Biomimicking Atherosclerotic Vessels: A Relevant and (Yet) Sub-Explored Topic
Abstract
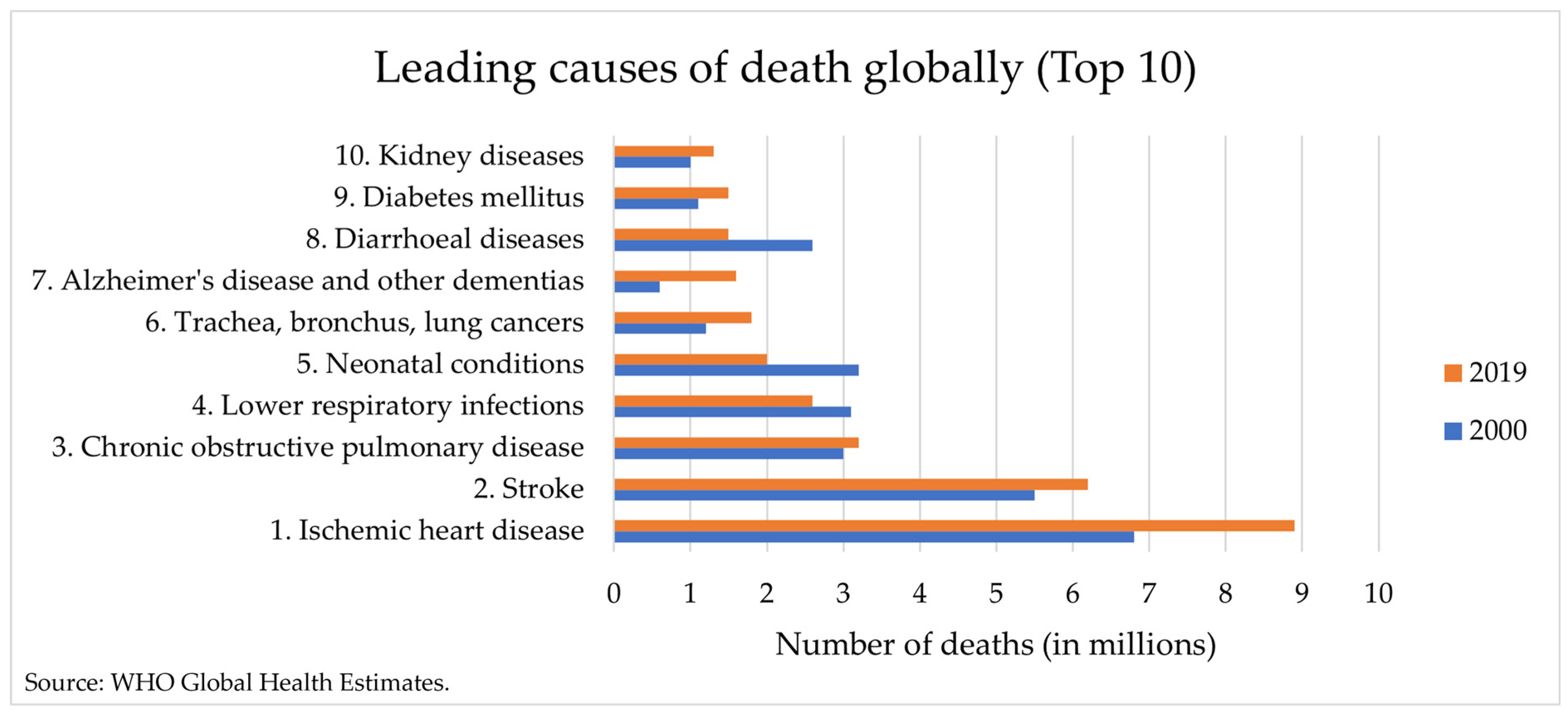
1. Introduction
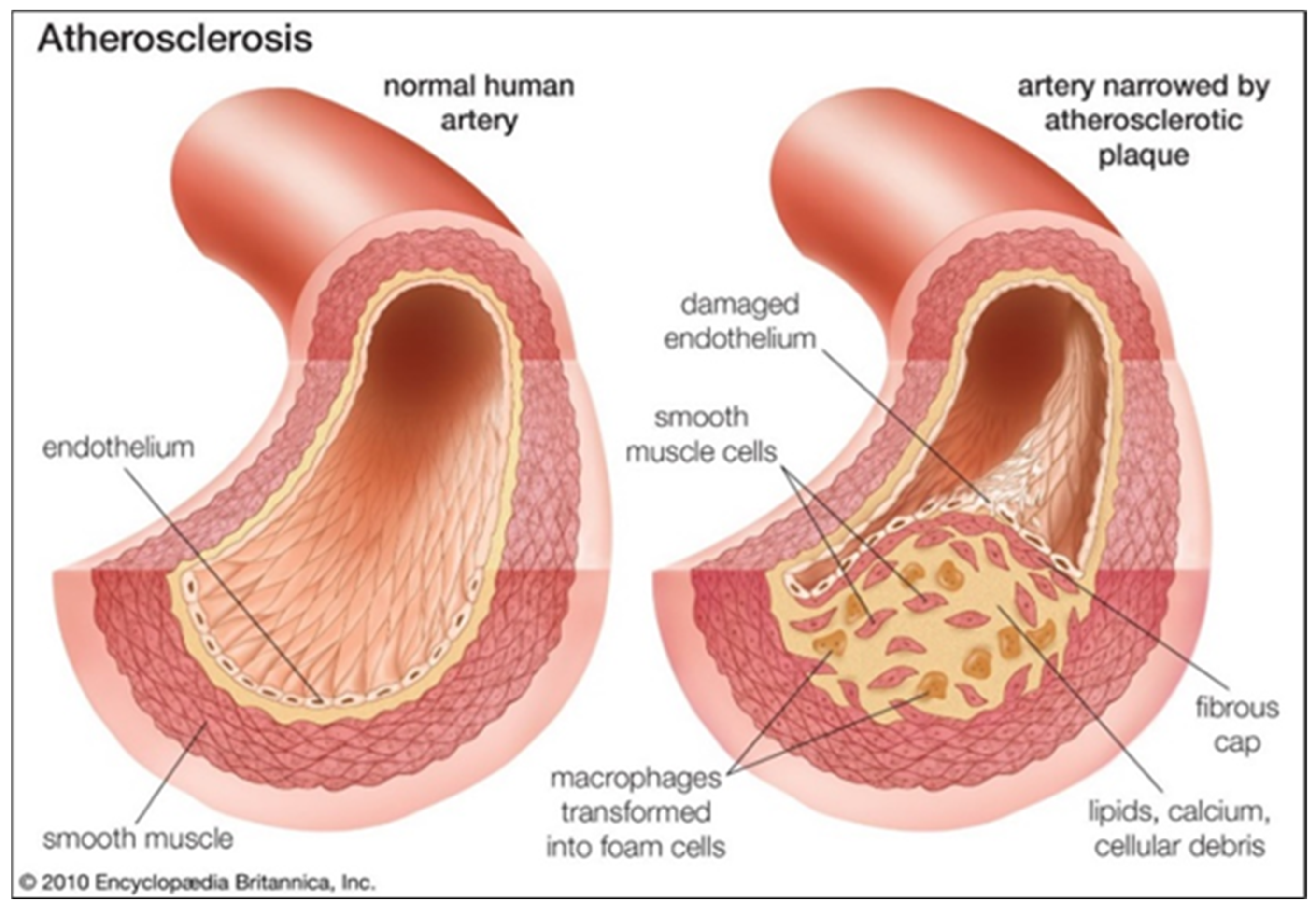
2. Pathophysiology of Atherosclerosis
3. Applications of Biomimetic Vascular Models for Atherosclerosis
3.1. Imaging Protocols Optimization
3.1.1. Ultrasonography
3.1.2. Computed Tomography
3.1.3. Magnetic Resonance Imaging
3.1.4. Optical Coherence Tomography
3.2. Hemodynamic Studies (Flow Models)
3.3. Validation of Numerical Studies
3.4. Clinical Practice Assistance
3.5. Assessment of Novel Therapeutic Strategies
4. Conclusions and Prospects
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Turner, M.B.; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322. [Google Scholar] [CrossRef]
- Timmis, A.; Townsend, N.; Gale, C.P.; Torbica, A.; Lettino, M.; Petersen, S.E.; Mossialos, E.A.; Maggioni, A.P.; Kazakiewicz, D.; May, H.T.; et al. European Society of Cardiology: Cardiovascular Disease Statistics 2019. Eur. Heart J. 2020, 41, 12–85. [Google Scholar] [CrossRef]
- Wang, X.; Gao, B.; Feng, Y. Recent advances in inhibiting atherosclerosis and restenosis: From pathogenic factors, therapeutic molecules to nano-delivery strategies. J. Mater. Chem. B 2022, 10, 1685. [Google Scholar] [CrossRef]
- Kobielarz, M.; Kozun, M.; Gasior-Glogowska, M.; Chwilkowska, A. Mechanical and structural properties of different types of human atherosclerotic plaques. J. Mech. Behav. Biomed. Mater. 2020, 109, 103837. [Google Scholar] [CrossRef]
- Bergheanu, S.C.; Bodde, M.C.; Jukema, J.W. Pathophysiology and treatment of atherosclerosis. Neth. Heart J. 2017, 25, 231–242. [Google Scholar] [CrossRef]
- Holzapfle, G.; Sommer, G.; Regitnig, P. Anisotropic Mechanical Properties of Tissue Components in Human Atherosclerotic Plaques. J. Biomech. Eng. 2004, 126, 657–665. [Google Scholar] [CrossRef]
- Gold, K.; Gaharwar, A.K.; Jain, A. Emerging trends in multiscale modeling of vascular pathophysiology: Organ-on-a-chip and 3D printing. Biomaterials 2019, 196, 2–17. [Google Scholar] [CrossRef]
- World Health Organization. The Top 10 Causes of Death. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 18 December 2023).
- Britannica. Atherosclerosis—Pathology. Available online: https://www.britannica.com/science/atherosclerosis (accessed on 18 December 2023).
- Stephen, S.L.; Freestone, K.; Dunn, S.; Twigg, M.W.; Homer-Vanniasinkam, S.; Walker, J.H.; Wheatcroft, S.B.; Ponnambalam, S. Scavenger Receptors and Their Potential as Therapeutic Targets in the Treatment of Cardiovascular Disease. Int. J. Hypertens. 2010, 2010, 646929. [Google Scholar] [CrossRef]
- Johns Hopkins Medicine. Atherosclerosis. Available online: https://www.hopkinsmedicine.org/health/conditions-and-diseases/atherosclerosis (accessed on 30 November 2023).
- Byrne, R.A.; Stone, G.W.; Ormiston, J.; Kastrati, A. Coronary balloon angioplasty, stents, and scaffolds. Lancet 2017, 390, 781–792. [Google Scholar] [CrossRef]
- Sousa, A.M.; Amaro, A.M.; Piedade, A.P. 3D Printing of Polymeric Bioresorbable Stents: A Strategy to Improve Both Cellular Compatibility and Mechanical Properties. Polymers 2022, 14, 1099. [Google Scholar] [CrossRef]
- Hicks, C.W.; Holscher, C.M.; Wang, P.; Dun, C.; Abularrage, C.J.; Black, J.H.; Hodgson, K.J.; Makary, M.A. Use of Atherectomy During Index Peripheral Vascular Interventions. JACC Cardiovasc. Interv. 2021, 14, 678–688. [Google Scholar] [CrossRef]
- Hangge, P.; Pershad, Y.; Witting, A.A.; Albadawi, H.; Rahmi, O. Three-dimensional (3D) printing and its applications for aortic diseases. Cardiovasc. Diagn. Ther. 2018, 8, S19–S25. [Google Scholar] [CrossRef]
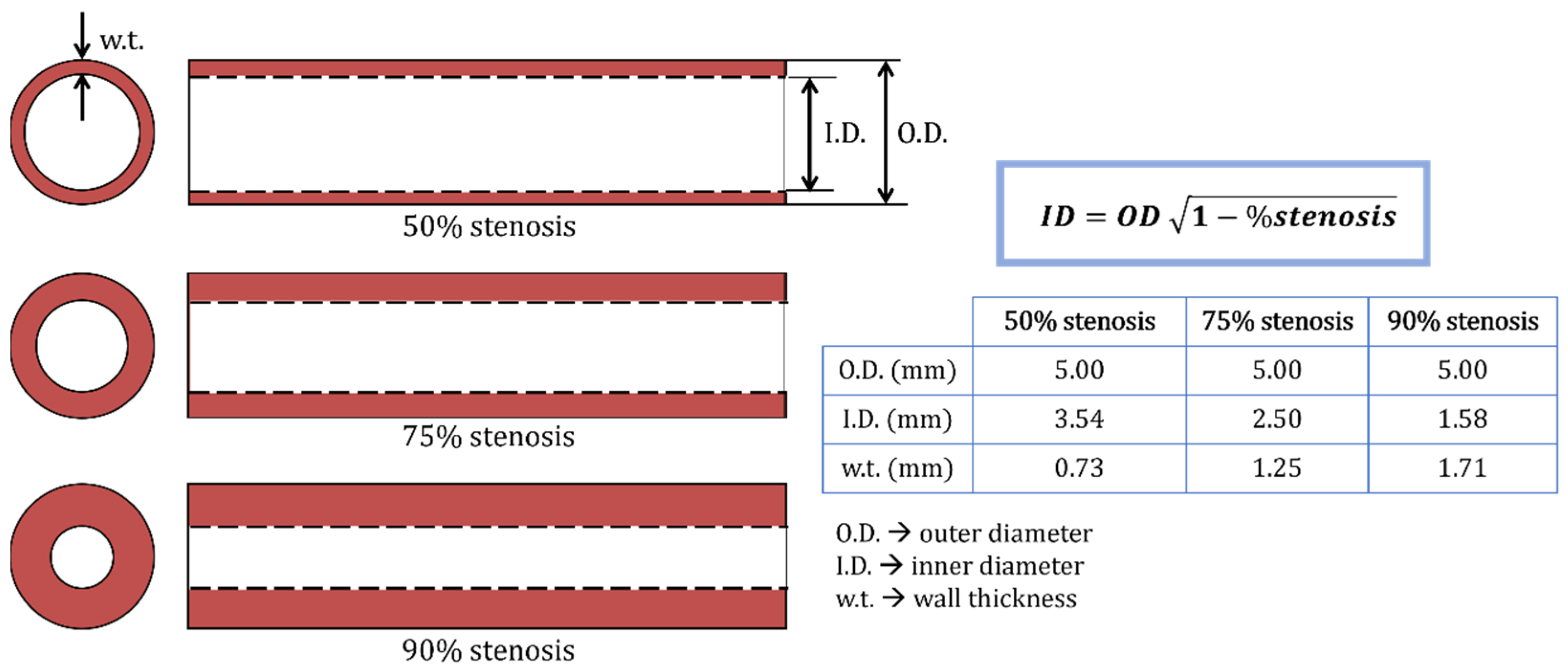
- Friedrich, T.; Wegner, F.; Buzug, T.M. 3D printing of elastic stenosis phantoms. Trans. AMMM 2020, 2. [Google Scholar] [CrossRef]
- Kiraly, L.; Tofeig, M.; Jha, N.K.; Talo, H. Three-dimensional printed prototypes refine the anatomy of post-modified Norwood-1 complex aortic arch obstruction and allow presurgical simulation on repair. Interact. Cardiovas. Thorac. Surg. 2016, 22, 238–240. [Google Scholar] [CrossRef]
- Russ, M.; O’Hara, R.; Setlur Nagesh, S.V.S.; Mokin, M.; Jimenez, C.; Siddiqui, A.; Bednarek, D.; Rudin, S.; Ionita, C. Treatment planning for image-guided neuro-vascular interventions using patient-specific 3D printed phantoms. In Proceedings of the Medical Imaging 2015: Biomedical Applications in Molecular, Structural, and Functional Imaging, Orlando, FL, USA, 21–26 February 2015; Volume 9417. [Google Scholar] [CrossRef]
- Higgins, M.; Leung, S.; Radacsi, N. 3D printing surgical phantoms and their role in the visualization of medical procedures. Ann. 3D Print. Med. 2022, 6, 100057. [Google Scholar] [CrossRef]
- Wu, Y.; Chee, A.J.Y.; Golzar, H.; Yu, A.C.H.; Tang, X. Embedded 3D Printing of Ultrasound-Compatible Arterial Phantoms with Biomimetic Elasticity. Adv. Funct. Mater. 2022, 32, 2110153. [Google Scholar] [CrossRef]
- Valeanu, L.; Ginghina, C.; Bubenek-Turconi, S. Blood Rheology Alterations in Patients with Cardiovascular Diseases. Rom. J. Anaesth. Intensive Care 2021, 28, 41–46. [Google Scholar] [CrossRef]
- Hashemi, J.; Patel, B.; Chatzizisis, Y.S.; Kassab, G.S. Study of Coronary Atherosclerosis Using Blood Residence Time. Front. Physiol. 2021, 12, 625420. [Google Scholar] [CrossRef]
- Carvalho, V.; Rodrigues, N.; Ribeiro, R.; Costa, P.F.; Lima, R.A.; Teixeira, S.F. 3D printed biomodels for flow visualization in stenotic vessels: An experimental and numerical study. Micromachines 2020, 11, 549. [Google Scholar] [CrossRef]
- Mallone, A.; Stenger, C.; Eckardstein, A.V.; Hoerstrup, S.P.; Weber, B. Biofabricating atherosclerotic plaques: In vitro engineering of a three-dimensional human fibroatheroma model. Biomaterials 2018, 150, 49–59. [Google Scholar] [CrossRef]
- Razzi, F.; Lovrak, M.; Gruzdyte, D.; Hartog, Y.D.; Duncker, D.J.; van Esch, J.H.; van Steijn, V.; van Beusekom, H.M.M. An implantable artificial atherosclerosis plaque as a novel approach for drug transport studies on drug-eluting stents. Adv. Healthc. Mater. 2022, 11, 2101570. [Google Scholar] [CrossRef]
- Garcia-Sabaté, A.; Mohamed, W.K.E.; Sapudom, J.; Alatoom, A.; Safadi, L.A.; Teo, J.C.M. Biomimetic 3D Models for Investigating the Role of Monocytes and Macrophages in Atherosclerosis. Bioengineering 2020, 7, 113. [Google Scholar] [CrossRef]
- Henriques, J.; Amaro, A.M.; Piedade, A.P. Understanding Atherosclerosis Pathophysiology: Can Additive Manufacturing Be Helpful? Polymers 2023, 15, 480. [Google Scholar] [CrossRef]
- Stary, H.C.; Chandler, A.B.; Dinsmore, R.E.; Fuster, V.; Glagov, S.; Insull, W.; Rosenfeld, M.E.; Schwartz, C.J.; Wagner, W.D.; Wissler, R.W. A definition of advanced types of atherosclerotic lesions and a histological classification of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Circulation 1995, 92, 1355–1374. [Google Scholar] [CrossRef]
- Poznyak, A.V.; Grechko, A.V.; Orekhova, V.A.; Chegodaev, Y.S.; Wu, W.-K.; Orekhov, A.N. Oxidative stress and antioxidants in atherosclerosis development and treatment. Biology 2020, 9, 60. [Google Scholar] [CrossRef]
- Hu, B.; Boakye-Yiadom, K.O.; Yu, W.; Yuan, Z.-W.; Ho, W.; Xu, X.; Zhang, X.-Q. Nanomedicine Approaches for Advanced Diagnosis and Treatment of Atherosclerosis and Related Ischemic Diseases. Adv. Healthc. Mater. 2020, 9, 2000336. [Google Scholar] [CrossRef] [PubMed]
- Chiu, J.-J.; Chien, S. Effects of Disturbed Flow on Vascular Endothelium: Pathophysiological Basis and Clinical Perspectives. Physiol. Rev. 2011, 91, 327–387. [Google Scholar] [CrossRef]
- Shi, X.; Gao, J.; Lv, Q.; Cai, H.; Wang, F.; Ye, R.; Liu, X. Calcification in Atherosclerotic Plaque Vulnerability: Friend or Foe? Front. Physiol. 2020, 11, 56. [Google Scholar] [CrossRef] [PubMed]
- Wong, K.; Thavornpattanapong, P.; Cheung, S.; Sun, Z.; Tu, J. Effect of calcification on the mechanical stability of plaque based on a three-dimensional carotid bifurcation model. BMC Cardiovasc. Disord. 2012, 12, 7. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Li, X.; Zhao, X.; Zhou, W.; Cai, Z.; Yang, L.; Guo, A.; Zhao, S. Classification of Human Coronary Atherosclerotic Plaques Using Ex Vivo High-Resolution Multicontrast-Weighted MRI Compared With Histopathology. AJR Am. J. Roentgenol. 2012, 198, 1069–1075. [Google Scholar] [CrossRef] [PubMed]
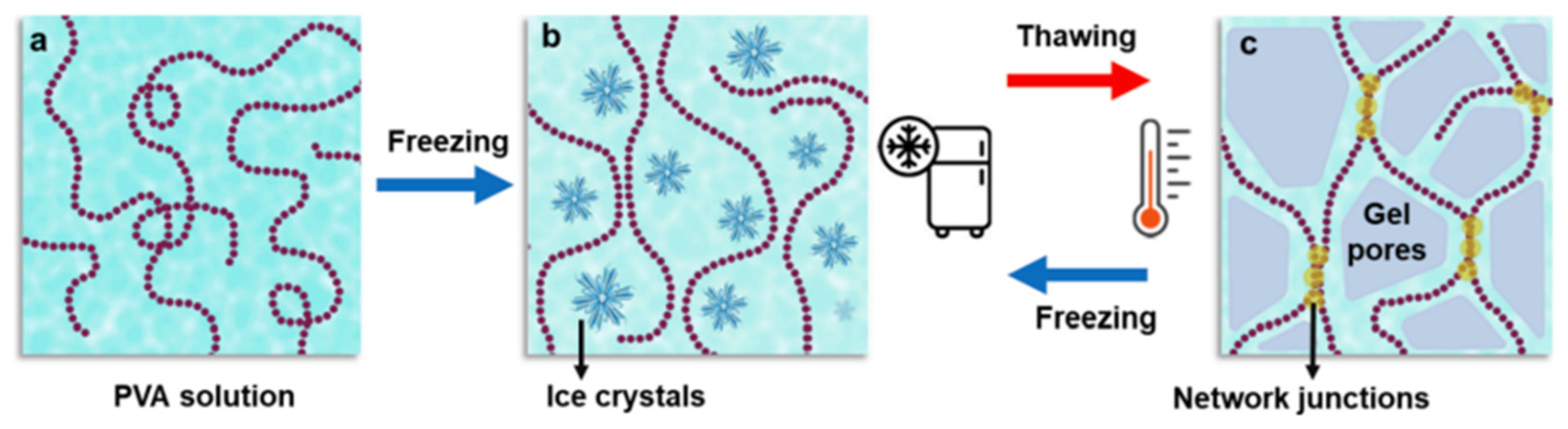
- Malone, A.J.; Cournane, S.; Naydenova, I.G.; Fagan, A.J.; Browne, J.E. Polyvinyl alcohol cryogel based vessel mimicking material for modelling the progression of atherosclerosis. Phys. Medica 2020, 69, 1–8. [Google Scholar] [CrossRef]
- Stupic, K.F.; Ainslie, M.; Boss, M.A.; Charles, C.; Dienstfrey, A.M.; Evelhoch, J.L.; Finn, P.; Gimbutas, Z.; Gunter, J.L.; Hill, D.L.G.; et al. A standard system phantom for magnetic resonance imaging. Magn. Reason. Med. 2021, 86, 1194–1211. [Google Scholar] [CrossRef]
- Dakok, K.K.; Matjafri, M.Z.; Suardi, N.; Oglat, A.A.; Nabasu, S.E. A Review of Carotid Artery Phantoms for Doppler Ultrasound Applications. J. Med. Ultrasound 2021, 29, 157–166. [Google Scholar] [CrossRef] [PubMed]
- IEC 61685:2001; Ultrasonics—Flow Measurement Systems—Flow Test Object. International Electrotechnical Commission: Geneva, Switzerland, 2001. Available online: https://webstore.iec.ch/publication/5721 (accessed on 18 December 2023).
- Wong, E.Y.; Thorne, M.L.; Nikolov, H.N.; Poepping, T.L.; Holdsworth, D.W. Dopper Ultrasound Compatible Plastic Material for Use in Rigid Flow Models. Ultrasound Med. Biol. 2008, 34, 1846–1856. [Google Scholar] [CrossRef] [PubMed]
- Fox, A.J. How to measure carotid stenosis. Radiology 1993, 186, 316–318. [Google Scholar] [CrossRef]
- Galluzo, F.; Ceruti, L.A.; De Marchi, L.; Corsi, C. Design of anthropomorphic atherosclerotic carotid artery flow phantoms for ultrasound images. In Proceedings of the Computing in Cardiology Conference (CinC), Nice, France, 6–9 September 2015. [Google Scholar] [CrossRef]
- Chee, A.J.Y.; Ho, C.K.; Yiu, B.Y.S.; Yu, A.C.H. Walled Carotid Bifurcation Phantoms for Imaging Investigations of Vessel Wall Motion and Blood Flow Dynamics. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2016, 63, 1852–1864. [Google Scholar] [CrossRef] [PubMed]
- Chayer, B.; Hoven, M.v.D.; Cardinal, M.-H.R.; Li, H.; Swillens, A.; Lopata, R.G.P.; Cloutier, G. Atherosclerotic carotid bifurcation phantoms with stenotic soft inclusions for ultrasound flow and vessel wall elastography imaging. Phys. Med. Biol. 2019, 64, 095025. [Google Scholar] [CrossRef]
- King, D.M.; Moran, C.M.; McNamara, J.D.; Fagan, A.J.; Browne, J.E. Development of a vessel-mimicking material for use in anatomically realistic Doppler flow phantoms. Ultrasound Med. Biol. 2011, 37, 813–826. [Google Scholar] [CrossRef]
- Adelnia, H.; Ensandoost, R.; Vasafi, E.I.; Ta, H.T. Freeze/thawed polyvinyl alcohol hydrogels: Present, past and future. Eur. Polym. J. 2022, 164, 110974. [Google Scholar] [CrossRef]
- Dewey, M.; Zimmermann, E.; Deissenrieder, F.; Laule, M.; Dübel, H.-P.; Schlattmann, P.; Knebel, F.; Rutsch, W.; Hamm, B. Noninvasive coronary angiography by 320-row computed tomography with lower radiation exposure and maintained diagnostic accuracy: Comparison of results with cardiac catheterization in a head-to-head pilot investigation. Circulation 2009, 120, 867–875. [Google Scholar] [CrossRef]
- Pohle, K.; Achenbach, S.; MacNeill, B.; Ropers, D.; Ferencik, M.; Moselewski, F.; Hoffmann, U.; Brady, T.J.; Jang, I.-K.; Daniel, W.G. Characterization of noncalcified coronary atherosclerotic plaque by multi-detector row CT: Comparison to IVUS. Atherosclerosis 2007, 190, 174–180. [Google Scholar] [CrossRef]
- Schroeder, S.; Kuettner, A.; Leitritz, M.; Janzen, J.; Kopp, A.F.; Herdeg, C.; Heuschmid, M.; Burgstahler, C.; Baumbach, A.; Wehrmann, M.; et al. Reliability of differentiating human coronary plaque morphology using contrastenhanced multislice spiral computed tomography: A comparison with histology. J. Comput. Assist. Tomogr. 2004, 28, 449–454. [Google Scholar] [CrossRef]
- Leber, A.W.; Knez, A.; Becker, A.; Becker, C.; von Ziegler, F.; Nikolaou, K.; Rist, C.; Reiser, M.; White, C.; Steinbeck, G.; et al. Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques: A comparative study with intracoronary ultrasound. J. Am. Coll. Cardiol. 2004, 43, 1241–1247. [Google Scholar] [CrossRef]
- Toepker, M.; Euller, G.; Unger, E.; Weber, M.; Kienzl, D.; Herold, C.J.; Ringl, H. Stenosis quantification of coronary arteries in coronary vessel phantoms with second-generation dual-source CT: Influence of measurement parameters and limitations. AJR Am. J. Roentgenol. 2013, 201, W227–W234. [Google Scholar] [CrossRef] [PubMed]
- Richards, T.; Sturgeon, G.M.; Segars, W.P.; Samei, E. Quantification of uncertainty in the assessment of coronary plaque in CCTA through a dynamic cardiac phantom and 3D-printed plaque model. J. Med. Imaging 2018, 5, 013501. [Google Scholar] [CrossRef]
- Jin, K.N.; Chung, J.W.; Park, E.-A.; Lee, W. Dual-energy computed tomography angiography: Virtual calcified plaque subtraction in a vascular phantom. Acta Radiol. 2017, 6, 2058460117717765. [Google Scholar] [CrossRef] [PubMed]
- Stepniak, K.; Ursani, A.; Paul, N.; Naguib, H. Novel 3D printing technology for CT phantom coronary arteries with high geometrical accuracy for biomedical imaging applications. Bioprinting 2020, 18, e00074. [Google Scholar] [CrossRef]
- Mørup, S.D.; Stowe, J.; Precht, H.; Gervig, M.H.; Foley, S. Design of a 3D printed coronary artery model for CT optimization. Radiography 2022, 28, 426–432. [Google Scholar] [CrossRef] [PubMed]
- Crasto, N.; Kirubarajan, A.; Sussman, D. Anthropomorphic brain phantoms for use in MRI systems: A systematic review. Magn. Reason. Mater. Phys. Biol. Med. 2022, 35, 277–289. [Google Scholar] [CrossRef] [PubMed]
- Urbina, J.; Sotelo, J.A.; Springmüller, D.; Montalba, C.; Letelier, K.; Tejos, C.; Irarrázaval, P.; Andia, M.E.; Razavi, R.; Valverde, I.; et al. Realistic Aortic Phantom to Study Hemodynamics Using MRI and Cardiac Cathererization in Normal and Aortic Coarctation Conditions. J. Magn. Reason. Imaging 2016, 44, 683–697. [Google Scholar] [CrossRef] [PubMed]
- Chueh, J.; Turan, T.; van der Marel, K.; LeMatty, T.; Brown, T.; Ansari, S.; Carroll, T.; Buck, A.; Zhou, X.; Chatterjee, A.; et al. An atherosclerotic plaque phantom for medical imaging. J. Neurointerv. Surg. 2016, 8, A53–A54. [Google Scholar] [CrossRef]
- Smith, R.F.; Rutt, B.K.; Holdworth, D.W. Anthropomorphic carotid bifurcation phantom for MRI applications. J. Magn. Reson. Imaging 1999, 10, 533–544. [Google Scholar] [CrossRef]
- Lorenz, R.; Benk, C.; Bock, J.; Stalder, A.F.; Korvink, J.G.; Hennig, J.; Markl, M. Closed circuit MR compatible pulsatile pump system using a ventricular assist device and pressure control unit. Magn. Reason. Med. 2012, 67, 258–268. [Google Scholar] [CrossRef]
- Chueh, J.-Y.; van der Marel, K.; Gounis, M.J.; LeMatty, T.; Brown, T.R.; A Ansari, S.; Carroll, T.J.; Buck, A.K.; Zhou, X.J.; Chatterjee, A.R.; et al. Development of a high-resolution MRI intracranial atherosclerosis imaging phantom. J. Neurointerv. Surg. 2018, 10, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Canstein, C.; Cachot, P.; Faust, A.; Stalder, A.; Bock, J.; Frydrychowicz, A.; Küffer, J.; Hennig, J.; Markl, M. 3D MR flow analysis in realistic rapid-prototyping model systems of the thoracic aorta: Comparison with in vivo data and computational fluid dynamics in identical vessel geometries. Magn. Reson. Med. 2008, 59, 535–546. [Google Scholar] [CrossRef]
- Stalder, A.; Russe, M.; Frydrychowicz, A.; Bock, J.; Hennig, J.; Markl, M. Quantitative 2D and 3D phase contrast MRI: Optimized analysis of blood flow and vessel wall parameters. Magn. Reson. Med. 2008, 60, 1218–1231. [Google Scholar] [CrossRef]
- Gadda, G.; Cocozza, S.; Gambaccini, M.; Taibi, A.; Tedeschi, E.; Zamboni, P.; Palma, G. No-HYPE: A novel hydrodynamic phantom for the evaluation of MRI flow measurements. Med. Biol. Eng. Comput. 2021, 59, 1889–1899. [Google Scholar] [CrossRef]
- Wan, B.; Ganier, C.; Du-Harpur, X.; Harun, N.; Watt, F.M.; Patalay, R.; Lynch, M.D. Applications and future directions for optical coherence tomography in dermatology. Br. J. Dermatol. 2021, 184, 1014–1022. [Google Scholar] [CrossRef] [PubMed]
- Viedma, I.A.; Alonso-Caneiro, D.; Read, S.A.; Collins, M.J. Deep learning in retinal optical coherence tomography (OCT): A comprehensive survey. Neurocomputing 2022, 507, 247–264. [Google Scholar] [CrossRef]
- Shah, N.R.; Howlett, P.J.; Fluck, D.S.; Williams, M.; Jacques, A.; Mahmoudi, M. Optical coherence tomography in coronary atherosclerosis. MOJ Anat. Physiol. 2015, 1, 11–14. [Google Scholar] [CrossRef]
- Yamanaka, M.; Hayakawa, N.; Nishizawa, N. High-spatial-resolution deep tissue imaging with spectral-domain optical coherence microscopy in the 1700- nm spectral band. J. Biomed. Opt. 2019, 24, 070502. [Google Scholar] [CrossRef] [PubMed]
- van Soest, G.; Goderie, T.P.M.; Regar, E.; Koljenović, S.; van Leenders, G.L.J.H.; Gonzalo, N.; van Noorden, S.; Okamura, T.; Bouma, B.E.; Tearney, G.J.; et al. Atherosclerotic tissue characterization in vivo by optical coherence tomography attenuation imaging. J. Biomed. Opt. 2010, 15, 011105. [Google Scholar] [CrossRef] [PubMed]
- Xu, C.; Schmitt, J.M.; Carlier, S.G.; Virmani, R. Characterization of atherosclerosis plaques by measuring both backscattering and attenuation coefficients in optical coherence tomography. J. Biomed. Opt. 2008, 13, 034003. [Google Scholar] [CrossRef] [PubMed]
- Little, C.D.; Poduval, R.K.; Caulfield, R.; Noimark, S.; Colchester, R.J.; Loder, C.D.; Tiwari, M.K.; Rakhit, R.D.; Papakonstantinou, I.; Desjardins, A.E. Micron resolution, high-fidelity three-dimensional vascular optical imaging phantoms. J. Biomed. Opt. 2019, 24, 020502. [Google Scholar] [CrossRef]
- Fleming, C.P.; Eckert, J.; Halpern, E.F.; Gardecki, J.A.; Tearney, G.J. Depth resolved detection of lipid using spectroscopic optical coherence tomography. Biomed. Opt. Express 2013, 4, 1269–1284. [Google Scholar] [CrossRef]
- Nam, H.S.; Song, J.W.; Jang, S.-J.; Lee, J.J.; Oh, W.-Y.; Kim, J.W.; Yoo, H. Characterization of lipid-rich plaques using spectroscopic optical coherence tomography. J. Biomed. Opt. 2016, 21, 075004. [Google Scholar] [CrossRef]
- Shang, S.; Chen, Z.; Zhao, Y.; Yang, S.; Xing, D. Simultaneous imaging of atherosclerotic plaque composition and structure with dual-mode photoacoustic and optical coherence tomography. Opt. Express 2017, 25, 530–539. [Google Scholar] [CrossRef]
- Victor, A.; Ribeiro, J.; Araújo, F.S. Study of PDMS characterization and its applications in biomedicine: A review. J. Mech. Eng. Biomech. 2019, 4, 1–9. [Google Scholar] [CrossRef]
- Costa, P.; Albers, H.J.; Linssen, J.E.A.; Middelkamp, H.H.T.; Van Der Hout, L.; Passier, R.; van den Berg, A.; Malda, J.; Van Der Meer, A.D. Mimicking arterial thrombosis in a 3D-printed microfluidic in vitro vascular model based on computed tomography angiography data. Lab Chip 2017, 17, 2785. [Google Scholar] [CrossRef]
- Siddique, A.; Pause, I.; Narayan, S.; Kruse, L.; Satrk, R.W. Endothelization of PDMS-based microfluidic devices under high shear stress conditions. Colloids Surf. B 2021, 197, 111394. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, C.G.M.; Brandt, M.M.; Poulis, N.; Anten, J.; van der Moolen, M.; Kramer, L.; Homburg, E.F.G.A.; Louzao-Martinez, L.; Pei, J.; Krebber, M.M.; et al. A new microfluidic model that allows monitoring of complex vascular structures and cell interactions in a 3D biological matrix. Lab Chip 2020, 20, 1827–1844. [Google Scholar] [CrossRef]
- DiCarlo, A.L.; Holdsworth, D.W.; Poepping, T.L. Study of the effect of stenosis severity and non-Newtonian viscosity on multidirectional wall shear stress and flow disturbances in the carotid artery using particle image velocimetry. Med. Eng. Phys. 2019, 65, 8–23. [Google Scholar] [CrossRef]
- Doutel, E.; Carneiro, J.; Oliveira, M.S.N.; Campos, J.B.L.M.; Miranda, J.M. Fabrication of 3D mili-scale channels for hemodynamics studies. J. Mech. Med. Biol. 2015, 15, 1550004. [Google Scholar] [CrossRef]
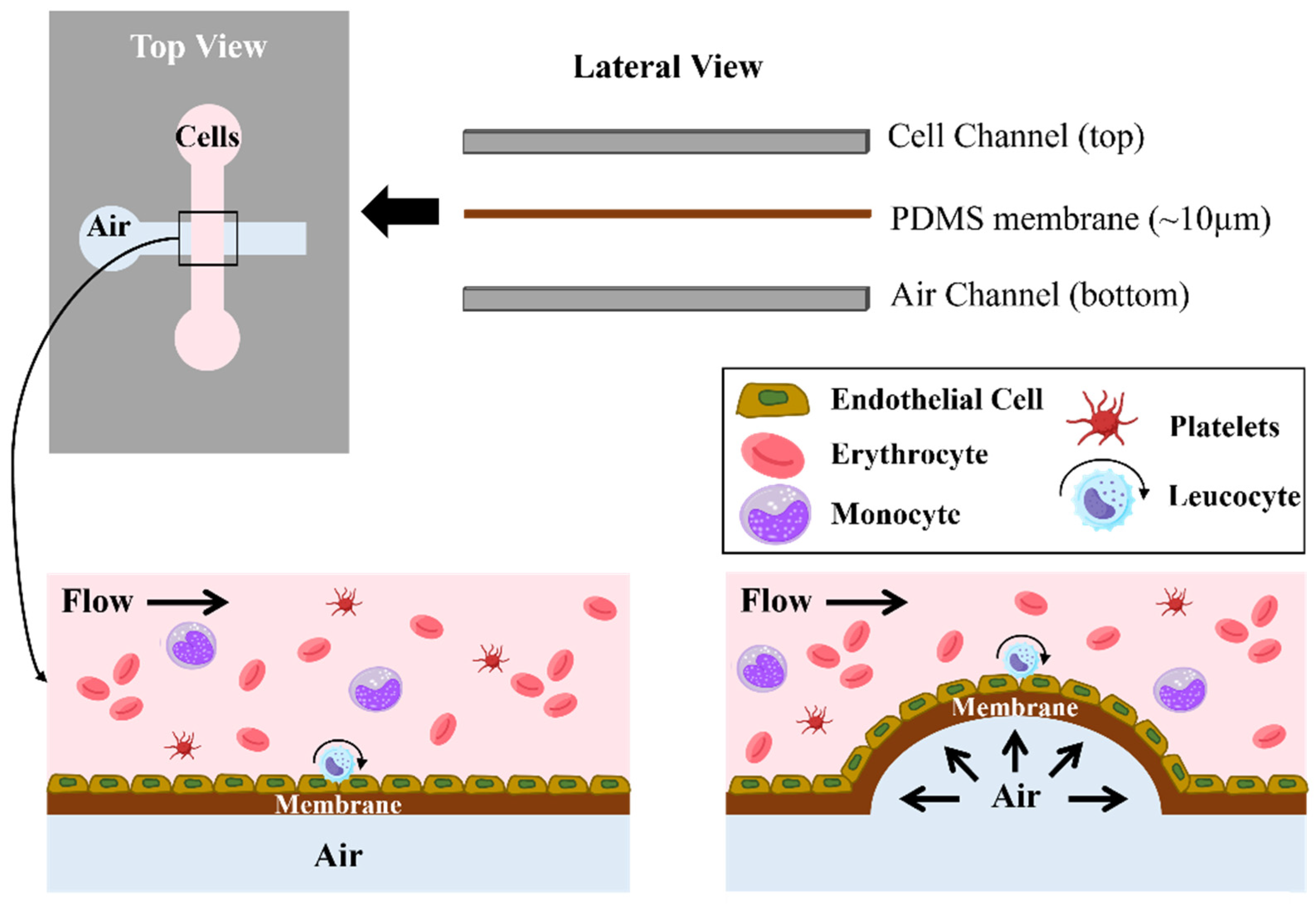
- Menon, N.V.; Tay, H.M.; Pang, K.T.; Dalan, R.; Wong, S.C.; Wang, X.; Li, K.H.H.; Hou, H.W. A tunable microfluidic 3D stenosis model to study leucocyte-endothelial interactions in atherosclerosis. APL Bioeng. 2018, 2, 016103. [Google Scholar] [CrossRef]
- Nilsson, D.P.G.; Holmgren, M.; Holmlund, P.; Wåhlin, A.; Eklund, A.; Dahlberg, T.; Wiklund, K.; Andersson, M. Patient-specific brain arteries molded as a flexible phantom model using 3D printed water-soluble resin. Sci. Rep. 2022, 12, 10172. [Google Scholar] [CrossRef]
- Kefayati, S.; Poepping, T.L. Transitional flow analysis in the carotid artery bifurcation by proper orthogonal decomposition and particle image velocimetry. Med. Eng. Phys. 2013, 35, 898–909. [Google Scholar] [CrossRef] [PubMed]
- Kolli, K.K.; Min, J.K.; Ha, S.; Soohoo, H.; Xiong, G. Effect of Varying Hemodynamic and Vascular Conditions on Fractional Flow Reserve: An in vitro Study. J. Am. Heart Assoc. 2016, 5, e003634. [Google Scholar] [CrossRef] [PubMed]
- Maragiannis, D.; Jackson, M.S.; Igo, S.R.; Schutt, R.C.; Connell, P.; Grande-Allen, J.; Barker, C.M.; Chang, S.M.; Reardon, M.J.; Zoghbi, W.A.; et al. Replicating Patient-Specific Severe Aortic Valve Stenosis with Functional 3D Modeling. Circ. Cardiovasc. Imaging 2015, 8, e003626. [Google Scholar] [CrossRef] [PubMed]
- Lopes, D.; Puga, H.; Teixeira, J.C.; Teixeira, S.F. Influence of arterial mechanical properties on carotid blood flow: Comparison of CFD and FSI. Int. J. Mech. Sci. 2019, 160, 209–218. [Google Scholar] [CrossRef]
- Guarnera, D.; Carrera, E.; Hansen, C.J.; Maiarù, M. Mechanical characterization of 3D printed mimic of human artery affected by atherosclerotic plaque through numerical and experimental methods. Biomech. Model. Mechanobiol. 2021, 20, 1969–1980. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review. Int. J. Environ. Res. Public Health 2022, 19, 3331. [Google Scholar] [CrossRef]
- Agung, N.P.; Nadhif, M.H.; Irdam, G.A.; Mochtar, C.A. The Role of 3D-Printed Phantoms and Devices for Organ-specified Appliances in Urology. Int. J. Bioprint. 2021, 7, 333. [Google Scholar] [CrossRef]
- Coles-Black, J.; Bolton, D.; Chuen, J. Accessing 3D Printed Vascular Phantoms for Procedural Simulation. Front. Surg. 2021, 7, 626212. [Google Scholar] [CrossRef]
- Sun, Z.; Wee, C. 3D Printed Models in Cardiovascular Disease: An Exciting Future to Deliver Personalized Medicine. Micromachines 2022, 13, 1575. [Google Scholar] [CrossRef]
- Gómez-Ciriza, G.; Gómez-Cía, T.; Rivas-González, J.A.; Forte, M.N.V.; Valverde, I. Affordable Three-Dimensional Printed Heart Models. Front. Cardiovasc. Med. 2021, 8, 642011. [Google Scholar] [CrossRef]
- Russo, J.J.; Yuen, T.; Tan, J.; Wilson, A.B.; Gurvitch, R. Assessment of Coronary Artery Obstruction During Transcatheter Aortic Valve Replacement Utilising 3D-Printing. Heart Lung Circ. 2022, 31, 1134–1143. [Google Scholar] [CrossRef] [PubMed]
- Torres, I.O.; Luccia, N.D. A simulator for training in endovascular aneurysm repair: The use of three-dimensional printers. Eur. J. Vasc. Endovasc. Surg. 2017, 54, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Sheu, A.Y.; Laidlaw, G.L.; Fell, J.C.; Triana, B.P.; Goettl, C.S.; Shah, R.P. Custom 3-Dimensional Printed Ultrasound-Compatible Vascular Access Models: Training Medical Students for Vascular Access. J. Vasc. Interv. Radiol. 2019, 30, 922–927. [Google Scholar] [CrossRef] [PubMed]
- Bortman, J.; Mahmood, F.; Schermerhorn, M.; Lo, R.; Swerdlow, N.; Mahmood, F.; Matyal, R. Use of 3-dimensional printing to create patientspecific abdominal aortic aneurysm models for preoperative planning. J. Cardiothorac. Vasc. Anesth. 2019, 33, 1442–1446. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Ng, C.K.C.; Wong, Y.H.; Yeong, C.H. 3D-Printed Coronary Plaques to Simulate High Calcification in the Coronary Arteries for Investigation of Blooming Artifacts. Biomolecules 2021, 11, 1307. [Google Scholar] [CrossRef] [PubMed]
- Oliveira-Santos, M.; Santos, E.O.; Marinho, A.V.; Leite, L.; Guardado, J.; Matos, V.; Pego, G.M.; Marques, J.S. Patient-specific 3D printing simulation to guide complex coronary intervention. Rev. Port. Cardiol. 2018, 37, 541.e1–541.e5. [Google Scholar] [CrossRef] [PubMed]
- Vukicevic, M.; Mosadegh, B.; Min, J.K.; Little, S.H. Cardiac 3D Printing and Its Future Directions. JACC Cardiovasc. Imaging 2017, 10, 171–184. [Google Scholar] [CrossRef] [PubMed]
- Kiraly, L.; Shah, N.C.; Abdullah, O.; Al-Ketan, O.; Rowshan, R. Three-Dimensional Virtual and Printed Prototypes in Complex Congenital and Pediatric Cardiac Surgery—A Multidisciplinary Team-Learning Experience. Biomolecules 2021, 11, 1703. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, R.M.; Jolley, M.A.; Mascio, C.E.; Chen, J.M.; Fuller, S.; Rome, J.J.; Silvestro, E.; Whitehead, K.K. Clinical 3D modelling to guide paediatric cardiothoracic surgery and intervention using 3D printed anatomic models, computer aided design and virtual reality. 3D Print. Med. 2022, 8, 11. [Google Scholar] [CrossRef] [PubMed]
- Goitein, O.; Fink, N.; Guettar, V.; Beinart, R.; Brodov, Y.; Konen, E.; Goitein, D.; Segni, E.D.; Grupper, A.; Glikson, M. Printed MDCT 3D models for prediction of left atrial appendage (LAA) occlude device size: A feasibility study. EuroIntervention 2017, 13, e1076–e1079. [Google Scholar] [CrossRef]
- Goudie, C.; Kinnin, J.; Bartellas, M.; Gullipalli, R.; Dubrowski, A. The use of 3D printed vasculature for simulation-based medical education within interventional radiology. Cureus 2019, 11, e4381. [Google Scholar] [CrossRef]
- Sotiriou, M.; Yiannakou, M.; Damianou, C. Investigating atherosclerotic plaque phantoms for ultrasound therapy. J. Ultrasound 2022, 25, 709–720. [Google Scholar] [CrossRef]
- Gholampour, S.; Hajirayat, K. Minimizing thermal damage to vascular nerves while drilling of calcified plaque. BMC Res. Notes 2019, 12, 338. [Google Scholar] [CrossRef]

| Lesion Type | Nomenclature | Lesion Characteristics–Main Histology Properties |
|---|---|---|
| Type I | Early lesion | Initial lesion with foam cells |
| Type II | Fatty streak | Fatty streak with multiple foam cell layers |
| Type III | Pre-atheroma | Pre-atheroma with extracellular lipid pools |
| Type IV | Atheroma | Atheroma with a confluent extracellular lipid core |
| Type V | Fibro-atheroma | Fibrotic and calcified layers with lipid cores |
| Type VI | Rupture lesion | Complex plaque with possible surface defect |
| Type VII | Calcified lesion | Calcified plaque |
| Type VIII | Fibrotic lesion | Fibrotic plaque without lipid core |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Henriques, J.; Amaro, A.M.; Piedade, A.P. Biomimicking Atherosclerotic Vessels: A Relevant and (Yet) Sub-Explored Topic. Biomimetics 2024, 9, 135. https://doi.org/10.3390/biomimetics9030135
Henriques J, Amaro AM, Piedade AP. Biomimicking Atherosclerotic Vessels: A Relevant and (Yet) Sub-Explored Topic. Biomimetics. 2024; 9(3):135. https://doi.org/10.3390/biomimetics9030135
Chicago/Turabian StyleHenriques, Joana, Ana M. Amaro, and Ana P. Piedade. 2024. "Biomimicking Atherosclerotic Vessels: A Relevant and (Yet) Sub-Explored Topic" Biomimetics 9, no. 3: 135. https://doi.org/10.3390/biomimetics9030135
APA StyleHenriques, J., Amaro, A. M., & Piedade, A. P. (2024). Biomimicking Atherosclerotic Vessels: A Relevant and (Yet) Sub-Explored Topic. Biomimetics, 9(3), 135. https://doi.org/10.3390/biomimetics9030135








