Inconsistent Provider Testing Practices for Congenital Cytomegalovirus: Missed Diagnoses and Missed Opportunities
Abstract
:1. Introduction
2. Methods
2.1. Study Overview
2.2. Cohort Creation
2.3. Data Collection
2.4. Statistical Analysis
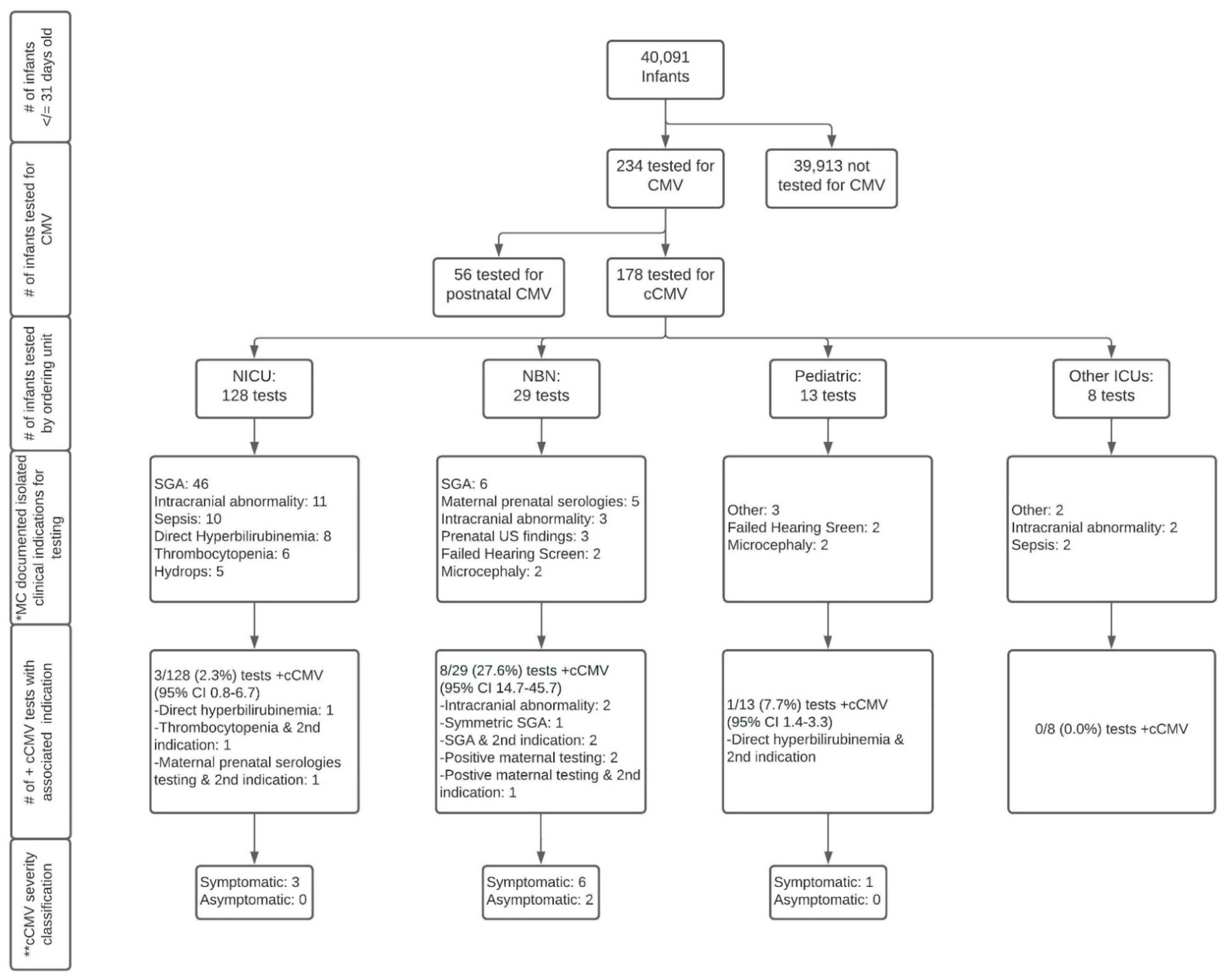
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fowler, K.B.; Ross, S.A.; Shimamura, M.; Ahmed, A.; Palmer, A.L.; Michaels, M.G.; Bernstein, D.I.; Sánchez, P.J.; Feja, K.N.; Stewart, A. Racial and ethnic differences in the prevalence of congenital cytomegalovirus infection. J. Pediatr. 2018, 200, 196–201.e191. [Google Scholar] [CrossRef] [PubMed]
- Dollard, S.C.; Dreon, M.; Hernandez-Alvarado, N.; Amin, M.M.; Wong, P.; Lanzieri, T.M.; Osterholm, E.A.; Sidebottom, A.; Rosendahl, S.; McCann, M.T. Sensitivity of Dried Blood Spot Testing for Detection of Congenital Cytomegalovirus Infection. JAMA Pediatr. 2021, 3, e205441. [Google Scholar] [CrossRef] [PubMed]
- Rawlinson, W.D.; Boppana, S.B.; Fowler, K.B.; Kimberlin, D.W.; Lazzarotto, T.; Alain, S.; Daly, K.; Doutré, S.; Gibson, L.; Giles, M.L. Congenital cytomegalovirus infection in pregnancy and the neonate: Consensus recommendations for prevention, diagnosis, and therapy. Lancet Infect. Dis. 2017, 17, e177–e188. [Google Scholar] [CrossRef]
- Pesch, M.H.; Kuboushek, K.; Weinberg, J.B.; McKee, M.; Thorne, M. Congenital cytomegalovirus infection. BMJ 2021, 373, n1212. [Google Scholar] [CrossRef]
- Ronchi, A.; Zeray, F.; Lee, L.E.; Owen, K.E.; Shoup, A.G.; Garcia, F.; Vazquez, L.N.; Cantey, J.B.; Varghese, S.; Pugni, L. Evaluation of clinically asymptomatic high risk infants with congenital cytomegalovirus infection. J. Perinatol. 2020, 40, 89–96. [Google Scholar] [CrossRef]
- Sorichetti, B.; Goshen, O.; Pauwels, J.; Kozak, F.K.; Tilley, P.; Krajden, M.; Gantt, S. Symptomatic congenital cytomegalovirus infection is underdiagnosed in British Columbia. J. Pediatr. 2016, 169, 316–317. [Google Scholar] [CrossRef]
- Lopez, A.S.; Ortega-Sanchez, I.R.; Bialek, S.R. Congenital cytomegalovirus-related hospitalizations in infants <1 year of age, United States, 1997–2009. Pediatric Infect. Dis. J. 2014, 33, 1119–1123. [Google Scholar] [CrossRef] [Green Version]
- Luck, S.E.; Wieringa, J.W.; Blázquez-Gamero, D.; Henneke, P.; Schuster, K.; Butler, K.; Capretti, M.G.; Cilleruelo, M.J.; Curtis, N.; Garofoli, F. Congenital cytomegalovirus: A European expert consensus statement on diagnosis and management. Pediatr. Infect. Dis. J. 2017, 36, 1205–1213. [Google Scholar] [CrossRef]
- Kimberlin, D.W.; Jester, P.M.; Sánchez, P.J.; Ahmed, A.; Arav-Boger, R.; Michaels, M.G.; Ashouri, N.; Englund, J.A.; Estrada, B.; Jacobs, R.F.; et al. Valganciclovir for symptomatic congenital cytomegalovirus disease. N. Engl. J. Med. 2015, 372, 933–943. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yassine, B.B.; Hulkower, R.; Dollard, S.; Cahill, E.; Lanzieri, T. A legal mapping assessment of cytomegalovirus-related laws in the United States. J. Public Health Manag. Pract. 2022, 28, E624–E629. [Google Scholar] [CrossRef] [PubMed]
- The University of Michigan Health System. DataDirect. Available online: https://datadirect.med.umich.edu/ (accessed on 1 September 2020).
- De Onis, M. World Health Organization Reference Curves. In ECOG’s eBook on Child and Adolescent Obesity; 2015; pp. 1–19. Available online: http://ebook.ecog-obesity.eu/wp-content/uploads/2014/10/ECOG-Obesity-eBook-World-Health-Organization-Reference-Curves-V1.pdf (accessed on 1 September 2020).
- Fenton, T.R.; Kim, J.H. A systematic review and meta-analysis to revise the Fenton growth chart for preterm infants. BMC Pediatr 2013, 13, 59. [Google Scholar] [CrossRef] [Green Version]
- Leung, J.; Dollard, S.C.; Grosse, S.D.; Chung, W.; Do, T.; Patel, M.; Lanzieri, T.M. Valganciclovir use among commercially and Medicaid-insured infants with congenital CMV infection in the United States, 2009–2015. Clin. Ther. 2018, 40, 430–439.e431. [Google Scholar] [CrossRef] [Green Version]
- Leung, J.; Grosse, S.D.; Hong, K.; Pesch, M.H.; Lanzieri, T.M. Changes in Valganciclovir Use Among Infants with Congenital Cytomegalovirus Diagnosis in the United States, 2009–2015 and 2016–2019. J. Pediatr. 2022, 246, 274–278.e2. [Google Scholar] [CrossRef] [PubMed]
- Kee, V.R.; Gilchrist, B.; Granner, M.A.; Sarrazin, N.R.; Carnahan, R.M. A systematic review of validated methods for identifying seizures, convulsions, or epilepsy using administrative and claims data. Pharmacoepidemiol. Drug Saf. 2012, 21, 183–193. [Google Scholar] [CrossRef]
- Swanson, N. Prepare for New ICD-10-CM and CPT Codes in 2022. Leader Live, 4 October 2021. [Google Scholar]
- Creel, L.; Van Horn, A.; Hines, A.; Bush, M.L. Neonatal Abstinence Syndrome and Infant Hearing Assessment: A Kids’ Inpatient Database Review. J. Early Heart Detect. Interv. 2020, 5, 20–27. [Google Scholar]
- Greenwald, R.; Stackowiak, R.; Stern, J. Oracle Essentials: Oracle Database 12c; O’Reilly Media, Inc.: Newton, MA, USA, 2013. [Google Scholar]
- Agresti, A.; Coull, B.A. Approximate is better than “exact” for interval estimation of binomial proportions. Am. Stat. 1998, 52, 119–126. [Google Scholar]
- World Health Organization. International Classification of Diseases: [9th] Ninth Revision, Basic Tabulation List with Alphabetic Index; World Health Organization: Geneva, Switzerland, 1978. [Google Scholar]
- World Health Organization. ICD-10: International Statistical Classification of Diseases and Related Health Problems: Tenth Revision, 2nd ed.; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Istas, A.S.; Demmler, G.J.; Dobbins, J.G.; Stewart, J.A. Surveillance for congenital cytomegalovirus disease: A report from the National Congenital Cytomegalovirus Disease Registry. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 1995, 20, 665–670. [Google Scholar] [CrossRef]
- Townsend, C.L.; Peckham, C.S.; Tookey, P.A. Surveillance of congenital cytomegalovirus in the UK and Ireland. Arch. Dis. Childhood. Fetal Neonatal Ed. 2011, 96, F398–F403. [Google Scholar] [CrossRef] [Green Version]
- Vaudry, W.; Lee, B.E.; Rosychuk, R.J. Congenital cytomegalovirus infection in Canada: Active surveillance for cases diagnosed by paediatricians. Paediatr. Child Health 2014, 19, e1–e5. [Google Scholar]
- Dedhia, K.; Fifer, R.C.; Muldoon, K.M.; Park, A. A Cross-Sectional Survey Evaluating Awareness of Congenital Cytomegalovirus Among Audiologists and Speech-Language Pathologists. Am. J. Audiol. 2021, 30, 145–159. [Google Scholar] [CrossRef] [PubMed]
- Fellah, T.; Sibiude, J.; Vauloup-Fellous, C.; Cordier, A.; Guitton, S.; Grangeot-Keros, L.; Benachi, A.; Mandelbrot, L.; Picone, O. Evolution of awareness and knowledge of congenital cytomegalovirus infection among health care providers in France between 2011 and 2018. J. Clin. Virol. 2020, 129, 104335. [Google Scholar] [CrossRef] [PubMed]
- Pesch, M.H.; Muldoon, K.M. Congenital Cytomegalovirus Knowledge, Practices, and Beliefs Among Primary Care Physicians and Newborn Hospitalists. J. Prim. Care Community Health 2022, 13, 21501319221106880. [Google Scholar] [CrossRef] [PubMed]
- Smiljkovic, M.; Le Meur, J.B.; Malette, B.; Boucoiran, I.; Minsart, A.F.; Lamarre, V.; Tapiero, B.; Renaud, C.; Kakkar, F. Blood viral load in the diagnostic workup of congenital cytomegalovirus infection. J. Clin. Virol. 2020, 122, 104231. [Google Scholar] [CrossRef] [PubMed]
- Dreher, A.M.; Arora, N.; Fowler, K.B.; Novak, Z.; Britt, W.J.; Boppana, S.B.; Ross, S.A. Spectrum of disease and outcome in children with symptomatic congenital cytomegalovirus infection. J. Pediatr. 2014, 164, 855–859. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blázquez-Gamero, D.; Soriano-Ramos, M.; Vicente, M.; Pallás-Alonso, C.R.; Pérez-Rivilla, A.; García-Álvarez, M.; Pinilla Martín, M.T.; Freire, X.; De Vergas, J.; De Aragón, A.M. Prevalence and clinical manifestations of congenital cytomegalovirus infection in a screening program in Madrid (PICCSA Study). Pediatr. Infect. Dis. J. 2020, 39, 1050–1056. [Google Scholar] [CrossRef]
- Leung, J.; Kennedy, J.L.; Haberling, D.L.; Apostolou, A.; Lanzieri, T.M. Congenital CMV-coded diagnosis among American Indian and Alaska Native infants in the United States, 2000–2017. J. Immigr. Minority Health 2020, 22, 1101–1104. [Google Scholar] [CrossRef]
- Grosse, S.D.; Leung, J.; Lanzieri, T.M. Identification of congenital CMV cases in administrative databases and implications for monitoring prevalence, healthcare utilization, and costs. Curr. Med. Res. Opin. 2021, 37, 769–779. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. Practice bulletin no. 151: Cytomegalovirus, parvovirus B19, varicella zoster, and toxoplasmosis in pregnancy. Obstet. Gynecol. 2015, 125, 1510–1525. [Google Scholar]
- Kilby, M.D.; Ville, Y.; Acharya, G. Screening for cytomegalovirus infection in pregnancy. BMJ 2019, 367, I6507. [Google Scholar] [CrossRef] [PubMed]
- Leruez-Ville, M.; Magny, J.-F.; Couderc, S.; Pichon, C.; Parodi, M.; Bussières, L.; Guilleminot, T.; Ghout, I.; Ville, Y. Risk Factors for Congenital Cytomegalovirus Infection Following Primary and Nonprimary Maternal InfectionA Prospective Neonatal Screening Study Using Polymerase Chain Reaction in Saliva. Clin. Infect. Dis. 2017, 65, 398–404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Torii, Y.; Yoshida, S.; Yanase, Y.; Mitsui, T.; Horiba, K.; Okumura, T.; Takeuchi, S.; Suzuki, T.; Kawada, J.I.; Kotani, T.; et al. Serological screening of immunoglobulin M and immunoglobulin G during pregnancy for predicting congenital cytomegalovirus infection. BMC Pregnancy Childbirth 2019, 19, 205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shimada, K.; Toriyabe, K.; Kitamura, A.; Morikawa, F.; Ikejiri, M.; Minematsu, T.; Nakamura, H.; Suga, S.; Ikeda, T. Characteristics and serology of pregnant women with cytomegalovirus immunoglobulin G seroconversion during pregnancy in Japan. Taiwan. J. Obstet. Gynecol. 2021, 60, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Hui, L.; Shand, A. Is it time to adopt routine cytomegalovirus screening in pregnancy? No! Am. J. Obstet. Gynecol. MFM 2021, 3, 100355. [Google Scholar] [CrossRef]
- Ssentongo, P.; Hehnly, C.; Birungi, P.; Roach, M.A.; Spady, J.; Fronterre, C.; Wang, M.; Murray-Kolb, L.E.; Al-Shaar, L.; Chinchilli, V.M. Congenital Cytomegalovirus Infection Burden and Epidemiologic Risk Factors in Countries With Universal Screening: A Systematic Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2120736. [Google Scholar] [CrossRef]
- Joint Committee on Infant Hearing. Year 2019 Position Statement: Principles and Guidelines for Early Hearing Detection and Intervention Programs. J. Early Hear. Detect. Interv. 2019, 4, 1–44. [Google Scholar]
- Bartlett, A.W.; Hall, B.M.; Palasanthiran, P.; McMullan, B.; Shand, A.W.; Rawlinson, W.D. Recognition, treatment, and sequelae of congenital cytomegalovirus in Australia: An observational study. J. Clin. Virol. 2018, 108, 121–125. [Google Scholar] [CrossRef]
- Pinninti, S.; Christy, J.; Almutairi, A.; Cochrane, G.; Fowler, K.B.; Boppana, S. Vestibular, gaze, and balance disorders in asymptomatic congenital cytomegalovirus infection. Pediatrics 2021, 147, e20193945. [Google Scholar] [CrossRef]
- Letamendia-Richard, E.; Périllaud-Dubois, C.; de La Guillonnière, L.; Thouard, I.; Cordier, A.G.; Roque-Afonso, A.M.; de Luca, D.; Benachi, A.; Vauloup-Fellous, C. Universal newborn screening for congenital cytomegalovirus infection: Feasibility and relevance in a French type-III maternity cohort. BJOG Int. J. Obstet. Gynaecol. 2022, 129, 291–299. [Google Scholar] [CrossRef]
- Diener, M.L.; Zick, C.D.; McVicar, S.B.; Boettger, J.; Park, A.H. Outcomes From a Hearing-Targeted Cytomegalovirus Screening Program. Pediatrics 2017, 139, e20160789. [Google Scholar] [CrossRef] [Green Version]
- Vandrevala, T.; Barber, V.; Mbire-Chigumba, E.; Calvert, A.; Star, C.; Khalil, A.; Griffiths, P.; Book, A.S.; Book, G.M.; Heath, P. Parenting a child with congenital cytomegalovirus infection: A qualitative study. BMJ Paediatr. Open 2020, 4, e000844. [Google Scholar] [CrossRef]
- Diener, M.L.; Shi, K.; Park, A.H. A cross-sectional study of caregiver perceptions of congenital cytomegalovirus infection: Knowledge and attitudes about screening. J. Pediatr. 2020, 218, 151–156.e152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cannon, M.J.; Levis, D.M.; McBride, H.; Watson, D.; Rheaume, C.; Hall, M.A.K.; Lanzieri, T.M.; Demmler-Harrison, G. Family Perceptions of Newborn Cytomegalovirus Screening: A Qualitative Study. Int. J. Neonatal Screen. 2021, 7, 80. [Google Scholar] [CrossRef]
- Tastad, K.J.; Schleiss, M.R.; Lammert, S.M.; Basta, N.E. Awareness of congenital cytomegalovirus and acceptance of maternal and newborn screening. PLoS ONE 2019, 14, e0221725. [Google Scholar] [CrossRef]
- Cushing, S.L.; Purcell, P.L.; Papaiaonnou, V.; Neghandi, J.; Daien, M.; Blaser, S.I.; Ertl-Wagner, B.; Wagner, M.; Sheng, M.; James, A.L. Hearing Instability in Children with Congenital Cytomegalovirus: Evidence and Neural Consequences. Laryngoscope 2022, 132 (Suppl. S11), S1–S24. [Google Scholar] [CrossRef] [PubMed]
- Grosse, S.D.; Dollard, S.C.; Ortega-Sanchez, I.R. Economic assessments of the burden of congenital cytomegalovirus infection and the cost-effectiveness of prevention strategies. Semin. Perinatol. 2021, 45, 151393. [Google Scholar] [CrossRef] [PubMed]
- Dhondt, C.; Maes, L.; Oostra, A.; Dhooge, I. Episodic Vestibular Symptoms in Children With a Congenital Cytomegalovirus Infection: A Case Series. Otol. Neurotol. 2019, 40, e636–e642. [Google Scholar] [CrossRef]
- Laccourreye, L.; Ettienne, V.; Prang, I.; Couloigner, V.; Garabedian, E.N.; Loundon, N. Speech perception, production and intelligibility in French-speaking children with profound hearing loss and early cochlear implantation after congenital cytomegalovirus infection. Eur. Ann. Otorhinolaryngol. Head Neck Dis. 2015, 132, 317–320. [Google Scholar] [CrossRef] [Green Version]
- Turriziani Colonna, A.; Buonsenso, D.; Pata, D.; Salerno, G.; Chieffo, D.P.; Romeo, D.M.; Faccia, V.; Conti, G.; Molle, F.; Baldascino, A. Long-Term Clinical, Audiological, Visual, Neurocognitive and Behavioral Outcome in Children with Symptomatic and Asymptomatic Congenital Cytomegalovirus Infection Treated With Valganciclovir. Front. Med. 2020, 7, 268. [Google Scholar] [CrossRef]
- Pasternak, Y.; Ziv, L.; Attias, J.; Amir, J.; Bilavsky, E. Valganciclovir is beneficial in children with congenital cytomegalovirus and isolated hearing loss. J. Pediatr. 2018, 199, 166–170. [Google Scholar] [CrossRef]


| (a) Sociodemographic Characteristics | ||||
|---|---|---|---|---|
| Not Tested for cCMV n = 39,913 | Tested for cCMV n = 178 | cCMV Negative n = 166 | cCMV Positive n = 12 | |
| Maternal age (years); mean (SD) | 30.2 (5.4) a* | 29.8 (5.7) a | 29.9 (0.9) a | 27.0 (8.0) a |
| Maternal parity; median (SD) | 1.1 (0.3) a* | 2 (0.3) a | 1(0.3) a | 2 (0.8) b |
| Male sex; n (%) | 20,821 (51.9) a | 97 (54.5) a | 91 (54.8) a | 6 (50.0) a |
| Infant race; n (%) | ||||
| African American | 4,794 (12.0) a | 22 (12.4) a | 21 (12.7) a | 1(8.3) a |
| Asian | 2,444 (6.1) a | 7 (3.0) a | 7 (4.2) a | 0 (0.0) a |
| Caucasian | 25,621 (64.2) a | 119 (66.9) a | 109 (65.6) a | 10 (83.3) a |
| Other (e.g., Native American, Pacific Islander, Native Alaskan) | 1955 (5.0) a | 15 (8.4) b | 13 (7.8) ab | 1 (8.3) ab |
| Unknown | 5,099 (12.8) a | 7 (3.0) b | 8 (4.8) b | 0 (0.0) ab |
| Hispanic ethnicity (vs. non-Hispanic or unknown); n (%) | 2124 (5.3) a | 8 (4.5) a | 8 (4.8) a | 0 (0.0) a |
| Public insurance (vs. other); n (%) | 15,672 (39.1) a | 96 (53.9) bc | 90 (54.2) bc | 6 (50.0) ac |
| (b) Clinical Characteristics | ||||
| Not Tested for cCMV n = 39,913 | Tested for cCMV n = 178 | cCMV Negative n = 166 | cCMV Positive n = 12 | |
| Birth characteristics | ||||
| Inborn delivery (vs. born at outside hospital); n (%) | 31,402 (78.7) a | 120 (67.4) b | 111 (66.8) b | 9 (75.0) ab |
| Premature < 370/7 weeks; n (%) | 4581 (14.6) *a | 62 (34.8) b | 62 (37.3) b | 1 (8.3) a |
| Gestational age (weeksdays); mean (SD) | 385/7 (10/7) *a | 373/7 (31/7) b | 361/7 (40/7) c | 376/7 (12/7) bc |
| Birth weight (grams); mean (SD) | 3652.8 (277.2) *a | 2472.5 (936.1) b | 2471.2 (949.9) b | 2664.0 (601.5) b |
| Birth weight %ile for GA; mean (SD) | 52.0 (31.1) *a | 22.5 (32.6) b | 31.5 (33.0) c | 17.0 (19.2) b |
| Head circumference (cm); mean (SD) | 34.2 (3.7) *a | 32.8 (3.0) b | 32.8 (0.3) b | 32.6 (1.8) b |
| Head circumference %ile for GA; mean (SD) | 37.4 (30.0) *a | 33.0 (32.6) ab | 31.5 (37.8) b | 18.7 (16.6) b |
| Clinical findings/diagnoses in medical record (vs. absent); n (%) | ||||
| Chorioretinitis | 2 (<0.0) a | 0 (0.0) a | 0 (0.0) a | 0 (0.0) a |
| Direct hyperbilirubinemia (>3 mg/dL) | 246 (0.6) a | 26 (14.6) b | 23 (13.9) b | 3 (25.0) b |
| Elevated ALT (>100 IU/L) | 547 (1.4) a | 30 (16.9) b | 27 (16.3) b | 3 (25.0) b |
| Elevated AST (>80 IU/L) | 1,174 (2.9) a | 56 (31.5) b | 48 (28.9) b | 8 (66.7) b |
| Hepatomegaly | 74 (0.2) a | 24 (13.5) c | 19 (11.4) b | 5 (41.7) b |
| Intracranial abnormalities | 783 (2.0) a | 50 (28.1) b | 41 (24.7) b | 9 (75.0) c |
| Jaundice | 12,483 (31.1) a | 93 (52.2) b | 86 (52.0) b | 7 (58.3) b |
| Microcephaly | 301 (0.8) a | 80 (44.9) b | 73 (44.0) c | 7 (58.3) b |
| Petechiae | 32 (<0.0) a | 20 (12.4) b | 15 (9.0) b | 5 (41.7) c |
| Referred/failed hearing screen | 2,944 (7.3) a | 30 (16.8) b | 25 (15.1) b | 5 (41.7) c |
| Seizures | 825 (2.1) a | 15 (8.4) b | 14 (8.4) b | 1 (8.3) b |
| Small-for-gestational age | 2,317 (5.8) a | 83 (46.6) bd | 79 (47.6) d | 4 (33.3) cd |
| Splenomegaly | 34 (<0.0) a | 11 (6.2) b | 7 (2.4) b | 4 (33.3) c |
| Thrombocytopenia (<150 K/uL) | 430 (1.1) a | 82 (46.1) b | 76 (45.7) b | 6 (50.0) b |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilson, K.L.; Shah, K.; Pesch, M.H. Inconsistent Provider Testing Practices for Congenital Cytomegalovirus: Missed Diagnoses and Missed Opportunities. Int. J. Neonatal Screen. 2022, 8, 60. https://doi.org/10.3390/ijns8040060
Wilson KL, Shah K, Pesch MH. Inconsistent Provider Testing Practices for Congenital Cytomegalovirus: Missed Diagnoses and Missed Opportunities. International Journal of Neonatal Screening. 2022; 8(4):60. https://doi.org/10.3390/ijns8040060
Chicago/Turabian StyleWilson, Kate L., Kimi Shah, and Megan H. Pesch. 2022. "Inconsistent Provider Testing Practices for Congenital Cytomegalovirus: Missed Diagnoses and Missed Opportunities" International Journal of Neonatal Screening 8, no. 4: 60. https://doi.org/10.3390/ijns8040060
APA StyleWilson, K. L., Shah, K., & Pesch, M. H. (2022). Inconsistent Provider Testing Practices for Congenital Cytomegalovirus: Missed Diagnoses and Missed Opportunities. International Journal of Neonatal Screening, 8(4), 60. https://doi.org/10.3390/ijns8040060





