Geographical Pattern Evolution of Health Resources in China: Spatio-Temporal Dynamics and Spatial Mismatch
Abstract
1. Introduction
2. Literature Review
2.1. Medical Resource Change and Allocation Spatial Inequality Analysis Are the Mainstream, and the Research on Geospatial Health Is Insufficient
2.2. Qualitative, Statistical and Regression Analysis Are the Mainstream, and Lack of Support for Evidence-Based Decision Making
3. Materials and Methods
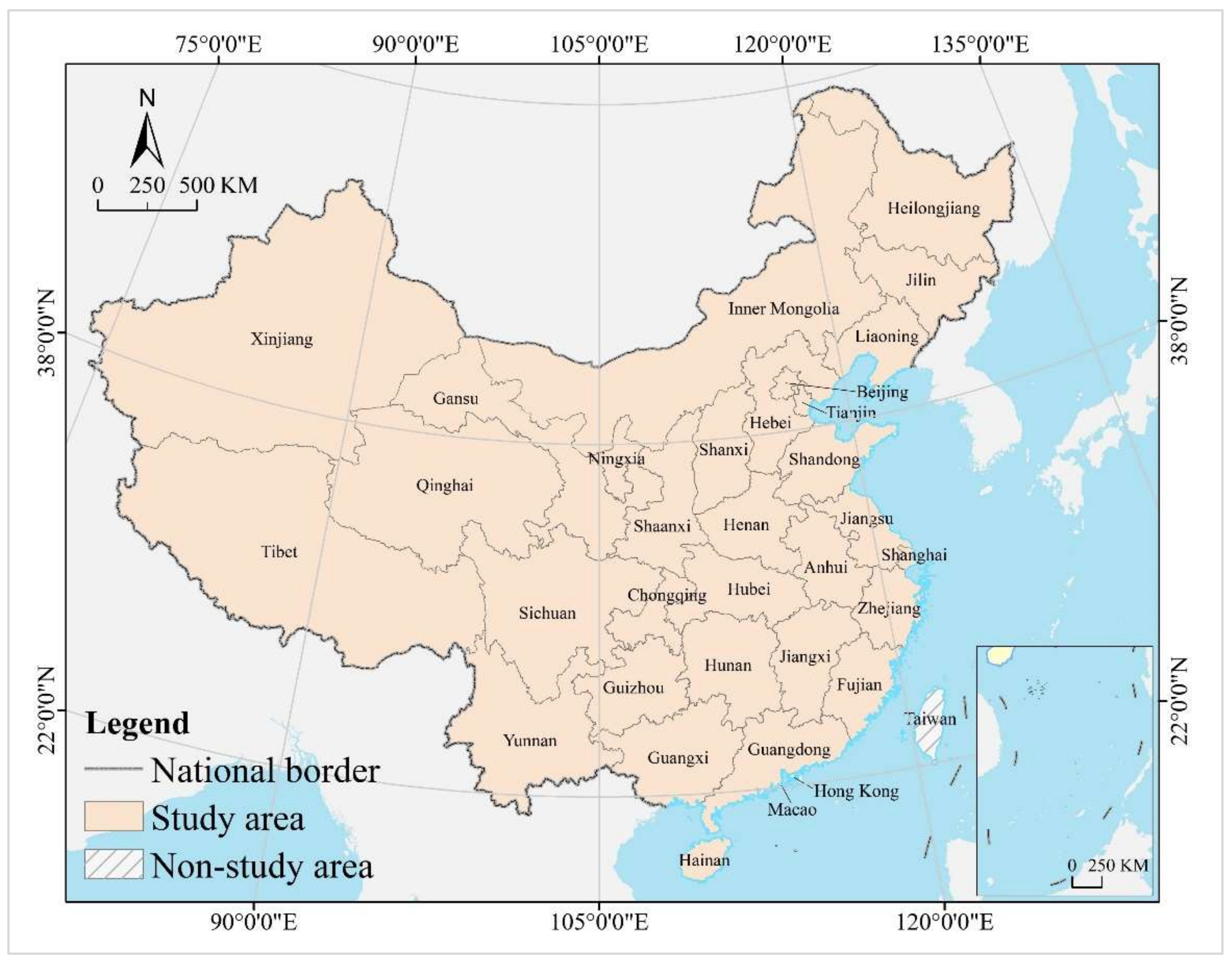
3.1. Study Area
3.2. Research Steps and Data Sources
3.3. Research Methods
3.3.1. Boston Consulting Group Matrix
3.3.2. Spatial Mismatch Index
3.3.3. Spatial Econometric Model
3.3.4. Geodetector
4. Results
4.1. Spatio-Temporal Dynamics
4.1.1. Spatial Pattern
4.1.2. Change Process
4.1.3. Evolution Trend
4.2. Spatial Mismatch Analysis
4.2.1. Demand: Population Potential Consumption
- (1)
- Spatial Mismatch Type of Population
- (2)
- Mismatch Index Contribution Rate of Population
4.2.2. Supply: Economic Carrying Capacity
- (1)
- Spatial Mismatch Type of GDP
- (2)
- Mismatch Index Contribution Rate of GDP
4.3. Driving Mechanism
4.3.1. Influence Factor
4.3.2. Interaction Effect
5. Discussion
5.1. Extended Thinking and External Evidence
5.2. Sustainable Development Spatial Strategies
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| City | Hospitals | Doctors | Beds | GDP | Population | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2010 | 2020 | 2010 | 2020 | 2010 | 2020 | 2010 | 2020 | 2010 | 2020 | |
| Beijing | 0.0100 | 0.0104 | 0.0273 | 0.0258 | 0.0194 | 0.0140 | 0.0323 | 0.0357 | 0.0147 | 0.0155 |
| Tianjin | 0.0048 | 0.0057 | 0.0118 | 0.0106 | 0.0102 | 0.0075 | 0.0211 | 0.0139 | 0.0097 | 0.0098 |
| Hebei | 0.0869 | 0.0850 | 0.0534 | 0.0501 | 0.0522 | 0.0486 | 0.0467 | 0.0358 | 0.0539 | 0.0529 |
| Shanxi | 0.0439 | 0.0402 | 0.0337 | 0.0261 | 0.0326 | 0.0246 | 0.0211 | 0.0174 | 0.0268 | 0.0248 |
| Inner Mongolia | 0.0241 | 0.0240 | 0.0206 | 0.0189 | 0.0195 | 0.0178 | 0.0267 | 0.0171 | 0.0185 | 0.0170 |
| Liaoning | 0.0371 | 0.0334 | 0.0386 | 0.0298 | 0.0427 | 0.0346 | 0.0422 | 0.0248 | 0.0328 | 0.0302 |
| Jilin | 0.0207 | 0.0250 | 0.0228 | 0.0203 | 0.0240 | 0.0190 | 0.0198 | 0.0122 | 0.0206 | 0.0170 |
| Heilongjiang | 0.0236 | 0.0200 | 0.0320 | 0.0231 | 0.0334 | 0.0278 | 0.0237 | 0.0135 | 0.0287 | 0.0225 |
| Shanghai | 0.0050 | 0.0058 | 0.0210 | 0.0194 | 0.0220 | 0.0167 | 0.0393 | 0.0382 | 0.0173 | 0.0176 |
| Jiangsu | 0.0330 | 0.0349 | 0.0560 | 0.0611 | 0.0563 | 0.0588 | 0.0948 | 0.1015 | 0.0590 | 0.0601 |
| Zhejiang | 0.0320 | 0.0336 | 0.0430 | 0.0490 | 0.0385 | 0.0397 | 0.0634 | 0.0638 | 0.0408 | 0.0459 |
| Anhui | 0.0245 | 0.0287 | 0.0377 | 0.0374 | 0.0393 | 0.0448 | 0.0283 | 0.0382 | 0.0447 | 0.0433 |
| Fujian | 0.0288 | 0.0275 | 0.0243 | 0.0261 | 0.0236 | 0.0238 | 0.0337 | 0.0434 | 0.0277 | 0.0295 |
| Jiangxi | 0.0364 | 0.0359 | 0.0282 | 0.0273 | 0.0260 | 0.0314 | 0.0216 | 0.0254 | 0.0335 | 0.0320 |
| Shandong | 0.0715 | 0.0830 | 0.0788 | 0.0763 | 0.0799 | 0.0711 | 0.0896 | 0.0722 | 0.0719 | 0.0721 |
| Henan | 0.0808 | 0.0730 | 0.0721 | 0.0698 | 0.0684 | 0.0733 | 0.0528 | 0.0543 | 0.0705 | 0.0705 |
| Hubei | 0.0366 | 0.0347 | 0.0426 | 0.0400 | 0.0419 | 0.0452 | 0.0365 | 0.0429 | 0.0429 | 0.0407 |
| Hunan | 0.0634 | 0.0548 | 0.0452 | 0.0456 | 0.0488 | 0.0571 | 0.0367 | 0.0413 | 0.0493 | 0.0471 |
| Guangdong | 0.0479 | 0.0546 | 0.0723 | 0.0747 | 0.0627 | 0.0621 | 0.1053 | 0.1094 | 0.0783 | 0.0895 |
| Guangxi | 0.0349 | 0.0331 | 0.0325 | 0.0351 | 0.0300 | 0.0325 | 0.0219 | 0.0219 | 0.0346 | 0.0356 |
| Hainan | 0.0050 | 0.0060 | 0.0063 | 0.0070 | 0.0054 | 0.0064 | 0.0047 | 0.0055 | 0.0065 | 0.0072 |
| Chongqing | 0.0187 | 0.0205 | 0.0195 | 0.0224 | 0.0216 | 0.0259 | 0.0181 | 0.0247 | 0.0216 | 0.0228 |
| Sichuan | 0.0793 | 0.0809 | 0.0570 | 0.0612 | 0.0629 | 0.0714 | 0.0393 | 0.0480 | 0.0603 | 0.0594 |
| Guizhou | 0.0271 | 0.0282 | 0.0188 | 0.0272 | 0.0220 | 0.0304 | 0.0105 | 0.0176 | 0.0261 | 0.0274 |
| Yunnan | 0.0244 | 0.0260 | 0.0253 | 0.0341 | 0.0328 | 0.0357 | 0.0165 | 0.0242 | 0.0345 | 0.0335 |
| Tibet | 0.0053 | 0.0068 | 0.0020 | 0.0030 | 0.0018 | 0.0020 | 0.0012 | 0.0019 | 0.0023 | 0.0026 |
| Shaanxi | 0.0381 | 0.0342 | 0.0317 | 0.0331 | 0.0297 | 0.0299 | 0.0232 | 0.0259 | 0.0280 | 0.0280 |
| Gansu | 0.0285 | 0.0256 | 0.0168 | 0.0170 | 0.0189 | 0.0189 | 0.0094 | 0.0089 | 0.0192 | 0.0177 |
| Qinghai | 0.0062 | 0.0063 | 0.0043 | 0.0048 | 0.0043 | 0.0045 | 0.0031 | 0.0030 | 0.0042 | 0.0042 |
| Ningxia | 0.0044 | 0.0045 | 0.0048 | 0.0053 | 0.0049 | 0.0045 | 0.0039 | 0.0039 | 0.0047 | 0.0051 |
| Xinjiang | 0.0171 | 0.0178 | 0.0194 | 0.0182 | 0.0243 | 0.0199 | 0.0124 | 0.0136 | 0.0164 | 0.0184 |
| City | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Beijing | 0.0550 | 0.0751 | 0.0548 | 0.0350 | 0.0443 | 0.0124 | 0.0597 | 0.0321 | 0.0591 | 0.0593 |
| Tianjin | 0.0165 | 0.0463 | 0.0192 | 0.0091 | 0.0429 | 0.0088 | 0.0211 | 0.0093 | 0.0446 | 0.0162 |
| Hebei | 0.0340 | 0.0221 | 0.0382 | 0.0324 | 0.0304 | 0.0574 | 0.0381 | 0.0433 | 0.0292 | 0.0413 |
| Shanxi | 0.0164 | 0.0230 | 0.0229 | 0.0172 | 0.0317 | 0.0230 | 0.0267 | 0.0230 | 0.0328 | 0.0208 |
| Inner Mongolia | 0.0154 | 0.0328 | 0.0205 | 0.0121 | 0.0342 | 0.0147 | 0.0200 | 0.0199 | 0.0321 | 0.0147 |
| Liaoning | 0.0244 | 0.0268 | 0.0265 | 0.0229 | 0.0365 | 0.0274 | 0.0380 | 0.0219 | 0.0394 | 0.0298 |
| Jilin | 0.0117 | 0.0231 | 0.0108 | 0.0098 | 0.0317 | 0.0148 | 0.0211 | 0.0159 | 0.0349 | 0.0130 |
| Heilongjiang | 0.0123 | 0.0194 | 0.0115 | 0.0130 | 0.0332 | 0.0186 | 0.0227 | 0.0213 | 0.0348 | 0.0197 |
| Shanghai | 0.0515 | 0.0710 | 0.0704 | 0.0407 | 0.0452 | 0.0146 | 0.0510 | 0.0289 | 0.0506 | 0.0495 |
| Jiangsu | 0.0981 | 0.0552 | 0.0905 | 0.0946 | 0.0372 | 0.0599 | 0.0727 | 0.0534 | 0.0343 | 0.0754 |
| Zhejiang | 0.0655 | 0.0459 | 0.0724 | 0.0680 | 0.0365 | 0.0388 | 0.0524 | 0.0444 | 0.0333 | 0.0639 |
| Anhui | 0.0360 | 0.0289 | 0.0321 | 0.0468 | 0.0295 | 0.0471 | 0.0352 | 0.0404 | 0.0262 | 0.0350 |
| Fujian | 0.0379 | 0.0482 | 0.0307 | 0.0475 | 0.0348 | 0.0285 | 0.0284 | 0.0277 | 0.0271 | 0.0264 |
| Jiangxi | 0.0225 | 0.0259 | 0.0250 | 0.0265 | 0.0306 | 0.0344 | 0.0223 | 0.0340 | 0.0250 | 0.0264 |
| Shandong | 0.0712 | 0.0329 | 0.0655 | 0.0746 | 0.0319 | 0.0775 | 0.0644 | 0.0554 | 0.0330 | 0.0693 |
| Henan | 0.0487 | 0.0253 | 0.0416 | 0.0574 | 0.0281 | 0.0820 | 0.0464 | 0.0575 | 0.0279 | 0.0526 |
| Hubei | 0.0405 | 0.0339 | 0.0251 | 0.0459 | 0.0318 | 0.0402 | 0.0406 | 0.0540 | 0.0299 | 0.0371 |
| Hunan | 0.0393 | 0.0287 | 0.0300 | 0.0415 | 0.0297 | 0.0514 | 0.0325 | 0.0391 | 0.0349 | 0.0380 |
| Guangdong | 0.1137 | 0.0402 | 0.1291 | 0.1026 | 0.0375 | 0.0778 | 0.0854 | 0.0939 | 0.0283 | 0.0889 |
| Guangxi | 0.0209 | 0.0202 | 0.0171 | 0.0200 | 0.0274 | 0.0404 | 0.0227 | 0.0331 | 0.0267 | 0.0289 |
| Hainan | 0.0061 | 0.0251 | 0.0081 | 0.0050 | 0.0305 | 0.0069 | 0.0064 | 0.0117 | 0.0240 | 0.0062 |
| Chongqing | 0.0240 | 0.0356 | 0.0209 | 0.0301 | 0.0352 | 0.0238 | 0.0222 | 0.0230 | 0.0364 | 0.0223 |
| Sichuan | 0.0463 | 0.0265 | 0.0425 | 0.0531 | 0.0287 | 0.0622 | 0.0482 | 0.0546 | 0.0328 | 0.0527 |
| Guizhou | 0.0165 | 0.0211 | 0.0178 | 0.0200 | 0.0269 | 0.0309 | 0.0198 | 0.0300 | 0.0227 | 0.0205 |
| Yunnan | 0.0230 | 0.0237 | 0.0211 | 0.0250 | 0.0253 | 0.0322 | 0.0248 | 0.0377 | 0.0276 | 0.0272 |
| Tibet | 0.0017 | 0.0239 | 0.0022 | 0.0019 | 0.0181 | 0.0025 | 0.0020 | 0.0076 | 0.0109 | 0.0016 |
| Shaanxi | 0.0228 | 0.0302 | 0.0225 | 0.0245 | 0.0317 | 0.0273 | 0.0330 | 0.0270 | 0.0367 | 0.0223 |
| Gansu | 0.0090 | 0.0164 | 0.0087 | 0.0093 | 0.0264 | 0.0180 | 0.0162 | 0.0196 | 0.0274 | 0.0135 |
| Qinghai | 0.0028 | 0.0232 | 0.0030 | 0.0022 | 0.0304 | 0.0039 | 0.0040 | 0.0091 | 0.0349 | 0.0046 |
| Ningxia | 0.0036 | 0.0248 | 0.0042 | 0.0033 | 0.0329 | 0.0049 | 0.0058 | 0.0063 | 0.0333 | 0.0047 |
| Xinjiang | 0.0129 | 0.0244 | 0.0148 | 0.0078 | 0.0286 | 0.0176 | 0.0166 | 0.0250 | 0.0292 | 0.0182 |
References
- Roadevin, C.; Hill, H. How can we decide a fair allocation of healthcare resources during a pandemic? J. Med. Ethic 2021, 47, e84. [Google Scholar] [CrossRef] [PubMed]
- Grover, S.; McClelland, A.; Furnham, A. Preferences for scarce medical resource allocation: Differences between experts and the general public and implications for the COVID-19 pandemic. Br. J. Health Psychol. 2020, 25, 889–901. [Google Scholar] [CrossRef] [PubMed]
- Colwell, R.R.; Machlis, G.E. The Role of GeoHealth in Science During Crisis. GeoHealth 2019, 3, 176–177. [Google Scholar] [CrossRef] [PubMed]
- Zhou, J.; Liu, C.; Xu, W.; Li, L.; Zhou, M. Research on the Spatial Adaptability of China’s New Urbanization and Urban Medical Resources. Sci. Geogr. Sin. 2021, 41, 1168–1177. [Google Scholar] [CrossRef]
- Asamani, J.A.; Alugsi, S.A.; Ismaila, H.; Nabyonga-Orem, J. Balancing Equity and Efficiency in the Allocation of Health Resources—Where Is the Middle Ground? Healthcare 2021, 9, 1257. [Google Scholar] [CrossRef]
- Love-Koh, J.; Griffin, S.; Kataika, E.; Revill, P.; Sibandze, S.; Walker, S. Methods to promote equity in health resource allocation in low- and middle-income countries: An overview. Glob. Health 2020, 16, 6–12. [Google Scholar] [CrossRef]
- Pinho, M.; Araújo, A. How to fairly allocate scarce medical resources? Controversial preferences of healthcare professionals with different personal characteristics. Heal. Econ. Policy Law 2021, 17, 398–415. [Google Scholar] [CrossRef] [PubMed]
- Hassoun, N.; Herlitz, A. Distributing global health resources: Contemporary issues in political philosophy. Philos. Compass 2019, 14, e12632. [Google Scholar] [CrossRef]
- De Vries, D.H.; Pool, R. The Influence of Community Health Resources on Effectiveness and Sustainability of Community and Lay Health Worker Programs in Lower-Income Countries: A Systematic Review. PLoS ONE 2017, 12, e0170217. [Google Scholar] [CrossRef]
- Withanachchi, N.; Uchida, Y.; Nanayakkara, S.; Samaranayake, D.; Okitsu, A. Resource allocation in public hospitals: Is it effective? Health Policy 2007, 80, 308–313. [Google Scholar] [CrossRef]
- Bergquist, R.; Manda, S. The world in your hands: GeoHealth then and now. Geospat. Heal. 2019, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yang, H.; Pan, J. Gaining from rational health planning: Spatial reallocation of top-tier general hospital beds in China. Comput. Ind. Eng. 2021, 157, 107344. [Google Scholar] [CrossRef]
- Zhao, H.; Wang, Q.; Zhu, L.; Li, X.; Tian, H. Spatial-temporal evolution and influencing factors of health resources in underde-veloped areas based on Geodetectors. Arid. Land Geogr. 2021, 44, 594–603. [Google Scholar] [CrossRef]
- Yan, J.; Xu, L.; Tan, Y. The Spatial Pattern and Dynamic Evolution of Public Health Expenditure in China. Econ. Geogr. 2017, 37, 82–91. [Google Scholar] [CrossRef]
- Tian, L.; Zhang, J.; Wang, F.; Li, X.; Zheng, W.; Luo, J. Rural Public Medical Resources Allocation Spatial Optimization Towards Equity and Efficiency Access: A Case Study on Xiantao City, Hubei Province. Sci. Geogr. Sin. 2019, 39, 1455–1463. [Google Scholar] [CrossRef]
- Griffin, S.; Claxton, K.; Sculpher, M. Decision analysis for resource allocation in health care. J. Heal. Serv. Res. Policy 2008, 13, 23–30. [Google Scholar] [CrossRef]
- Myllyla, Y.; Kaivo-Oja, J. Integrating Delphi methodology to some classical concepts of the Boston consulting group framework: Arctic maritime technology BCG Delphi foresight-a pilot study from Finland. Eur. J. Futures Res. 2015, 3, 2. [Google Scholar] [CrossRef]
- Salvati, L.; Venanzoni, G.; Serra, P.; Carlucci, M. Scattered or polycentric? Untangling urban growth in three southern European metropolitan regions through exploratory spatial data analysis. Ann. Reg. Sci. 2016, 57, 1–29. [Google Scholar] [CrossRef]
- Shaltynov, A.; Rocha, J.; Jamedinova, U.; Myssayev, A. Assessment of primary healthcare accessibility and inequality in north-eastern Kazakhstan. Geospat. Health 2022, 17, 1046. [Google Scholar] [CrossRef]
- Behr, M.; Le Borgne, P.; Baicry, F.; Lavoignet, C.E.; Berard, L.; Tuzin, N.; Oberlin, M.; Bilbault, P. French national emergency de-partment’s crisis: The outcome of growing gap between health resources and needs? Rev. Med. Interne 2020, 41, 684–692. [Google Scholar] [CrossRef]
- Omrani-Khoo, H.; Lotfi, F.; Safari, H.; Zargar Balaye Jame, S.; Moghri, J.; Shafii, M. Equity in Distribution of Health Care Resources; Assessment of Need and Access, Using Three Practical Indicators. Iran. J. Public Health 2013, 42, 1299–1308. [Google Scholar] [PubMed]
- Dong, E.H.; Liu, S.P.; Chen, M.J.; Wang, H.M.; Chen, L.W.; Xu, T.; Wang, T.; Zhang, L.F. Differences in regional distribution and in-equality in health-resource allocation at hospital and primary health centre levels: A longitudinal study in Shanghai, China. BMJ Open 2021, 10, e035635. [Google Scholar] [CrossRef] [PubMed]
- Chai, K.C.; Zhang, Y.B.; Chang, K.C. Regional Disparity of Medical Resources and Its Effect on Mortality Rates in China. Front. Public Health 2020, 8, 8. [Google Scholar] [CrossRef] [PubMed]
- Fang, P.; Hu, R.; Han, Q. Effects of healthcare reform on health resource allocation and service utilization in 1110 Chinese county hospitals: Data from 2006 to 2012. Int. J. Heal. Plan. Manag. 2017, 32, 400–415. [Google Scholar] [CrossRef]
- Yang, C.C. Measuring health indicators and allocating health resources: A DEA-based approach. Health Care Manag. Sci. 2017, 20, 365–378. [Google Scholar] [CrossRef]
- Retzlaff-Roberts, D.; Chang, C.F.; Rubin, R.M. Technical efficiency in the use of health care resources: A comparison of OECD countries. Health Policy 2004, 69, 55–72. [Google Scholar] [CrossRef]
- Liu, L.N.; Xu, W.; Su, Y.X.; Zhou, X. Evaluation of Health Resource Allocation Efficiency Based on Data Envelopment Analysis 2014–2018 in Two Dimensions of Time-Region. Discret. Dyn. Nat. Soc. 2022, 2021, 8273415. [Google Scholar] [CrossRef]
- Giraldes, M.D. Allocative efficiency in the use of health resources in Portugal. J. Public Health Med. 1999, 21, 55–59. [Google Scholar] [CrossRef][Green Version]
- Hayhow, C.M.; Brabander, D.J.; Jim, R.; Lively, M.; Filippelli, G.M. Addressing the Need for Just GeoHealth Engagement: Evolving Models for Actionable Research That Transform Communities. Geohealth 2021, 5, e2021GH000496. [Google Scholar] [CrossRef]
- Gorris, M.E.; Anenberg, S.C.; Goldberg, D.L.; Kerr, G.H.; Stowell, J.D.; Tong, D.I.; Zaitchik, B.F. Shaping the Future of Science: COVID-19 Highlighting the Importance of GeoHealth. Geohealth 2021, 5, e2021GH000412. [Google Scholar] [CrossRef]
- Sa, J.H.G.; Rebelo, M.S.; Brentani, A.; Grisi, S.; Gutierrez, M.A. GeoHealth: A Georeferenced System for Health Data Analysis in Primary Care. IEEE Lat. Am. Trans. 2012, 10, 1352–1356. [Google Scholar] [CrossRef]
- Maire, N.; Hegnauer, M.; Nguyen, D.; Godelmann, L.; Peterhans, B.; Hoffmann, A.; de Savigny, D.; Tanner, M. The Health Re-sources Allocation Model (HRAM) for the 21st century. Geospat. Health 2012, 6, 295–298. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Anselmi, L.; Lagarde, M.; Hanson, K. Going beyond horizontal equity: An analysis of health expenditure allocation across geographic areas in Mozambique. Soc. Sci. Med. 2015, 130, 216–224. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, D.; Muirhead, D.; Gilson, L. Geographic patterns of deprivation in South Africa: Informing health equity analyses and public resource allocation strategies. Health Policy Plan. 2002, 17, 30–39. [Google Scholar] [CrossRef]
- Hall, W.; Smith, N.; Mitton, C.; Urquhart, B.; Bryan, S. Assessing and Improving Performance: A Longitudinal Evaluation of Priority Setting and Resource Allocation in a Canadian Health Region. Int. J. Health Policy Manag. 2018, 7, 328–335. [Google Scholar] [CrossRef]
- Sendi, P.; Gafni, A.; Birch, S.; Walter, S.D. Incorporating Portfolio Uncertainty in Decision Rules for Healthcare Resource Al-location. Healthcare 2021, 9, 325. [Google Scholar] [CrossRef]
- Mihaylova, B.; Briggs, A.; O’Hagan, A.; Thompson, S.G. Review of Statistical Methods for Analysing Healthcare Resources and Costs. Health Econ. 2011, 20, 897–916. [Google Scholar] [CrossRef]
- Giacomini, M.; Hurley, J.; DeJean, D. Fair reckoning: A qualitative investigation of responses to an economic health resource allocation survey. Health Expect. 2014, 17, 174–185. [Google Scholar] [CrossRef]
- Kolasa, K.; Lewandowski, T. Does it matter whose opinion we seek regarding the allocation of healthcare resources?—A case study. BMC Health Serv. Res. 2016, 15, 564. [Google Scholar] [CrossRef]
- Frew, E.; Breheny, K. Health economics methods for public health resource allocation: A qualitative interview study of decision makers from an English local authority. Health Econ. Policy Law 2019, 15, 128–140. [Google Scholar] [CrossRef]
- Freedman, A.M.; Kuester, S.A.; Jernigan, J. Evaluating Public Health Resources: What Happens When Funding Disappears? Prev. Chronic Dis. 2014, 10, 130130. [Google Scholar] [CrossRef] [PubMed]
- Ahlert, M.; Schwettmann, L. Allocating health care resources: A questionnaire experiment on the predictive success of rules. Int. J. Equity Health 2017, 16, 112. [Google Scholar] [CrossRef] [PubMed]
- Furnham, A.; Ofstein, A. Ethical ideology and the allocation of scarce medical resources. Br. J. Med. Psychol. 1997, 70, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Zhang, L.X.; Boswell, M. Inequities in the allocation of medical resources in China’s Township Health Centers. China Agric. Econ. Rev. 2016, 8, 637–646. [Google Scholar] [CrossRef]
- Bhattacharyya, S.; Issac, A.; Girase, B.; Guha, M.; Schellenberg, J.; Avan, B.I. “There Is No Link Between Resource Allocation and Use of Local Data”: A Qualitative Study of District-Based Health Decision-Making in West Bengal, India. Int. J. Environ. Res. Public Health 2020, 179, 8283. [Google Scholar] [CrossRef]
- Krones, C.J.; Willis, S.; Steinau, G.; Schumpelick, V. Fair allocation of reduced resources in the German health care system—The patient’s view. Chirurg 2007, 78, 543–547. [Google Scholar] [CrossRef]
- Smith, N.; Mitton, C.; Bryan, S.; Davidson, A.; Urquhart, B.; Gibson, J.L.; Peacock, S.; Donaldson, C. Decision maker perceptions of resource allocation processes in Canadian health care organizations: A national survey. BMC Health Serv. Res. 2013, 13, 247. [Google Scholar] [CrossRef]
- Pourat, N.; Chen, X.; Lu, C.N.; Zhou, W.H.; Hoang, H.; Sripipatana, A. Assessing clinical quality performance and staffing ca-pacity differences between urban and rural Health Resources and Services Administration-funded health centers in the United States: A cross sectional study. PLoS ONE 2020, 15, e0242844. [Google Scholar] [CrossRef]
- Avelino, G.; Barberia, L.G.; Biderman, C. Governance in managing public health resources in Brazilian municipalities. Health Policy Plan. 2014, 29, 694–702. [Google Scholar] [CrossRef]
- Jain, R.; Mishra, S. Climate change modeling based public health resource planning for Narmada basin, India. Indian J. Geo-Mar. Sci. 2016, 45, 621–638. [Google Scholar]
- Lopes, L.D.N.; Acurcio, F.D.; Diniz, S.D.; Coelho, T.L.; Andrade, E.I.G. (Un)Equitable distribution of health resources and the judicial-ization of healthcare: 10 years of experience in Brazil. Int. J. Equity Health 2019, 18, 10. [Google Scholar] [CrossRef] [PubMed]
- Owili, P.O.; Hsu, Y.H.E.; Chern, J.Y.; Chiu, C.H.M.; Wang, B.; Huang, K.C.; Muga, M.A. Perceptions and Attitudes of Health Professionals in Kenya on National Health Care Resource Allocation Mechanisms: A Structural Equation Modeling. PLoS ONE 2015, 10, e0127160. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.S.; Wang, S.H.; Zhao, H.J.; Zhou, X.; Zhang, L.D.; Shi, J.P. Does descending health resources reform impact patient low-level hospital selection behavior? Evidence from Zhejiang, China. Arch. Public Health 2021, 79, 179. [Google Scholar] [CrossRef] [PubMed]
- Pinho, M.M.; Veiga, P.A.C.V. Cost-utility analysis as a mechanism for allocation of health care resources: A review of the debate. Cad. Saude Publica 2009, 25, 239–250. [Google Scholar] [CrossRef]
- John, T.M.; Millum, J.; Wasserman, D. How to Allocate Scarce Health Resources Without Discriminating Against People with Disabilities. Econ. Philos. 2017, 33, 161–186. [Google Scholar] [CrossRef]
- Powell-Jackson, T.; Mills, A. A review of health resource tracking in developing countries. Health Policy Plan. 2007, 22, 353–362. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rivero-Garcia, A.; Santos-Gonzalez, I.; Hernandez-Goya, C.; Caballero-Gil, P. A secure approach to monitoring emergency health resources. EURASIP J. Wirel. Commun. Netw. 2021, 2021, 202. [Google Scholar] [CrossRef]
- Pichon-Riviere, A.; Augustovski, F.; Marti, S.G.; Alfie, V.; Sampietro-Colom, L. The link between health technology assessment and decision making for the allocation of health resources in Latin America. Int. J. Technol. Assess. Health Care 2020, 36, 173–178. [Google Scholar] [CrossRef]
- Bekemeier, B.; Chen, A.L.T.; Kawakyu, N.; Yang, Y. Local Public Health Resource Allocation Limited Choices and Strategic Deci-sions. Am. J. Prev. Med. 2013, 45, 769–775. [Google Scholar] [CrossRef]
- Gong, S.; Chen, Y. Temporal-spatial relationship between health resources and residents’ health in Southern China. Geogr. Res. 2020, 39, 115–128. [Google Scholar] [CrossRef]
- Angelis, A.; Kanavos, P.; Montibeller, G. Resource Allocation and Priority Setting in Health Care: A Multi-criteria Decision Analysis Problem of Value? Glob. Policy 2017, 8, 76–83. [Google Scholar] [CrossRef]
- Wipfli, H.; Kumie, A.; Atuyambe, L.; Oguge, O.; Rugigana, E.; Zacharias, K.; Simane, B.; Samet, J.; Berhane, K. The GEOHealth Hub for Eastern Africa: Contributions and Lessons Learned. Geohealth 2021, 5, e2021GH000406. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.P.; Xu, J.; Jiang, X.F.; Li, C.F.; Li, H.M.; Song, S.H.; Huang, E.D.; Meng, Q.Y. Trends in health resource disparities in primary health care institutions in Liaoning Province in Northeast China. Int. J. Equity Health 2018, 17, 178. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Xu, Y.J.; Ren, J.P.; Sun, L.Q.; Liu, C.J. Inequality in the distribution of health resources and health services in China: Hospitals versus primary care institutions. Int. J. Equity Health 2017, 16, 42. [Google Scholar] [CrossRef]
- Radinmanesh, M.; Azar, F.E.; Hashjin, A.A.; Najafi, B.; Majdzadeh, R. A review of appropriate indicators for need-based financial resource allocation in health systems. BMC Health Serv. Res. 2021, 21, 674. [Google Scholar] [CrossRef]
- Igoumenidis, M.; Kiekkas, P.; Papastavrou, E. The gap between macroeconomic and microeconomic health resources allocation decisions: The case of nurses. Nurs. Philos. 2020, 21, e12283. [Google Scholar] [CrossRef]
- Segev, R. Well-being and fairness in the distribution of scarce health resources. J. Med. Philos. 2005, 30, 231–260. [Google Scholar] [CrossRef]
- Williams, I.; Bryan, S. Understanding the limited impact of economic evaluation in health care resource allocation: A conceptual framework. Health Policy 2007, 80, 135–143. [Google Scholar] [CrossRef]
- Wu, J.S.; Fu, J.Y.; Wang, H.L.; Zhao, Y.H.; Yi, T.Y. Identifying Spatial Matching between the Supply and Demand of Medical Resource and Accessing Carrying Capacity: A Case Study of Shenzhen, China. Int. J. Environ. Res. Public Health 2022, 19, 2354. [Google Scholar] [CrossRef]
- Qin, X.Z.; Hsieh, C.R. Economic growth and the geographic maldistribution of health care resources: Evidence from China, 1949–2010. China Econ. Rev. 2015, 31, 228–246. [Google Scholar] [CrossRef]
- Haghparast-Bidgoli, H.; Kiadaliri, A.A.; Skordis-Worrall, J. Do economic evaluation studies inform effective healthcare resource allocation in Iran? A critical review of the literature. Cost Eff. Resour. Alloc. 2014, 12, 15. [Google Scholar] [CrossRef] [PubMed]
- Selvaraj, D.; McClelland, A.; Furnham, A. Allocating Scarce Medical Resources: Using Social Usefulness as a Criterion. Ethics Behav. 2019, 29, 274–286. [Google Scholar] [CrossRef]
- Zhao, S.; Zhang, P.; Li, W. A Study on Evaluation of Influencing Factors for Sustainable Development of Smart Construction Enterprises: Case Study from China. Buildings 2021, 11, 221. [Google Scholar] [CrossRef]
- Kain, J.F. Housing Segregation, Negro Employment, and Metropolitan Decentralization. Q. J. Econ. 1968, 82, 175–197. [Google Scholar] [CrossRef]
- Rogerson, P.A. Scan Statistics Adjusted for Global Spatial Autocorrelation. Geogr. Anal. 2022. In print. [Google Scholar] [CrossRef]
- Watson, S.I. Efficient design of geographically-defined clusters with spatial autocorrelation. J. Appl. Stat. 2021, 1–19. [Google Scholar] [CrossRef]
- Zhang, P.; Li, W.; Zhao, K.; Zhao, S. Spatial Pattern and Driving Mechanism of Urban–Rural Income Gap in Gansu Province of China. Land 2021, 10, 1002. [Google Scholar] [CrossRef]
- Wang, J.F.; Li, X.H.; Christakos, G.; Liao, Y.L.; Zhang, T.; Gu, X.; Zheng, X.Y. Geographical detectors-based health risk assessment and its application in the neural tube defects study of the Heshun region, China. Int. J. Geogr. Inf. Sci. 2010, 24, 107–127. [Google Scholar] [CrossRef]
- Wang, J.F.; Xu, C.D. Geodetector: Principle and prospective. Acta Geogr. Sin. 2017, 72, 116–134. [Google Scholar]
- Zhao, S.; Yan, Y.; Han, J. Industrial Land Change in Chinese Silk Road Cities and Its Influence on Environments. Land. 2021, 10, 806. [Google Scholar] [CrossRef]
- Liu, W.; Liu, Y.; Twum, P.; Li, S.X. National equity of health resource allocation in China: Data from 2009 to 2013. Int. J. Equity Health 2016, 15, 68. [Google Scholar] [CrossRef] [PubMed]
- Dlouhy, M. Measuring Geographic Inequalities: Dealing with Multiple Health Resources by Data Envelopment Analysis. Front. Public Health 2018, 6, 53. [Google Scholar] [CrossRef] [PubMed]
- Dong, E.H.; Xu, J.; Sun, X.T.; Xu, T.; Zhang, L.F.; Wang, T. Differences in regional distribution and inequality in health-resource allocation on institutions, beds, and workforce: A longitudinal study in China. Arch. Public Health 2021, 79, 78. [Google Scholar] [CrossRef] [PubMed]
- Yu, M.; He, S.J.; Wu, D.X.; Zhu, H.P.; Webster, C. Examining the Multi-Scalar Unevenness of High-Quality Healthcare Resources Distribution in China. Int. J. Environ. Res. Public Health 2019, 16, 2813. [Google Scholar] [CrossRef] [PubMed]
- Dell, A.J.; Kahn, D. Geographical maldistribution of surgical resources in South Africa: A review of the number of hospitals, hospital beds and surgical beds. SAMJ S. Afr. Med. J. 2017, 107, 1099–1105. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.; Shallcross, D. Geographic distribution of hospital beds throughout China: A county-level econometric analysis. Int. J. Equity Health 2016, 15, 179. [Google Scholar] [CrossRef] [PubMed]
- Lu, L.M.; Zeng, J.C. Inequalities in the geographic distribution of hospital beds and doctors in traditional Chinese medicine from 2004 to 2014. Int. J. Equity Health 2018, 17, 165. [Google Scholar] [CrossRef]
- Chen, J.; Lin, Z.C.; Li, L.A.; Li, J.; Wang, Y.Y.; Pan, Y.; Yang, J.; Xu, C.C.; Zeng, X.J.; Xie, X.X. Ten years of China’s new healthcare reform: A longitudinal study on changes in health resources. BMC Public Health 2021, 21, 2272. [Google Scholar] [CrossRef]
- Wang, J.; Wu, H.T. Health Shocks and Unbalanced Growth of Medical Resources: Evidence from the SARS Epidemic in China. Int. J. Health Serv. 2021, 52, 47–60. [Google Scholar] [CrossRef]
- Meliala, A.; Hort, K.; Trisnantoro, L. Addressing the unequal geographic distribution of specialist doctors in Indonesia: The role of the private sector and effectiveness of current regulations. Soc. Sci. Med. 2013, 82, 30–34. [Google Scholar] [CrossRef]
- Yao, H.H.; Zhan, C.H.; Sha, X.P. Current situation and distribution equality of public health resource in China. Arch. Public Health 2020, 78, 86. [Google Scholar] [CrossRef] [PubMed]
- Zhu, B.; Hsieh, C.W.; Mao, Y. Addressing the Licensed Doctor Maldistribution in China: A Demand-And-Supply Perspective. Int. J. Environ. Res. Public Health 2019, 16, 1753. [Google Scholar] [CrossRef] [PubMed]
- Chien, G.S.; Chee-Khoon, C.; Wai, V.H.C.; Ng, C.W. Equitable Distribution of Public Hospitals According to Health Needs in Malaysia: Does It Exist or Not? Asia-Pac. J. Public Health 2015, 27, 79S–85S. [Google Scholar] [CrossRef]
- Ge, E.J.; Su, M.; Zhao, R.L.; Huang, Z.Y.; Shan, Y.N.; Wei, X.L. Geographical disparities in access to hospital care in Ontario, Canada: A spatial coverage modelling approach. BMJ Open 2021, 11, e041474. [Google Scholar] [CrossRef] [PubMed]
- Bruni, M.L.; Mammi, I. Spatial effects in hospital expenditures: A district level analysis. Health Econ. 2017, 26, 63–77. [Google Scholar] [CrossRef]
- Shinjo, D.; Aramaki, T. Geographic distribution of healthcare resources, healthcare service provision, and patient flow in Japan: A cross sectional study. Soc. Sci. Med. 2012, 75, 1954–1963. [Google Scholar] [CrossRef] [PubMed]
- Paramita, S.A.; Yamazaki, C.; Setiawati, E.P.; Koyama, H. Distribution trends of Indonesia’s health care resources in the decen-tralization era. Int. J. Health Plan. Manag. 2018, 33, E586–E596. [Google Scholar] [CrossRef]
- Ismail, M. Regional disparities in the distribution of Sudan’s health resources. East. Mediterr. Health J. 2020, 26, 1105–1114. [Google Scholar] [CrossRef]
- Woldemichael, A.; Takian, A.; Sari, A.A.; Olyaeemanesh, A. Inequalities in healthcare resources and outcomes threatening sus-tainable health development in Ethiopia: Panel data analysis. BMJ Open 2019, 9, e022923. [Google Scholar] [CrossRef]
- Chavehpour, Y.; Rashidian, A.; Woldemichael, A.; Takian, A. Inequality in geographical distribution of hospitals and hospital beds in densely populated metropolitan cities of Iran. BMC Health Serv. Res. 2019, 19, 614. [Google Scholar] [CrossRef]
- Rezaei, S.; Karyani, A.K.; Fallah, R.; Matin, B.K. Relative inequalities in geographic distribution of health care resources in Ker-manshah province, Islamic Republic of Iran. East. Mediterr. Health J. 2017, 22, 20–27. [Google Scholar] [CrossRef]
- Erdenee, O.; Paramita, S.A.; Yamazaki, C.; Koyama, H. Distribution of health care resources in Mongolia using the Gini coefficient. Hum. Resour. Health 2017, 15, 56. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.; Tenedorio, J.A.; Santana, P. Disparities in Geographical Access to Hospitals in Portugal. ISPRS Int. J. Geo-Inf. 2020, 9, 567. [Google Scholar] [CrossRef]
- Russo, L.X. Effect of More Doctors (Mais Medicos) Program on geographic distribution of primary care physicians. Cienc. Saude Coletiva 2021, 26, 1585–1594. [Google Scholar] [CrossRef] [PubMed]
- Horev, T.; Pesis-Katz, I.; Mukamel, D.B. Trends in geographic disparities in allocation of health care resources in the US. Health Policy 2004, 68, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Kaur, G.; Prinja, S.; Lakshmi, P.V.M.; Downey, L.; Sharma, D.; Teerawattananon, Y. Criteria Used for Priority-Setting for Public Health Resource Allocation in Low- and Middle-Income Countries: A Systematic Review. Int. J. Technol. Assess. Health Care 2019, 35, 474–483. [Google Scholar] [CrossRef]
- Alvarez, A.A.A. Threshold considerations in fair allocation of health resources: Justice beyond scarcity. Bioethics 2007, 21, 426–438. [Google Scholar] [CrossRef]
- Li, J.M.; Chen, X.L.; Han, X.L.; Zhang, G.H. Spatiotemporal matching between medical resources and population ageing in China from 2008 to 2017. BMC Public Health 2020, 20, 845. [Google Scholar] [CrossRef]
- Zheng, X.Y.; Wang, J.; Li, X.L.; Yu, Y.H. On the supply of China’s healthcare resources in a decentralized healthcare system. Soc. Sci. J. 2015, 52, 449–458. [Google Scholar] [CrossRef]
- Guo, Q.B.; Luo, K.; Hu, R.D. The Spatial Correlations of Health Resource Agglomeration Capacities and Their Influencing Factors: Evidence from China. Int. J. Environ. Res. Public Health 2020, 17, 8705. [Google Scholar] [CrossRef]
- Song, C.; Wang, Y.D.; Yang, X.; Yang, Y.L.; Tang, Z.Y.; Wang, X.L.; Pan, J. Spatial and Temporal Impacts of Socioeconomic and En-vironmental Factors on Healthcare Resources: A County-Level Bayesian Local Spatiotemporal Regression Modeling Study of Hos-pital Beds in Southwest China. Int. J. Environ. Res. Public Health 2020, 17, 5890. [Google Scholar] [CrossRef] [PubMed]
- Ding, L.; Zhang, N.; Mao, Y. Addressing the maldistribution of health resources in Sichuan Province, China: A county-level analysis. PLoS ONE 2021, 16, e0250526. [Google Scholar] [CrossRef]
- Guo, Q.B.; Luo, K. Concentration of Healthcare Resources in China: The Spatial-Temporal Evolution and Its Spatial Drivers. Int. J. Environ. Res. Public Health 2020, 16, 4606. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.D.; Liu, Y.; Hu, N.J.; Sun, X.W.; Wu, Q. Governance mechanism for medical security and economic development. J. Natl. Sch. Adm. 2016, 73–76. [Google Scholar] [CrossRef]
- Qian, Y.; Yang, J. Analysis on Equity of Health Resource Allocation in Gansu Province Based on Gini Coefficient and Agglom-eration Degree. Med. Soc. 2021, 34, 11–16. [Google Scholar] [CrossRef]
- Eckenwiler, L.A. A Global Ecological Ethic for Human Health Resources. J. Bioethical Inq. 2020, 17, 575–580. [Google Scholar] [CrossRef] [PubMed]
- Pu, L.D. Fairness of the Distribution of Public Medical and Health Resources. Front. Public Health 2021, 9, 768728. [Google Scholar] [CrossRef]
- Zhang, X.Y.; Zhao, L.; Cui, Z.; Wang, Y.G. Study on Equity and Efficiency of Health Resources and Services Based on Key In-dicators in China. PLoS ONE 2016, 10, e0144809. [Google Scholar] [CrossRef]
- Simonsson, T.; Sjolund, K.; Bumming, P.; Ahlman, H.; Nilsson, B.; Oden, A. Reducing uncertainty in health-care resource alloca-tion. Br. J. Cancer 2007, 96, 1834–1838. [Google Scholar] [CrossRef]
- Gaynor, M.; Anderson, G.F. Uncertain Demand, The Structure of Hospital Costs, and the Cost of Empty Hospital Beds. J. Health Econ. 1995, 14, 291–317. [Google Scholar] [CrossRef]
- Asthana, S.; Gibson, A.; Halliday, J. The medicalisation of health inequalities and the English NHS: The role of resource allocation. Health Econ. Policy Law 2013, 8, 167–183. [Google Scholar] [CrossRef] [PubMed]
- Jakovljevic, M.B. Resource allocation strategies in Southeastern European health policy. Eur. J. Health Econ. 2013, 14, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Smith, N.; Mitton, C.; Davidson, A.; Williams, I. A politics of priority setting: Ideas, interests and institutions in healthcare resource allocation. Public Policy Adm. 2014, 29, 331–347. [Google Scholar] [CrossRef]














| Type | Code | Indicator | Data Source |
|---|---|---|---|
| Dependent variable | Hospital | China statistical yearbook China health statistical yearbook | |
| Doctor | |||
| Bed | |||
| Independent variable | Service industry added value | China statistical yearbook Provincial statistical yearbook | |
| Per capita GDP | |||
| Government revenue | |||
| Social consumption | |||
| Urbanization rate | |||
| Children and elderly population | |||
| High quality (university or above) population | |||
| Health care government investment | |||
| Residents’ medical services consumption | |||
| Medical insurance fund expenditure | |||
| Demand and supply variable | Population | ||
| GDP |
| Indicator Name | Global Moran’s I | p | Z | ||
|---|---|---|---|---|---|
| Evolution trend | Hospitals | 0.14 | 0.10 | 1.39 | |
| doctors | 0.15 | 0.08 | 1.45 | ||
| beds | 0.23 | 0.02 | 2.23 | ||
| Spatial mismatch type of population | Hospitals | 2010 | 0.21 | 0.03 | 2.06 |
| 2020 | 0.28 | 0.00 | 2.69 | ||
| Doctors | 2010 | 0.15 | 0.06 | 1.67 | |
| 2020 | −0.10 | 0.30 | −0.55 | ||
| Beds | 2010 | 0.18 | 0.05 | 1.72 | |
| 2020 | 0.07 | 0.21 | 0.80 | ||
| Spatial mismatch type of GDP | Hospitals | 2010 | 0.23 | 0.03 | 2.24 |
| 2020 | 0.24 | 0.02 | 2.42 | ||
| Doctors | 2010 | 0.30 | 0.01 | 2.81 | |
| 2020 | 0.46 | 0.00 | 4.25 | ||
| Beds | 2010 | 0.15 | 0.07 | 1.49 | |
| 2020 | 0.19 | 0.04 | 1.94 | ||
| Indicator | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hospital | q | 0.54 | 0.03 | 0.48 | 0.33 | 0.06 | 0.80 | 0.34 | 0.58 | 0.10 | 0.36 | 0.52 |
| P | 0.01 | 0.34 | 0.05 | 0.08 | 0.17 | 0.00 | 0.04 | 0.02 | 0.09 | 0.04 | 0.05 | |
| Doctor | q | 0.74 | 0.03 | 0.66 | 0.83 | 0.00 | 0.92 | 0.73 | 0.87 | 0.04 | 0.76 | 0.79 |
| P | 0.00 | 0.57 | 0.01 | 0.00 | 0.92 | 0.00 | 0.00 | 0.00 | 0.29 | 0.00 | 0.05 | |
| Bed | q | 0.71 | 0.08 | 0.59 | 0.75 | 0.01 | 0.95 | 0.60 | 0.83 | 0.07 | 0.64 | 0.72 |
| P | 0.00 | 0.66 | 0.02 | 0.00 | 0.65 | 0.00 | 0.01 | 0.00 | 0.16 | 0.00 | 0.05 | |
| 0.54 | ||||||||||
| 0.69 | 0.03 | |||||||||
| 0.72 | 0.73 | 0.48 | ||||||||
| 0.63 | 0.61 | 0.74 | 0.33 | |||||||
| 0.72 | 0.09 | 0.73 | 0.64 | 0.06 | ||||||
| 0.85 | 0.88 | 0.88 | 0.91 | 0.87 | 0.80 | |||||
| 0.59 | 0.64 | 0.60 | 0.48 | 0.64 | 0.84 | 0.34 | ||||
| 0.73 | 0.69 | 0.76 | 0.64 | 0.69 | 0.87 | 0.67 | 0.58 | |||
| 0.64 | 0.16 | 0.67 | 0.51 | 0.14 | 0.83 | 0.57 | 0.63 | 0.10 | ||
| 0.66 | 0.69 | 0.61 | 0.45 | 0.71 | 0.85 | 0.47 | 0.72 | 0.63 | 0.36 |
| 0.74 | ||||||||||
| 0.81 | 0.03 | |||||||||
| 0.81 | 0.81 | 0.66 | ||||||||
| 0.91 | 0.89 | 0.92 | 0.83 | |||||||
| 0.85 | 0.07 | 0.83 | 0.91 | 0.00 | ||||||
| 0.97 | 0.96 | 0.97 | 0.98 | 0.96 | 0.92 | |||||
| 0.83 | 0.84 | 0.88 | 0.92 | 0.85 | 0.97 | 0.73 | ||||
| 0.95 | 0.89 | 0.93 | 0.93 | 0.89 | 0.97 | 0.96 | 0.87 | |||
| 0.83 | 0.21 | 0.81 | 0.85 | 0.10 | 0.93 | 0.87 | 0.88 | 0.04 | ||
| 0.93 | 0.92 | 0.90 | 0.93 | 0.93 | 0.98 | 0.80 | 0.94 | 0.91 | 0.76 |
| 0.71 | ||||||||||
| 0.88 | 0.08 | |||||||||
| 0.78 | 0.83 | 0.59 | ||||||||
| 0.87 | 0.95 | 0.89 | 0.75 | |||||||
| 0.85 | 0.17 | 0.79 | 0.91 | 0.01 | ||||||
| 0.97 | 0.99 | 0.97 | 0.98 | 0.97 | 0.95 | |||||
| 0.81 | 0.90 | 0.86 | 0.86 | 0.83 | 0.97 | 0.60 | ||||
| 0.93 | 0.92 | 0.90 | 0.94 | 0.89 | 0.98 | 0.91 | 0.83 | |||
| 0.79 | 0.27 | 0.74 | 0.80 | 0.10 | 0.96 | 0.81 | 0.87 | 0.07 | ||
| 0.90 | 0.90 | 0.87 | 0.91 | 0.90 | 0.97 | 0.68 | 0.93 | 0.89 | 0.64 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhou, Y.; Zhao, K.; Han, J.; Zhao, S.; Cao, J. Geographical Pattern Evolution of Health Resources in China: Spatio-Temporal Dynamics and Spatial Mismatch. Trop. Med. Infect. Dis. 2022, 7, 292. https://doi.org/10.3390/tropicalmed7100292
Zhou Y, Zhao K, Han J, Zhao S, Cao J. Geographical Pattern Evolution of Health Resources in China: Spatio-Temporal Dynamics and Spatial Mismatch. Tropical Medicine and Infectious Disease. 2022; 7(10):292. https://doi.org/10.3390/tropicalmed7100292
Chicago/Turabian StyleZhou, Yong, Kaixu Zhao, Junling Han, Sidong Zhao, and Jingyuan Cao. 2022. "Geographical Pattern Evolution of Health Resources in China: Spatio-Temporal Dynamics and Spatial Mismatch" Tropical Medicine and Infectious Disease 7, no. 10: 292. https://doi.org/10.3390/tropicalmed7100292
APA StyleZhou, Y., Zhao, K., Han, J., Zhao, S., & Cao, J. (2022). Geographical Pattern Evolution of Health Resources in China: Spatio-Temporal Dynamics and Spatial Mismatch. Tropical Medicine and Infectious Disease, 7(10), 292. https://doi.org/10.3390/tropicalmed7100292










