Baseline and Impact of First-Year Intervention on Schistosoma haematobium Infection in Seasonal Transmission Foci in the Northern and Central Parts of Côte d’Ivoire
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Study Area
2.3. Study Design and Participants
2.4. Interventions
2.5. Parasitological Procedures
2.5.1. Eligibility Survey
2.5.2. Baseline and One-Year Follow-up Survey
2.6. Statistical Analysis
3. Results
3.1. Population Characteristics
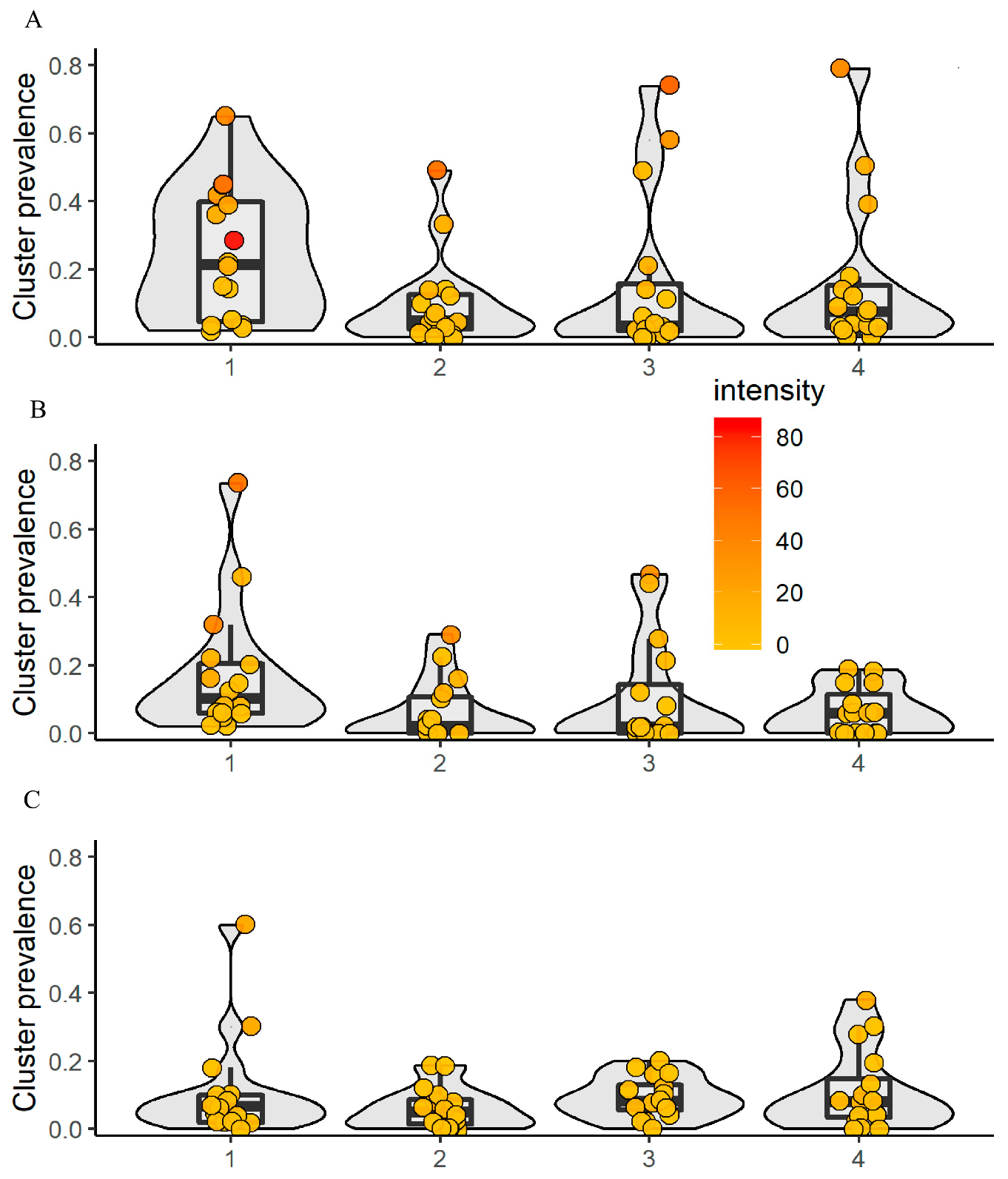
3.2. S. haematobium Infection at Baseline
3.2.1. Children Aged 9−12 Years
3.2.2. First-Grade Children and Adults
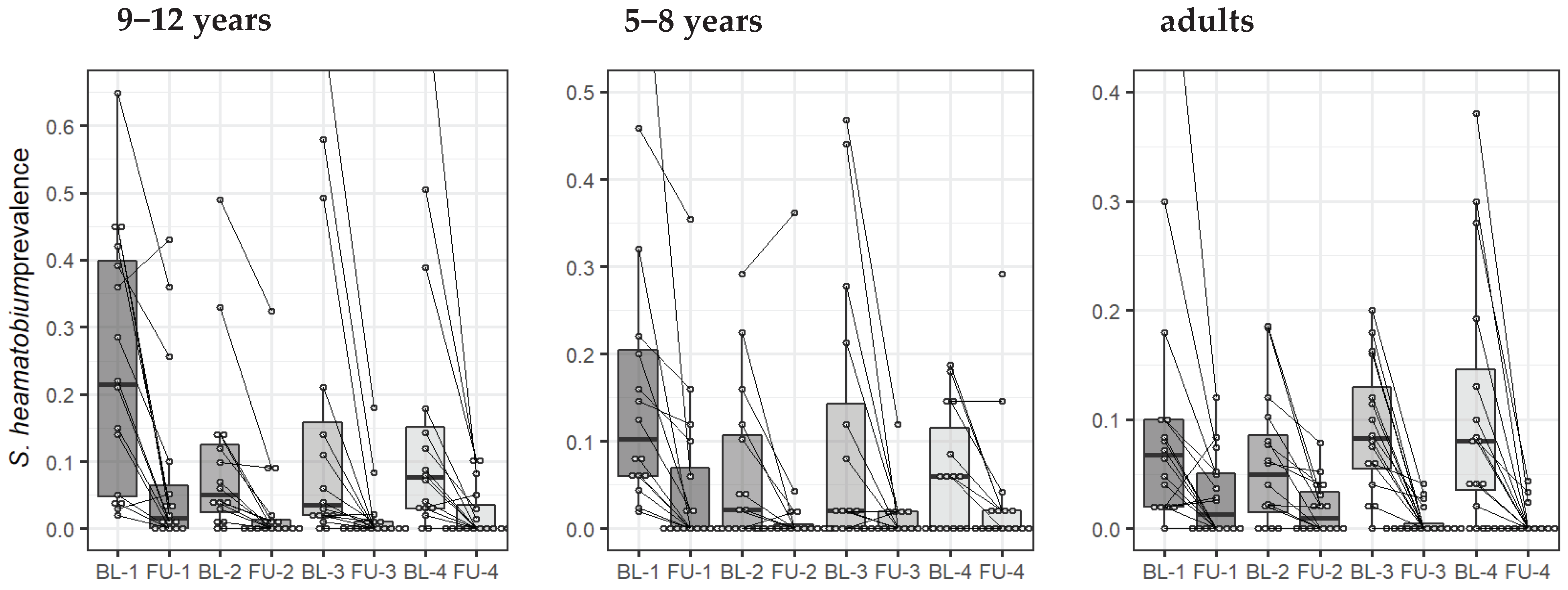
3.3. Differences Among Treatment Arms One Year After Intervention
3.3.1. Children Aged 9−12 Years
3.3.2. First-Grade Children
3.3.3. Adults
3.4. Coverage Rate of Preventive Chemotherapy
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Colley, D.G.; Bustinduy, A.L.; Secor, W.E.; King, C.H. Human schistosomiasis. Lancet 2014, 383, 2253–2264. [Google Scholar] [CrossRef]
- WHO. Schistosomiasis and soil-transmitted helminthiases: Number of people treated in 2016. Wkly. Epidemiol. Rec. 2017, 92, 749–760. [Google Scholar]
- Hotez, P.J.; Alvarado, M.; Basáñez, M.-G.; Bolliger, I.; Bourne, R.; Boussinesq, M.; Brooker, S.J.; Brown, A.S.; Buckle, G.; Budke, C.M.; et al. The Global Burden of Disease Study 2010: Interpretation and implications for the neglected tropical diseases. PLoS Negl. Trop. Dis. 2014, 8, e2865. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- GBD 2017 DALYs and Hale Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar]
- WHO. Schistosomiasis: Progress Report 2001–2011 and Strategic Plan 2012–2020; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- WHO. Elimination of Schistosomiasis. WHA Resolution 65.21. Available online: http://www.who.int/neglected_diseases/mediacentre/WHA_65.21_Eng.pdf (accessed on 1 September 2017).
- French, M.D.; Evans, D.; Fleming, F.M.; Secor, W.E.; Biritwum, N.K.; Brooker, S.J.; Bustinduy, A.; Gouvras, A.; Kabatereine, N.; King, C.H.; et al. Schistosomiasis in Africa: Improving strategies for long-term and sustainable morbidity control. PLoS Negl. Trop. Dis. 2018, 12, e0006484. [Google Scholar] [CrossRef]
- Ezeamama, A.E.; He, C.; Shen, Y.; Yin, X.P.; Binder, S.C.; Campbell, C.H., Jr.; Rathbun, S.; Whalen, C.C.; N’Goran, E.K.; Utzinger, J.; et al. Gaining and sustaining schistosomiasis control: Study protocol and baseline data prior to different treatment strategies in five African countries. BMC Infect. Dis. 2016, 16, 229. [Google Scholar] [CrossRef] [Green Version]
- Knopp, S.; Ame, S.M.; Person, B.; Hattendorf, J.; Rabone, M.; Juma, S.; Muhsin, J.; Khamis, I.S.; Hollenberg, E.; Mohammed, K.A.; et al. A 5-year intervention study on elimination of urogenital schistosomiasis in Zanzibar: Parasitological results of annual cross-sectional surveys. PLoS Negl. Trop. Dis. 2019, 13, e0007268. [Google Scholar] [CrossRef] [Green Version]
- Colley, D.G.; Jacobson, J.A.; Binder, S. Schistosomiasis Consortium for Operational Research and Evaluation (SCORE): Its foundations, development, and evolution. Am. J. Trop. Med. Hyg. 2020, 103 (Suppl. 1), 5–13. [Google Scholar] [CrossRef]
- Tian-Bi, Y.-N.T.; Ouattara, M.; Knopp, S.; Coulibaly, J.T.; Hürlimann, E.; Webster, B.; Allan, F.; Rollinson, D.; Meïté, A.; Diakité, N.R.; et al. Interrupting seasonal transmission of Schistosoma haematobium and control of soil-transmitted helminthiasis in northern and central Côte d’Ivoire: A SCORE study protocol. BMC Public Health 2018, 18, 186. [Google Scholar] [CrossRef] [Green Version]
- King, C.H.; Kittur, N.; Binder, S.; Campbell, C.H.; N’Goran, E.K.; Meite, A.; Utzinger, J.; Olsen, A.; Magnussen, P.; Kinung’hi, S.; et al. Impact of different mass drug administration strategies for gaining and sustaining control of Schistosoma mansoni and Schistosoma haematobium infection in Africa. Am. J. Trop. Med. Hyg. 2020, 103 (Suppl. 1), 14–23. [Google Scholar] [CrossRef]
- Binder, S.; Campbell, C.H.; Castleman, J.D.; Kittur, N.; Kinung’hi, S.M.; Olsen, A.; Magnussen, P.; Karanja, D.M.S.; Mwinzi, P.N.M.; Montgomery, S.P.; et al. Lessons learned in conducting mass drug administration for schistosomiasis control and measuring coverage in an operational research setting. Am. J. Trop. Med. Hyg. 2020, 103 (Suppl. 1), 105–113. [Google Scholar] [CrossRef]
- Plouvier, S.; Leroy, J.C.; Colette, J. A propos d’une technique simple de filtration des urines dans le diagnostic de la bilharziose urinaire en enquête de masse. Med. Trop. 1975, 35, 229–230. [Google Scholar]
- Montresor, A.; Crompton, D.W.T.; Hall, A.; Bundy, D.A.P.; Savioli, L. Guidelines for the Evaluation of Soil-Transmitted Helminthiasis and Schistosomiasis at Community Level; World Health Organization: Geneva, Switzerland, 1998. [Google Scholar]
- WHO. Prevention and control of schistosomiasis and soil-transmitted helminthiasis: Report of a WHO expert committee. World Health Organ. Tech. Rep. Ser. 2002, 912, 1–57. [Google Scholar]
- Colley, D.G.; Fleming, F.M.; Matendechero, S.H.; Knopp, S.; Rollinson, D.; Utzinger, J.; Castleman, J.D.; Kittur, N.; King, C.H.; Campbell, C.H.; et al. Contributions of the Schistosomiasis Consortium for Operational Research and Evaluation (SCORE) to schistosomiasis control and elimination: Key findings and messages for future goals, thresholds, and operational research. Am. J. Trop. Med. Hyg. 2020, 103 (Suppl. 1), 125–134. [Google Scholar] [CrossRef] [PubMed]
- N’Goran, E.K. Biodiversité, Transmission et Epidemiologie de Schistosoma haematobium, Bilharz, 1852, et des Schistosomoses Apparentées en Côte d’Ivoire. Ph.D. Thesis, Université de Perpignan, Perpignan, France, 1997. [Google Scholar]
- Cecchi, P.; Baldé, S.; Yapi, Y.G. Mollusques hôtes intermédiaires de bilharzioses dans les petits barrages. In L’eau en partage. Les petits barrages de Côte d’Ivoire; Cecchi, P., Ed.; IRD Editions; Latitudes 23: Paris, France, 2007; pp. 175–189. [Google Scholar]
- Krauth, S.J.; Musard, C.; Traoré, S.I.; Zinsstag, J.; Achi, Y.L.; N’Goran, E.K.; Utzinger, J. Access to, and use of, water by populations living in a schistosomiasis and fascioliasis co-endemic area of northern Côte d’Ivoire. Acta Trop. 2015, 149, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Diakité, N.R.; Winkler, M.S.; Coulibaly, J.T.; Guindo-Coulibaly, N.; Utzinger, J.; N’Goran, E.K. Dynamics of freshwater snails and Schistosoma infection prevalence in schoolchildren during the construction and operation of a multipurpose dam in central Côte d’Ivoire. Infect. Dis. Poverty 2017, 6, 93. [Google Scholar] [CrossRef] [PubMed]
- Agnew, A.; Fulford, A.J.; Mwanje, M.T.; Gachuhi, K.; Gutsmann, V.; Krijger, F.W.; Sturrock, R.F.; Vennervald, B.J.; Ouma, J.H.; Butterworth, A.E.; et al. Age-dependent reduction of schistosome fecundity in Schistosoma haematobium but not Schistosoma mansoni infections in humans. Am. J. Trop. Med. Hyg. 1996, 55, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Woolhouse, M.E.J. Patterns in parasite epidemiology: The peak shift. Parasitol. Today 1998, 14, 428–434. [Google Scholar] [CrossRef]
- Shashie, G.; Agersew, A.; Sisay, G.; Zeleke, M.; Berhanu, E. Prevalence of urinary schistosomiasis and associated risk factors among Abobo Primary School children in Gambella Regional State, southwestern Ethiopia: A cross sectional study. Parasit. Vectors 2015, 8, 215. [Google Scholar]
- Midzi, N.; Sangweme, D.; Zinyowera, S.; Mapingure, M.P.; Brouwer, K.C.; Kumar, N.; Mutapi, F.; Woelk, G.; Mduluza, T. Efficacy and side effects of praziquantel treatment against Schistosoma haematobium infection among primary school children in Zimbabwe. Trans. R. Soc. Trop. Med. Hyg. 2008, 102, 759–766. [Google Scholar] [CrossRef]
- Chaula, S.A.; Tarimo, D.S. Impact of praziquantel mass drug administration campaign on prevalence and intensity of Schistosoma haematobium among school children in Bahi district, Tanzania. Tanzan. J. Health Res. 2014, 16, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahmed, A.M.; Abbas, H.; Mansour, F.A.; Gasim, G.I.; Adam, I. Schistosoma haematobium infections among schoolchildren in central Sudan one year after treatment with praziquantel. Parasit. Vectors 2012, 5, 108. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Senghor, B.; Diaw, O.T.; Doucoure, S.; Sylla, S.N.; Seye, M.; Talla, I.; Bâ, C.T.; Diallo, A.; Sokhna, C. Efficacy of praziquantel against urinary schistosomiasis and reinfection in Senegalese school children where there is a single well-defined transmission period. Parasit. Vectors 2015, 8, 362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ojurongbe, O.; Sina-Agbaje, O.R.; Busari, A.; Okorie, P.N.; Ojurongbe, T.A.; Akindele, A.A. Efficacy of praziquantel in the treatment of Schistosoma hematobium infection among school-age children in rural communities of Abeokuta, Nigeria. Infect. Dis. Poverty 2014, 3, 30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinmann, P.; Keiser, J.; Bos, R.; Tanner, M.; Utzinger, J. Schistosomiasis and water resources development: Systematic review, meta-analysis, and estimates of people at risk. Lancet Infect. Dis. 2006, 6, 411–425. [Google Scholar] [CrossRef]
- Grimes, J.E.T.; Croll, D.; Harrison, W.E.; Utzinger, J.; Freeman, M.C.; Templeton, M.R. The roles of water, sanitation and hygiene in reducing schistosomiasis: A review. Parasit. Vectors 2015, 8, 156. [Google Scholar] [CrossRef] [Green Version]
- Salari, P.; Fürst, T.; Knopp, S.; Rollinson, D.; Kabole, F.; Khamis, M.I.; Omar, M.A.; Bacon, O.; Ali, S.M.; Utzinger, J.; et al. Financial costs of the Zanzibar elimination of schistosomiasis transmission project. Am. J. Trop. Med. Hyg. 2020, 103, 2260–2267. [Google Scholar] [CrossRef]


| School-Aged Children (9−12 years) | ||||
|---|---|---|---|---|
| Arm 1 | Arm 2 | Arm 3 | Arm 4 | |
| Villages | 16 | 16 | 16 | 16 |
| Total participants | 1548 | 1579 | 1510 | 1495 |
| Mean age (years) | 10.3 | 10.2 | 10.4 | 10.4 |
| Sex | ||||
| Females | 628 | 710 | 673 | 671 |
| Males | 920 | 869 | 837 | 824 |
| Number of individuals infected with S. haematobium (prevalence) | 383 (24.8%) | 159 (10.1%) | 210 (13.9%) | 233 (15.8%) |
| Arithmetic mean infection intensity (eggs per 10 mL of urine) | 73.5 | 55.6 | 54.1 | 40.2 |
| Infection intensity | ||||
| Light (1−49 eggs per 10 mL of urine) | 277 (17.9%) | 129 (8.2%) | 154 (10.2%) | 183 (12.4%) |
| Heavy (≥50 eggs per 10 mL of urine) | 106 (6.8%) | 30 (1.9%) | 56 (3.7%) | 50 (3.4%) |
| First-grade children (5−8 years) | ||||
| Total participants | 840 | 792 | 806 | 746 |
| Mean age (years) | 6.8 | 6.9 | 6.8 | 6.8 |
| Sex | ||||
| Females | 408 | 407 | 426 | 391 |
| Males | 432 | 385 | 380 | 355 |
| Number of individuals infected with S. haematobium (prevalence) | 147 (17.9%) | 50 (6.3%) | 87 (10.8%) | 48 (6.6%) |
| Arithmetic mean infection intensity (eggs per 10 mL of urine) | 55.7 | 64.0 | 41.7 | 30.3 |
| Infection intensity | ||||
| Light (1−49 eggs per 10 mL of urine) | 104 (12.7%) | 34 (4.3%) | 67 (8.3%) | 40 (5.5%) |
| Heavy (≥50 eggs per 10 mL of urine) | 43 (5.2%) | 16 (2.0%) | 20 (2.5%) | 8 (1.1%) |
| Adults (20−55 years) | ||||
| Total participants | 734 | 765 | 768 | 761 |
| Mean age (years) | 37.9 | 37.4 | 37 | 37.2 |
| Sex | ||||
| Females | 437 | 475 | 463 | 444 |
| Males | 297 | 290 | 305 | 317 |
| Age (20−55 years) | 727 | 761 | 762 | 757 |
| Number of individuals infected with S. haematobium (prevalence) | 85 (11.7%) | 46 (6.0%) | 70 (10.8%) | 83 (11.0%) |
| Arithmetic mean infection intensity (eggs per 10 mL of urine) | 37.2 | 29.9 | 11.7 | 20.3 |
| Infection intensity | ||||
| Light (1−49 eggs per 10 mL of urine) | 71 (9.7%) | 40 (5.2%) | 68 (8.2%) | 75 (9.9%) |
| Heavy (≥50 eggs per 10 mL of urine) | 14 (1.9%) | 6 (0.8%) | 2 (0.3%) | 8 (1.0%) |
| School-Aged Children (9−12 years) | First-Grade Children (5−8 years) | Adults (20−55 years) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | Arm 1 | Arm 2 | Arm 3 | Arm 4 | Arm 1 | Arm 2 | Arm 3 | Arm 4 | Arm 1 | Arm 2 | Arm 3 | Arm 4 |
| Baseline | ||||||||||||
| Examined | 1544 | 1573 | 1506 | 1469 | 820 | 788 | 804 | 726 | 727 | 761 | 762 | 759 |
| Infected | 383 | 159 | 210 | 233 | 147 | 50 | 87 | 48 | 85 | 46 | 70 | 85 |
| Prevalence (%) | 24.8 | 10.1 | 13.9 | 15.9 | 17.9 | 6.4 | 10.8 | 6.6 | 11.7 | 6.0 | 9.2 | 11.0 |
| Village-level AM infection intensity (eggs per 10 mL of urine) | 17.9 | 5.7 | 8.4 | 6.2 | 9.6 | 4.1 | 4.5 | 2.0 | 4.0 | 2.0 | 1.1 | 2.1 |
| Individual-level AM infection intensity (eggs per 10 mL of urine) | 73.5 | 55.9 | 54.1 | 40.2 | 55.7 | 64.0 | 41.7 | 30.4 | 37.2 | 29.9 | 11.7 | 20.0 |
| Year 1 | ||||||||||||
| Examined | 1538 | 1561 | 1510 | 1487 | 789 | 805 | 774 | 777 | 596 | 694 | 626 | 590 |
| Infected | 124 | 55 | 29 | 33 | 41 | 21 | 10 | 27 | 18 | 13 | 5 | 4 |
| Prevalence (%) | 8.1 | 3.5 | 1.9 | 2.2 | 5.2 | 2.6 | 1.3 | 3.5 | 3.0 | 1.9 | 0.8 | 0.7 |
| Village-level AM infection intensity (eggs per 10 mL of urine) | 3.7 | 2.3 | 0.2 | 0.6 | 1.1 | 2.1 | 0.2 | 2.9 | 0.8 | 0.8 | 0.1 | 0.2 |
| Individual-level AM infection intensity (eggs per 10 mL of urine) | 46.1 | 65.3 | 9.4 | 26.4 | 21.8 | 76.1 | 18.1 | 84.3 | 23.9 | 50.0 | 19.2 | 23.3 |
| Absolute difference prevalence (%-points) | −16.7 | −6.6 | −12.0 | 13.7 | −12.7 | −3.7 | −9.5 | −9.5 | −8.7 | −4,1 | −8.4 | −8.4 |
| Relative difference prevalence (% change) | −67.3 | −65.3 | −86.3 | −86.1 | −70.9 | −58.7 | −88.0 | −88.0 | −74.3 | −68.3 | −91.3 | −91.3 |
| Egg reduction rate (%) | −79.3 | −59.6 | 97.6 | 90.3 | −88.5 | −48.8 | 95.5 | −45.0 | −80.0 | 60.0 | 90.9 | 93.6 |
| Age Group | Comparison | Difference in Prevalence | |
|---|---|---|---|
| OR (95% CI) | aOR (95% CI) | ||
| 9−12 years | Arm 2 vs. arm 1 | 0.42 (0.10-1.80) | 1.03 (0.34−3.07) |
| Arm 3 vs. arm 1 | 0.22 (0.05−0.95) | 0.19 (0.08−0.48) | |
| Arm 4 vs. arm 1 | 0.26 (0.08−0.85) | 0.23 (0.06−0.87) | |
| 5−8 years | Arm 2 vs. arm 1 | 0.49 (0.08−3.01) | 1.38 (0.17−11.10) |
| Arm 3 vs. arm 1 | 0.24 (0.06−1.03) | 0.39 (0.10−1.54) | |
| Arm 4 vs. arm 1 | 0.33 (0.08−1.31) | 0.91 (0.20−4.23) | |
| 20−55 years | Arm 2 vs. arm 1 | 0.61 (0.25−1.52) | 0.88 (0.36−2.12) |
| Arm 3 vs. arm 1 | 0.26 (0.08−0.81) | 0.32 (0.11−0.96) | |
| Arm 4 vs. arm 1 | 0.22 (0.06−0.79) | 0.21 (0.07−0.64) | |
| Treatment | Annual MDA Before the Peak Transmission Season | Annual MDA After the Peak Transmission Season | |||
|---|---|---|---|---|---|
| Year 1 | Arm 1 | Arm 3 | Arm 4 | Arm 2 | Arm 3 |
| MDA period | December 2015 | December 2015 | December 2015 | April 2016 | April 2016 |
| No. of villages treated | 16 | 16 | 16 | 16 | |
| School-aged children treated | 4988 | 7086 | 5018 | 4206 | 7024 |
| Total number of school-aged children | 5145 | 7440 | 5381 | 5572 | 7440 |
| Treatment coverage in school-aged children (%) | 96.9 | 95.2 | 93.3 | 75.5 | 94.4 |
| Adults treated | 8942 | 12,671 | 12,700 | 9897 | 12,992 |
| Total number of adults | 12,081 | 20,267 | 21,650 | 15,809 | 20,978 |
| Treatment coverage in adults (%) | 74.0 | 62.5 | 58.6 | 62.6 | 62.0 |
| Total no. of participants treated | 13,930 | 19,757 | 17,718 | 16,391 | 23,849 |
| Total participants | 17,226 | 27,707 | 27,031 | 21,381 | 28,418 |
| Overall coverage (%) | 80.9 | 71.3 | 65.5 | 76.7 | 83.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diakité, N.R.; Ouattara, M.; Bassa, F.K.; Coulibaly, J.T.; Tian-Bi, Y.-N.T.; Meïté, A.; Hattendorf, J.; Utzinger, J.; N’Goran, E.K. Baseline and Impact of First-Year Intervention on Schistosoma haematobium Infection in Seasonal Transmission Foci in the Northern and Central Parts of Côte d’Ivoire. Trop. Med. Infect. Dis. 2021, 6, 7. https://doi.org/10.3390/tropicalmed6010007
Diakité NR, Ouattara M, Bassa FK, Coulibaly JT, Tian-Bi Y-NT, Meïté A, Hattendorf J, Utzinger J, N’Goran EK. Baseline and Impact of First-Year Intervention on Schistosoma haematobium Infection in Seasonal Transmission Foci in the Northern and Central Parts of Côte d’Ivoire. Tropical Medicine and Infectious Disease. 2021; 6(1):7. https://doi.org/10.3390/tropicalmed6010007
Chicago/Turabian StyleDiakité, Nana R., Mamadou Ouattara, Fidèle K. Bassa, Jean T. Coulibaly, Yves-Nathan T. Tian-Bi, Aboulaye Meïté, Jan Hattendorf, Jürg Utzinger, and Eliézer K. N’Goran. 2021. "Baseline and Impact of First-Year Intervention on Schistosoma haematobium Infection in Seasonal Transmission Foci in the Northern and Central Parts of Côte d’Ivoire" Tropical Medicine and Infectious Disease 6, no. 1: 7. https://doi.org/10.3390/tropicalmed6010007
APA StyleDiakité, N. R., Ouattara, M., Bassa, F. K., Coulibaly, J. T., Tian-Bi, Y.-N. T., Meïté, A., Hattendorf, J., Utzinger, J., & N’Goran, E. K. (2021). Baseline and Impact of First-Year Intervention on Schistosoma haematobium Infection in Seasonal Transmission Foci in the Northern and Central Parts of Côte d’Ivoire. Tropical Medicine and Infectious Disease, 6(1), 7. https://doi.org/10.3390/tropicalmed6010007





