Rapidly Containing the First Indigenous Outbreak of Chikungunya in Taiwan—Lessons Learned
Abstract
:1. Introduction
2. Materials and Methods
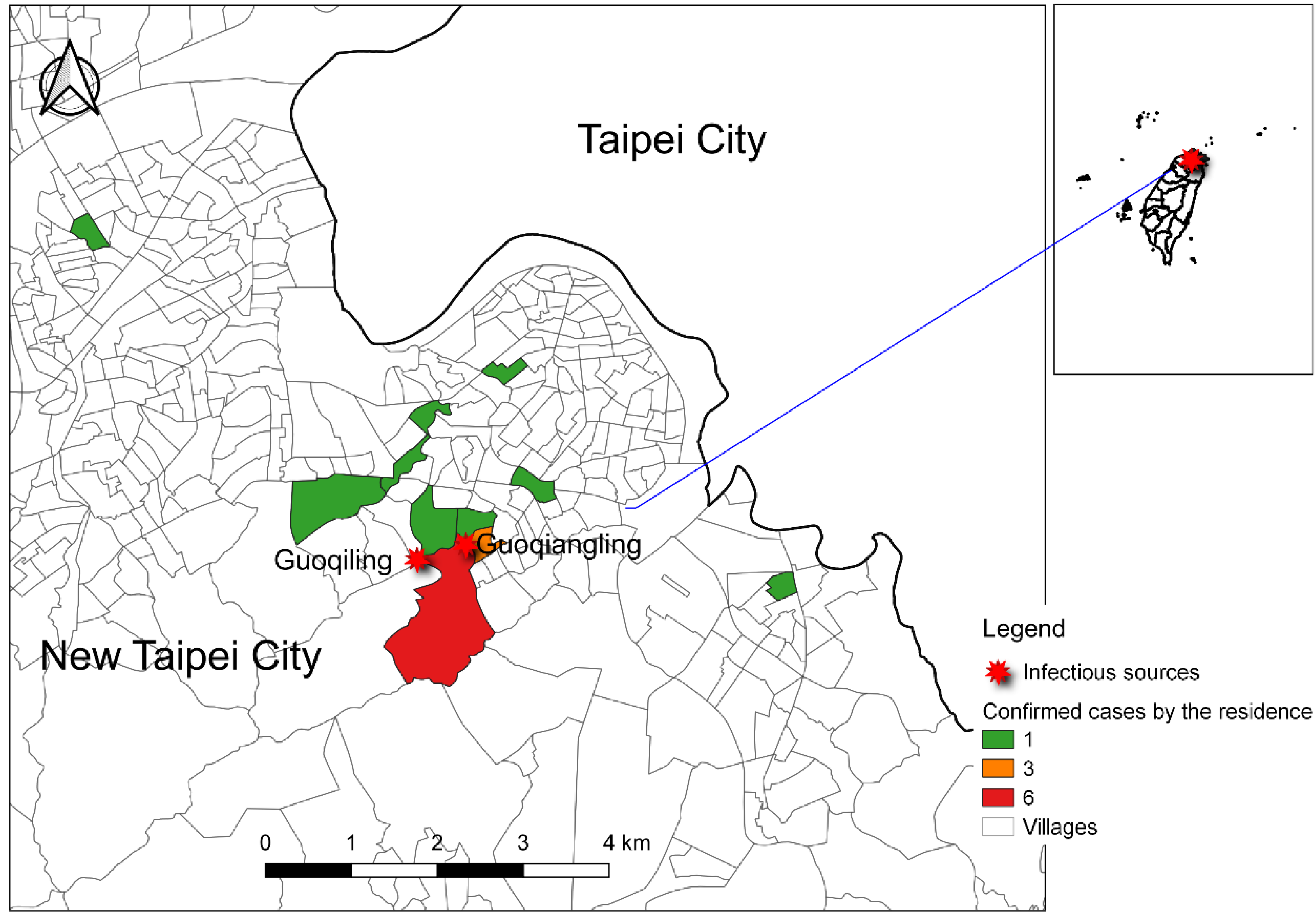
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

References
- Chang, S.F.; Huang, J.H.; Shu, P.Y. Characteristics of dengue epidemics in Taiwan. J. Formos. Med. Assoc. 2012, 111, 297–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yeh, C.Y.; Chen, P.L.; Chuang, K.T.; Shu, Y.C.; Chien, Y.W.; Perng, G.C.; Ko, W.C.; Ko, N.Y. Symptoms associated with adverse dengue fever prognoses at the time of reporting in the 2015 dengue outbreak in Taiwan. PLoS Negl. Trop. Dis. 2017, 11, e0006091. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shang, C.S.; Fang, C.T.; Liu, C.M.; Wen, T.H.; Tsai, K.H.; King, C.C. The role of imported cases and favorable meteorological conditions in the onset of dengue epidemics. PLoS Negl. Trop. Dis. 2010, 4, e775. [Google Scholar] [CrossRef] [PubMed]
- Akiner, M.M.; Demirci, B.; Babuadze, G.; Robert, V.; Schaffner, F. Spread of the invasive mosquitoes aedes aegypti and aedes albopictus in the Black Sea region increases risk of chikungunya, dengue, and zika outbreaks in europe. PLoS Negl. Trop. Dis. 2016, 10, e0004664. [Google Scholar] [CrossRef] [Green Version]
- Vairo, F.; Di Pietrantonj, C.; Pasqualini, C.; Mammone, A.; Lanini, S.; Nicastri, E.; Castilletti, C.; Ferraro, F.; Di Bari, V.; Puro, V.; et al. The surveillance of chikungunya virus in a temperate climate: Challenges and possible solutions from the experience of Lazio Region, Italy. Viruses 2018, 10, 501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shu, P.Y.; Yang, C.F.; Su, C.L.; Chen, C.Y.; Chang, S.F.; Tsai, K.H.; Cheng, C.H.; Huang, J.H. Two imported chikungunya cases, Taiwan. Emerg. Infect. Dis. 2008, 14, 1326–1327. [Google Scholar] [CrossRef] [PubMed]
- Wei, H.Y.; Chung, Y.J.; Chou, C.Y.; Hung, M.L.; Tsai, Y.F.; Tung, H.P.; Hsieh, J.W. The investigation of the first autochthonous chikungunya outbreak in Taiwan, 2019. Taiwan Epidemiol. Bull. 2019, 35, 130. [Google Scholar] [CrossRef]
- Wang, W.H.; Lin, C.Y.; Chang, K.; Urbina, A.N.; Assavalapsakul, W.; Thitithanyanont, A.; Lu, P.L.; Chen, Y.H.; Wang, S.F. A clinical and epidemiological survey of the largest dengue outbreak in Southern Taiwan in 2015. Int. J. Infect. Dis. 2019, 88, 88–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kao, J.H.; Chen, C.D.; Tiger Li, Z.R.; Chan, T.C.; Tung, T.H.; Chu, Y.H.; Cheng, H.Y.; Liu, J.W.; Shih, F.Y.; Shu, P.Y.; et al. The critical role of early dengue surveillance and limitations of clinical reporting—Implications for non-endemic countries. PLoS ONE 2016, 11, e0160230. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakkhara, P.; Chongsuvivatwong, V.; Thammapalo, S. Risk factors for symptomatic and asymptomatic chikungunya infection. Trans. R. Soc. Trop. Med. Hyg. 2013, 107, 789–796. [Google Scholar] [CrossRef] [PubMed]
- Rudolph, K.E.; Lessler, J.; Moloney, R.M.; Kmush, B.; Cummings, D.A. Incubation periods of mosquito-borne viral infections: A systematic review. Am. J. Trop. Med. Hyg. 2014, 90, 882–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, W.J. Dengue outbreaks and the geographic distribution of dengue vectors in Taiwan: A 20-year epidemiological analysis. Biomed. J. 2018, 41, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Ogden, N.H. Climate change and vector-borne diseases of public health significance. FEMS Microbiol. Lett. 2017, 364. [Google Scholar] [CrossRef] [PubMed]
- Rezza, G.; Nicoletti, L.; Angelini, R.; Romi, R.; Finarelli, A.C.; Panning, M.; Cordioli, P.; Fortuna, C.; Boros, S.; Magurano, F.; et al. Infection with chikungunya virus in Italy: An outbreak in a temperate region. Lancet 2007, 370, 1840–1846. [Google Scholar] [CrossRef]
- Venturi, G.; Di Luca, M.; Fortuna, C.; Remoli, M.E.; Riccardo, F.; Severini, F.; Toma, L.; Del Manso, M.; Benedetti, E.; Caporali, M.G.; et al. Detection of a chikungunya outbreak in Central Italy, August to September 2017. Euro Surveill. 2017, 22, 17-00646. [Google Scholar] [CrossRef] [Green Version]
- Bustos Carrillo, F.; Collado, D.; Sanchez, N.; Ojeda, S.; Lopez Mercado, B.; Burger-Calderon, R.; Gresh, L.; Gordon, A.; Balmaseda, A.; Kuan, G.; et al. Epidemiological evidence for lineage-specific differences in the risk of inapparent chikungunya virus infection. J. Virol. 2019, 93, e01622-18. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Risk Factors | n | Mean/Percent | S.D. | Min. | Max. |
|---|---|---|---|---|---|
| Age | 19 | 58.89 | 13.01 | 34 | 88 |
| Sex (%) | |||||
| Male | 5 | 26.30 | - | - | - |
| Female | 14 | 73.70 | - | - | - |
| # of medical visits | 19 | 2.79 | 1.65 | 1 | 7 |
| Wave 1 (8/23–9/12) a | 13 | 3.15 | 1.86 | p = 0.244 | |
| Wave 2 (9/13–10/3) a | 6 | 2.00 | 0.63 | ||
| Days between onset and reporting | 19 | 6.21 | 5.62 | 0 | 23 |
| Wave 1 (8/23–9/12) a | 13 | 6.54 | 5.95 | p = 0.521 | |
| Wave 2 (9/13–10/3) a | 6 | 5.50 | 5.28 | ||
| Serological Tests | n | Days Since Illness Onset | |||
|---|---|---|---|---|---|
| Mean | S.D. | Min. | Max. | ||
| First blood collection (n = 19) | |||||
| PCR+ | 8 | 3.13 | 2.75 | 1 | 9 |
| IgM+ | 5 | 9.60 | 7.73 | 4 | 23 |
| IgG+ | 4 | 10.75 | 8.42 | 4 | 23 |
| Second blood collection (n = 9) | |||||
| IgM+ and IgG+ | 9 | 12.33 | 4.21 | 5 | 20 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, T.-C.; Hsu, Y.-F.; Huang, S.-C.; Chen, R.-C. Rapidly Containing the First Indigenous Outbreak of Chikungunya in Taiwan—Lessons Learned. Trop. Med. Infect. Dis. 2021, 6, 165. https://doi.org/10.3390/tropicalmed6030165
Chan T-C, Hsu Y-F, Huang S-C, Chen R-C. Rapidly Containing the First Indigenous Outbreak of Chikungunya in Taiwan—Lessons Learned. Tropical Medicine and Infectious Disease. 2021; 6(3):165. https://doi.org/10.3390/tropicalmed6030165
Chicago/Turabian StyleChan, Ta-Chien, Yu-Fen Hsu, Shao-Chun Huang, and Ran-Chou Chen. 2021. "Rapidly Containing the First Indigenous Outbreak of Chikungunya in Taiwan—Lessons Learned" Tropical Medicine and Infectious Disease 6, no. 3: 165. https://doi.org/10.3390/tropicalmed6030165
APA StyleChan, T.-C., Hsu, Y.-F., Huang, S.-C., & Chen, R.-C. (2021). Rapidly Containing the First Indigenous Outbreak of Chikungunya in Taiwan—Lessons Learned. Tropical Medicine and Infectious Disease, 6(3), 165. https://doi.org/10.3390/tropicalmed6030165






