, M.; López-Gurreonero, C.; Cachay-Criado, H.; Aliaga-Mariñas, A.; Cornejo-Pinto, A.; Cervantes-Ganoza, L.; Cayo-Rojas, C.F. The Microhardness and Surface Roughness Assessment of Bulk-Fill Resin Composites Treated with and without the Application of an Oxygen-Inhibited Layer and a Polishing System: An In Vitro Study. Polymers 2022, 14, 3053. [Google Scholar] [CrossRef] [PubMed]
- Veček, N.N.; Par, M.; Sever, E.K.; Miletić, I.; Krmek, S.J. The Effect of a Green Smoothie on Microhardness, Profile Roughness and Color Change of Dental Restorative Materials. Polymers 2022, 14, 2067. [Google Scholar] [CrossRef] [PubMed]
- Kumari, C.M.; Bhat, K.M.; Bansal, R.; Singh, N.; Anupama, A.; Lavanya, T. Evaluation of Surface Roughness and Hardness of Newer Nanoposterior Composite Resins after Immersion in Food-Simulating Liquids. Contemp. Clin. Dent. 2019, 10, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, C.S.; Mozzaquatro, L.R.; Dala Nora, B.; Jacques, L.B.; Mallmann, A. Effect of bleaching on color stability and roughness of composite resins aged in staining beverage. Gen. Dent. 2017, 65, e5–e10. [Google Scholar]
| Material | Type | Lot no. | Shade | Filler Weight | Monomer | Manufacturer |
|---|---|---|---|---|---|---|
| Filtek Z350 | Nano-filled | NE14538 | A2 | 72.50% | Bis-GMA, UDMA, Bis-EMA, TEGDMA | 3M Oral Care St. Paul, MN, USA |
| IPS Empress Direct | Nanohybrid | Z0199Y | A2 | 75–79% | Dimethacrylates 20–21.5 wt% | Ivoclar Vivadent Liechtenstein, Zurich |
| Omnichroma | Supra-nano spherical filler | 1081 | A1 to D4 | 79% | UDMA, TEGDMA | Tokuyama Dental, Tokyo, Japan |
| Estalite Palfique LX5 | Supra-nano spherical filler | 468 | A2 | 82% | Bis-GMA, Triethylene glycol dimethacrylate. | Tokuyama Dental, Tokyo, Japan |
| Baseline Color (T0) (No = 15) | After Stain (T1) (No = 15) | After Polishing (T2) (No = 15) | Test of Significance (p) | |
|---|---|---|---|---|
| Omnichroma | (X2Friedman = 30, p < 0.0001) | |||
| L* | 75.8 (74.8–76.0) | 69.6 (68.7–70.7) | 73.9 (72.3–75.2) | |
| Sig detected between episodes | {(L1 vs. L0) and (L2 vs. (L0&L1))} | |||
| a* | 1.6 (1.4–1.7) | 4.6 (4.2–4.9) | 1.3 (0.8–1.8) | (X2Friedman = 27.76, p < 0.00001) |
| Sig detected between episodes | a1 vs. (a0&a2) | |||
| b* | 13.4 (12.9–13.8) | 15.8 (15.1–16.5) | 13.1 (11.0–14.0) | (X2Friedman = 26.9, p < 0.0001) |
| Sig detected between episodes | b1 vs. (b0&b2) | |||
| IPS Empress Direct | (X2Friedman = 28.1, p < 0.0001) | |||
| L* | 70.0 (69.2–70.5) | 63.2 (61.9–70.1) | 71.8 (70.2–72.6) | |
| Sig detected between episodes | L1 vs. (L0&L2) | |||
| a* | 1.3 (1.1–2.4) | 7.6 (6.5–8.1) | 1.1 (0.8–1.4) | (X2Friedman = 28, p < 0.0001) |
| Sig detected between episodes | a1 vs. (a0&a2) | |||
| b* | 19.2 (17.3–20.0) | 22.5 (18.5–28.0) | 18.9 (18.1–19.5) | (X2Friedman = 17.4, p < 0.0001) |
| Sig detected between episodes | b1 vs. (b0&b2) | |||
| Estalite Palfique LX5 | (X2Friedman = 25.2, p < 0.0001) | |||
| L* | 73.2 (72.1–5.2) | 69.4 (68.0–71.0) | 74.2 (73.7–75.1) | |
| Sig detected between episodes | L1 vs. (L0&L2) | |||
| a* | 0.4 (0.0–1.1) | 1.0 (0.9–1.4) | 0.7 (0.1–1.1) | (X2Friedman = 19.6, p <0.0001) |
| Sig detected between episodes | a1 vs. (a0&a2) | |||
| b* | 20.5 (19.0–22.4) | 22.2 (21.4–23.2) | 20.4 (19.1–22.1) | (X2Friedman = 17.2, p < 0.0001) |
| Sig detected between episodes | b1 vs. (b0&b2) | |||
| Filtek Z350 | (X2Friedman = 25.1, p < 0.0001) | |||
| L* | 75.2 (74.8–75.9) | 70.8 (68.3–72.3) | 74.7 (74.3–75.3) | |
| Sig detected between episodes | L1 vs. (L0&L2) | |||
| a* | 1.2 (1.0–1.4) | 1.2 (0.8–1.7) | 1.4 (1.2–1.7) | (X2Friedman = 20.7, p < 0.0001) |
| Sig detected between episodes | a1 vs. (a0&a2) | |||
| b* | 12.5 (10.1–14.2) | 19.1 (18.0–19.7) | 12.0 (11.4–12.9) | (X2Friedman = 23.4, p < 0.0001) |
| Sig detected between episodes | b1 vs. (b0&b2) | |||
| Color Change after Stain (T1) | Color Change after Polishing (T2) | Test of Significance (p) | |
|---|---|---|---|
| Omnichroma | −6.1 (−6.7–0.0) | −1.4 (−2.9–−0.2) | (z= −3.35, p = 0.001) |
| ΔL* | |||
| Δa* | 3.1 (2.6–3.2) | −0.3 (−0.6–0.1) | (z = 3.42, p = 0.001) |
| Δb* | 2.1 (1.9–3.0) | 0.0 (−2.4–1.0) | (z = 3.41, p = 0.001) |
| ΔE | 7.1 (4.06–7.79) | 1.7 (0.22–3.1) | (z = −3.41, p = 0.001) |
| IPS Empress Direct | (z = −3.41, p = 0.001) | ||
| ΔL* | −6.6 (−8.5–−0.4) | 1.8 (−0.3–2.7) | |
| Δa* | 6.1 (5.0–6.8) | −0.1 (−1.2–0.0) | (z = −3.41, p = 0.001) |
| Δb* | 4.0 (−0.7–9.8) | −0.3 (−1.0–1.8) | (z = −3.23, p = 0.001) |
| ΔE | 9.54 (7.23–14.21) | 1.99 (0.62–2.98) | (z = −3.41, p = 0.001) |
| Estalite Palfique LX5 | (z = −3.41, p = 0.001) | ||
| ΔL* | −3.9 (−7.2–−2.1) | 1.3 (−1.2–3.0) | |
| Δa* | 0.7 (−0.2–1.4) | 0.4 (−1.0–1.1) | (z = −3.06, p = 0.001) |
| Δb* | 1.6 (−0.3–3.6) | 0.0 (−2.4–2.6) | (z = −3.29, p = 0.001) |
| ΔE | 4.72 (2.4–7.69) | 1.75 (0.24–3.5) | (z = −3.29, p = 0.001) |
| Filtek Z350 | (z = −3.41, p = 0.001) | ||
| ΔL* | −4.8 (−7.0–−3.2) | −0.5 (−1.5–0.2) | |
| Δa* | 0.0 (−0.4–0.5) | 0.3 (0.0–0.7) | (z = 3.2, p = 0.001) |
| Δb* | 6.3 (4.5–9.5) | −0.5 (−2.8–2.6) | (z = 3.4, p = 0.001) |
| ΔE | 7.75 (6.0–11.4) | 1.66 (0.24–3.22) | (z = −3.4, p = 0.001) |
| Roughness (µm) | Roughness (Baseline) | Roughness (After Stain) | Roughness (After Polishing) | Test of Significance (p) |
|---|---|---|---|---|
| Omnichroma | 0.203 (0.084–0.543) | 0.202 (0.117–0.793) | 0.2 (0.1–0.63) | (X2Friedman = 4.8, p = 0.09) |
| IPS Empress Direct | 0.2 (0.09–0.42) | 0.22 (0.1–0.57) | 0.23 (0.1–0.44) | (X2Friedman = 2.8, p = 0.247) |
| Estalite Palfique LX5 | 0.5 (0.27–0.78) | 0.58 (0.31–0.9) | 0.53 (0.29–0.81) | (X2Friedman = 16.8, p = 0.0001) |
| Sig detected between Roughness episodes | (Roughness at baseline) vs. (Roughness after stain) | |||
| Filtek Z350 | 0.28 (0.17–0.54) | 0.29 (0.22–0.6) | 0.31 (0.15–0.51) | (X2Friedman = 4.2, p = 0.12) |
| Roughness (µm) | Omnichroma (No = 15) | IPS Empress Direct (No = 15) | Estalite Palfique LX5 (No = 15) | Filtek Z350 (No = 15) | Test of Significance (p) |
|---|---|---|---|---|---|
| At baseline | 0.203 (0.084–0.543) | 0.2 (0.09–0.42) | 0.5 (0.27–0.78) | 0.28 (0.17–0.54) | (H= 24.9, p = 0.0001) |
| Sig between groups | Group C vs. {group A& group B & group D} | ||||
| After stain | 0.202 (0.117–0.793) | 0.22 (0.1–0.57) | 0.58 (0.31–0.9) | 0.29 (0.22–0.6) | (H= 25.2, p = 0.0001) |
| Sig between groups | Group C vs. {group A& group B & group D} | ||||
| After polishing | 0.2 (0.1–0.63) | 0.23 (0.1–0.44) | 0.53 (0.29–0.81) | 0.31 (0.15–0.51) | (H= 27.5, p = 0.0001) |
| Sig between groups | Group C vs. {group A& group B & group D} | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshehri, A.; Alhalabi, F.; Mustafa, M.; Awad, M.M.; Alqhtani, M.; Almutairi, M.; Alhijab, F.; Jurado, C.A.; Fischer, N.G.; Nurrohman, H.; et al. Effects of Accelerated Aging on Color Stability and Surface Roughness of a Biomimetic Composite: An In Vitro Study. Biomimetics 2022, 7, 158. https://doi.org/10.3390/biomimetics7040158
Alshehri A, Alhalabi F, Mustafa M, Awad MM, Alqhtani M, Almutairi M, Alhijab F, Jurado CA, Fischer NG, Nurrohman H, et al. Effects of Accelerated Aging on Color Stability and Surface Roughness of a Biomimetic Composite: An In Vitro Study. Biomimetics. 2022; 7(4):158. https://doi.org/10.3390/biomimetics7040158
Chicago/Turabian StyleAlshehri, Abdullah, Feras Alhalabi, Mohammed Mustafa, Mohamed M. Awad, Mohammed Alqhtani, Mohammed Almutairi, Faisal Alhijab, Carlos A. Jurado, Nicholas G. Fischer, Hamid Nurrohman, and et al. 2022. "Effects of Accelerated Aging on Color Stability and Surface Roughness of a Biomimetic Composite: An In Vitro Study" Biomimetics 7, no. 4: 158. https://doi.org/10.3390/biomimetics7040158
APA StyleAlshehri, A., Alhalabi, F., Mustafa, M., Awad, M. M., Alqhtani, M., Almutairi, M., Alhijab, F., Jurado, C. A., Fischer, N. G., Nurrohman, H., & Alshabib, A. (2022). Effects of Accelerated Aging on Color Stability and Surface Roughness of a Biomimetic Composite: An In Vitro Study. Biomimetics, 7(4), 158. https://doi.org/10.3390/biomimetics7040158











