Virtual Reality in Health Science Education: Professors’ Perceptions
Abstract
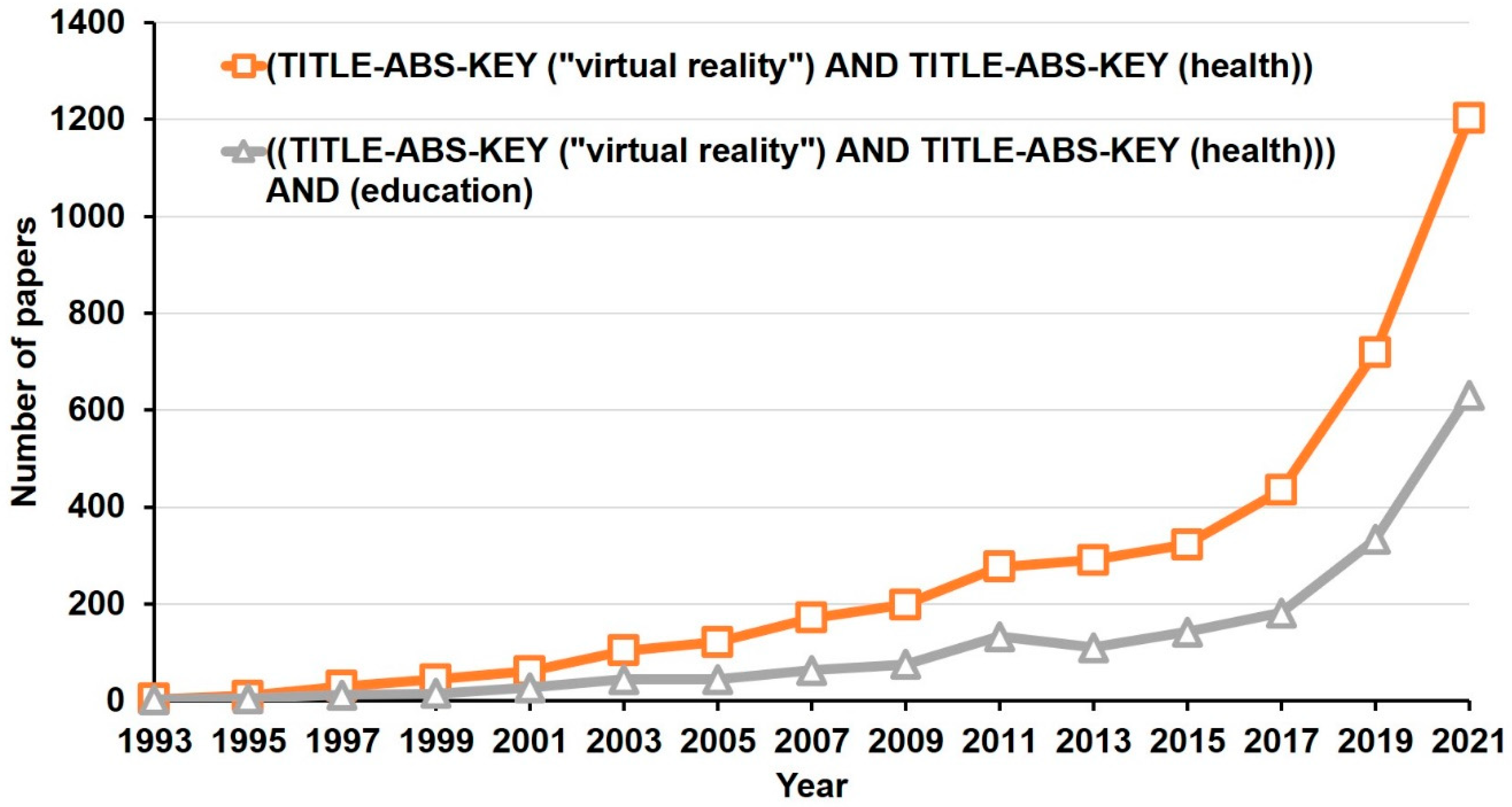
:1. Introduction
2. Materials and Methods
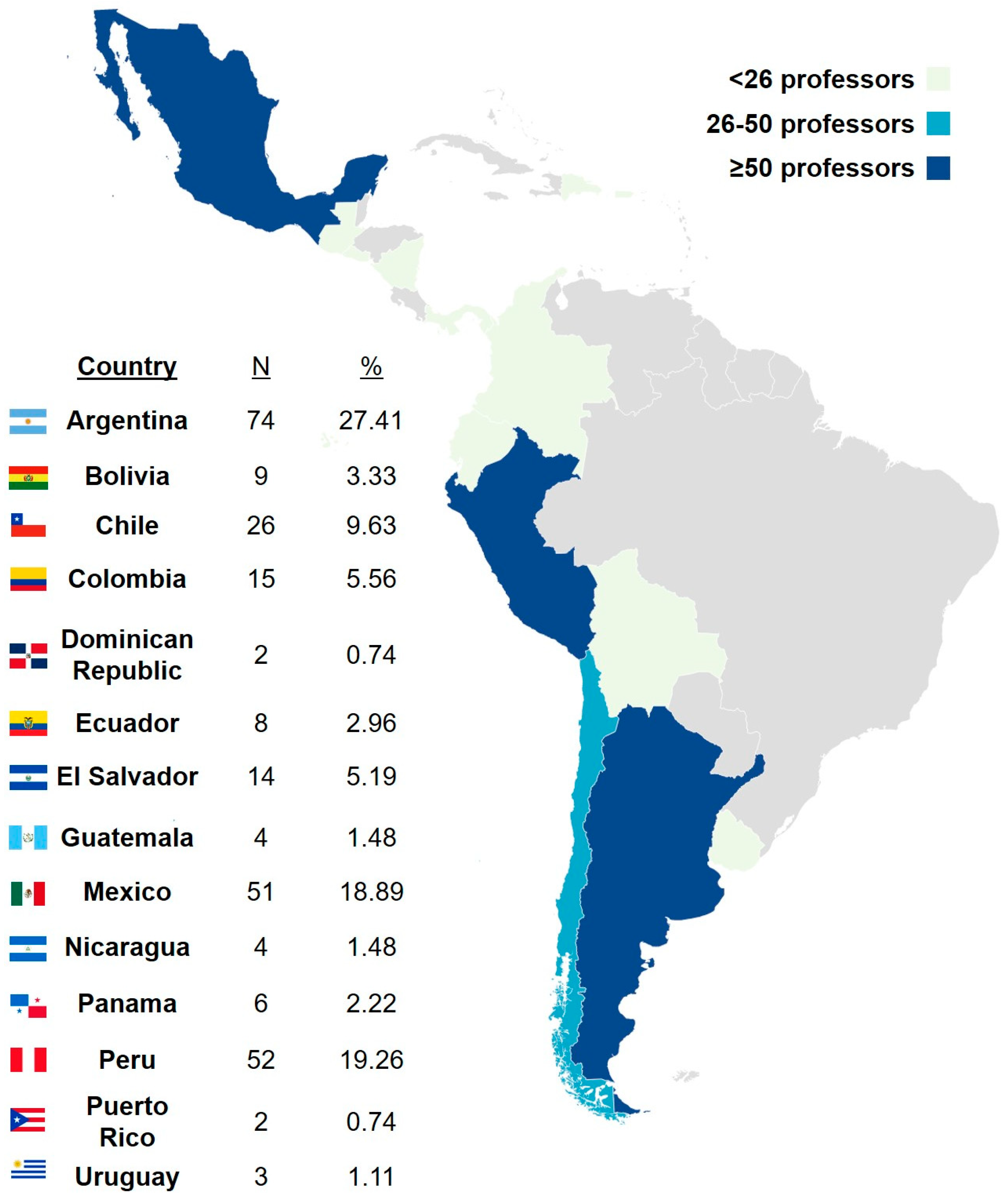
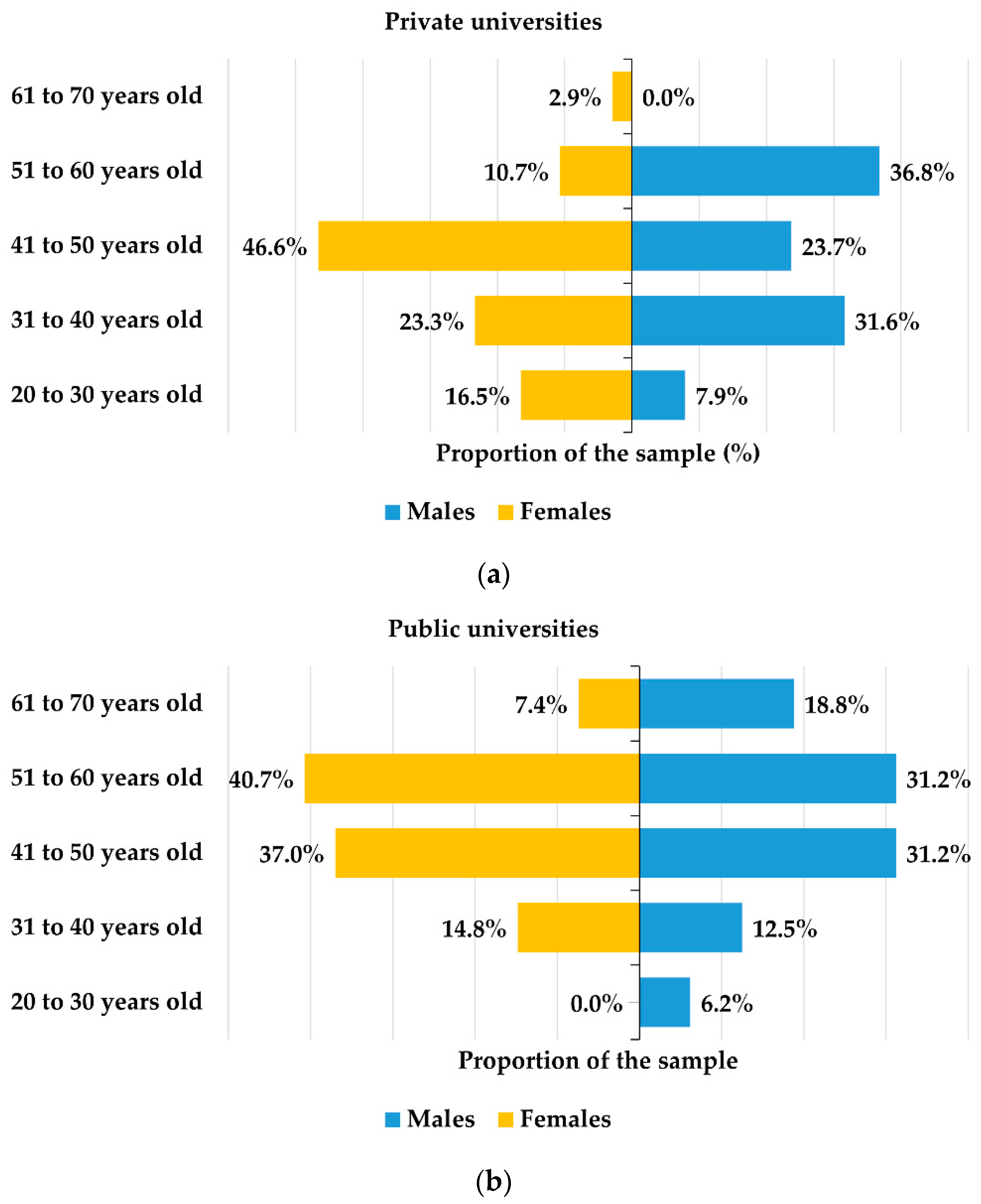
2.1. Participants
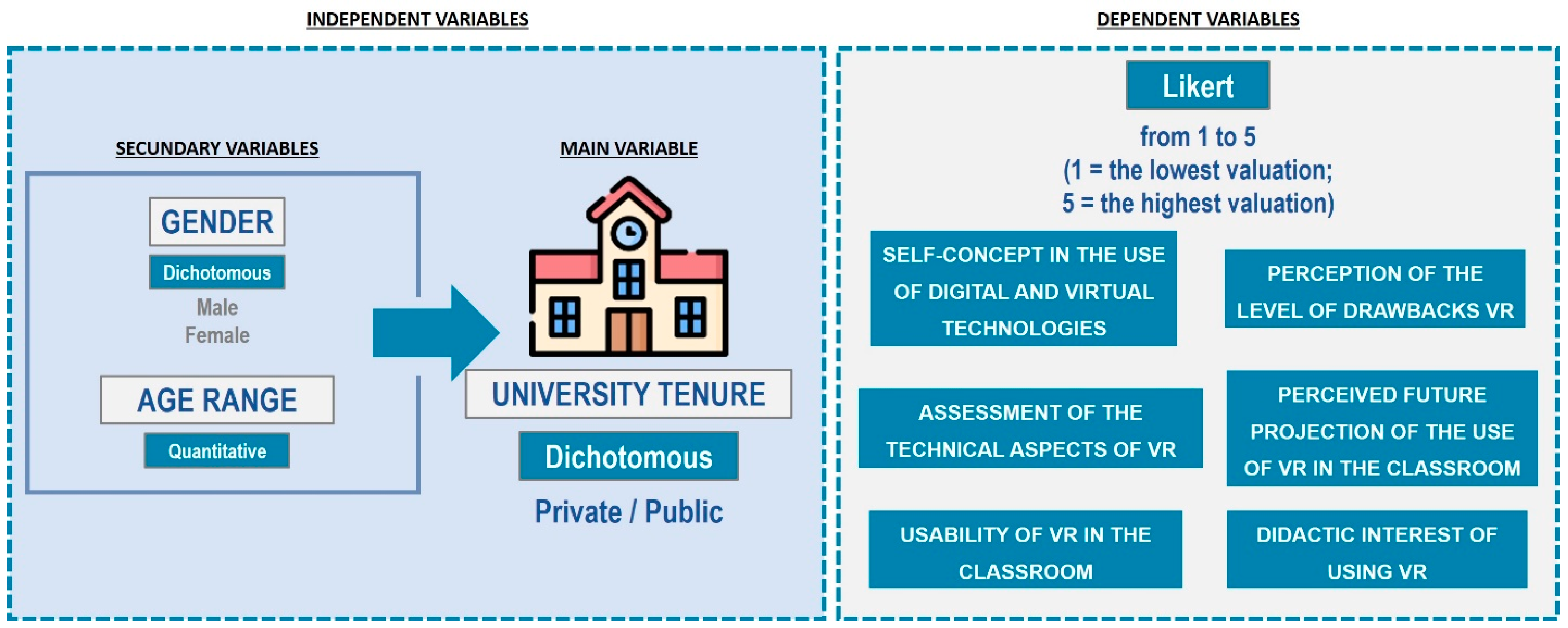
2.2. Objectives and Variables
2.3. Instrument
2.4. Design and Statistical Analysis
3. Results
4. Discussion
5. Limitations and Lines of Future Research
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wang, S.; Parsons, M.; Stone-McLean, J.; Rogers, P.; Boyd, S.; Hoover, K.; Meruvia-Pastor, O.; Gong, M.; Smith, A. Augmented Reality as a Telemedicine Platform for Remote Procedural Training. Sensors 2017, 17, 2294. [Google Scholar] [CrossRef] [PubMed]
- Koulouris, D.; Menychtas, A.; Maglogiannis, I. An IoT-Enabled Platform for the Assessment of Physical and Mental Activities Utilizing Augmented Reality Exergaming. Sensors 2022, 22, 3181. [Google Scholar] [CrossRef] [PubMed]
- Dahl, T.S.; Boulos, M.N.K. Robots in Health and Social Care: A Complementary Technology to Home Care and Telehealthcare? Robotics 2014, 3, 1–21. [Google Scholar] [CrossRef] [Green Version]
- Vergara-Rodríguez, D.; Gómez-Asenjo, A.; Fernández-Arias, P.; Gómez-Vallecillo, A.I.; Lamas-Álvarez, V.E.; Santos-Iglesia, C. Immersive vs. Non-Immersive Virtual Reality Learning Environments. In Proceedings of the 2021 XI International Conference on Virtual Campus (JICV), Salamanca, Spain, 30 September 2021–1 October 2021; pp. 1–3. [Google Scholar] [CrossRef]
- Miguel, C.; Castro, L.; Marques dos Santos, J.P.; Serrão, C.; Duarte, I. Impact of COVID-19 on Medicine Lecturers’ Mental Health and Emergency Remote Teaching Challenges. Int. J. Environ. Res. Public Health 2021, 18, 6792. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Javaid, M.; Kataria, R.; Tyagi, M.; Haleem, A.; Suman, R. Significant Applications of Virtual Reality for COVID-19 Pandemic. Diabetes Metab. Syndr. 2020, 14, 661–664. [Google Scholar] [CrossRef]
- Petrigna, L.; Musumeci, G. The Metaverse: A New Challenge for the Healthcare System: A Scoping Review. J. Funct. Morphol. Kinesiol. 2022, 7, 63. [Google Scholar] [CrossRef]
- Sánchez-Cabrero, R.; Arigita-García, A.; Barrientos-Fernández, A.; León-Mejía, A.C. Online Explorative Study on the Learning Uses of Virtual Reality Among Early Adopters. JoVE (J. Vis. Exp.) 2019, 153, e60188. [Google Scholar] [CrossRef]
- Sánchez-Cabrero, R.; Costa-Román, O.; Pericacho-Gomez, F.J.; Novillo-López, M.A.; Arigita-García, A.; Barrientos-Fernandez, A. Early Virtual Reality Adopters in Spain: Sociodemographic Profile and Interest in the Use of Virtual Reality as a Learning Tool. Heliyon 2019, 5, 01338. [Google Scholar] [CrossRef] [Green Version]
- Rutkowski, S. Management Challenges in Chronic Obstructive Pulmonary Disease in the COVID-19 Pandemic: Telehealth and Virtual Reality. J. Clin. Med. 2021, 10, 1261. [Google Scholar] [CrossRef]
- Vergara, D.; Rubio, M.P.; Lorenzo, M. On the Design of Virtual Reality Learning Environments in Engineering. Multimodal Technol. Interact. 2017, 1, 11. [Google Scholar] [CrossRef] [Green Version]
- Muhanna, M.A. Virtual Reality and the CAVE: Taxonomy, Interaction Challenges and Research Directions. J. King Saud Univ.-Comput. Inf. Sci. 2015, 27, 344–361. [Google Scholar] [CrossRef] [Green Version]
- Gu, C. Short-Range Noncontact Sensors for Healthcare and Other Emerging Applications: A Review. Sensors 2016, 16, 1169. [Google Scholar] [CrossRef] [Green Version]
- Caponnetto, P.; Casu, M. Update on Cyber Health Psychology: Virtual Reality and Mobile Health Tools in Psychotherapy, Clinical Rehabilitation, and Addiction Treatment. Int. J. Environ. Res. Public Health 2022, 19, 3516. [Google Scholar] [CrossRef]
- Bopp, T.; Stellefson, M. Practical and Ethical Considerations for Schools Using Social Media to Promote Physical Literacy in Youth. Int. J. Environ. Res. Public Health 2020, 17, 1225. [Google Scholar] [CrossRef] [Green Version]
- Riva, G. From Telehealth to E-Health: Internet and Distributed Virtual Reality in Health Care. CyberPsychology Behav. 2000, 3, 989–998. [Google Scholar] [CrossRef]
- Matamala-Gomez, M.; Maselli, A.; Malighetti, C.; Realdon, O.; Mantovani, F.; Riva, G. Virtual Body Ownership Illusions for Mental Health: A Narrative Review. J. Clin. Med. 2021, 10, 139. [Google Scholar] [CrossRef]
- Morimoto, T.; Kobayashi, T.; Hirata, H.; Otani, K.; Sugimoto, M.; Tsukamoto, M.; Yoshihara, T.; Ueno, M.; Mawatari, M. XR (Extended Reality: Virtual Reality, Augmented Reality, Mixed Reality) Technology in Spine Medicine: Status Quo and Quo Vadis. J. Clin. Med. 2022, 11, 470. [Google Scholar] [CrossRef]
- Tian, S.; Yang, W.; Grange, J.M.L.; Wang, P.; Huang, W.; Ye, Z. Smart healthcare: Making medical care more intelligent. Glob. Health J. 2019, 3, 62–65. [Google Scholar] [CrossRef]
- Liu, Z.; Ren, L.; Xiao, C.; Zhang, K.; Demian, P. Virtual Reality Aided Therapy towards Health 4.0: A Two-Decade Bibliometric Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1525. [Google Scholar] [CrossRef]
- Alauddin, M.S.; Baharuddin, A.S.; Mohd Ghazali, M.I. The Modern and Digital Transformation of Oral Health Care: A Mini Review. Healthcare 2021, 9, 118. [Google Scholar] [CrossRef]
- Carpinello, A.; Vezzetti, E.; Ramieri, G.; Moos, S.; Novaresio, A.; Zavattero, E.; Borbon, C. Evaluation of HMDs by QFD for Augmented Reality Applications in the Maxillofacial Surgery Domain. Appl. Sci. 2021, 11, 11053. [Google Scholar] [CrossRef]
- Wu, I.-C.; Lin, Y.-C.; Yien, H.-W.; Shih, F.-Y. Constructing Constraint-Based Simulation System for Creating Emergency Evacuation Plans: A Case of an Outpatient Chemotherapy Area at a Cancer Medical Center. Healthcare 2020, 8, 137. [Google Scholar] [CrossRef] [PubMed]
- Tlapa, D.; Tortorella, G.; Fogliatto, F.; Kumar, M.; Mac Cawley, A.; Vassolo, R.; Enberg, L.; Baez-Lopez, Y. Effects of Lean Interventions Supported by Digital Technologies on Healthcare Services: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 9018. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.N.; Kim, M.J.; Hwang, W.J. Potential of Augmented Reality and Virtual Reality Technologies to Promote Wellbeing in Older Adults. Appl. Sci. 2019, 9, 3556. [Google Scholar] [CrossRef] [Green Version]
- González, F.C.J.; Villegas, O.O.V.; Ramírez, D.E.T.; Sánchez, V.G.C.; Domínguez, H.O. Smart Multi-Level Tool for Remote Patient Monitoring Based on a Wireless Sensor Network and Mobile Augmented Reality. Sensors 2014, 14, 17212–17234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Berton, A.; Longo, U.G.; Candela, V.; Fioravanti, S.; Giannone, L.; Arcangeli, V.; Alciati, V.; Berton, C.; Facchinetti, G.; Marchetti, A.; et al. Virtual Reality, Augmented Reality, Gamification, and Telerehabilitation: Psychological Impact on Orthopedic Patients’ Rehabilitation. J. Clin. Med. 2020, 9, 2567. [Google Scholar] [CrossRef]
- Obinikpo, A.A.; Kantarci, B. Big Sensed Data Meets Deep Learning for Smarter Health Care in Smart Cities. J. Sens. Actuator Netw. 2017, 6, 26. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Chan, A.P.C.; Shan, M.; Gao, R.; Bao, F.; Lyu, S.; Zhang, Q.; Guan, J. Opportunities and Challenges for Construction Health and Safety Technologies under the COVID-19 Pandemic in Chinese Construction Projects. Int. J. Environ. Res. Public Health 2021, 18, 13038. [Google Scholar] [CrossRef]
- Chang, A.-H.; Lin, P.-C.; Lin, P.-C.; Lin, Y.-C.; Kabasawa, Y.; Lin, C.-Y.; Huang, H.-L. Effectiveness of Virtual Reality-Based Training on Oral Healthcare for Disabled Elderly Persons: A Randomized Controlled Trial. J. Pers. Med. 2022, 12, 218. [Google Scholar] [CrossRef]
- Hatta, M.H.; Sidi, H.; Siew Koon, C.; Che Roos, N.A.; Sharip, S.; Abdul Samad, F.D.; Wan Xi, O.; Das, S.; Mohamed Saini, S. Virtual Reality (VR) Technology for Treatment of Mental Health Problems during COVID-19: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5389. [Google Scholar] [CrossRef]
- Riva, G.; Bernardelli, L.; Castelnuovo, G.; Di Lernia, D.; Tuena, C.; Clementi, A.; Pedroli, E.; Malighetti, C.; Sforza, F.; Wiederhold, B.K.; et al. A Virtual Reality-Based Self-Help Intervention for Dealing with the Psychological Distress Associated with the COVID-19 Lockdown: An Effectiveness Study with a Two-Week Follow-Up. Int. J. Environ. Res. Public Health 2021, 18, 8188. [Google Scholar] [CrossRef]
- Fleming, M.; Olsen, D.; Stathes, H.; Boteler, L.; Grossberg, P.; Pfeifer, J.; Schiro, S.; Banning, J.; Skochelak, S. Virtual Reality Skills Training for Health Care Professionals in Alcohol Screening and Brief Intervention. J. Am. Board Fam. Med. 2009, 22, 387–398. [Google Scholar] [CrossRef] [Green Version]
- Bayahya, A.Y.; Alhalabi, W.; AlAmri, S.H. Smart Health System to Detect Dementia Disorders Using Virtual Reality. Healthcare 2021, 9, 810. [Google Scholar] [CrossRef]
- Leemhuis, E.; Giuffrida, V.; Giannini, A.M.; Pazzaglia, M. A Therapeutic Matrix: Virtual Reality as a Clinical Tool for Spinal Cord Injury-Induced Neuropathic Pain. Brain Sci. 2021, 11, 1201. [Google Scholar] [CrossRef]
- Ahmad, M.A.; Singh, D.K.A.; Mohd Nordin, N.A.; Hooi Nee, K.; Ibrahim, N. Virtual Reality Games as an Adjunct in Improving Upper Limb Function and General Health among Stroke Survivors. Int. J. Environ. Res. Public Health 2019, 16, 5144. [Google Scholar] [CrossRef] [Green Version]
- Sánchez-Herrera-Baeza, P.; Cano-de-la-Cuerda, R.; Oña-Simbaña, E.D.; Palacios-Ceña, D.; Pérez-Corrales, J.; Cuenca-Zaldivar, J.N.; Gueita-Rodriguez, J.; Balaguer-Bernaldo de Quirós, C.; Jardón-Huete, A.; Cuesta-Gomez, A. The Impact of a Novel Immersive Virtual Reality Technology Associated with Serious Games in Parkinson’s Disease Patients on Upper Limb Rehabilitation: A Mixed Methods Intervention Study. Sensors 2020, 20, 2168. [Google Scholar] [CrossRef] [Green Version]
- Riaz, W.; Khan, Z.Y.; Jawaid, A.; Shahid, S. Virtual Reality (VR)-Based Environmental Enrichment in Older Adults with Mild Cognitive Impairment (MCI) and Mild Dementia. Brain Sci. 2021, 11, 1103. [Google Scholar] [CrossRef]
- Léger, M.T.; Mekari, S. Simulating the Benefits of Nature Exposure on Cognitive Performance in Virtual Reality: A Window into Possibilities for Education and Cognitive Health. Brain Sci. 2022, 12, 725. [Google Scholar] [CrossRef]
- Baeza-Barragán, M.R.; Labajos, M.T.; Ruiz, C.; Casuso-Holgado, M.J.; Martín-Valero, R. The Use of Virtual Reality Technologies in the Treatment of Duchenne Muscular Dystrophy: Systematic Review. JMIR Mhealth Uhealth 2020, 8, e21576. [Google Scholar] [CrossRef]
- Mishra, R.; Narayanan, M.D.K.; Umana, G.E.; Montemurro, N.; Chaurasia, B.; Deora, H. Virtual Reality in Neurosurgery: Beyond Neurosurgical Planning. Int. J. Environ. Res. Public Health 2022, 19, 1719. [Google Scholar] [CrossRef]
- Rogers, C.; Lau, J.; Huynh, D.; Albertson, S.; Beem, J.; Qian, E. Capturing the Perceived Phantom Limb through Virtual Reality. Adv. Hum.-Comput. Interact. 2016, 2016, 8608972. [Google Scholar] [CrossRef] [Green Version]
- Lin, A.P.C.; Trappey, C.V.; Luan, C.-C.; Trappey, A.J.C.; Tu, K.L.K. A Test Platform for Managing School Stress Using a Virtual Reality Group Chatbot Counseling System. Appl. Sci. 2021, 11, 9071. [Google Scholar] [CrossRef]
- Zeng, N.; Pope, Z.; Lee, J.E.; Gao, Z. Virtual Reality Exercise for Anxiety and Depression: A Preliminary Review of Current Research in an Emerging Field. J. Clin. Med. 2018, 7, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.-Y.; Lee, J.-H.; Lee, E.-H. Virtual Experience of Perioperative Patients: Walking in the Patients’ Shoes Using Virtual Reality and Blended Learning. Int. J. Environ. Res. Public Health 2021, 18, 6457. [Google Scholar] [CrossRef] [PubMed]
- Pandrangi, V.C.; Gaston, B.; Appelbaum, N.P.; Albuquerque, F.C.; Levy, M.M.; Larson, R.A. The Application of Virtual Reality in Patient Education. Ann. Vasc. Surg. 2019, 59, 184–189. [Google Scholar] [CrossRef]
- Van der Kruk, S.R.; Zielinski, R.; MacDougall, H.; Hughes-Barton, D.; Gunn, K.M. Virtual reality as a patient education tool in healthcare: A scoping review. Patient Educ. Couns. 2022, 105, 1928–1942. [Google Scholar] [CrossRef]
- Sheperd, T.; Trinder, M.; Theophilus, M. Does Virtual Reality in the Perioperative Setting for Patient Education Improve Understanding? A Scoping Review. Surg. Pract. Sci. 2022, 10, 100101. [Google Scholar] [CrossRef]
- Habak, S.; Bennett, J.; Davies, A.; Davies, M.; Christensen, H.; Boydell, K.M. Edge of the Present: A Virtual Reality Tool to Cultivate Future Thinking, Positive Mood and Wellbeing. Int. J. Environ. Res. Public Health 2021, 18, 140. [Google Scholar] [CrossRef]
- Lim, S.-G.; Jung, S.-H.; Huh, J.-H. Visual Algorithm of VR E-Sports for Online Health Care. Healthcare 2021, 9, 824. [Google Scholar] [CrossRef]
- Dębska, M.; Polechoński, J.; Mynarski, A.; Polechoński, P. Enjoyment and Intensity of Physical Activity in Immersive Virtual Reality Performed on Innovative Training Devices in Compliance with Recommendations for Health. Int. J. Environ. Res. Public Health 2019, 16, 3673. [Google Scholar] [CrossRef] [Green Version]
- Hughes, S.; Warren-Norton, K.; Spadafora, P.; Tsotsos, L.E. Supporting Optimal Aging through the Innovative Use of Virtual Reality Technology. Multimodal Technol. Interact. 2017, 1, 23. [Google Scholar] [CrossRef] [Green Version]
- Montana, J.I.; Matamala-Gomez, M.; Maisto, M.; Mavrodiev, P.A.; Cavalera, C.M.; Diana, B.; Mantovani, F.; Realdon, O. The Benefits of emotion Regulation Interventions in Virtual Reality for the Improvement of Wellbeing in Adults and Older Adults: A Systematic Review. J. Clin. Med. 2020, 9, 500. [Google Scholar] [CrossRef] [Green Version]
- Nobari, H.; Rezaei, S.; Sheikh, M.; Fuentes-García, J.P.; Pérez-Gómez, J. Effect of Virtual Reality Exercises on the Cognitive Status and Dual Motor Task Performance of the Aging Population. Int. J. Environ. Res. Public Health 2021, 18, 8005. [Google Scholar] [CrossRef]
- Nichols, S.; Patel, H. Health and Safety Implications of Virtual Reality: A Review of Empirical Evidence. Appl. Ergon. 2002, 33, 251–271. [Google Scholar] [CrossRef]
- Behm-Morawitz, E. Mirrored selves: The Influence of Self-Presence in a Virtual World on Health, Appearance, and Well-Being. Comput. Hum. Behav. 2013, 29, 119–128. [Google Scholar] [CrossRef]
- Gourlay, D.; Lun, K.C.; Liya, G. Virtual Reality and Telemedicine for Home Health Care. Comput. Graph. 2000, 24, 695–699. [Google Scholar] [CrossRef]
- Brown-Johnson, C.G.; Berrean, B.; Cataldo, J.K. Development and Usability Evaluation of the mHealth Tool for Lung Cancer (mHealth TLC): A Virtual World Health Game for Lung Cancer Patients. Patient Educ. Couns. 2015, 98, 506–511. [Google Scholar] [CrossRef] [Green Version]
- Liu, Z.; Yang, Z.; Xiao, C.; Zhang, K.; Osmani, M. An Investigation into Art Therapy Aided Health and Well-Being Research: A 75-Year Bibliometric Analysis. Int. J. Environ. Res. Public Health 2022, 19, 232. [Google Scholar] [CrossRef]
- Mantovani, F.; Castelnuovo, G.; Gaggioli, A.; Riva, G. Virtual Reality Training for Health-Care Professionals. CyberPsychology Behav. 2003, 6, 389–395. [Google Scholar] [CrossRef]
- Patterson, D.R.; Drever, S.; Soltani, M.; Sharar, S.R.; Wiechman, S.; Meyer, W.J.; Hoffman, H.G. A Comparison of Interactive Immersive Virtual Reality and Still Nature Pictures as Distraction-Based Analgesia in Burn Wound Care. Burns, 2022; in press. [Google Scholar] [CrossRef]
- O’Connor, M.; Stowe, J.; Potocnik, J.; Giannotti, N.; Murphy, S.; Rainford, L. 3D Virtual Reality Simulation in Radiography Education: The Students’ Experience. Radiography 2020, 27, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Partner, A.; Shiner, N.; Hyde, E.; Errett, S. First Year Student Radiographers’ Perceptions of a One-Week Simulation-Based Education Package Designed to Increase Clinical Placement Capacity. Radiography 2022, 28, 577–585. [Google Scholar] [CrossRef] [PubMed]
- Sapkaroski, D.; Mundy, M.; Dimmock, M.R. Virtual Reality versus Conventional Clinical Role-Play for Radiographic Positioning Training: A Students’ Perception Study. Radiography 2020, 26, 57–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viglialoro, R.M.; Condino, S.; Turini, G.; Carbone, M.; Ferrari, V.; Gesi, M. Augmented Reality, Mixed Reality, and Hybrid Approach in Healthcare Simulation: A Systematic Review. Appl. Sci. 2021, 11, 2338. [Google Scholar] [CrossRef]
- Birckhead, B.; Khalil, C.; Liu, X.; Conovitz, S.; Rizzo, A.; Danovitch, I.; Bullock, K.; Spiegel, B. Recommendations for Methodology of Virtual Reality Clinical Trials in Health Care by an International Working Group: Iterative Study. JMIR Ment Health 2019, 6, e11973. [Google Scholar] [CrossRef] [Green Version]
- Balian, S.; McGovern, S.K.; Abella, B.S.; Blewer, A.L.; Leary, M. Feasibility of an Augmented Reality Cardiopulmonary Resuscitation Training System for Health Care Providers. Heliyon 2019, 5, e02205. [Google Scholar] [CrossRef]
- Carlson, K.J.; Gagnon, D.J. Augmented Reality Integrated Simulation Education in Health Care. Clin. Simul. Nurs. 2016, 12, 123–127. [Google Scholar] [CrossRef]
- Hirt, J.; Beer, T. Use and Impact of Virtual Reality Simulation in Dementia Care Education: A Scoping Review. Nurse Educ. Today 2020, 84, 104207. [Google Scholar] [CrossRef]
- Shorey, S.; Debby, E. The Use of Virtual Reality Simulation among Nursing Students and Registered Nurses: A Systematic Review. Nurse Educ. Today 2020, 98, 104662. [Google Scholar] [CrossRef]
- McCarthy, C.J.; Uppot, R.N. Advances in Virtual and Augmented Reality—Exploring the Role in Health-care Education. J. Radiol. Nurs. 2019, 38, 104–105. [Google Scholar] [CrossRef]
- Liaw, S.Y.; Wu, L.T.; Soh, S.L.H.; Ringsted, C.; Lau, T.C.; Lim, W.S. Virtual Reality Simulation in Interprofessional Round Training for Health Care Students: A Qualitative Evaluation Study. Clin. Simul. Nurs. 2020, 45, 42–46. [Google Scholar] [CrossRef]
- Plotzky, C.; Lindwedel, U.; Sorber, M.; Loessl, B.; König, P.; Kunze, C.; Kugler, C.; Meng, M. Virtual Reality Simulations in Nurse Education: A Systematic Mapping Review. Nurse Educ. Today 2021, 101, 104868. [Google Scholar] [CrossRef]
- Bayram, S.B.; Caliskan, N. Effect of a Game-Based Virtual Reality Phone Application on Tracheostomy Care Education for Nursing Students: A Randomized Controlled Trial. Nurse Educ. Today 2019, 79, 25–31. [Google Scholar] [CrossRef]
- Park, J.-S.; Jung, Y.-J.; Lee, G. Virtual Reality-Based Cognitive–Motor Rehabilitation in Older Adults with Mild Cognitive Impairment: A Randomized Controlled Study on Motivation and Cognitive Function. Healthcare 2020, 8, 335. [Google Scholar] [CrossRef]
- Gachet Páez, D.; Aparicio, F.; De Buenaga, M.; Padrón, V. Personalized Health Care System with Virtual Reality Rehabilitation and Appropriate Information for Seniors. Sensors 2012, 12, 5502–5516. [Google Scholar] [CrossRef] [Green Version]
- Varela-Aldás, J.; Buele, J.; Ramos Lorente, P.; García-Magariño, I.; Palacios-Navarro, G. A Virtual Reality-Based Cognitive Telerehabilitation System for Use in the COVID-19 Pandemic. Sustainability 2021, 13, 2183. [Google Scholar] [CrossRef]
- Aloyuni, S.; Alharbi, R.; Kashoo, F.; Alqahtani, M.; Alanazi, A.; Alzhrani, M.; Ahmad, M. Knowledge, Attitude, and Barriers to Telerehabilitation-Based Physical Therapy Practice in Saudi Arabia. Healthcare 2020, 8, 460. [Google Scholar] [CrossRef]
- Norouzi-Gheidari, N.; Hernandez, A.; Archambault, P.S.; Higgins, J.; Poissant, L.; Kairy, D. Feasibility, Safety and Efficacy of a Virtual Reality Exergame System to Supplement Upper Extremity Rehabilitation Post-Stroke: A Pilot Randomized Clinical Trial and Proof of Principle. Int. J. Environ. Res. Public Health 2020, 17, 113. [Google Scholar] [CrossRef] [Green Version]
- Demolder, C.; Molina, A.; Hammond, F.L.; Yeo, W.-H. Recent Advances in Wearable Biosensing Gloves and Sensory Feedback Biosystems for Enhancing Rehabilitation, Prostheses, Healthcare, and Virtual Reality. Biosens. Bioelectron. 2021, 190, 113443. [Google Scholar] [CrossRef]
- Hwang, N.-K.; Shim, S.-H. Use of Virtual Reality Technology to Support the Home Modification Process: A Scoping Review. Int. J. Environ. Res. Public Health 2021, 18, 11096. [Google Scholar] [CrossRef]
- Kim, S.-H.; Kim, H.J.; Shin, G. Self-Management Mobile Virtual Reality Program for Women with Gestational Diabetes. Int. J. Environ. Res. Public Health 2021, 18, 1539. [Google Scholar] [CrossRef] [PubMed]
- Won, A.S.; Bailey, J.; Bailenson, J.; Tataru, C.; Yoon, I.A.; Golianu, B. Immersive Virtual Reality for Pediatric Pain. Children 2017, 4, 52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klas, J.; Grzywacz, A.; Kulszo, K.; Grunwald, A.; Kluz, N.; Makaryczew, M.; Samardakiewicz, M. Challenges in the Medical and Psychosocial Care of the Paediatric Refugee—A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 10656. [Google Scholar] [CrossRef] [PubMed]
- Antón-Sancho, Á.; Fernández-Arias, P.; Vergara, D. Assessment of Virtual Reality among University Professors: Influence of the Digital Generation. Computers 2022, 11, 92. [Google Scholar] [CrossRef]
- Noghabaei, M.; Heydarian, A.; Balali, V.; Han, K. Trend Analysis on Adoption of Virtual and Augmented Reality in the Architecture, Engineering, and Construction Industry. Data 2020, 5, 26. [Google Scholar] [CrossRef] [Green Version]
- Wang, P.; Wu, P.; Wang, J.; Chi, H.-L.; Wang, X. A Critical Review of the Use of Virtual Reality in Construction Engineering Education and Training. Int. J. Environ. Res. Public Health 2018, 15, 1204. [Google Scholar] [CrossRef] [Green Version]
- Moro, C.; McLean, M. Supporting Students’ Transition to University and Problem-Based Learning. Med. Sci. Educ. 2017, 27, 353–361. [Google Scholar] [CrossRef]
- Vergara-Rodríguez, D.; Antón-Sancho, Á.; Fernández-Arias, P. Variables Influencing Professors’ Adaptation to Digital Learning Environments during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 3732. [Google Scholar] [CrossRef]
- Kasurinen, J. Usability Issues of Virtual Reality Learning Simulator in Healthcare and Cybersecurity. Procedia Comput. Sci. 2017, 119, 341–349. [Google Scholar] [CrossRef]
- Castiblanco, I.A.; Cepeda, L.C.; Violante, M.G.; Marcolin, F.; Vezzetti, E. Commonly Used External TAM Variables in e-Learning, Agriculture and Virtual Reality Applications. Future Internet 2021, 13, 7. [Google Scholar] [CrossRef]
- Kovacevic, A.; Bär, S.; Starystach, S.; Elsässer, M.; van der Locht, T.; Mohammadi Motlagh, A.; Ostermayer, E.; Oberhoffer-Fritz, R.; Ewert, P.; Gorenflo, M.; et al. Fetal Cardiac Services during the COVID-19 Pandemic: How Does It Affect Parental Counseling? J. Clin. Med. 2021, 10, 3423. [Google Scholar] [CrossRef]
- Fernández-Arias, P.; Antón-Sancho, Á.; Vergara, D.; Barrientos, A. Soft Skills of American University Teachers: Self-Concept. Sustainability 2021, 13, 12397. [Google Scholar] [CrossRef]
- Gillespie, G.L.; Farra, S.; Regan, S.L.; Brammer, S.V. Impact of Immersive Virtual Reality Simulations for Changing Knowledge, Attitudes, And Behaviors. Nurse Educ. Today 2021, 105, 105025. [Google Scholar] [CrossRef]
- Qiao, J.; Xu, J.; Li, L.; Ouyang, Y.-Q. The Integration of Immersive Virtual Reality Simulation in Interprofessional Education: A Scoping Review. Nurse Educ. Today 2021, 98, 104773. [Google Scholar] [CrossRef]
- Riva, G. Virtual Reality for Health Care: The Status of Research. CyberPsychology Behav. 2002, 5, 219–225. [Google Scholar] [CrossRef]
- Birt, J.; Stromberga, Z.; Cowling, M.; Moro, C. Mobile Mixed Reality for Experiential Learning and Simulation in Medical and Health Sciences Education. Information 2018, 9, 31. [Google Scholar] [CrossRef] [Green Version]
- Liaw, S.Y.; Ooi, S.L.; Mildon, R.; Ang, E.N.K.; Lau, T.C.; Chua, W.L. Translation of an Evidence-Based Virtual Reality Simulation-Based Interprofessional Education into Health Education Curriculums: An Implementation Science Method. Nurse Educ. Today 2022, 110, 105262. [Google Scholar] [CrossRef]
- Kamińska, D.; Sapiński, T.; Wiak, S.; Tikk, T.; Haamer, R.E.; Avots, E.; Helmi, A.; Ozcinar, C.; Anbarjafari, G. Virtual Reality and Its Applications in Education: Survey. Information 2019, 10, 318. [Google Scholar] [CrossRef] [Green Version]
- Chen, F.; Leng, Y.; Ge, J.; Wang, D.; Li, C.; Chen, B.; Sun, Z. Effectiveness of Virtual Reality in Nursing Education: Meta-Analysis. J. Med. Internet Res. 2020, 22, e18290. [Google Scholar] [CrossRef]
- Kyaw, B.M.; Saxena, N.; Posadzki, P.; Vseteckova, J.; Nikolaou, C.K.; George, P.P.; Divakar, U.; Masiello, I.; Kononowicz, A.A.; Zary, N.; et al. Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12959. [Google Scholar] [CrossRef] [Green Version]
- Mäkinen, H.; Haavisto, E.; Havola, S.; Koivisto, J.-M. User Experiences of Virtual Reality Technologies for Healthcare in Learning: An Integrative Review. Behav. Inf. Technol. 2022, 41, 1–17. [Google Scholar] [CrossRef]
- King, D.; Tee, S.; Falconer, L.; Angell, C.; Holley, D.; Mills, A. Virtual Health Education: Scaling Practice to Transform Student Learning: Using Virtual Reality Learning Environments in Healthcare Education to Bridge the Theory/Practice Gap and Improve Patient Safety. Nurse Educ. Today 2018, 71, 7–9. [Google Scholar] [CrossRef] [PubMed]
- López-Chávez, O.; Rodríguez, L.-F.; Gutierrez-Garcia, J.-O. A Comparative Case Study of 2D, 3D and Immersive-Virtual-Reality Applications for Healthcare Education. Int. J. Med. Inform. 2020, 141, 104226. [Google Scholar] [CrossRef] [PubMed]
- Nakai, K.; Terada, S.; Takahara, A.; Hage, D.; Tubbs, R.S.; Iwanaga, J. Anatomy Education for Medical Students in a Virtual Reality Workspace: A Pilot Study. Clin. Anat. 2022, 35, 40–44. [Google Scholar] [CrossRef] [PubMed]
- Jung, Y. Virtual Reality Simulation for Disaster Preparedness Training in Hospitals: Integrated Review. J. Med. Internet Res. 2022, 24, e30600. [Google Scholar] [CrossRef]
- Touloudi, E.; Hassandra, M.; Galanis, E.; Goudas, M.; Theodorakis, Y. Applicability of an Immersive Virtual Reality Exercise Training System for Office Workers during Working Hours. Sports 2022, 10, 104. [Google Scholar] [CrossRef]
- Alam, F.; Matava, C. A New Virtual World? The Future of Immersive Environments in Anesthesiology. Anesth. Analg. 2022, 135, 230–238. [Google Scholar] [CrossRef]
- Gasteiger, N.; Van-der-Veer, S.N.; Wilson, P.; Dowding, D. How, for Whom, and in Which Contexts or Conditions Augmented and Virtual Reality Training Works in Upskilling Health Care Workers: Realist Synthesis. JMIR Serious Games 2022, 10, e31644. [Google Scholar] [CrossRef]
- Jiang, H.; Vimalesvaran, S.; Wang, J.K.; Lim, K.B.; Mogali, S.R.; Car, L.T. Virtual Reality in Medical Students’ Education: Scoping Review. JMIR Med. Educ. 2022, 8, e34860. [Google Scholar] [CrossRef]
- Spreij, L.A.; Visser-Meily, J.M.A.; Sibbel, J.; Gosselt, I.K.; Nijboer, T.C.W. Feasibility and User-Experience of Virtual Reality in Neuropsychological Assessment Following Stroke. Neuropsychol. Rehabil. 2022, 32, 499–519. [Google Scholar] [CrossRef]
- Pardini, S.; Gabrielli, S.; Dianti, M.; Novara, C.; Zucco, G.M.; Mich, O.; Forti, S. The Role of Personalization in the User Experience, Preferences and Engagement with Virtual Reality Environments for Relaxation. Int. J. Environ. Res. Public Health 2022, 19, 7237. [Google Scholar] [CrossRef]
- Saxena, N.; Kyaw, B.M.; Vseteckova, J.; Dev, P.; Paul, P.; Lim, K.T.K.; Kononowicz, A.A.; Masiello, I.; Tudor-Car, L.; Nikolaou, C.K.; et al. Virtual Reality Environments for Health Professional Education. Cochrane Database Syst. Rev. 2018, 2, CD012090. [Google Scholar] [CrossRef]
- Vergara, D.; Antón-Sancho, Á.; Extremera, J.; Fernández-Arias, P. Assessment of Virtual Reality as a Didactic Resource in Higher Education. Sustainability 2021, 13, 12730. [Google Scholar] [CrossRef]
- Hsin, L.J.; Chao, Y.P.; Chuang, H.H.; Kuo, T.B.J.; Yang, C.C.H.; Huang, C.-G.; Kang, C.J.; Lin, W.-N.; Fang, T.-J.; Li, H.-Y.; et al. Mild Simulator Sickness Can Alter Heart Rate Variability, Mental Workload, and Learning Outcomes in a 360° Virtual Reality Application for Medical Education: A Post Hoc Analysis of a Randomized Controlled Trial. Virtual Real. 2022. [Google Scholar] [CrossRef]
- Chao, Y.P.; Kang, C.J.; Chuang, H.H.; Hsieh, M.-J.; Chang, Y.-C.; Kuo, T.B.J.; Yang, C.C.H.; Huang, C.-G.; Fang, T.-J.; Li, H.-Y.; et al. Comparison of the Effect of 360° versus Two-Dimensional Virtual Reality Video on History Taking and Physical Examination Skills Learning among Undergraduate Medical Students: A Randomized Controlled Trial. Virtual Real. 2022. [Google Scholar] [CrossRef]
- Muñoz, E.G.; Fabregat, R.; Bacca-Acosta, J.; Duque-Méndez, N.; Avila-Garzon, C. Augmented Reality, Virtual Reality, and Game Technologies in Ophthalmology Training. Information 2022, 13, 222. [Google Scholar] [CrossRef]
- Ojala, S.; Sirola, J.; Nykopp, T.; Kröger, H.; Nuutinen, H. The Impact of Teacher’s Presence on Learning Basic Surgical Tasks with Virtual Reality Headset among Medical Students. Med. Educ. Online 2022, 27, 2050345. [Google Scholar] [CrossRef]
- Saab, M.M.; Landers, M.; Murphy, D.; O’Mahony, B.; Cooke, E.; O’Driscoll, M.; Hegarty, J. Nursing Students’ Views of Using Virtual Reality in Healthcare: A Qualitative Study. J. Clin. Nurs. 2022, 31, 1228–1242. [Google Scholar] [CrossRef]
- Chang, C.-Y.; Sung, H.-Y.; Guo, J.-L.; Chang, B.-Y.; Kuo, F.-R. Effects of Spherical Video-Based Virtual Reality on Nursing Students’ Learning Performance in Childbirth Education Training. Interact. Learn. Environ. 2022, 30, 400–416. [Google Scholar] [CrossRef]
- Behmadi, S.; Asadi, F.; Okhovati, M.; Ershad-Sarabi, R. Virtual Reality-Based Medical Education Versus Lecture-Based Method in Teaching Start Triage Lessons in Emergency Medical Students: Virtual Reality in Medical Education. J. Adv. Med. Educ. Prof. 2022, 10, 48–53. [Google Scholar] [CrossRef]
- Dincelli, E.; Yayla, A. Immersive Virtual Reality in the Age of the Metaverse: A Hybrid-Narrative Review Based on the Technology Affordance Perspective. J. Strateg. Inform. Syst. 2022, 31, 101717. [Google Scholar] [CrossRef]
- Yu, M.; Yang, M.R. Effectiveness and Utility of Virtual Reality Infection Control Simulation for Children with COVID-19: Quasi-Experimental Study. JMIR Serious Games 2022, 10, e36707. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Car, L.; Poon, S.; Kyaw, B.M.; Cook, D.A.; Ward, V.; Atun, R.; Majeed, A.; Johnston, J.; Van-der-Kleij, R.M.J.J.; Molokhia, M.V.; et al. Digital Education for Health Professionals: An Evidence Map, Conceptual Framework, and Research Agenda. J. Med. Internet Res. 2022, 24, e31977. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Poyato, M.J.; Eito-Mateo, A.; Mira-Tamayo, D.C.; Matías-Solanilla, A. Digital Skills, ICTs and Students’ Needs: A Case Study in Social Work Degree, University of Zaragoza (Aragón-Spain). Educ. Sci. 2022, 12, 443. [Google Scholar] [CrossRef]
- Vergara, D.; Antón-Sancho, A.; Dávila, L.P.; Fernández-Arias, P. Virtual Reality as a Didactic Resource from the Perspective of Engineering Teachers. Comput. Appl. Eng. Educ. 2022, 30, 1086–1101. [Google Scholar] [CrossRef]
- Antón-Sancho, Á.; Sánchez-Calvo, M. Influence of Knowledge Area on the Use of Digital Tools during the COVID-19 Pandemic among Latin American Professors. Educ. Sci. 2022, 12, 635. [Google Scholar] [CrossRef]
- Kröplin, J.; Huber, T.; Geis, C.; Braun, B.; Fritz, T. eSurgery—Digital Transformation in Surgery, Surgical Education and Training: Survey Analysis of the Status Quo in Germany. Eur. Surg. 2022, 54, 249–258. [Google Scholar] [CrossRef]
- Whewell, E.; Caldwell, H.; Frydenberg, M.; Andone, D. Changemakers as Digital Makers: Connecting and Co-Creating. Educ. Inf. Technol. 2022, 27, 6691–6713. [Google Scholar] [CrossRef]
- Pottle, J. Virtual Reality and the Transformation of Medical Education. Future Health J. 2019, 6, 181–185. [Google Scholar] [CrossRef]
- Basco, A.I.; Lavena, C. Competencias y Habilidades Para la Cuarta Revolución Industrial en El Contexto de Pandemia; Inter-American Development Bank (IDB): Washington, DC, USA, 2021. [Google Scholar] [CrossRef]
- Curioso, W.H. Building Capacity and Training for Digital Health: Challenges and Opportunities in Latin America. J. Med. Internet Res. 2019, 21, e16513. [Google Scholar] [CrossRef]
- Luo, X.; Wu, W.; Zúñiga-Cañón, C.; Lozano-Garzón, C. From Great Wall to the Andes: Sino-Latin America Collaborations on Urban Computing, Virtual Reality, and Visualization Research. In Proceedings of the 2016 International Conference on Virtual Reality and Visualization (ICVRV), Hangzhou, China, 24–26 September 2016; pp. 346–349. [Google Scholar] [CrossRef]
- Medina-Romero, M.A. Legal Framework for Hasty Digitization in Educational Institutions of Latin American Countries during the COVID-19 Epidemic. J. Posit. Sch. Psychol. 2022, 6, 5392–5404. [Google Scholar] [CrossRef]
- Rodríguez-Abitia, G.; Martínez-Pérez, S.; Ramirez-Montoya, M.S.; Lopez-Caudana, E. Digital Gap in Universities and Challenges for Quality Education: A Diagnostic Study in Mexico and Spain. Sustainability 2020, 12, 9069. [Google Scholar] [CrossRef]
- Antón-Sancho, Á.; Vergara, D.; Lamas-Álvarez, V.E.; Fernández-Arias, P. Digital Content Creation Tools: American University Teachers’ Perception. Appl. Sci. 2021, 11, 11649. [Google Scholar] [CrossRef]
- Rama, C. University Virtualisation in Latin America. Int. J. Educ. Technol. High. Educ. 2014, 11, 32–41. [Google Scholar] [CrossRef] [Green Version]
- Vergara, D.; Antón-Sancho, A.; Fernández-Arias, P. Player Profiles for Game-Based Applications in Engineering Education. Comput. Appl. Eng. Educ. 2022. [Google Scholar] [CrossRef]
- UNESCO Institute for Statistics. International Standard Classification of Education ISCED 2011; UNESCO-UIS: Montreal, QC, Canada, 2012; Available online: http://uis.unesco.org/sites/default/files/documents/international-standard-classification-of-education-isced-2011-en.pdf (accessed on 23 October 2022).
- Streiner, D.L. Starting at the Beginning: An Introduction to Coefficient Alpha and Internal Consistency. J. Pers. Med. 2003, 80, 99–103. [Google Scholar] [CrossRef]
- Schmitt, T.A. Current Methodological Considerations in Exploratory and Confirmatory Factor Analysis. J. Psychoeduc. Assess. 2011, 29, 304–321. [Google Scholar] [CrossRef]
- Antón-Sancho, Á.; Vergara, D.; Fernández-Arias, P.; Ariza-Echeverri, E.A. Didactic Use of Virtual Reality in Colombian Universities: Professors’ Perspective. Multimodal Technol. Interact. 2022, 6, 38. [Google Scholar] [CrossRef]


| Factor | Cronbach’s Alpha |
|---|---|
| Competence | 0.7799 |
| Technical aspects | 0.8537 |
| Usability of VR | 0.7923 |
| Disadvantages | 0.7915 |
| Future | 0.8032 |
| Didactic usefulness of VR | 0.8121 |
| Factor | Mean (Out of 5) | Std. Deviation (Out of 5) | Coefficient of Variation (%) | Skewness |
|---|---|---|---|---|
| Competence | 2.60 | 1.13 | 43.46 | 0.15 |
| Technical aspects | 3.94 | 0.98 | 24.83 | −0.69 |
| Usability of VR | 4.16 | 0.90 | 21.54 | −1.13 |
| Disadvantages | 3.60 | 1.24 | 34.48 | −0.46 |
| Future | 3.89 | 0.91 | 23.39 | −0.40 |
| Didactic usefulness of VR | 4.07 | 0.99 | 24.39 | −0.89 |
| Competence | Technical | Usability | Disadvantages | Future | Didactic | |
|---|---|---|---|---|---|---|
| Competence | 1 | −0.12 | 0.15 | 0.15 | 0.06 | 0.26 |
| Technical | 1 | 0.58 | 0.03 | 0.13 | 0.20 | |
| Usability | 1 | 0.14 | 0.09 | 0.34 | ||
| Disadvantages | 1 | 0.05 | 0.36 | |||
| Future | 1 | 0.17 | ||||
| Didactic | 1 |
| Mean Private (Out of 5) | Mean Public (Out of 5) | t | p-Value | |
|---|---|---|---|---|
| Competence | 2.57 | 2.63 | −0.7281 | 0.4667 |
| Technical | 3.98 | 3.89 | 0.9414 | 0.3468 |
| Usability | 4.19 | 4.13 | 1.3267 | 0.1850 |
| Disadvantages | 3.61 | 3.59 | 0.3721 | 0.7099 |
| Future | 3.80 | 3.99 | −2.4982 | 0.0128 * |
| Didactic | 4.13 | 4.01 | 2.4112 | 0.0160 * |
| Private | Public | MANOVA F | MANOVA p-Value | |||
|---|---|---|---|---|---|---|
| Female | Male | Female | Male | |||
| Competence | 2.58 | 2.54 | 2.40 | 3.02 | 15.3584 | 0.0001 * |
| Technical | 4.10 | 3.67 | 4.02 | 3.67 | 0.2683 | 0.6046 |
| Usability | 4.27 | 3.98 | 4.12 | 4.15 | 5.1734 | 0.0232 * |
| Disadvantages | 3.57 | 3.74 | 3.75 | 3.31 | 17.5445 | <0.0001 * |
| Future | 3.80 | 3.80 | 3.93 | 4.10 | 1.0393 | 0.3085 |
| Didactic | 4.16 | 4.05 | 4.06 | 3.92 | 0.1168 | 0.7325 |
| Variable | Estimate | Std. Error | F-Statistic | p-Value | |
|---|---|---|---|---|---|
| Competence | Slope | 0.0064 | 0.0050 | 1.6610 | 0.1982 |
| Independent term | 2.2723 | 0.2364 | |||
| Technical aspects | Slope | −0.0040 | 0.0042 | 0.9415 | 0.3325 |
| Independent term | 4.1717 | 0.1988 | |||
| Usability of VR | Slope | −0.0019 | 0.0040 | 0.2194 | 0.6397 |
| Independent term | 4.2778 | 0.1887 | |||
| Disadvantages | Slope | −0.0061 | 0.0043 | 2.0580 | 0.1519 |
| Independent term | 3.8957 | 0.2031 | |||
| Future | Slope | 0.0012 | 0.0054 | 0.0486 | 0.8256 |
| Independent term | 3.7426 | 0.2566 | |||
| Didactic usefulness | Slope | 0.0070 | 0.0030 | 5.5980 | 0.0182 * |
| Independent term | 3.8011 | 0.1414 |
| Variable | Estimate | Std. Error | F-Statistic | p-Value | |
|---|---|---|---|---|---|
| Competence | Slope | −0.0086 | 0.0065 | 1.7670 | 0.1845 |
| Independent term | 3.0931 | 0.3552 | |||
| Technical aspects | Slope | 0.0215 | 0.0056 | 14.6100 | 0.0002 * |
| Independent term | 2.7241 | 0.3100 | |||
| Usability of VR | Slope | 0.0112 | 0.0051 | 4.8020 | 0.0290 * |
| Independent term | 3.5268 | 0.2802 | |||
| Disadvantages | Slope | 0.0126 | 0.0054 | 5.3580 | 0.0209 * |
| Independent term | 2.9027 | 0.2997 | |||
| Future | Slope | 0.0073 | 0.0057 | 1.2720 | 0.2050 |
| Independent term | 3.5969 | 0.3158 | |||
| Didactic usefulness | Slope | 0.0018 | 0.0041 | 0.1907 | 0.6620 |
| Independent term | 3.9100 | 0.2272 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Antón-Sancho, Á.; Fernández-Arias, P.; Vergara, D. Virtual Reality in Health Science Education: Professors’ Perceptions. Multimodal Technol. Interact. 2022, 6, 110. https://doi.org/10.3390/mti6120110
Antón-Sancho Á, Fernández-Arias P, Vergara D. Virtual Reality in Health Science Education: Professors’ Perceptions. Multimodal Technologies and Interaction. 2022; 6(12):110. https://doi.org/10.3390/mti6120110
Chicago/Turabian StyleAntón-Sancho, Álvaro, Pablo Fernández-Arias, and Diego Vergara. 2022. "Virtual Reality in Health Science Education: Professors’ Perceptions" Multimodal Technologies and Interaction 6, no. 12: 110. https://doi.org/10.3390/mti6120110
APA StyleAntón-Sancho, Á., Fernández-Arias, P., & Vergara, D. (2022). Virtual Reality in Health Science Education: Professors’ Perceptions. Multimodal Technologies and Interaction, 6(12), 110. https://doi.org/10.3390/mti6120110