Kinematic Assessment of Fine Motor Skills in Children: Comparison of a Kinematic Approach and a Standardized Test
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
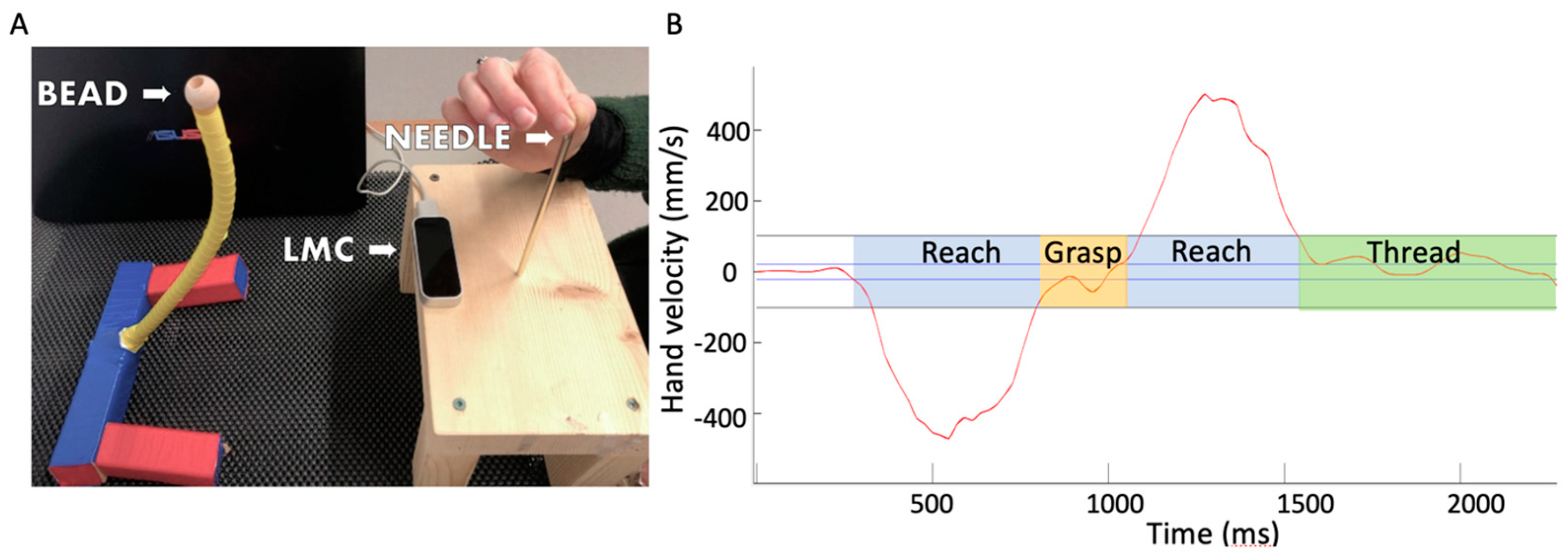
2.2. Procedure
2.3. Analyses
3. Results
3.1. Typically Developing Children
3.2. Clinical Application—Case Study
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grant, S.; Suttle, C.; Melmoth, D.R.; Conway, M.L.; Sloper, J.J. Age- and stereovision-dependent eye-hand coordination deficits in children with amblyopia and abnormal binocularity. Investig. Ophthalmol. Vis. Sci. 2014, 55, 5687–5715. [Google Scholar] [CrossRef]
- Suttle, C.M.; Melmoth, D.R.; Finlay, A.L.; Sloper, J.J.; Grant, S. Eye-hand coordination skills in children with and without amblyopia. Investig. Ophthalmol. Vis. Sci. 2011, 52, 1851–1864. [Google Scholar] [CrossRef] [PubMed]
- Zipori, A.B.; Colpa, L.; Wong, A.M.; Cushing, S.L.; Gordon, K.A. Postural stability and visual impairment: Assessing balance in children with strabismus and amblyopia. PLoS ONE 2018, 13, e0205857. [Google Scholar] [CrossRef] [PubMed]
- Birch, E.E.; Kelly, K.R. Amblyopia and slow reading. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2017, 21, 442–444. [Google Scholar] [CrossRef] [PubMed]
- Kelly, K.R.; Jost, R.M.; De La Cruz, A.; Birch, E.E. Amblyopic children read more slowly than controls under natural, binocular reading conditions. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2015, 19, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Kelly, K.R.; Jost, R.M.; De La Cruz, A.; Birch, E.E. Multiple-choice answer form completion time in children with amblyopia and strabismus. JAMA Ophthalmol. 2018, 136, 938–941. [Google Scholar] [CrossRef] [PubMed]
- Kelly, K.R.; Jost, R.M.; Wang, Y.Z.; Dao, L.; Beauchamp, C.L.; Leffler, J.N.; Birch, E.E. Improved binocular outcomes following binocular treatment for childhood amblyopia. Investig. Ophthalmol. Vis. Sci. 2018, 59, 1221–1228. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.E.; Sugden, D.; Barnett, A.L. Movement Assessment Battery for Children-2: Examiner’s Manual, 2nd ed.; Pearson Assessment: Toronto, ON, Canada, 2007. [Google Scholar]
- Crosetto Deitz, J.; Kartin, D.; Kopp, K. Review of the Bruininks-Oseretsky Test of Motor Proficiency, second edition (BOT-2). Phys. Occup. Ther. Pediatr. 2007, 27, 87–102. [Google Scholar] [CrossRef]
- Venetsanou, F.; Kambas, A.; Ellinoudis, T.; Fatouros, I.; Giannakidou, D.; Kourtessis, T. Can the movement assessment battery for children-test be the “gold standard” for the motor assessment of children with Developmental Coordination Disorder? Res. Dev. Disabil. 2011, 32, 1–10. [Google Scholar] [CrossRef]
- Van Waelvelde, H.; De Weerdt, W.; De Cock, P.; Smits-Engelsman, B.C. Aspects of the validity of the Movement Assessment Battery for Children. Hum. Mov. Sci. 2004, 23, 49–60. [Google Scholar] [CrossRef]
- Niechwiej-Szwedo, E.; Nouredanesh, M.; Tung, J. Test-retest repeatability reveals a temporal kinematic signature for an upper limb precision grasping task in adults. Hum. Mov. Sci. 2021, 75, 102721. [Google Scholar] [CrossRef] [PubMed]
- Niechwiej-Szwedo, E.; Meier, K.; Christian, L.; Nouredanesh, M.; Tung, J.; Bryden, P.; Giaschi, D. Concurrent maturation of visuomotor skills and motion perception in typically-developing children and adolescents. Dev. Psychobiol. 2020, 62, 353–367. [Google Scholar] [CrossRef] [PubMed]
- Niechwiej-Szwedo, E.; Colpa, L.; Wong, A.M.F. Visuomotor behaviour in amblyopia: Deficits and compensatory adaptations. Neural Plast. 2019, 2019, 6817839. [Google Scholar] [CrossRef] [PubMed]
- Niechwiej-Szwedo, E.; Gonzalez, D.; Nouredanesh, M.; Tung, J. Evaluation of the leap motion controller during the performance of visually-guided upper limb movements. PLoS ONE 2018, 13, e0193639. [Google Scholar] [CrossRef] [PubMed]
- Gaul, D.; Issartel, J. Fine motor skill proficiency in typically developing children: On or off the maturation track? Hum. Mov. Sci. 2016, 46, 78–85. [Google Scholar] [CrossRef] [PubMed]
- Cools, W.; Martelaer, K.D.; Samaey, C.; Andries, C. Movement skill assessment of typically developing preschool children: A review of seven movement skill assessment tools. J. Sports Sci. Med. 2009, 8, 154–168. [Google Scholar] [PubMed]
- Cancer, A.; Minoliti, R.; Crepaldi, M.; Antonietti, A. Identifying developmental motor difficulties: A review of tests to assess motor coordination in children. J. Funct. Morphol. Kinesiol. 2020, 5, 16. [Google Scholar] [CrossRef]
- van der Veer, G.; Kamphorst, E.; Minnaert, A.; Cantell, M.; Kakebeeke, T.H.; Houwen, S. Assessing motor performance in preschool children: The Zurich Neuromotor Assessment-2 and the Movement Assessment Battery for Children-2. Percept. Mot. Ski. 2021, 128, 2014–2032. [Google Scholar] [CrossRef]
- Alramis, F.; Roy, E.; Christian, L.; Niechwiej-Szwedo, E. Contribution of binocular vision to the performance of complex manipulation tasks in 5–13 years old visually-normal children. Hum. Mov. Sci. 2016, 46, 52–62. [Google Scholar] [CrossRef]
- Niechwiej-Szwedo, E.; Thai, G.; Christian, L. Contribution of streoposis, vergence, and accommodative function to the performance of a precision grasping and placement task in typically developing children age 8-14 years. Hum. Mov. Sci. 2020, 72, 102652. [Google Scholar] [CrossRef]
- Hou, S.; Zhang, Y.Y.; Christian, L.; Niechwiej-Szwedo, E.; Giaschi, D. Evaluating visuomotor coordination in children with amblyopia. Dev. Psychobiol. 2022, 64, e22270. [Google Scholar] [CrossRef]
- Kelly, K.R.; Morale, S.E.; Beauchamp, C.L.; Dao, L.M.; Luu, B.A.; Birch, E.E. Factors associated with impaired motor skills in strabismic and anisometropic children. Investig. Ophthalmol. Vis. Sci. 2020, 61, 43. [Google Scholar] [CrossRef] [PubMed]
- Webber, A.L.; Wood, J.M.; Thompson, B. Fine motor skills of children with amblyopia improve following binocular treatment. Investig. Ophthalmol. 2016, 57, 4713–4720. [Google Scholar] [CrossRef] [PubMed]
- Sheppard, W.E.A.; Dickerson, P.; Baraas, R.C.; Mon-Williams, M.; Barrett, B.T.; Wilkie, R.M.; Coats, R.O. Exploring the effects of degraded vision on sensorimotor performance. PLoS ONE 2021, 16, 0258678. [Google Scholar] [CrossRef] [PubMed]
- Smits-Engelsman, B.C.; Niemeijer, A.S.; van Galen, G.P. Fine motor deficiencies in children diagnosed as DCD based on poor grapho-motor ability. Hum. Mov. Sci. 2001, 20, 161–182. [Google Scholar] [CrossRef] [PubMed]
- Lin, Q.; Luo, J.; Wu, Z.; Shen, F.; Sun, Z. Characterization of fine motor development: Dynamic analysis of children’s drawing movements. Hum. Mov. Sci. 2015, 40, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Rueckriegel, S.; Blankenburg, F.; Burghardt, R.; Ehrlich, S.; Henze, G.; Mergl, R.; Driever, P.H. Influence of age and movement complexity on kinematic hand movement parameters in childhood and adolescence. Int. J. Dev. Neurosci. 2008, 26, 655–663. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.C.T.; Bisi, M.C.; Duncan, M.J.; Stagni, R. Technology-based methods for the assessment of fine and gross motor skill in children: A systematic overview of available solutions and future steps for effective in-field use. J. Sports Sci. 2021, 39, 1236–1276. [Google Scholar] [CrossRef]
- Mailleux, L.; Jaspers, E.; Ortibus, E.; Simon-Martinez, C.; Desloovere, K.; Molenaers, G.; Klingels, K.; Feys, H. Clinical assessment and three-dimensional movement analysis: An integrated approach for upper limb evaluation in children with unilateral cerebral palsy. PLoS ONE 2017, 12, 0180196. [Google Scholar] [CrossRef]
- Lapresa, M.; Zollo, L.; Cordella, F. A user-friendly automatic toolbox for hand kinematic analysis, clinical assessment and postural synergies extraction. Front. Bioeng. Biotechnol. 2022, 10, 1010073. [Google Scholar] [CrossRef]
- Schwarz, A.; Kanzler, C.; Lambercy, O.; Luft, A.; Veerbeek, J. Systematic review on kinematic assessments of upper limb movements after stroke. Stroke 2019, 50, 718–727. [Google Scholar] [CrossRef]
- Cronin, N.J. Using deep neural networks for kinematic analysis: Challenges and opportunities. J. Biomech. 2021, 123, 110460. [Google Scholar] [CrossRef] [PubMed]
- Hay, L. Spatial-temporal analysis of movements in children. J. Mot. Behav. 1979, 11, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Smyth, M.M.; Peacock, K.A.; Katamba, J. The role of sight of the hand in the development of prehension in childhood. Q. J. Exp. Psychol. 2004, 57A, 269–296. [Google Scholar] [CrossRef] [PubMed]
- Von Hofsten, C. Developmental changes in the organization of pre-reaching movements. Dev. Psychol. 1984, 3, 378–388. [Google Scholar] [CrossRef]
- Elliott, D.; Lyons, J.; Hayes, S.J.; Burkitt, J.J.; Hansen, S.; Grierson, L.E.; Foster, N.C.; Roberts, J.W.; Bennett, S.J. The multiple process model of goal-directed aiming/reaching: Insights on limb control from various special populations. Exp. Brain Res. 2020, 238, 2685–2699. [Google Scholar] [CrossRef] [PubMed]
- Burr, D.; Gori, M. Multisensory Integration Develops Late in Humans; Murray, M., Wallace, M., Eds.; CRC Press/Taylor & Francis: Boca Raton, FL, USA, 2012. [Google Scholar]
- Mohan, A.; Sen, P.; Shah, C.; Datt, K.; Jain, E. Binocular Accommodation and Vergence Dysfunction in Children Attending Online Classes During the COVID-19 Pandemic: Digital Eye Strain in Kids (DESK) Study-2. J. Pediatr. Ophthalmol. Strabismus 2021, 58, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Hussaindeen, J.R.; Rakshit, A.; Singh, N.K.; Swaminathan, M.; George, R.; Kapur, S.; Scheiman, M.; Ramani, K.K. Binocular vision anomalies and normative data (BAND) in Tamil Nadu: Report 1. Clin. Exp. Optom. 2017, 100, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Maharjan, U.; Rijal, S.; Jnawali, A.; Sitaula, S.; Bhattarai, S.; Shrestha, G.B. Binocular vision findings in normally-sighted school aged children who used digital devices. PLoS ONE 2022, 17, e0266068. [Google Scholar] [CrossRef]
- Porcar, E.; Martinez-Palomera, A. Prevalence of general binocular dysfunctions in a population of university students. Optom. Vis. Sci. 1997, 74, 111–113. [Google Scholar] [CrossRef]
- Jorge, J.; Diaz-Rey, A.; Lira, M. Prevalence of binocular vision dysfunctions in professional football players. Clin. Exp. Optom. 2022, 105, 853–859. [Google Scholar] [CrossRef] [PubMed]
- García-Muñoz, Á.; Carbonell-Bonete, S.; Cantó-Cerdán, M.; Cacho-Martínez, P. Accommodative and binocular dysfunctions: Prevalence in a randomised sample of university students. Clin. Exp. Optom. 2016, 99, 313–321. [Google Scholar] [CrossRef] [PubMed]


| Patient 1 | Patient 2 | |
|---|---|---|
| Age (years); Sex | 12; female | 13; male |
| Type of amblyopia Visual acuity (logMAR): | Strabismic Right eye: 0.10 Left eye: 0.40 | * NA Right eye: 0.40 Left eye: 0.70 |
| Stereoacuity (arc sec) | >400 | >400 |
| Handedness | Left | Right |
| Vision and Motor Outcomes | Middle Age Band (7–10 Years Old) (n = 23, 44% Girls) | Older Age Band (11–16 Years Old) (n = 24, 46% Girls) | t-Test (df = 45) p-Value |
|---|---|---|---|
| Vision assessment (mean ± standard deviation) | |||
| Binocular visual acuity (logMAR) | −0.04 ± 0.10 | −0.11 ± 0.11 | 2.21 p = 0.032 |
| Monocular visual acuity (logMAR) | 0.00 ± 0.10 | −0.03 ± 0.09 | 1.32 p = 0.192 |
| Stereoacuity (arc sec) | 39 ± 21 | 36 ± 27 | 0.46 p = 0.645 |
| MABC-2 assessment (mean ± standard deviation) | |||
| Peg-board task with the preferred hand (standard score) | 7.61 ± 2.90 | 9.25 ± 3.43 | 1.32 p = 0.193 |
| Peg-board task with the non-preferred hand (standard score) | 7.82 ± 3.01 | 9.04 ± 3.29 | 1.77 p = 0.084 |
| Manipulation task (standard score) | 8.08 ± 3.50 | 7.17 ± 3.98 | 0.84 p = 0.406 |
| Trail-making task (standard score) | 6.78 ± 3.94 | 10.37 ± 3.10 | 3.48 p = 0.001 |
| PERCENTILE | 27.52 ± 27.25 | 40.54 ± 26.58 | 1.66 p = 0.104 |
| Kinematic assessment (mean ± standard deviation) | |||
| Peak velocity (m/s) | 1.183 ± 0.154 | 1.088 ± 0.239 | t = 1.60 p = 0.116 |
| Reach duration (ms) | 410 ± 50 | 405 ± 96 | t = 0.32 p = 0.753 |
| Grasp duration (ms) | 240 ± 94 | 192 ± 152 | t = 1.30 p = 0.200 |
| Thread duration (ms) | 615 ± 169 | 445 ± 95 | t = 4.26 p < 0.001 |
| Total movement time (ms) | 1675 ± 282 | 1452 ± 275 | t = 2.74 p = 0.008 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niechwiej-Szwedo, E.; Brin, T.A.; Thompson, B.; Christian, L.W.T. Kinematic Assessment of Fine Motor Skills in Children: Comparison of a Kinematic Approach and a Standardized Test. Vision 2024, 8, 6. https://doi.org/10.3390/vision8010006
Niechwiej-Szwedo E, Brin TA, Thompson B, Christian LWT. Kinematic Assessment of Fine Motor Skills in Children: Comparison of a Kinematic Approach and a Standardized Test. Vision. 2024; 8(1):6. https://doi.org/10.3390/vision8010006
Chicago/Turabian StyleNiechwiej-Szwedo, Ewa, Taylor A. Brin, Benjamin Thompson, and Lisa W. T. Christian. 2024. "Kinematic Assessment of Fine Motor Skills in Children: Comparison of a Kinematic Approach and a Standardized Test" Vision 8, no. 1: 6. https://doi.org/10.3390/vision8010006
APA StyleNiechwiej-Szwedo, E., Brin, T. A., Thompson, B., & Christian, L. W. T. (2024). Kinematic Assessment of Fine Motor Skills in Children: Comparison of a Kinematic Approach and a Standardized Test. Vision, 8(1), 6. https://doi.org/10.3390/vision8010006






