Healthcare Management of Human African Trypanosomiasis Cases in the Eastern, Muchinga and Lusaka Provinces of Zambia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Permissions and Consent to Participate
2.2. Study Site and Design
2.3. Methods for Data Collection
2.4. Data Analysis
3. Results
3.1. Number of rHAT Cases 2004 to 2014
3.2. Knowledge of rHAT Transmission
3.3. Common Signs and Symptoms Developed by rHAT Patients
3.4. Case Management of rHAT Patients
The standard protocol for detection of rHAT is used on all cases received at UTH. This involves screening for potential infection, diagnosing by establishing whether the parasite is present in the body fluids, and staging to determine the level of the disease’s progression. The second stage disease detection involves a lumbar puncture. The drug used for treatment of the first stage patient is suramin and in the second stage melarsoprol.
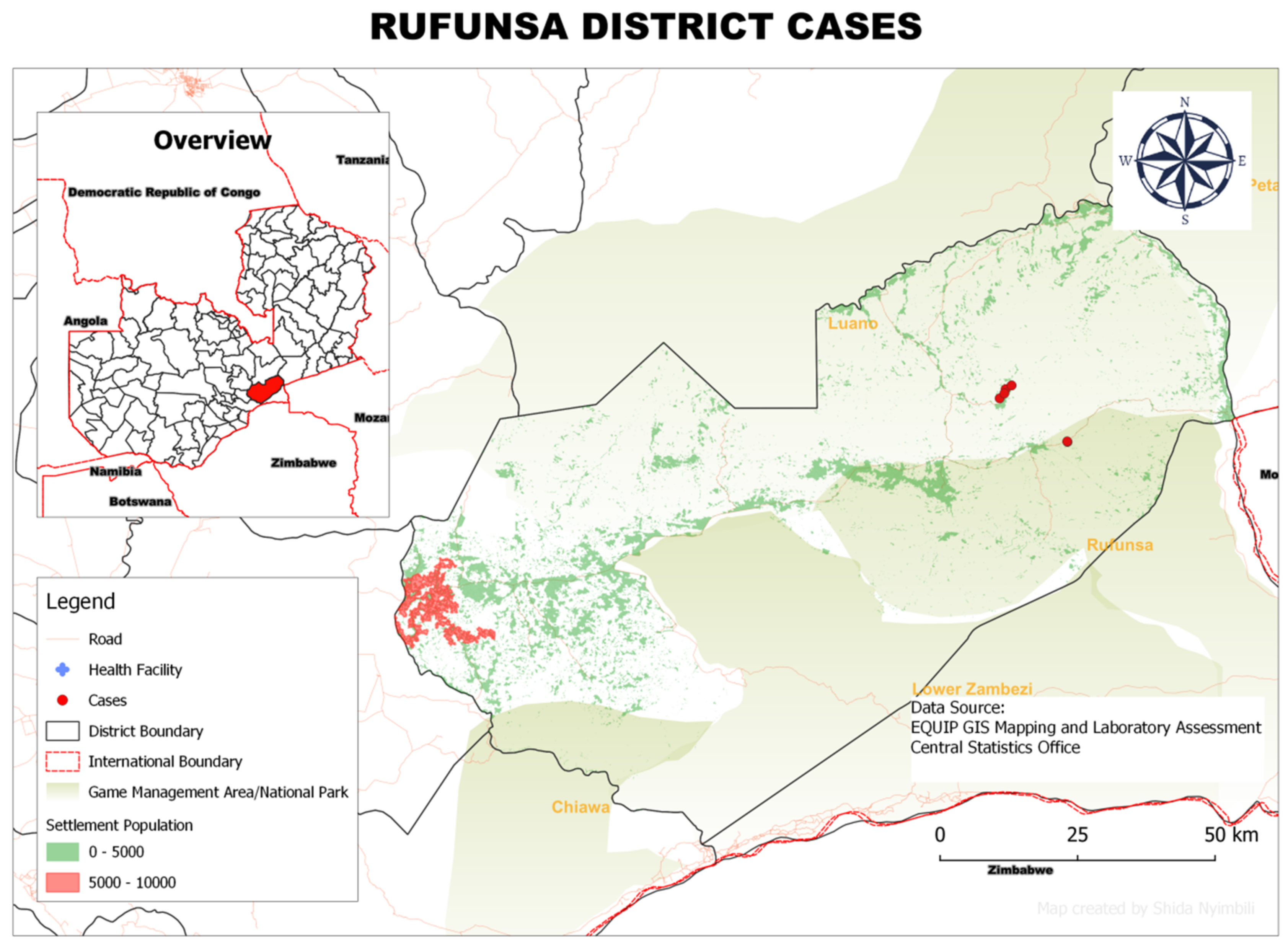
A common challenge in the treatment of sleeping sickness is organ failure. A case was recorded of a 49 year old game ranger who was admitted to UTH hospital. His lung was normal and there was no leg swelling. Early stage HAT was detected by both microscopy and SRA-LAMP. Another example related to delays in diagnosis: A female adult aged 58 was admitted with fever and a reduced level of consciousness. On examination she was noted with lethargy and had an abnormal lung. However, late stage HAT was confirmed by microscopy and SRA-LAMP which was missed for several weeks while being treated for other conditions. Due to the delay in diagnosis, she died eight days after starting melarsoprol treatment. Not all HAT cases present the same signs and symptoms. This depends also on the index of suspicion from the onset of diagnosis.” Although it is recommended that patients come for review after completing the treatment, the key respondents indicated that this rarely happens at UTH: “It is also recommended that patients come for review at UTH. However, we have no record of a patient who came for review after being discharged. For example, we had a case of re-occurrence of infection in Rufunsa (St Luke’s hospital). This was after the patient was discharged from UTH. However, there has been no communication regarding the patients who are re-admitted at the various districts.
3.5. The Population at Risk and Land Cover
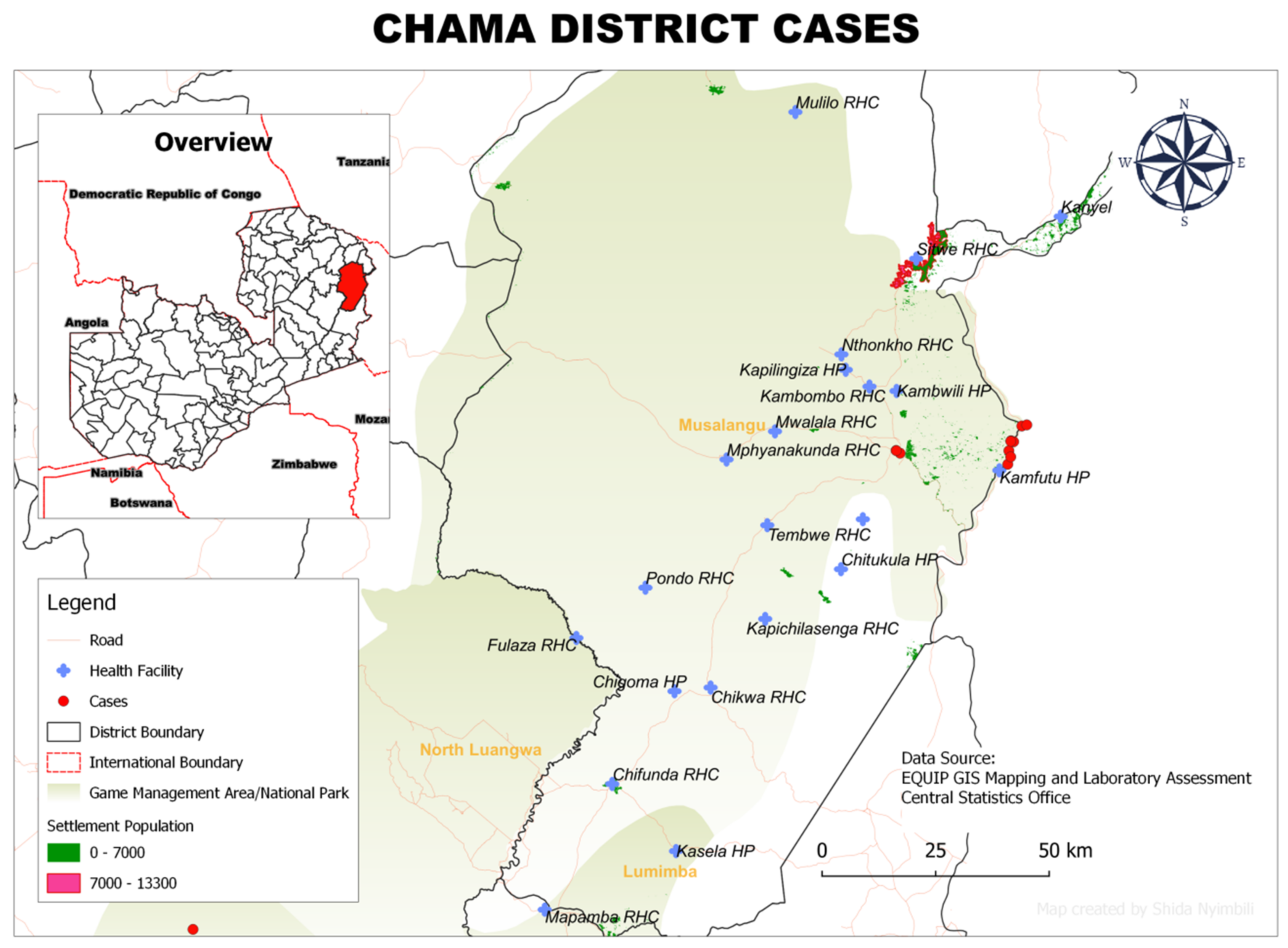
3.6. Spatial Distribution of rHAT Cases in Each District
The transmission of rHAT is also due to the game animals especially elephants and Buffalos. Encroachment of the human habitable land is very common. It’s not always the people who go in the game reserve areas. As a result, they come along with the tsetse flies and shed them in the communities. Currently, as residents we don’t see much of the mechanisms available to control the game animals they are elusive.
3.7. Healthcare Delivery Systems
4. Discussion
- (i)
- Enhancement of rHAT (and its transmission dynamics) advocacy and sensitisation among both health personnel and local communities in tsetse-inhabited rural areas. This is expected to increase the suspicion index among health workers and promote earlier reporting of suspicious cases to health centres by local communities;
- (ii)
- Governments in tsetse-inhabited regions should be urged to invest in basic diagnostic equipment, such as microscopes for detection of various haemoparasites, including plasmodium and trypanosome parasites, as well as detection of ectoparasites and endoparasites. Each rural health centre should have at least one microscope and a trained technician, who should attend refresher courses regularly. Both (i) and (ii) are ingredients of early and accurate detection of rHAT cases, which should lead eventually to successful case management with minimal complications;
- (iii)
- In referral centres with advanced diagnostic capacity, regular screening of domestic animals, wildlife and tsetse flies for trypanosome species by means of microscopy and more sensitive molecular tests such as PCR and, in particular, the user-friendly and cost-effective LAMP, should be encouraged;
- (iv)
- Because wild animals are natural reservoirs of T. b. rhodesiense, local communities and their domestic animals should be discouraged from encroaching into game management areas and national parks in order to minimise interactions with wildlife and tsetse flies. Furthermore, local communities should be sensitised to the dangers of poaching and related activities, which expose them to tsetse bites, and the management of rHAT should be considered when developing management plans for game management areas;
- (v)
- Health workers in rural health centres should be trained in basic record keeping and its significance in management and control of diseases, including rHAT;
- (vi)
- Governments in tsetse-inhabited regions should be encouraged to invest in effective tsetse control measures, such as insecticide-impregnated targets or aerial spraying with pyrethroids. Considering that rHAT is a transboundary disease, countries sharing boundaries in such regions should work closely and conduct such activities jointly to more sustainably control tsetse flies and subsequently rHAT.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| HAT | Human African trypanosomiasis |
| LAMP | Loop-mediated isothermal amplification |
| LE | Life expectancy |
| PCR | Polymerise chain reaction |
| rHAT | Human African trypanosomiasis rhodesiense |
| UTH | University Teaching Hospital, Lusaka |
| WHO | World Health Organization |
References
- Stict, A.; Abel, M.P.; Kreshna, S. Clinical Review Human African Trypanosomiasis. Br. Med. J. 2012, 325, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Fèvre, E.M.; Wissman, B.V.W.; Welburn, C.S.; Lutumba, P. The Burden of Human African Trypanosomiasis. PLoS Negl. Trop. Dis. 2008, 2, e333. [Google Scholar] [CrossRef] [PubMed]
- Franco, J.R.; Cecchi, G.; Priotto, G.; Paone, M.; Diarra, A.; Grout, L.; Simarro, P.P.; Zhao, W.; Argaw, D. Monitoring the Elimination of Human African Trypanosomiasis: Update to 2016. PLoS Negl. Trop. Dis. 2018, 12, e0005585. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Report of a WHO Meeting on Elimination of African Trypanosomiasis (Trypanosoma brucei Gambiense) 2013, 4. Available online: https://apo.who.int/publications/i/item/WHO-HTM-NTD-IDM-2013.4 (accessed on 18 July 2020).
- WHO. Trypanosomiasis, Human African (Sleeping Sickness); WHO: Geneva, Switzerland, 2019. [Google Scholar]
- Bonnet, J.; Boudot, C.; Courtioux, B. Overview of the Diagnostic Methods Used in the Field for Human African Trypanosomiasis: What Could Change in the Next Years? BioMed Res. Int. 2015, 10, 1155. [Google Scholar] [CrossRef] [PubMed]
- Franco, J.R.; Cecchi, G.; Priotto, G.; Paone, M.; Diarra, A.; Grout, L.; Simarro, P.P.; Zhao, W.; Argaw, D. Monitoring the elimination of human African trypanosomiasis at continental and country level: Update to 2018. PLoS Negl. Trop. Dis. 2020, 14, e0008261. [Google Scholar] [CrossRef] [PubMed]
- Hotez, P.; Pecoul, B.; Rijal, S.; Boehme, C.; Askoy, S.; Malecela, M.; Tapia-Conyer, R.; Reeder, C.J. Eliminating the Neglected Tropical Diseases Translational Science and New Technologies. PLos Negl. Trop. Dis. 2016, 10, e0003895. [Google Scholar] [CrossRef] [PubMed]
- Neuberger, A.; Meltzer, E.; Leshem, E.; Dickstein, Y.; Stienlauf, S.; Schwartz, E. The Changing Epidemiology of Human African Trypanosomiasis among Patients from Nonendemic Countries—1902–2012. PLoS ONE 2014, 9, e88647. [Google Scholar] [CrossRef] [PubMed]
- Central Statistics Office. Zambia in Figures, Information, Research and Dissemination Division; Central Statistics Office: Lusaka, Zambia, 2018. [Google Scholar]
- Mwanakasale, V.; Songolo, P. Disappearance of some human African trypanosomiasis transmission foci in Zambia in the absence of a tsetse fly and trypanosomiasis control program over a period of forty years. Trans. R. Soc. Trop. Med. Hyg. 2011, 105, 167–172. [Google Scholar] [CrossRef]
- Mwanakasale, V.; Songolo, P.; Babaniyi, O.; Simarro, P. Clinical presentation of human African trypanosomiasis in Zambia is linked to the existence of strains of Trypanosoma brucei rhodesiense with varied virulence: Two case reports. J. Med. Case Rep. 2014, 8, 53. [Google Scholar] [CrossRef]
- Mwiinde, M.A.; Simuunza, M.; Namangala, B.; Chama-Chiliba, M.C.; Machila, N.; Anderson, N.; Shaw, A.; Welburn, C.S. Estimating the economic and social consequences for patients diagnosed with human African trypanosomiasis in Muchinga, Lusaka and Eastern Provinces of Zambia (2004–2014). Infect. Dis. Poverty 2017, 6, 150. [Google Scholar] [CrossRef] [Green Version]
- Squarre, D.; Kabongo, I.; Munyeme, M.; Mumba, C.; Mwasinga, W.; Hachaambwa, L.; Sugimoto, C.; Namangala, B. Human African Trypanosomiasis in the Kafue National Park, Zambia. PLoS Negl. Trop. Dis. 2016, 19, 10. [Google Scholar] [CrossRef]
- WHO. Trypanosomiasis, Human African (Sleeping Sickness); WHO: Geneva, Switzerland, 2018. [Google Scholar]
- Mwiinde, A.M.; Simuunza, M.; Namangala, B.; Chama-Chiliba, C.M.; Machila, N.; Anderson, N.; Shaw, A.; Welburn, S.C. Economic and Social Data on the Impact of Human African Trypanosomiasis in Eastern Zambia (2004–2014); NERC Environmental Information Data Centre: Lancaster, UK, 2017. [Google Scholar] [CrossRef]
- World Bank. Climate Change Knowledge Portal for Development Practitioners and Policy makers. Data Snap Shots 1991–2020. 2021. Available online: https://climateknowledgeportal.worldbank.org/country/zambia/climate-data-historical (accessed on 16 August 2022).
- Climate Data: Zambia Climate Data.Org. Available online: https://en.climate-data.org/africa/zambia-192/ (accessed on 16 August 2022).
- Welburn, S.C.; Picozz, K.; Fèvre, E.M.; Coleman, P.G.; Odiit, M.; Carrington, M.; Maudlin, I. Identification of human-infective trypanosomes in animal reservoir of sleeping sickness in Uganda by means of serum-resistance-associated (SRA) gene. Lancet 2001, 358, 2017–2019. [Google Scholar] [CrossRef]
- Namangala, B.; Hachaambwa, L.; Kajino, K.; Mweene, S.A.; Hayashida, K.; Simuunza, M.; Simukoko, H.; Choongo, K.; Chansa, P.; Lakhi, S.; et al. The use of Loop-Mediated Isothermal Amplification (LAMP) to detect the Re-Emerging Human African Trypanosomiasis (HAT) in the Luangwa and Zambezi Valleys. Parasites Vectors 2012, 5, 282. [Google Scholar] [CrossRef]
- Franco, J.R.; Cecchi, G.; Priotto, G.; Paone, M.; Diarra, A.; Grout, L.; Mattioli, C.R.; Argaw, D. Monitoring the elimination of human African trypanosomiasis: Update to 2014. PLoS Negl. Trop. Dis. 2017, 11, e0005585. [Google Scholar] [CrossRef]
- Central Statistics Office. 2010 Population Census and Housing; National Analytical Report; Central Statistics Office: Lusaka, Zambia, 2012. [Google Scholar]
- Padgett, D. Qualitative and Mixed Methods in Public Health; Sage Publications: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Bourgeault, I.; Dingwall, R.; de Vries, R. Sage Handbook on Qualitative Health Research; Sage Publications: London, UK, 2010. [Google Scholar]
- WHO. Control and Surveillance of African Trypanosomiasis—Report of a WHO Expert Committee; WHO Technical Report Series No. 984; WHO: Geneva, Switzerland, 2013; Available online: http://apps.who.int/iris/bitstream/10665/95732/1/9789241209847_eng.pdf (accessed on 23 June 2021).
- Bukachi, S.A.; Mumbo, A.A.; Alak, A.C.D.; Sebit, W.; Rumunu, J.; Bie’ler, S.; Ndung’, M.J. Knowledge, attitudes and practices about human African trypanosomiasis and their implications in designing intervention strategies for Yei county, South Sudan. PLoS Negl. Trop. Dis. 2018, 12, e000682. [Google Scholar] [CrossRef]
- Simarro, P.P.; Cecchi, G.; Franco, J.R.; Paone, M.; Diarra, A.; Priotto, G.; Mattioli, C.R.; Jannin, G.J. Monitoring the Progress towards the Elimination of Gambiense Human African Trypanosomiasis. PLoS Negl. Trop. Dis. 2015, 9, e0003785. [Google Scholar] [CrossRef]
- Mulenga, M.G.; Henning, L.; Chilongo, K.; Mubamba, C.; Namangala, B.; Gummow, B. Insights into the Control and Management of Human and Bovine African Trypanosomiasis in Zambia between 2009 and 2019—A Review. Trop. Med. Infect. Dis. 2020, 5, 115. [Google Scholar] [CrossRef]
- Mulenga, G.; Likwa, D.; Namangala, B. Assessing the capacity to diagnose human African trypanosomiasis among health care personnel from Chama and Mambwe districts of eastern Zambia. BMC Res. Notes 2015, 8, 433. [Google Scholar] [CrossRef]
- Kunda, J.; Rudovic, K.; Mfinanga, G.S. Knowledge of causes, clinical features and diagnosis of common zoonoses among medical practitioners in Tanzania. BMC Infect Dis. 2008, 8, 162. [Google Scholar]
- Lejon, V.; Jacobs, J.; Simarroc, P.P. Elimination of sleeping sickness hindered by difficult diagnosis. Bull. World Health Organ. 2013, 91, 718. [Google Scholar] [CrossRef]
- Shaw, A.P. Assessing the economics of animal trypanosomosis in Africa—history and current perspectives. Onderstepoort J. Vet. Res. 2009, 76, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Namangala, B.; Oparaocha, E.; Kajino, K.; Hayashida, K.; Moonga, L.; Inoue, N.; Suzuki, Y.; Sugimoto, C. Preliminary Investigation of Trypanosomosis in Exotic Dog Breeds from Zambia’s Luangwa and Zambezi Valleys Using LAMP. Am. J. Trop. Med. Hyg. 2013, 89, 116. [Google Scholar] [CrossRef] [PubMed]
- Anderson, N.E.; Mubanga, J.; Fevere, M.E.; Pikozzi, K.; Eisler, C.M.; Thomas, R.; Welburn, C.S. Characterisation of the Wildlife Reservoir Community for Human and Animal Trypanosomiasis in the Luangwa Valley, Zambia. PLoS Negl. Trop. Dis. 2011, 5, e1211. [Google Scholar] [CrossRef] [PubMed]
- Laohasinnarong, D.; Goto, Y.; Asada, M.; Nakao, R.; Hayashida, K.; Kajino, K.; Kawazu, S.; Sugimoto, C.; Inoue, N.; Namangala, B. Studies of trypanosomiasis in the Luangwa valley, north-eastern Zambia. Parasites Vectors 2015, 8, 497. [Google Scholar] [CrossRef]
- Wissmann, B.; Machila, N.; Picozzi, K.; Fèvre, M.E.; Bronsvoort, M.B.; Handel, G.; Welburn, C.S. Factors Associated with Acquisition of Human Infective and Animal Infective Trypanosome Infections in Domestic Livestock in Western Kenya. PLoS Negl. Trop. Dis. 2011, 5, e941. [Google Scholar] [CrossRef]
- Haji, J.I.; Sugimoto, C.; Kajino, K.; Malele, I.; Simukoko, H.; Chitambo, H.; Namangala, B. Determination of the prevalence of trypanosome species in cattle from Monduli district, northern Tanzania, by loop mediated isothermal amplification. Trop. Anim. Health Prod. 2015, 47, 1139–1143. [Google Scholar] [CrossRef]
- Mukadi, P.; Lejon, V.; Barbé, B.; Gillet, P.; Nyembo, C.; Lukuka, A.; Likwela, J.; Lumbala, C.; Mbaruku, J.; Vander Veken, W.; et al. Performance of Microscopy for the Diagnosis of Malaria and Human African Trypanosomiasis by Diagnostic Laboratories in the Democratic Republic of the Congo: Results of a Nation-Wide External Quality Assessment. PLoS ONE 2016, 11, e0146450. [Google Scholar] [CrossRef]
- Palmer, J.J.; Surur, I.E.; Goch, W.G.; Mayen, A.M.; Lindner, K.A.; Pittet, A.; Kasparian, S.; Checchi, F.; Whitty, C.J.M. Syndromic Algorithms for Detection of Gambiense Human African Trypanosomiasis in South Sudan. PLoS Negl. Trop. Dis. 2013, 7, e2003. [Google Scholar] [CrossRef]
- Odiit, M.; Coleman, P.G.; Liu, W.C.; McDermott, J.J.; Fèvre, E.M.; Welburn, S.C.; Woolhouse, M.E.J. Quantifying the level of under-detection of Trypanosoma brucei rhodesiense sleeping sickness cases. Trop. Med. Int. Health 2005, 10, 840–849. [Google Scholar] [CrossRef]
- Torreele, E.; Bourdin, T.B.; Tweats, D.; Kaiser, M.; Brun, R.; Mazué, G.; Bray, A.M.; Pécoul, B. Fexinidazole—A New Oral Nitroimidazole Drug Candidate Entering Clinical Development for the Treatment of Sleeping Sickness. PLoS Negl. Trop. Dis. 2010, 4, e923. [Google Scholar] [CrossRef] [Green Version]
- WHO. Trypanosomiasis, Human African (Sleeping Sickness); WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Moore, S.; Shrestha, S.; Tomlinson, W.K.; Vuong, H. Predicting the effect of climate change on African trypanosomiasis: Integrating epidemiology with parasite and vector biology. J. R. Soc. Interface 2012, 9, 817–830. [Google Scholar] [CrossRef]
- Anderson, N.E.; Mubanga, J.; Machila, N.; Atkinson, P.M.; Dzingirai, V.; Welburn, S.C. Sleeping sickness and its relationship with development and biodiversity conservation in the Luangwa Valley, Zambia. Parasite Vectors 2015, 15, 224. [Google Scholar] [CrossRef] [Green Version]
- WHO. Control and Surveillance of African Trypanosomiasis—Report of a WHO Expert Committee; WHO Technical Report Series No. 881; WHO: Geneva, Switzerland, 1998; Available online: http://apps.who.int/iris/bitstream/10665/42087/1/WHO_TRS_881.Pdf (accessed on 22 October 2021).



| Year | Male | Female | Chama | Mambwe | Mpika | Rufunsa | Total |
|---|---|---|---|---|---|---|---|
| 2004 | 3 | 0 | 3 | 0 | 0 | 0 | 3 |
| 2005 | 2 | 0 | 2 | 0 | 0 | 0 | 2 |
| 2006 | 4 | 0 | 3 | 0 | 1 | 0 | 4 |
| 2007 | 2 | 0 | 2 | 0 | 0 | 0 | 2 |
| 2008 | 3 | 2 | 3 | 1 | 1 | 0 | 5 |
| 2009 | 2 | 0 | 0 | 1 | 0 | 1 | 2 |
| 2010 | 3 | 1 | 4 | 0 | 0 | 4 | |
| 2011 | 1 | 1 | 0 | 0 | 1 | 1 | 2 |
| 2012 | 3 | 0 | 1 | 0 | 0 | 2 | 3 |
| 2013 | 9 | 5 | 1 | 1 | 8 | 4 | 14 |
| 2014 | 13 | 10 | 3 | 0 | 17 | 3 | 23 |
| Total | 45 | 19 | 22 | 3 | 28 | 11 | 64 |
| District | No. of Cases in 2014 | No. of Cases in 2013 | Total No. of Cases in 2013 and 2014 | Rural Population at Risk | Total District Population at Risk | Land Cover (km2) |
|---|---|---|---|---|---|---|
| Chama | 3 | 1 | 4 | 92,620 | 99,434 | 17,630 |
| Rufunsa | 3 | 4 | 7 | 71,000 | 71,000 | 9614 |
| Mpika | 17 | 8 | 25 | 154,199 | 191,329 | 40,935 |
| Mambwe | 2 | 1 | 3 | 59,076 | 64,627 | 5294 |
| Total | 23 | 14 | 37 | 376,895 | 649,946 | 73,477 |
| Mambwe District | Rufunsa District | ||||||
|---|---|---|---|---|---|---|---|
| Health centre | Kamoto M/H | Masumba | Kakumbi HC | Nsefu RHC | St Luke M/H | Lukwipa RHC | Shikabeta Rural H/C |
| Referral centre | UTH | Kamoto M/H | Kamoto M/H | Kamoto M/H | St Luke M/H | St Luke M/H | St Luke M/H |
| Equipment | Microsc * | 0 | 1 | 0 | Microsc * | 0 | 0 |
| Number of qualified staff | 5 | 3 | 4 | 2 | 9 | 1 | 1 |
| Number of staff able to diagnose HAT | 4 | 0 | 3 | 0 | 7 | 1 | 1 |
| Number of laboratory staff | 2 | 0 | 2 | 0 | 3 | 0 | 0 |
| Laboratory staff refresher course available? | No | No | No | No | No | No | No |
| Number of HAT cases Encountered | 1 | 0 | 1 | 0 | 10 | 1 | 0 |
| Pharmacy? | Yes | No | Yes | No | Yes | No | No |
| Drugs available? | No | No | No | No | No | Yes | No |
| Chama District | Mpika District | |||
|---|---|---|---|---|
| Health centre | Chama DH | Kamfupu RHC | Chilonga | Nabwalya RHC |
| Referral centre | UTH | Chama DHMT | Chilonga M/H | Chilonga M/H |
| Equipment | Microsc * | 0 | Microsc * | 0 |
| Number of qualified staff | 8 | 1 | 9 | 2 |
| Number of staff able to diagnose HAT | 6 | 0 | 4 | 0 |
| Number of laboratory staff | 2 | 0 | 2 | 0 |
| Laboratory staff refresher course available? | No | No | No | No |
| Number of HAT cases encountered | <10 | <10 | <10 | 0 |
| Pharmacy? | Yes | No | Yes | No |
| Drugs available? | No | No | No | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mwiinde, A.M.; Simuunza, M.; Namangala, B.; Chama-Chiliba, C.M.; Machila, N.; Anderson, N.E.; Atkinson, P.M.; Welburn, S.C. Healthcare Management of Human African Trypanosomiasis Cases in the Eastern, Muchinga and Lusaka Provinces of Zambia. Trop. Med. Infect. Dis. 2022, 7, 270. https://doi.org/10.3390/tropicalmed7100270
Mwiinde AM, Simuunza M, Namangala B, Chama-Chiliba CM, Machila N, Anderson NE, Atkinson PM, Welburn SC. Healthcare Management of Human African Trypanosomiasis Cases in the Eastern, Muchinga and Lusaka Provinces of Zambia. Tropical Medicine and Infectious Disease. 2022; 7(10):270. https://doi.org/10.3390/tropicalmed7100270
Chicago/Turabian StyleMwiinde, Allan Mayaba, Martin Simuunza, Boniface Namangala, Chitalu Miriam Chama-Chiliba, Noreen Machila, Neil E. Anderson, Peter M. Atkinson, and Susan C. Welburn. 2022. "Healthcare Management of Human African Trypanosomiasis Cases in the Eastern, Muchinga and Lusaka Provinces of Zambia" Tropical Medicine and Infectious Disease 7, no. 10: 270. https://doi.org/10.3390/tropicalmed7100270
APA StyleMwiinde, A. M., Simuunza, M., Namangala, B., Chama-Chiliba, C. M., Machila, N., Anderson, N. E., Atkinson, P. M., & Welburn, S. C. (2022). Healthcare Management of Human African Trypanosomiasis Cases in the Eastern, Muchinga and Lusaka Provinces of Zambia. Tropical Medicine and Infectious Disease, 7(10), 270. https://doi.org/10.3390/tropicalmed7100270









