Dengue Infections in Colombia: Epidemiological Trends of a Hyperendemic Country
Abstract
:1. Introduction
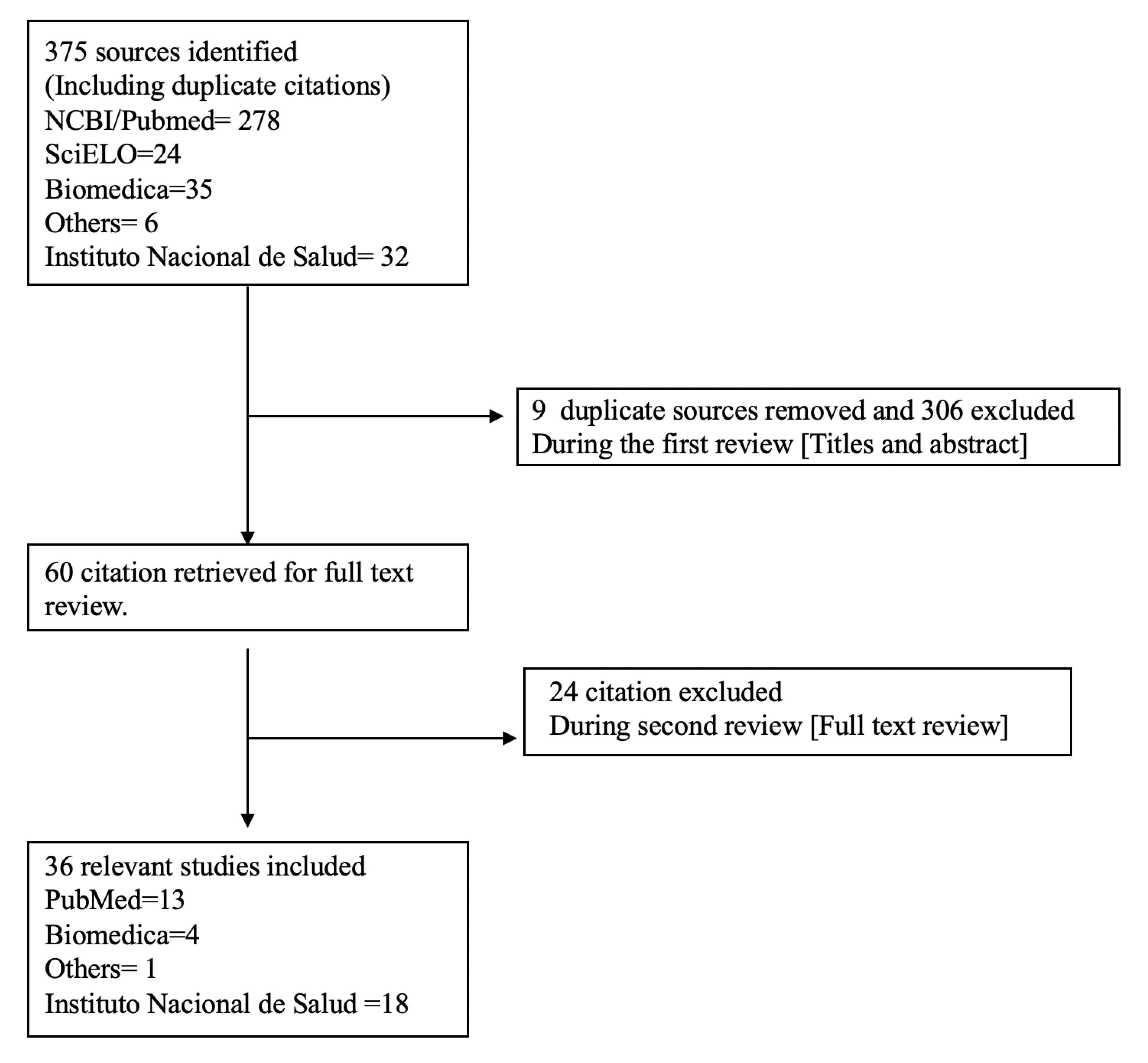
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Outcome Measure
3. Results
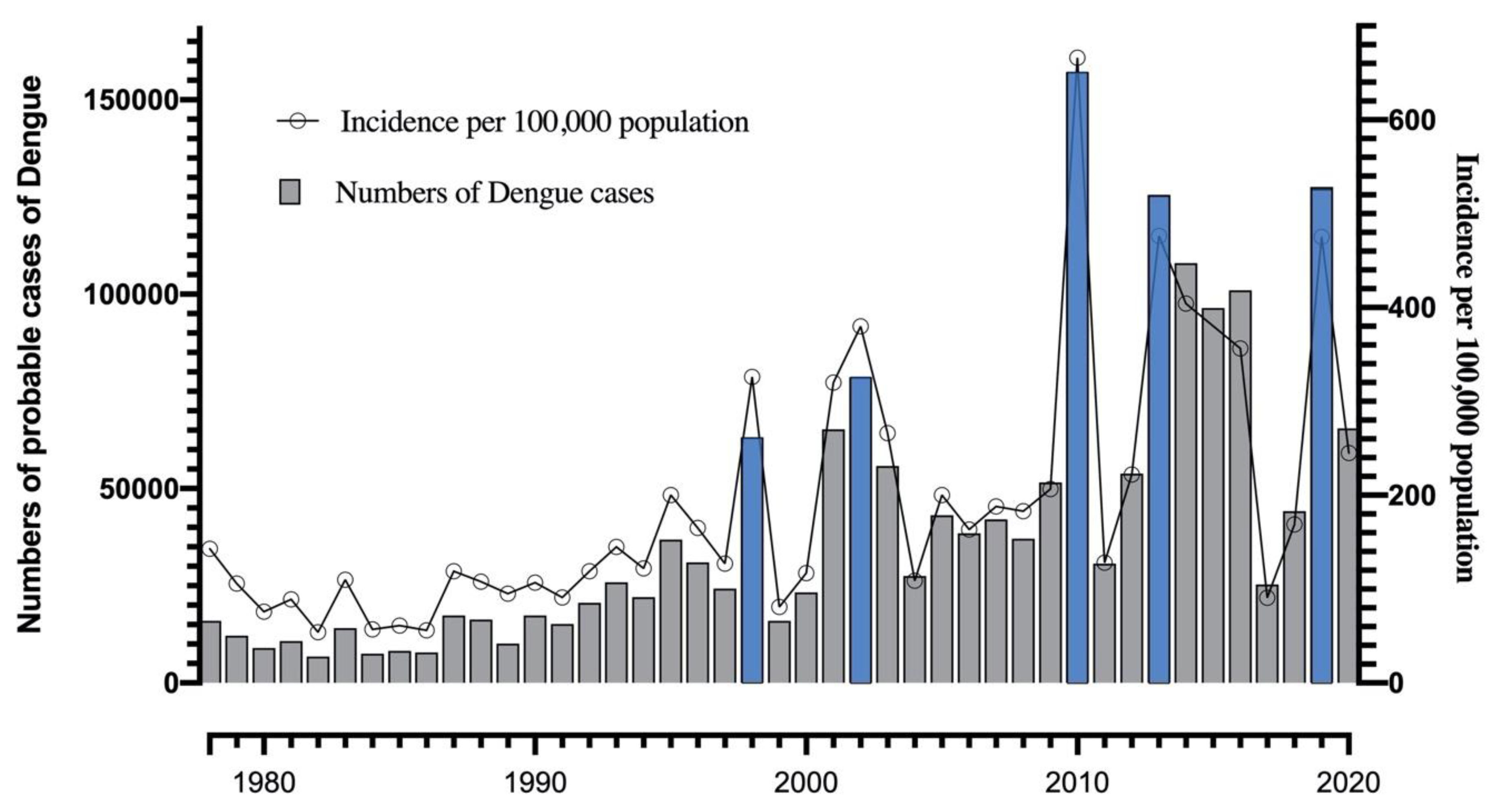
3.1. Epidemiology of Dengue in Colombia: Historical Dengue Outbreaks
3.2. Case Fatality Rate of Dengue in Colombia
3.3. Case Fatality Rate of Severe Dengue in Colombia
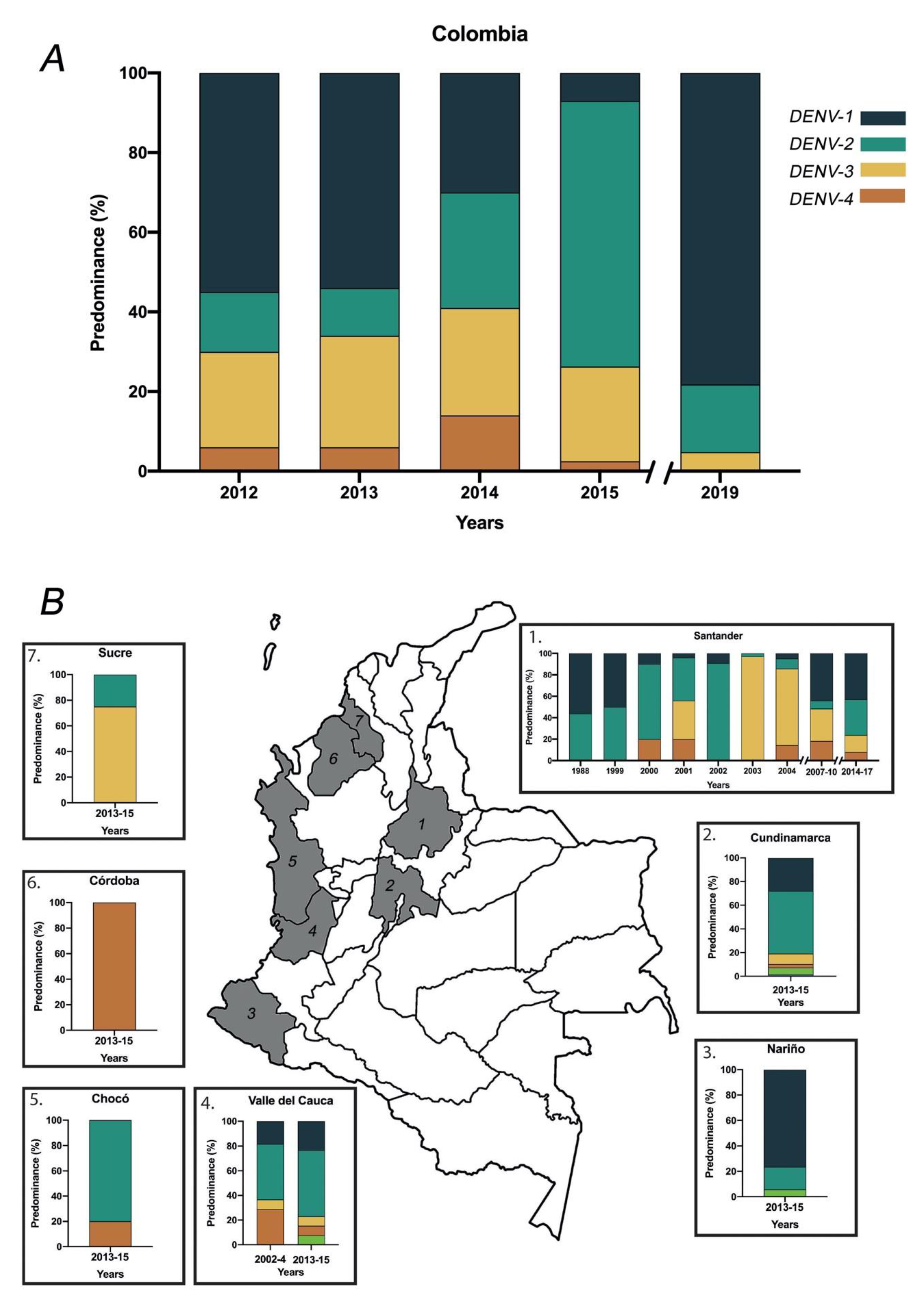
3.4. Dengue Virus Serotypes Distribution in Colombia
3.5. Regional Epidemiology of Dengue during the Predominant Outbreaks
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bhatt, S.; Gething, P.; Brady, O.J.; Messina, J.P.; Farlow, A.W.; Moyes, C.L.; Drake, J.M.; Brownstein, J.S.; Hoen, A.G.; Sankoh, O.; et al. The Global Distribution and Burden of Dengue. Nature 2013, 496, 504–507. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, M.U.; E Sinka, M.; A Duda, K.; Mylne, A.Q.; Shearer, F.M.; Barker, C.M.; Moore, C.G.; Carvalho, R.G.; E Coelho, G.; Van Bortel, W.; et al. The Global Distribution of the Arbovirus Vectors Aedes Aegypti and Ae. Albopictus. eLife 2015, 4, e08347. [Google Scholar] [CrossRef] [PubMed]
- Katzelnick, L.C.; Fonville, J.M.; Gromowski, G.D.; Bustos-Arriaga, J.; Green, A.; James, S.; Lau, L.; Montoya, M.; Wang, C.; VanBlargan, L.A.; et al. Dengue Viruses Cluster Antigenically but not as Discrete Serotypes. Science 2015, 349, 1338–1343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization. Dengue Guidelines for Diagnosis, Treatment, Prevention and Control; New Edition; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- OPS. PLISA Health Information Platform for the Americas. Edited by Pan American Health Organization. Available online: https://www.paho.org/data/index.php/en/mnu-topics/indicadores-dengue-en/dengue-regional-en.html (accessed on 25 June 2020).
- Pan American Health Organization/World Health Organization. Epidemiological Update: Dengue; PAHO/WHO: Washington, DC, USA, 2020. [Google Scholar]
- Suarez, M.R.; Olarte, S.M.F.; Ana, M.; González, U.C. Is what I have just a cold or is it dengue? Addressing the gap between the politics of dengue control and daily life in Villavicencio-Colombia. Soc. Sci. Med. 2005, 61, 495–502. [Google Scholar] [CrossRef]
- Méndez, J.A.; Usme-Ciro, J.; Domingo, C.; Rey, G.J.; Sánchez, J.A.; Tenorio, A.; Gallego-Gómez, J.C. Phylogenetic reconstruction of dengue virus type 2 in Colombia. Virol. J. 2012, 9, 64. [Google Scholar] [CrossRef] [Green Version]
- Chaparro, P.; León-Quevedo, W.; Castañeda-Orjuela, C. Comportamiento de la mortalidad por dengue en Colombia entre 1985 y 2012. Biomédica 2016, 36, 125–134. [Google Scholar] [CrossRef]
- Villar-Centeno, L.A.; Rojas, D.P.; Besada-Lombana, S.; Sarti, E. Epidemiological Trends of Dengue Disease in Colombia (2000–2011): A Systematic Review. PLoS Neglected Trop. Dis. 2015, 9, e0003499. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, U.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The Prisma Statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Teixeira, M.D.G.; Júnior, J.B.S.; Ferreira, G.L.C.; Bricks, L.; Joint, G. Epidemiological Trends of Dengue Disease in Brazil (2000–2010): A Systematic Literature Search and Analysis. PLoS Neglected Trop. Dis. 2013, 7, e2520. [Google Scholar] [CrossRef] [Green Version]
- Padilla, J.; Rojas, D.; Sáenz-Gómez, R. Dengue in Colombia: Epidemiology of Hyperendemic Re-Emergence; Guías de Impresion LTDA: Bogotá, Colombia, 2012; Volume 1, ISBN 9789584606617. [Google Scholar]
- National Institute of Health (Colombia). Dengue Year Event Report 2013. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Dengue Year Event Report, Colombia, First Semester 2019. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Comportamiento Epidemiológico Del Dengue En Colombia Año 2010. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Report 2004 Dengue. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Dengue Report 2005. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Epidemiological Behavior of Dengue in Colombia, 2008. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Epidemiological Behavior of Dengue in Colombia, 2009. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Epidemiological Behavior of Dengue in Colombia, 2011. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Dengue Year Event Report 2012. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Dengue Year Event Report 2014. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Dengue Year Event Report, Colombia, Until the Thirteenth Epidemiological Period, 2015. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Dengue year event report, Colombia, Until the Thirteenth Epidemiological Period, 2016. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Dengue Year Event Report, 2017. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Dengue Year Event Report, 2018. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Epidemiological Week 2 to 8 August 2020. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). 2006 Final Report Dengue Colombia Surveillance, Weeks 1–52. Edited by Ministerio de Salud. Available online: http://www.ins.gov.co/buscador-eventos/Paginas/Info-Evento.aspx (accessed on 25 June 2020).
- National Institute of Health (Colombia). Dengue Public Health Surveillance Protocol. Edited by Ministerio de Salud. Available online: https://www.paho.org/col/index.php?option=com_docman&view=download&category_slug=publicaciones-ops-oms-colombia&alias=1216-protocolo-para-la-vigilancia-en-salud-publica-del-dengue&Itemid=688 (accessed on 25 June 2020).
- World Health Organization. Dengue and Severe Dengue. Available online: https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue (accessed on 25 June 2020).
- Méndez, J.A.; Usme-Ciro, J.; Domingo, C.; Rey, G.J.; Sánchez, J.A.; Tenorio, A.; Gallego-Gómez, J.C. Phylogenetic history demonstrates two different lineages of dengue type 1 virus in Colombia. Virol. J. 2010, 7, 226. [Google Scholar] [CrossRef] [Green Version]
- Usme-Ciro, J.; Méndez, J.A.; Tenorio, A.; Rey, G.J.; Domingo, C.; Gallego-Gómez, J.C. Simultaneous circulation of genotypes I and III of dengue virus 3 in Colombia. Virol. J. 2008, 5, 101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiménez-Silva, C.L.; Carreño, M.F.; Ortiz-Baez, A.S.; Rey, L.A.; Villabona-Arenas, C.J.; Ocazionez, R.E. Evolutionary history and spatio-temporal dynamics of dengue virus serotypes in an endemic region of Colombia. PLoS ONE 2018, 13, e0203090. [Google Scholar] [CrossRef] [PubMed]
- Carreño, M.F.; Jiménez-Silva, C.L.; Rey-Caro, L.A.; Conde-Ocazionez, S.A.; Flechas-Alarcon, M.; Cruz, S.A.V.; Ocazionez, R.E.; Jiménez, C.L.; Flechas, M.C. Dengue in Santander State, Colombia: Fluctuations in the prevalence of virus serotypes are linked to dengue incidence and genetic diversity of the circulating viruses. Trop. Med. Int. Health 2019, 24, 1400–1410. [Google Scholar]
- Velandia-Romero, M.L.; Coronel-Ruiz, C.; Castro-Bonilla, L.; Camacho-Ortega, S.; Calderón-Peláez, M.A.; Castellanos, A.; Olano, V.A.; Porras, A.; Arevalo-Herrera, M.; Villamil-Gómez, W.; et al. Prevalence of dengue antibodies in healthy children and adults in different Colombian endemic areas. Int. J. Infect. Dis. 2020, 91, 9–16. [Google Scholar] [CrossRef] [Green Version]
- Méndez, F.; Parra, B.; Rengifo, G.; Burbano, M.E.; Arias, J.F.; Muñoz, J.; Barreto, M. Human And Mosquito Infections by Dengue Viruses During and after Epidemics in a dengue–endemic region Of Colombia. Am. J. Trop. Med. Hyg. 2006, 74, 678–683. [Google Scholar] [CrossRef] [Green Version]
- Bocanegra, J.E.M. Updating of the Meteorological Component of the Institutional Model of Ideam on the Climate Effect of the El NiñO and La Niña Phenomena in Colombia, as Input for the Climatological Atlas; Edited by IDEAM, 41; Instituto de hidrologia, Meteorologia y Estudios Ambientales, IDEAM-Subdirección de Meteorología: Bogotá, CO, USA, 2014.
- Ballesteros, H.B.; Enciso, C.R. Indicadores Que Manifiestan Cambios En El Sistema Climático de Colombia (Años Y Décadas Más Calientes Y Las Más Y Menos Lluviosas); Edited by IDEAM, 26; IDEAM: Bogotá, CO, USA, 2012.
- Yang, H.M.; Macoris, M.L.G.; Galvani, K.C.; Andrighetti, M.T.M.; Wanderley, D.M.V. Assessing the effects of temperature on dengue transmission. Epidemiol. Infect. 2009, 137, 1179–1187. [Google Scholar] [CrossRef] [Green Version]
- Watts, U.M.; Burke, N.S.; Harrison, B.A.; Whitmire, R.E.; Nisalak, A. Effect of Temperature on the Vector Efficiency of Aedes aegypti for Dengue 2 Virus. Am. J. Trop. Med. Hyg. 1987, 36, 143–152. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, Z.; Lai, Z.; Zhou, T.; Jia, Z.; Gu, J.; Wu, K.; Chen, X.-G. Temperature Increase Enhances Aedes albopictus Competence to Transmit Dengue Virus. Front. Microbiol. 2017, 8, 2337. [Google Scholar] [CrossRef] [Green Version]
- Roa, A.; Óscar, A.; Capítulo Vi. La Geografía Del Desplazamiento Forzado Reciente En Colombia Y La Estigmatización De La Condición De Desplazado En La Metrópoli Nacional. In Los Desequilibrios Territoriales En Colombia: Estudios Sobre El Sistema De Ciudades Y El Polimetropolitanismo; Universidad Externado de Colombia, Ed.; Universidad Externado de Colombia: Bogotá, CO, USA, 2014. [Google Scholar]
- Castro-Bonilla, L.; Coronel-Ruiz, C.; Parra-Alvarez, S.; Castellanos, J.E.; Porras-Ramírez, A.; Velandia-Romero, M.L. Factors Associated with Dengue Virus Infection and Reinfection in Asymptomatic Children in Two Colombian Municipalities. Am. J. Trop. Med. Hyg. 2018, 99, 1422–1429. [Google Scholar] [CrossRef] [Green Version]
- Bell, S.M.; Katzelnick, L.; Bedford, T. Dengue genetic divergence generates within-serotype antigenic variation, but serotypes dominate evolutionary dynamics. eLife 2019, 8, e42496. [Google Scholar] [CrossRef]
- Clapham, H.E.; Rodriguez-Barraquer, I.; Azman, A.S.; Althouse, B.M.; Salje, H.; Gibbons, R.V.; Rothman, A.L.; Jarman, R.G.; Nisalak, A.; Thaisomboonsuk, B.; et al. Dengue Virus (DENV) Neutralizing Antibody Kinetics in Children After Symptomatic Primary and Postprimary DENV Infection. J. Infect. Dis. 2016, 213, 1428–1435. [Google Scholar] [CrossRef] [PubMed]
- Katzelnick, L.C.; Gresh, L.; Halloran, M.E.; Mercado, J.C.; Kuan, G.; Gordon, A.; Balmaseda, A.; Harris, E. Antibody-dependent enhancement of severe dengue disease in humans. Science 2017, 358, 929–932. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hartl, D.L.; Andrew, G.C. Darwinian Selection. In Principles of Population Genetics; Sinauer Associates Inc.: Sunderland, MA, USA, 2007. [Google Scholar]
- Jaimes-Dueñez, J.; Arboleda, S.; Triana-Chávez, O.; Gómez-Palacio, A. Spatio-Temporal Distribution of Aedes aegypti (Diptera: Culicidae) Mitochondrial Lineages in Cities with Distinct Dengue Incidence Rates Suggests Complex Population Dynamics of the Dengue Vector in Colombia. PLoS Neglected Trop. Dis. 2015, 9, e0003553. [Google Scholar] [CrossRef] [PubMed]
- Chowell, G.; Cazelles, B.; Broutin, H.; Munayco, C.V. The influence of geographic and climate factors on the timing of dengue epidemics in Perú, 1994–2008. BMC Infect. Dis. 2011, 11, 164. [Google Scholar] [CrossRef] [Green Version]
- Parameswaran, P.; Wang, C.; Trivedi, S.B.; Eswarappa, M.; Montoya, M.; Balmaseda, A.; Harris, E. Intrahost Selection Pressures Drive Rapid Dengue Virus Microevolution in Acute Human Infections. Cell Host Microbe 2017, 22, 400–410.e5. [Google Scholar] [CrossRef] [Green Version]
- Ayala-García, J. La Salud En Colombia: Más Cobertura Pero Menos Acceso; Edited by Centor de Estudios Económicos Regionales del Banco de la República, 1–45; Banco De La Republica: Cundinamarca, Colombia, 2014.
- Carabalí, J.M.; Hendrickx, D. Dengue and health care access: The role of social determinants of health in dengue surveillance in Colombia. Glob. Health Promot. 2012, 19, 45–50. [Google Scholar] [CrossRef]
- Minsalud (Ed.) Dinámica Local En Los Niveles Departamentales Y Municipales, Historico De Afiliación, Y. Cobertura; Comportamiento del Aseguramiento: Bogota, Colombia, 2020.




| Region | Main Outbreaks | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1998 | 2002 | 2010 | 2013 | 2019 | ||||||
| Dengue | Severe Dengue | Dengue | Severe Dengue | Dengue | Severe Dengue | Dengue | Severe Dengue | Dengue | Severe Dengue | |
| Atlantic coast | 7072 | 563 | 15,332 | 486 | 12,627 | 622 | 42,167 | 863 | 32,341 | 5178 |
| Central-east | 16,137 | 2333 | 24,997 | 1988 | 49,059 | 5414 | 45,726 | 1007 | 46,598 | 504 |
| Central-west | 202,117 | 1100 | 15,563 | 490 | 48,561 | 850 | 8842 | 165 | 7275 | 58 |
| Orinoquía | 4130 | 353 | 4927 | 67 | 11,349 | 685 | 14,066 | 177 | 25,903 | 185 |
| Amazonía | 733 | 159 | 1375 | 103 | 2519 | 173 | 3133 | 39 | 4939 | 40 |
| Pacific coast | 9673 | 707 | 12,140 | 1768 | 20,822 | 1718 | 23,226 | 832 | 8430 | 92 |
| Total | 57,962 | 5215 | 74,334 | 4902 | 144,937 | 9462 | 137,160 | 3083 | 125,486 | 1397 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gutierrez-Barbosa, H.; Medina-Moreno, S.; Zapata, J.C.; Chua, J.V. Dengue Infections in Colombia: Epidemiological Trends of a Hyperendemic Country. Trop. Med. Infect. Dis. 2020, 5, 156. https://doi.org/10.3390/tropicalmed5040156
Gutierrez-Barbosa H, Medina-Moreno S, Zapata JC, Chua JV. Dengue Infections in Colombia: Epidemiological Trends of a Hyperendemic Country. Tropical Medicine and Infectious Disease. 2020; 5(4):156. https://doi.org/10.3390/tropicalmed5040156
Chicago/Turabian StyleGutierrez-Barbosa, Hernando, Sandra Medina-Moreno, Juan C. Zapata, and Joel V. Chua. 2020. "Dengue Infections in Colombia: Epidemiological Trends of a Hyperendemic Country" Tropical Medicine and Infectious Disease 5, no. 4: 156. https://doi.org/10.3390/tropicalmed5040156
APA StyleGutierrez-Barbosa, H., Medina-Moreno, S., Zapata, J. C., & Chua, J. V. (2020). Dengue Infections in Colombia: Epidemiological Trends of a Hyperendemic Country. Tropical Medicine and Infectious Disease, 5(4), 156. https://doi.org/10.3390/tropicalmed5040156





