Prevalence of Near-Vision-Related Symptoms in a University Population
Abstract
:1. Introduction
2. Materials and Methods
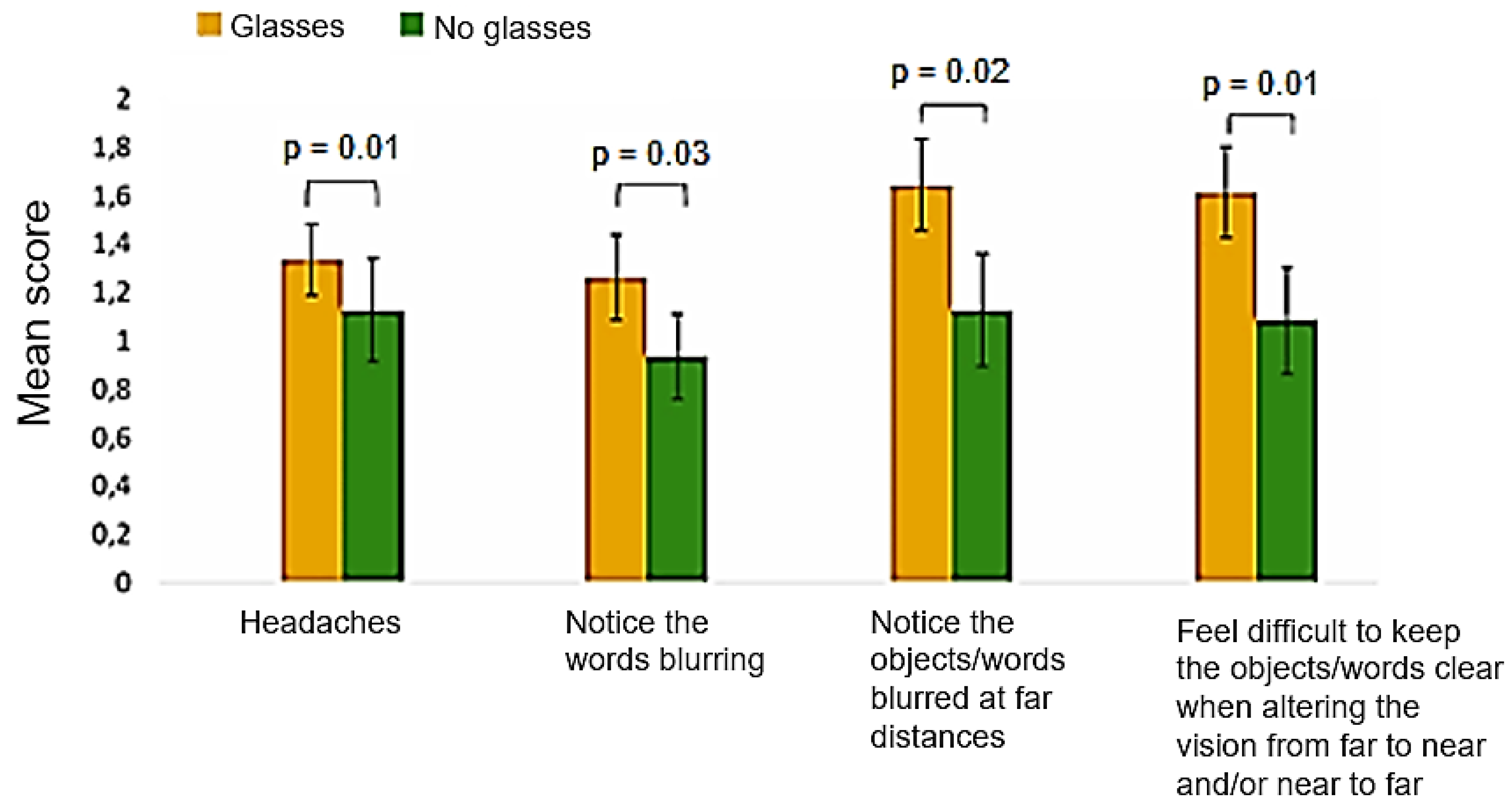
- Do you notice the objects/words blurred at far distances after reading/doing close work?
- Do you find it difficult to keep the objects/words clear when you alter the vision from far to near and/or near to far?
- Objective ocular refraction with static retinoscopy
- Subjective ocular refraction started from the value of the objective refraction, and the maximum plus refraction for best visual acuity was found for each eye. Myopia was defined as a spherical equivalent refractive error of greater than or equal to −0.50 D and hyperopia greater than or equal to +0.50 D [23].
- Assessment of monocular amplitude of accommodation by the minus lens method, adding negative lenses in steps of 0.25 D until the subject sees one line blur before the maximum visual acuity placed at 40 cm.
- Assessment of lag of accommodation by monocular estimated method (MEM) retinoscopy. While the subject read the words of a MEM card, retinoscopy was performed along the horizontal axis and estimated the amount of plus or minus necessary to neutralize the motion of the reflex observed through the retinoscope.
- Assessment of monocular facility of accommodation at near vision (targeting one line before the maximum visual acuity placed at 40 cm) with flippers of ±2.00 D.
- Measurement of horizontal phoria using the von Graefe technique for distance and near vision. A phoropter with Risley prisms of 12 base-in and 6 base-out was used for distance vision, and 15 base-in and 9 base-out for near vision. A column of letters with a visual acuity of 0.8 was used as a fixation target at 6 m and 40 cm for the far and near measurement of phoria, respectively. Negative values represent exophoria, and positive values esophoria.
- Measurement of positive and negative fusional vergences for far and near vision. The same target was used, and the values of blur, break and recovery were recorded.
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hayes, J.R.; Sheedy, J.E.; Stelmack, J.A.; Heaney, C.A. Computer use, symptoms, and quality of life. Optom. Vis. Sci. 2007, 84, 738–755. [Google Scholar] [CrossRef]
- Rossignol, A.M.; Morse, E.P.; Summers, V.M.; Pagnotto, L.D. Video display terminal use and reported health symptoms among massachusetts clerical workers. J. Occup. Med. Off. Publ. Ind. Med. Assoc. 1987, 29, 112–118. [Google Scholar]
- Cantó-Sancho, N.; Porru, S.; Casati, S.; Ronda, E.; Seguí-Crespo, M.; Carta, A. Prevalence and risk factors of computer vision syndrome—Assessed in office workers by a validated questionnaire. PeerJ 2023, 11, e14937. [Google Scholar] [CrossRef]
- Cantó-Sancho, N.; Sánchez-Brau, M.; Ivorra-Soler, B.; Seguí-Crespo, M. Computer vision syndrome prevalence according to individual and video display terminal exposure characteristics in Spanish university students. Int. J. Clin. Pr. 2021, 75, e13681. [Google Scholar] [CrossRef]
- Daum, K.M.; Clore, K.A.; Simms, S.S.; Vesely, J.W.; Wilczek, D.D.; Spittle, B.M.; Good, G.W. Productivity associated with visual status of computer users. Optometry 2004, 75, 33–47. [Google Scholar] [CrossRef]
- Hussaindeen, J.R.; Murali, A. Accommodative insufficiency: Prevalence, impact and treatment options. Clin. Optom. 2020, 12, 135–149. [Google Scholar] [CrossRef]
- Park, M.; Ahn, Y.J.; Kim, S.J.; You, J.K. Changes in accommoda tive function of young adults in their twenties following smartphone use. JKOOS 2014, 19, 253–260. [Google Scholar] [CrossRef]
- Kwon, K.-I.; Kim, H.J.; Park, M.; Kim, S.R. The functional change of accommodation and convergence in the mid-forties by using smartphone. J. Korean Ophthalmic Opt. Soc. 2016, 21, 127–135. [Google Scholar] [CrossRef]
- Jaiswal, S.; Asper, L.; Long, J.; Lee, A.; Harrison, K.; Golebiowski, B. Ocular and visual discomfort associated with smartphones, tablets and computers: What we do and do not know. Clin. Exp. Optom. 2019, 102, 463–477. [Google Scholar] [CrossRef]
- Abdi, S.; Rydberg, A. Asthenopia in schoolchildren, orthoptic and ophthalmological findings and treatment. Doc. Ophthalmol. 2005, 111, 65–72. [Google Scholar] [CrossRef]
- Cacho-Martínez, P.; García-Muñoz, Á.; Ruiz-Cantero, M.T. Do we really know the prevalence of accomodative and nonstrabismic binocular dysfunctions? J. Optom. 2010, 3, 185–197. [Google Scholar] [CrossRef]
- Negiloni, K.; Ramani, K.K.S.R. Do school classrooms meet the visual requirements of children and recommended vision standards? PLoS ONE 2017, 12, e0174983. [Google Scholar] [CrossRef]
- Adams, C.; Leach, S.; Kresch, Y.S.; Brooks, S.E. Actual Visual Acuity Demands in the Classroom. J. Pediatr. Ophthalmol. Strabismus. 2021, 58, 48–54. [Google Scholar] [CrossRef]
- Amiebenomo, O.M.-A.; Isong, E.M.; Edosa, M.E.; Woodhouse, J.M. Habitual visual acuity and visual acuity threshold demands in Nigerian school classrooms. Sci. Rep. 2022, 12, 17816. [Google Scholar] [CrossRef]
- Vision to Learn. UCLA Study: Impact Analysis of Vision to Learn. 2022. Available online: https://visiontolearn.org/impact/ucla-study-impact-analysis-of-vision-to-learn/ (accessed on 1 March 2024).
- Grisham, D.; Powers, M.; Riles, P. Visual skills of poor readers in high school. Optometry 2007, 78, 542–549. [Google Scholar] [CrossRef]
- Muzaliha, M.N.; Nurhamiza, B.; Hussein, A.; Norabibas, A.R.; Mohd-Hisham-Basrun, J.; Sarimah, A.; Leo, S.W.; Shatriah, I. Visual acuity and visual skills in Malaysian children with learning disabilities. Clin. Ophthalmol. 2011, 6, 1527–1533. [Google Scholar]
- Hashemi, H.; Khabazkhoob, M.; Nabovati, P.; Shahraki, F.A.; Ostadimoghaddam, H.; Faghihi, M.; Aghamirsalim, M.; Doostdar, A.; Yekta, A. Accommodative insufficiency in a student population in Iran. J. Optom. 2019, 12, 161–167. [Google Scholar] [CrossRef]
- Porcar, E.; Martinez-Palomera, A. Prevalence of general binocular dysfunctions in a population of university students. Optom. Vis. Sci. 1997, 74, 111–113. [Google Scholar] [CrossRef]
- Ma, M.M.-L.; Yeo, A.C.H.; Scheiman, M.; Chen, X. Vergence and Accommodative Dysfunctions in Emmetropic and Myopic Chinese Young Adults. J. Ophthalmol. 2019, 2019, 5904903. [Google Scholar] [CrossRef]
- Ma, J.; Yang, X.; Liu, Z.; Fu, H.; Fan, S.; Wang, K.; Li, Y.; Huang, L.; Zhao, M. The Impact of Vergence Dysfunction on Myopia Control in Children Wearing Defocus Spectacle Lenses. Clin. Ophthalmol. 2024, 18, 799–807. [Google Scholar] [CrossRef]
- Rouse, M.; Borsting, E.; Mitchell, G.L.; Cotter, S.A.; Kulp, M.; Scheiman, M.; Barnhardt, C.; Bade, A.; Yamada, T.; Convergence Insufficiency Treatment Trial (CITT) Investigator Group. Validity of the convergence insufficiency symptom survey: A confirmatory study. Optom. Vis. Sci. 2009, 86, 357–363. [Google Scholar] [CrossRef]
- Flitcroft, D.I.; He, M.; Jonas, J.B.; Jong, M.; Naidoo, K.; Ohno-Matsui, K.; Rahi, J.; Resnikoff, S.; Vitale, S.; Yannuzzi, L. IMI-Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies. Investig. Ophthalmol. Vis. Sci. 2019, 28, M20–M30. [Google Scholar] [CrossRef]
- Lara, F.; Cacho, P.; García, Á.; Megías, R. General binocular disorders: Prevalence in a clinic population. Ophthalmic Physiol. Opt. 2001, 21, 70–74. [Google Scholar] [CrossRef]
- Darko-Takyi, C.; Owusu-Ansah, A.; Boampong, F.; Morny, E.K.; Hammond, F.; Ocansey, S. Convergence insufficiency symptom survey (CISS) scores are predictive of severity and number of clinical signs of convergence insufficiency in young adult Africans. J. Optom. 2022, 15, 228–237. [Google Scholar] [CrossRef]
- Horwood, A.M.; Toor, S.; Riddell, P.M. Screening for convergence insufficiency using the CISS is not indicated in young adults. Br. J. Ophthalmol. 2014, 98, 679–683. [Google Scholar] [CrossRef]
- Shetty, A.; Fernandes, E.L.; Usgaonkar, U. Effect of stress on convergence insufficiency symptom score (CISS) among optometrists and optometry students. Ophthalmol. J. 2023, 8, 5–12. [Google Scholar] [CrossRef]
- AlQarni, A.M.; AlAbdulKader, A.M.; Alghamdi, A.N.; Altayeb, J.; Jabaan, R.; Assaf, L.; Alanazi, R.A. Prevalence of Digital Eye Strain Among University Students and Its Association with Virtual Learning During the COVID-19 Pandemic. Clin. Ophthalmol. 2023, 17, 1755–1768. [Google Scholar] [CrossRef]
- Zalat, M.M.; Amer, S.M.; Wassif, G.A.; El Tarhouny, S.A.; Mansour, T.M. Computer vision syndrome, visual ergonomics and amelioration among staff members in a Saudi medical college. Int. J. Occup. Saf. Erg. 2022, 28, 1033–1041. [Google Scholar] [CrossRef]
- Mowatt, L.; Gordon, C.; Santosh, A.B.R.; Jones, T. Computer vision syndrome and ergonomic practices among undergraduate university students. Computer vision syndrome and ergonomic practices among undergraduate university students. Int. J. Clin. Pr. 2018, 72, e13035. [Google Scholar] [CrossRef]
- Yap, T.P.; Luu, C.D.; Suttle, C.; Chia, A.; Boon, M.Y. Effect of Stimulus Orientation on Visual Function in Children with Refractive Amblyopia. Investig. Ophthalmol. Vis. Sci. 2020, 61, 5. [Google Scholar] [CrossRef]
- Franco, S.; Moreira, A.; Fernandes, A.; Baptista, A. Accommodative and binocular vision dysfunctions in a Portuguese clinical population. J. Optom. 2021, 15, 271–277. [Google Scholar] [CrossRef]
- De-Hita-Cantalejo, C.; Benítez-Rodríguez, M.D.; Sánchez-González, M.C.; Bautista-Llamas, M.J.; Sánchez-González, J.M. Accommodation Response Variations in University Students under High Demand for Near-Vision Activity. Life 2022, 12, 1837. [Google Scholar] [CrossRef]
- Wajuihian, S.O. Characterizing Refractive Errors, Near Accommodative and dysu Anomalies and Symptoms in an Optometry Clinic. Br. Ir. Orthopt. J. 2022, 18, 76–92. [Google Scholar] [CrossRef]
- Syeda, S.I.; Kumar, R.; Jayaseelan, X.C.; Vijayaraghavan, R. A Comparative Study to Assess the Accommodation and Vergence Relationship of Myopia in Indian Adolescent. Ethiop. J. Health Sci. 2023, 33, 523–532. [Google Scholar]
| Accommodative Dysfunctions | |||
|---|---|---|---|
| Infacility of accommodation | Excess of accommodation | Insufficiency of accommodation | |
| Criteria | Present signs a and b | Present signs a, b and c, and two between d and f | Present signs a and b, and two between c and e |
| Signal | (a) Monocular accommodative facility ≤ 6 cpm and binocular ≤ 3 cpm (b) PRA ≤ 1.25 D and NRA ≤ 1.50 D | (a) Variable VA (b) Variable static retinoscopy/subjective refraction (c) Monocular accommodative facility ≤ 6 cpm with difficulty with the lens +2.00 D (d) Binocular accommodative facility ≤ 3 cpm with difficulty with the lens +2.00 D (e) MEM < +0.25 D (f) NRA ≤ 1.50 D | (a) AA at least 2.00 D below (b) Monocular accommodative facility ≤ 6 cpm with difficulty with the lens −2.00 D (c) Binocular accommodative facility ≤ 3 cpm with difficulty with the lens −2.00 D (d) MEM > +0.75 D (e) PRA ≤ 1.25 D |
| Binocular dysfunctions | |||
| Convergence insufficiency | Convergence excess | ||
| Criteria | Present signs a, b and c, and two of d, e, f and g | Present signs a and b, and two of c, d e and f. | |
| Signal | (a) Exophoria at near > 6∆ (b) PFV at near ≤ 11/14/3 (blur/break/recovery) (c) NPC > 10 cm (d) AC/A ratio < 3/1 (e) Fails BAF with +2.00 D (≤3 cpm) (f) MEM < +0.25 D (g) PRA ≤ 1.50 D | (a) Esophoria > 2∆ (b) NFV ≤ 8/16/7 (blur/break/recovery) (c) AC/A > 7/1 (d) Fails BAF with −2.00 D (≤3 cpm) (e) MEM > +0.75 D (f) PRA ≤ 1.25 D | |
| Answer | |||||
|---|---|---|---|---|---|
| Question | Never | Infrequently/ Not Very Often | Sometimes | Fairly Often | Always |
| Eyes tired | 8.3% | 23.0% | 41.3% | 23.4% | 4.0% |
| Uncomfortable | 17.1% | 27.8% | 36.1% | 17.9% | 1.2% |
| Headaches | 25.0% | 35.3% | 29.8% | 2.3% | 1.6% |
| Sleepy | 23.4% | 26.2% | 33.7% | 14.7% | 2.0% |
| Difficulty maintaining attention/concentration | 20.6% | 31.7% | 28.6% | 16.7% | 2.4% |
| Trouble remembering | 15.5% | 29.0% | 34.1% | 19.4% | 2.0% |
| Double vision | 58.3% | 20.2% | 15.9% | 5.2% | 0.4% |
| Words moving, jumping or seeming to float across the page | 67.9% | 22.2% | 6.3% | 3.6% | 0.0% |
| Feel like reading slowly | 40.9% | 29.0% | 21.4% | 6.0% | 2.8% |
| Eyes hurt | 37.7% | 28.2% | 26.2% | 6.3% | 1.6% |
| Red eyes | 36.5% | 29.8% | 23.0% | 9.5% | 1.2% |
| “Pulling” feeling around eyes | 33.3% | 30.6% | 24.2% | 11.5% | 0.4% |
| Notice the words blurring while reading/doing close work | 33.3% | 31.7% | 23.4% | 10.3% | 1.2% |
| Lose own place | 28.2% | 38.1% | 24.2% | 9.1% | 0.4% |
| Need to reread the same line | 15.5% | 32.1% | 30.6% | 21.0% | 0.8% |
| Notice the objects/words blurred at far distances | 29.4% | 21.8% | 27.4% | 16.7% | 4.8% |
| Feel difficult to keep the objects/words clear when altering the vision from far to near and/or near to far | 26.2% | 30.6% | 23.4% | 14.7% | 5.2% |
| N | % | ||
|---|---|---|---|
| With accommodative dysfunction | 34 | 30.9 | |
| Infacility of accommodation | 6 | 5.5 | |
| Excess of accommodation | 11 | 10.0 | |
| Insufficiency of accommodation | 17 | 15.5 | |
| Without accommodative dysfunction | 76 | 69.1 | |
| Total | 110 | 100 | |
| Far | Phoria (∆) | Positive Fusional Vergence (∆) | Negative Fusional Vergence (∆) | ||||
| Blur | Break | Recovery | Blur | Break | Recovery | ||
| −1.12 ± 2.33 | 12.85 ± 4.95 | 19.82 ± 6.61 | 9.50 ± 6.20 | 8.65 ± 3.45 | 4.51 ± 2.65 | ||
| Near | Phoria (∆) | Positive Fusional Vergence (∆) | Negative Fusional Vergence (∆) | ||||
| Blur | Break | Recovery | Blur | Break | Recovery | ||
| −4.22 ± 4.89 | 20.42 ± 7.93 | 24.63 ± 8.32 | 14.63 ± 8.68 | 14.08 ± 5.35 | 20.10 ± 4.90 | 14.69 ± 11.39 | |
| N (Percentage) | |||||
|---|---|---|---|---|---|
| Without AD | With AD | Infacility | Excess | Insufficiency | |
| Emmetropes | 35 (67.3%) | 17 (32.7%) | 3 (5.8%) | 7 (13.5%) | 7 (13.5%) |
| Myopes | 28 (80%) | 7 (20%) | 2 (5.7%) | 0 (0.0%) | 5 (14.3%) |
| Hyperopes | 12 (57.1%) | 9 (42.9%) | 1 (4.8%) | 4 (19%) | 4 (19%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gomes, J.; Franco, S. Prevalence of Near-Vision-Related Symptoms in a University Population. Vision 2024, 8, 38. https://doi.org/10.3390/vision8020038
Gomes J, Franco S. Prevalence of Near-Vision-Related Symptoms in a University Population. Vision. 2024; 8(2):38. https://doi.org/10.3390/vision8020038
Chicago/Turabian StyleGomes, Jessica, and Sandra Franco. 2024. "Prevalence of Near-Vision-Related Symptoms in a University Population" Vision 8, no. 2: 38. https://doi.org/10.3390/vision8020038





