Assessment of Knowledge, Attitudes, and Practices towards Rift Valley Fever among Livestock Farmers in Selected Districts of Malawi
Abstract
1. Introduction
2. Materials and Methods
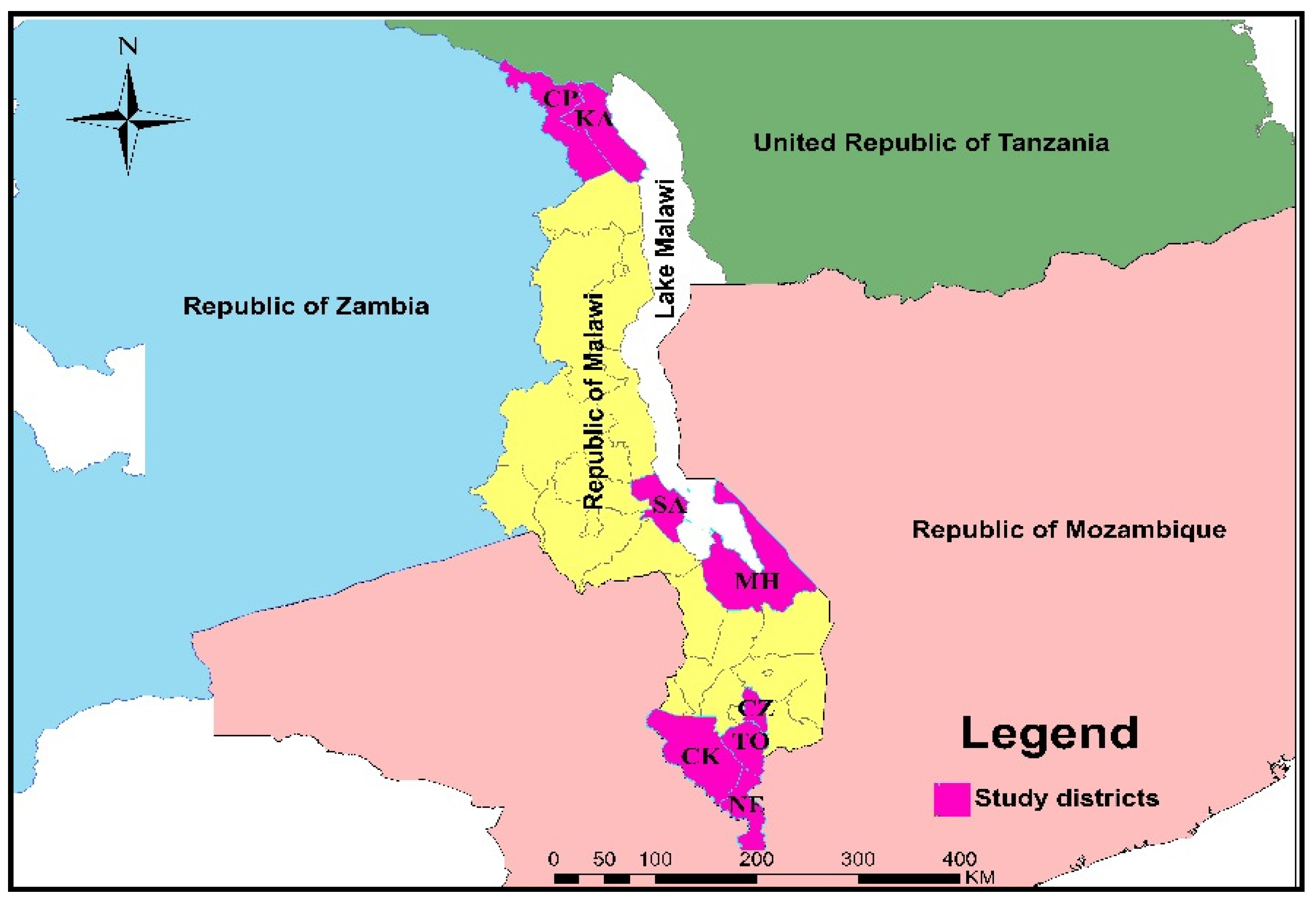
2.1. Study Site
2.2. Sample Size
2.3. Data Collection Instruments
2.4. Participant Identification and Data Collection
2.5. Determining KAP Scores
2.6. Data Processing and Analysis
2.7. Ethics Statement
3. Results
3.1. Socio-Demographic Characteristics
3.1.1. Knowledge of Participants of the RVF and KAP Score
3.1.2. Management Practices towards RVF and KAP Score
3.1.3. Attitude of Participants towards RVF and KAP Score
3.1.4. Mean Knowledge, Attitude, and Practices across the Socio-Demographic Characteristics
3.2. Analysis of the Association between RVF Knowledge of Participants and Potential Predictors of Knowledge
3.3. Predictors of RVF Knowledge for the Participants
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adams, M.J.; Lefkowitz, E.J.; King, A.M.Q.; Harrach, B.; Harrison, R.L.; Knowles, N.J.; Kropinski, A.M.; Krupovic, M.; Kuhn, J.H.; Mushegian, A.; et al. Changes to taxonomy and the International Code of Virus Classification and Nomenclature ratified by the International Committee on Taxonomy of Viruses (2017). Arch. Virol. 2017, 162, 2505–2538. [Google Scholar] [CrossRef]
- Turell, M.J.; Linthicum, K.J.; Patrican, L.A.; Davies, F.G.; Kairo, A.; Bailey, C.L. Vector competence of selected African mosquito (Diptera: Culicidae) species for Rift Valley fever virus. J. Med. Entomol. 2008, 45, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Linthicum, K.J.; Britch, S.C.; Anyamba, A. Rift Valley Fever: An Emerging Mosquito-Borne Disease. Annu. Rev. Entomol. 2016, 61, 395–415. [Google Scholar] [CrossRef] [PubMed]
- Cornel, A.J.; Lee, Y.; Almeida, A.P.G.; Johnson, T.; Mouatcho, J.; Venter, M.; de Jager, C.; Braack, L. Mosquito community composition in South Africa and some neighboring countries. Parasit. Vectors 2018, 11, 331. [Google Scholar] [CrossRef] [PubMed]
- Budasha, N.H.; Gonzalez, J.P.; Sebhatu, T.T.; Arnold, E. Rift Valley fever seroprevalence and abortion frequency among livestock of Kisoro district, South Western Uganda (2016): A prerequisite for zoonotic infection. BMC Vet. Res. 2018, 14, 271. [Google Scholar] [CrossRef] [PubMed]
- OIE. Available online: https://www.oie.int/app/uploads/2021/03/rift-valley-fever.pdf (accessed on 21 October 2021).
- Baudin, M.; Jumaa, A.M.; Jomma, H.J.E.; Karsany, M.S.; Bucht, G.; Näslund, J.; Ahlm, C.; Evander, M.; Mohamed, N. Association of Rift Valley fever virus infection with miscarriage in Sudanese women: A cross-sectional study. Lancet Glob. Health 2016, 4, e864–e871. [Google Scholar] [CrossRef]
- Ahmed, A.; Ali, Y.; Elduma, A.; Eldigail, M.H.; Mhmoud, R.A.; Mohamed, N.S.; Ksiazek, T.G.; Dietrich, I.; Weaver, S.C. Unique Outbreak of Rift Valley Fever in Sudan, 2019. Emerg. Infect Dis. 2020, 26, 3030–3033. [Google Scholar] [CrossRef]
- Chevalier, V.; Pépin, M.; Plée, L.; Lancelot, R. Rift Valley fever--a threat for Europe? Euro surveillance. Euro. Comm. Dis. Bull. 2010, 15, 322–329. [Google Scholar] [CrossRef]
- Sindato, C.; Karimuribo, E.; Mboera, L.E. The epidemiology and socio-economic impact of rift valley fever epidemics in Tanzania: A review. Tanzan. J. Health Res. 2011, 13, 305–318. [Google Scholar] [CrossRef]
- Peyre, M.; Chevalier, V.; Abdo-Salem, S.; Velthuis, A.; Antoine-Moussiaux, N.; Thiry, E.; Roger, F.A. Systematic Scoping Study of the Socio-Economic Impact of Rift Valley Fever: Research Gaps and Needs. Zoonoses Public Health 2015, 62, 309–325. [Google Scholar] [CrossRef]
- Javelle, E.; Lesueur, A.; Pommier de Santi, V.; de Laval, F.; Lefebvre, T.; Holweck, G.; Durand, G.A.; Leparc-Goffart, I.; Texier, G.; Simon, F. The challenging management of Rift Valley Fever in humans: Literature review of the clinical disease and algorithm proposal. Ann. Clin. Microbiol. Antimicrob. 2020, 19, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Sindato, C.; Karimuribo, E.; Mboera, E.G. The epidemiology and socio-economic impact of Rift Valley fever epidemics in Tanzania: A review. Onderstepoort. J. Vet. Res. 2012, 79, 410–412. [Google Scholar] [CrossRef]
- Himeidan, Y.E.; Kweka, E.J.; Mahgoub, M.M.; El Rayah, E.A.; Ouma, J.O. Recent Outbreaks Rift. Val. Fever East Afr. Middle East. Front. Public Health 2014, 2, 169. [Google Scholar] [CrossRef]
- Chengula, A.A.; Mdegela, R.H.; Kasanga, C.J. Socio-economic impact of Rift Valley fever to pastoralists and agro pastoralists in Arusha, Manyara and Morogoro regions in Tanzania. Springerplus 2013, 18, 549. [Google Scholar] [CrossRef] [PubMed]
- WHO. Introduction to Rift Valley Fever Managing Infectious. Hazards. Available online: https://cdn.who.int/media/docs/default-source/documents/emergencies/rift-valley-fever/rvf-presentation.pdf?sfvrsn=9ab8f0d3_4 (accessed on 9 January 2022).
- Petrova, V.; Kristiansen, P.; Norheim, G.; Yimer, S.A. Rift valley fever: Diagnostic challenges and investment needs for vaccine development. BMJ Glob. Health 2020, 5, e002694. [Google Scholar] [CrossRef]
- Bedard, B.G.; Martin, S.W.; Chinombo, D. A prevalence study of bovine tuberculosis and brucellosis in Malawi. P. Vet. Med. 1993, 16, 193–205. [Google Scholar] [CrossRef]
- Baur, I.; Tabin, L.; Banda, M.; Chiumia, D.; Lips, M. Improving dairy production in Malawi: A literature review. Trop. Anim. Health Prod. 2017, 49, 251–258. [Google Scholar] [CrossRef]
- Catley, A.; Alders, R.G.; Wood, J.L.N. Participatory epidemiology: Approaches, methods, experiences. Vet. J. 1992, 191, 151–160. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention. Available online: https://www.cdc.gov/vhf/rvf/outbreaks/summaries.html (accessed on 10 February 2022).
- Blomström, A.L.; Scharin, I.; Stenberg, H.; Figueiredo, J.; Nhambirre, O.; Abilio, A.; Berg, M.; Fafetine, J. Seroprevalence of Rift Valley fever virus in sheep and goats in Zambézia, Mozambique. Infect Ecol. Epidemiol. 2016, 6, 31343. [Google Scholar] [CrossRef][Green Version]
- Ahmed, A.; Makame, J.; Robert, F.; Julius, K.; Mecky, M. Sero-prevalence and spatial distribution of Rift Valley fever infection among agro-pastoral and pastoral communities during Interepidemic period in the Serengeti ecosystem, northern Tanzania. BMC Infect Dis. 2018, 18, 276. [Google Scholar] [CrossRef]
- Saasa, N.; Kajihara, M.; Dautu, G.; Mori-Kajihara, A.; Fukushi, S.; Sinkala, Y.; Morikawa, S.; Mweene, A.; Takada, A.; Yoshimatsu, K.; et al. Expression of a Recombinant Nucleocapsid Protein of Rift Valley Fever Virus in Vero Cells as an Immunofluorescence Antigen and Its Use for Serosurveillance in Traditional Cattle Herds in Zambia. Vect. Borne. Zoonotic. Dis. 2018, 18, 273–277. [Google Scholar] [CrossRef] [PubMed]
- Bryony, J. A Sero-Epidemiological Study of Rift Valley fever in the Zomba Area of Malawi. Master’s Thesis, University of Edinburgh, Centre for Tropical Veterinary Medicine, Royal (Dick) School of Veterinary Studies, Scotland, UK, 1992. [Google Scholar]
- Jost, C.C.; Mariner, J.C.; Roeder, P.L.; Sawitri, E.; Macgregor-Skinner, G.J. Participatory epidemiology in disease surveillance and research. Rev. Sci. Tech. 2007, 26, 537–549. [Google Scholar] [CrossRef] [PubMed]
- Alders, R.G.; Ali, S.N.; Ameri, A.A.; Bagnol, B.; Cooper, T.L.; Gozali, A.; Hidayat, M.M.; Rukambile, E.; Wong, J.T.; Catley, A. Participatory Epidemiology: Principles, Practice, Utility, and Lessons Learnt. Front. Vet. Sci. 2020, 7, 532763. [Google Scholar] [CrossRef]
- Tiongco, M.; Narrod, C.; Scott, R.; Kobayashi, M.; Omiti, J. Understanding Knowledge, Attitude, Perceptions, and Practices for HPAI Risks and Management Options among Kenyan Poultry Producers. In Health and Animal Agriculture in Developing Countries. Natural Resource Management and Policy; Zilberman, D., Otte, J., Roland-Holst, D., Pfeiffer, D., Eds.; Springer: New York, NY, USA, 2012; Volume 36. [Google Scholar]
- Edestein, M. Rift Valley Fever in Malawi. In Proceedings of the Annual Malawi Veterinary Association Conference, Blantyre, Malawi, December 1990. [Google Scholar]
- Cochran, W.G. Sampling Techniques, 3rd ed.; Wiley: New York, NY, USA, 1977. [Google Scholar]
- Adegoke, J.I.; Ajibade, B.L.; Damilola, R.; Abiodun. Knowledge, attitude and practice of preventive measures towards COVID-19 among pregnant women attending selected primary health centre’s in Osogbo, Osun State. Int. J. Nurs. Midwife Health Relat. Cases 2020, 6, 29–45. [Google Scholar]
- Namgyal, J.; Tenzin, T.; Checkley, S.; Lysyk, T.J.; Rinchen, S.; Gurung, R.; Doriee, S.; Couloigner, I.; Cork, S. A knowledge, attitudes, and practices study on ticks and tick-borne diseases in cattle among farmers in a selected area of eastern Bhutan. PLoS ONE 2021, 16, e0247302. [Google Scholar] [CrossRef] [PubMed]
- Habib, M.A.; Dayyab, F.M.; Iliyasu, G.; Habib, A.G. Knowledge, attitude and practice survey of COVID-19 pandemic in Northern Nigeria. PLoS ONE 2021, 16, e0245176. [Google Scholar] [CrossRef] [PubMed]
- Roy, D.; Ghosh, T.K.; Saha, M.; Sarker, S. Assessing Knowledge, Attitude, and Practice towards COVID-19 among Sub Assistant Agriculture Officers: An Empirical Study in Bangladesh. J. Contemp. Stud. Epi. Public Health 2020, 1, ep20009. [Google Scholar] [CrossRef]
- Ngoshe, Y.B.; Avenant, A.; Rostal, M.K.; Karesh, W.B.; Paweska, J.T.; Bagge, W.; Jansen van Vuren, P.; Kemp, A.; Cordel, C.; Msimang, V.; et al. Patterns of Rift Valley fever virus seropositivity in domestic ruminants in central South Africa four years after a large outbreak. Sci. Rep. 2020, 26, 5489. [Google Scholar] [CrossRef]
- Abdi, I.H.; Affognon, H.D.; Wanjoya, A.K.; Onyango-Ouma, W.; Sang, R. Knowledge, Attitudes and Practices (KAP) on Rift Valley Fever among Pastoralist Communities of Ijara District, North Eastern Kenya. PLoS Negl. Trop. Dis. 2015, 9, e0004239. [Google Scholar] [CrossRef]
- CDC, Viral Hemorrhagic Fevers, Chapter 4. Available online: Wwwnc.cdc.gov/travel/yellowbook/2020/travel-related-infectious-diseases/viral-hemorrhagic-fevers (accessed on 30 April 2022).
- Sarker, M.A.; Itohara, Y.; Hoque, M. Determinants of adoption decisions: The case of organic farming in Bangladesh. J. Farming Syst. Res. Ext. 2010, 5, 39–46. [Google Scholar]
- Seyed Abolhasan, S.; Hosain Shabanali, F.; Khalil, K.; Yaser, M.; Abbas, A. Investigating Effective Factors on Attitude of Paddy Growers towards Organic Farming: A Case Study in Babol County in Iran. Res. J. Appl. Sci. Eng. Technol. 2010, 3, 362–367. [Google Scholar]
- Tebug, S.F.; Kasulo, V.; Chikagwa-Malunga, S.; Wiedemann, S.; Roberts, D.J.; Chagunda, M.G.G. Smallholder dairy production in Northern Malawi: Production practices and constraints. Trop. Anim. Health Prod. 2012, 44, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Chingala, G.; Mapiye, C.; Raffrenato, E.; Hoffman, L.; Dzama, K. Determinants of smallholder farmers’ perceptions of impact of climate change on beef production in Malawi. Clim. Change 2017, 142, 129–141. [Google Scholar] [CrossRef]
- Banda, L.J.; Kamwanja, L.A.; Chagunda, M.G.G.; Ashworth, C.J.; Roberts, D.J. Status of dairy cow management and fertility in smallholder farms in Malawi. Trop. Anim. Health Prod. 2012, 44, 715–727. [Google Scholar] [CrossRef]
- Alemayehu, G.; Mamo, G.; Desta, H.; Alemu, B.; Wieland, B. Knowledge, attitude, and practices to zoonotic disease risks from livestock birth products among smallholder communities in Ethiopia. One Health 2021, 12, 100223. [Google Scholar] [CrossRef]
- Shabani, S.S.; Ezekiel, M.J.; Mohamed, M.; Moshiro, C.S. Knowledge, attitudes and practices on Rift Valley fever among agro pastoral communities in Kongwa and Kilombero districts, Tanzania. BMC Infect Dis. 2015, 21, 363. [Google Scholar] [CrossRef]
- Ng’ang’a, C.M.; Bukachi, S.A.; Bett, B.K. Lay perceptions of risk factors for Rift Valley fever in a pastoral community in northeastern Kenya. BMC Public Health 2016, 16, 32. [Google Scholar] [CrossRef][Green Version]
- Lernout, T.; Cardinale, E.; Jego, M.; Desprès, P.; Collet, L.; Zumbo, B.; Tillard, E.; Girard, S.; Filleul, L. Rift Valley Fever in Humans and Animals in Mayotte, an Endemic Situation? PLoS ONE 2013, 8, e74192. [Google Scholar] [CrossRef] [PubMed]
- Owange, N.O.; Ogara, W.O.; Kasiiti, J.; Gathura, P.B.; Okuthe, S.; Sang, R.; Affognon, H.; Onyango-Ouma, W.; Landmann, T.T.O. Perceived risk factors and risk pathways of Rift Valley fever in cattle in Ijara district, Kenya. Onderstepoort. J. Vet. Res. 2014, 81, 1. [Google Scholar] [CrossRef][Green Version]
- Scott, G.M.; Thomson, R.; Malone-Lee, J.; Ridgway, G.L. Cross-infection between animals and man: Possible feline transmission of Staphylococcus aureus infection in humans? J. Hosp. Infect. 1988, 12, 29–34. [Google Scholar] [CrossRef]
- Kabir, S.M.S. Positive attitude can change life. J. Chittagong Univ. Teach. Assoc. 2013, 7, 55–58. [Google Scholar]
- Baur, I.; Chiumia, D.; Gazzarin, C.; Lips, M. Perceived challenges in business development of smallholder dairy farmers in three Malawian Regions. Afri. J. Food Agr. Nutr. Dev. 2017, 17, 12791–12806. [Google Scholar] [CrossRef]
- Azher, B.M. Climate Change Resilience through Enhanced Reproduction and Lactation Performance in Malawian Zebu Cattle. Master’s Thesis, Norwegian University of Life Sciences, Oslo, Norway, 2016. [Google Scholar]
- McGowan, M.R.; Kirkland, P.D.; Richards, S.G.; Littlejohns, I.R. Increased reproductive losses in cattle infected with bovine pestivirus around the time of insemination. Vet. Rec. 1993, 133, 39–43. [Google Scholar] [CrossRef]
- Affognon, H.; Mburu, P.; Hassan, O.A.; Kingori, S.; Ahlm, C.; Sang, R.; Evander, M. Ethnic groups’ knowledge, attitude and practices and Rift Valley fever exposure in Isiolo County of Kenya. PLoS Negl. Trop. Dis. 2017, 11, e0005405. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Regional Office for South-East Asia. Comprehensive Guideline for Prevention and Control of Dengue and Dengue Haemorrhagic Fever. Revised and Expanded Edition. 2011; WHO Regional Office for South-East Asia. Available online: https://apps.who.int/iris/handle/10665/204894 (accessed on 3 December 2021).
- Monje, F.; Erume, J.; Mwiine, F.N.; Kazoora, H.; Okech, S.G. Knowledge, attitude and practices about rabies management among human and animal health professionals in Mbale District, Uganda. One Health Outlook 2020, 14, 2–24. [Google Scholar] [CrossRef] [PubMed]
| Variable | Category | Frequency | Proportion (%) n = 400 | 95% CI |
|---|---|---|---|---|
| Gender | ||||
| Male | 269 | 67.25 | 62.38–71.78 | |
| Female | 131 | 32.75 | 28.21–37.62 | |
| Age (years) | ||||
| 18–25 | 44 | 11.00 | 8.19–14.58 | |
| 26–35 | 55 | 13.75 | 10.38–17.33 | |
| 36–45 | 142 | 35.50 | 30.85–40.43 | |
| ≥46 | 159 | 39.75 | 34.95–44.75 | |
| Education | ||||
| None | 42 | 10.50 | 7.75–14.03 | |
| Primary | 270 | 67.50 | 62.63–72.02 | |
| Secondary | 85 | 21.25 | 17.41–25.65 | |
| Tertiary | 3 | 0.75 | 0.19–2.36 | |
| Marital Status | ||||
| Married | 352 | 88.00 | 84.31–90.93 | |
| Single | 18 | 4.50 | 2.77–7.15 | |
| Divorced | 24 | 6.00 | 3.96–8.92 | |
| Widowed | 6 | 1.50 | 0.16–3.40 | |
| Herd size | ||||
| <25 | 379 | 94.75 | 91.96–96.64 | |
| ≥25 | 21 | 5.25 | 3.36–8.04 | |
| District | ||||
| CP | 39 | 9.75 | 7.11–13.19 | |
| KA | 45 | 11.25 | 8.40–14.86 | |
| SA | 60 | 15.00 | 11.72–18.97 | |
| MH | 54 | 13.50 | 10.39–17.33 | |
| CZ | 36 | 9.00 | 6.47–12.35 | |
| TO | 48 | 12.00 | 9.06–15.69 | |
| CK | 52 | 13.00 | 9.94–16.79 | |
| NE | 66 | 16.50 | 13.07–20.57 | |
| Species on the farm | ||||
| Cattle | 35 | 8.75 | 6.25–12.07 | |
| Cattle, goat | 187 | 46.75 | 41.79–51.77 | |
| Cattle, goat, sheep | 106 | 26.50 | 22.30–31.16 | |
| Goat | 48 | 12.00 | 9.06–15.69 | |
| Goat, sheep | 21 | 5.25 | 3.36–8.04 | |
| Sheep | 3 | 0.75 | 0.19–2.36 |
| Factors of Knowledge | Category | Frequency (n = 400) | Proportion (%) | 95% CI | KAP Score (%) |
|---|---|---|---|---|---|
| Did your livestock abort | |||||
| Yes | 370 | 92.50 | 89.35–94.80 | ||
| No | 30 | 7.50 | 5.19–10.64 | ||
| Which months | |||||
| Jan, Feb, Mar | 349 | 87.25 | 83.86–90.27 | ||
| Apr, May, Jun | 51 | 12.75 | 9.72–16.51 | ||
| What causes abortion | |||||
| Diseases | 313 | 78.25 * | 73.81–82.12 | 78.25 | |
| Poor feeding | 48 | 12.00 | 9.06–15.69 | ||
| Misfortune | 39 | 9.75 | 7.10–13.19 | ||
| Do you know RVF | |||||
| Yes | 41 | 10.25 * | 7.54–13.75 | 10.25 | |
| No | 359 | 89.75 | 86.25–92.46 | ||
| Do you know clinical signs of RVF? | |||||
| Yes | 35 | 8.75 * | 6.25–12.07 | 8.75 | |
| No | 365 | 91.25 | 87.93–93.75 | ||
| Do you know what causes RVF | |||||
| Yes | 33 | 8.25 * | 5.83–11.50 | 8.25 | |
| No | 367 | 91.75 | 88.49–94.17 | ||
| Do you know RVF host species | |||||
| Yes | 38 | 9.50 * | 6.89–12.91 | 9.50 | |
| No | 362 | 90.50 | 87.09–93.11 | ||
| Do you know how it is transmitted | |||||
| Yes | 38 | 9.50 * | 6.89–12.91 | 9.50 | |
| No | 362 | 90.50 | 87.09–93.11 | ||
| Can mosquito transmit RVF | |||||
| Yes | 38 | 9.50 * | 6.89–12.91 | 9.50 | |
| No | 362 | 90.50 | 87.09–93.11 | ||
| Do you know that it is zoonotic | |||||
| Yes | 38 | 9.50 * | 6.89–12.91 | 9.50 | |
| No | 362 | 90.50 | 87.09–93.11 | ||
| Average KAP score on RVF knowledge of participants (143.5/8) | 17.90% | ||||
| Factors under Management Practices | Category | Frequency (n = 400) | Proportion (%) | 95% CI | KAP Score (%) |
|---|---|---|---|---|---|
| Did you experience neonatal death | |||||
| Yes | 339 | 84.75 | 80.76–88.05 | ||
| No | 61 | 15.25 | 11.95–19.24 | ||
| Did you experience retain placenta | |||||
| Yes | 228 | 57.00 | 51.98–61.88 | ||
| No | 172 | 43.00 | 38.11–48.02 | ||
| Are young and old livestock raised together | |||||
| Yes | 233 | 58.25 * | 53.23–63.10 | 58.25 | |
| No | 167 | 41.75 | 36.89–46.76 | ||
| How did you handle aborted materials | |||||
| Protected hands | 221 | 55.25 * | 50.22–60.17 | 55.25 | |
| Unprotected hands | 179 | 44.75 | 39.83–49.77 | ||
| How did you dispose aborted materials | |||||
| Buried | 178 | 44.50 * | 39.58–49.52 | 44.50 | |
| Unburied | 222 | 55.50 | 50.47–60.42 | ||
| How did you handle neonatal death materials | |||||
| Protected hands | 293 | 73.25 * | 68.58–77.47 | 73.25 | |
| Unprotected hands | 107 | 26.75 | 22.53–31.42 | ||
| Can you suspect RVF in livestock | |||||
| Yes | 38 | 9.50 * | 6.89–12.91 | 9.50 | |
| No | 362 | 90.50 | 87.09–93.11 | ||
| Can you prevent RVF in livestock | |||||
| Yes | 38 | 9.50 * | 6.89–12.91 | 9.50 | |
| No | 362 | 90.50 | 87.09–93.11 | ||
| Mode of night shelter | |||||
| Communal | 177 | 44.25 | 39.34–49.27 | 54.00 | |
| Private | 216 | 54.00 * | 48.97–58.94 | ||
| None | 7 | 1.75 | 0.77–3.73 | ||
| Type of grazing grounds | |||||
| Communal | 224 | 56.00 | 50.97–60.90 | 44.00 | |
| Private | 176 | 44.00 * | 39.09–49.02 | ||
| Type of herd composition | |||||
| Mixed species | 293 | 73.25 | 68.57–77.46 | 26.75 | |
| Single species | 107 | 26.75 * | 22.53–31.42 | ||
| Average KAP score on RVF attitude of participants (375.1/9) | 41.23% | ||||
| Factors under Attitude | Category | Frequency (n = 400) | Proportion (%) | 95% CI | KAP Score (%) |
|---|---|---|---|---|---|
| How do you feel on heavy rainfall and flooding? | |||||
| Destroy crops | 337 | 84.25 | 80.22–87.60 | ||
| Promote spread of RVF | 63 | 15.75 * | 12.39–19.78 | 15.75 | |
| How do you feel on increased mosquito population, can it spread RVF? | |||||
| Yes | 34 | 8.50 * | 6.04–11.78 | 8.50 | |
| No | 366 | 91.50 | 88.21–93.95 | ||
| Do you think RVF cause abortion? | |||||
| Yes | 34 | 8.50 * | 6.04–11.78 | 8.50 | |
| No | 366 | 91.50 | 88.21–93.95 | ||
| Do you think RVF cause neonatal death? | |||||
| Yes | 34 | 8.50 * | 6.04–11.78 | 8.50 | |
| No | 366 | 91.50 | 88.21–93.95 | ||
| Do you think there is production losses on your farm due to RVF? | |||||
| Yes | 34 | 8.50 * | 6.04–11.78 | 8.50 | |
| No | 366 | 91.5 | 88.21–93.95 | ||
| Do you think vendors bring RVF infected livestock? | |||||
| Yes | 34 | 8.50 * | 6.04–11.78 | 8.50 | |
| No | 366 | 91.50 | 88.21–93.95 | ||
| Do you fear suffering RVF? | |||||
| Yes | 34 | 8.50 * | 6.04–11.78 | 8.50 | |
| No | 366 | 91.50 | 88.21–93.95 | ||
| Are you capable to prevent RVF in livestock? | |||||
| Yes | 34 | 8.50 * | 6.04–11.78 | 8.50 | |
| No | 366 | 91.50 | 88.21–93.95 | ||
| Average KAP score on RVF attitude of participants (75.2/8) | 9.40% | ||||
| Variable | Mean Knowledge Score | Mean Attitude Score | Mean Practice Score | |||
|---|---|---|---|---|---|---|
| Mean | Std. Deviation | Mean | Std. Deviation | Mean | Std. Deviation | |
| Gender | ||||||
| Male | 63.50 | 17.90 | 24.88 | 8.13 | 147.44 | 72.52 |
| Female | 8.25 | 4.82 | 12.75 | 2.12 | 45.22 | 36.86 |
| p-value | 0.019 | 0.048 | 0.003 | |||
| Age (years) | ||||||
| 18–25 | 3.50 | 4.24 | 1.38 | 1.06 | 23.89 | 15.35 |
| 26–35 | 6.25 | 5.57 | 8.38 | 2.20 | 33.44 | 17.72 |
| 36–45 | 21.87 | 15.04 | 14.63 | 5.60 | 66.44 | 39.94 |
| ≥46 | 37.62 | 13.81 | 13.25 | 3.15 | 58.11 | 37.33 |
| p-value | 0.071 | 0.092 | 0.051 | |||
| Education | ||||||
| None | 5.50 | 6.74 | 1.13 | 0.35 | 24.56 | 12.78 |
| Primary | 30.62 | 72.10 | 8.25 | 1.83 | 106.00 | 60.28 |
| Secondary | 32.62 | 18.78 | 25.25 | 8.46 | 59.11 | 24.04 |
| Tertiary | 3.00 | 0.00 | 2.88 | 0.35 | 3.00 | 0.00 |
| p-value | 0.991 | 0.048 | 0.063 | |||
| Marital Status | ||||||
| Married | 54.87 | 16.97 | 25.00 | 8.29 | 155.56 | 86.86 |
| Single | 7.88 | 4.15 | 5.38 | 1.40 | 13.44 | 3.35 |
| Divorced | 3.88 | 6.17 | 4.13 | 2.80 | 18.22 | 5.33 |
| Widowed | 5.13 | 0.64 | 3.13 | 2.03 | 5.44 | 0.882 |
| p-value | 0.031 | 0.044 | 0.026 | |||
| Herd size | ||||||
| <25 | 62.13 | 16.63 | 174.22 | 96.10 | 23.50 | 8.142 |
| ≥25 | 9.00 | 4.92 | 18.44 | 2.12 | 14.63 | 3.739 |
| p-value | 0.011 | 0.001 | 0.047 | |||
| District | ||||||
| CP | 3.88 | 10.96 | 0.00 | 0.00 | 16.89 | 10.99 |
| KA | 5.00 | 11.31 | 1.00 | 0.00 | 21.33 | 12.63 |
| SA | 4.50 | 12.72 | 0.00 | 0.00 | 28.44 | 19.61 |
| MH | 4.75 | 13.43 | 0.00 | 0.00 | 23.44 | 14.03 |
| CZ | 25.13 | 3.52 | 16.87 | 4.91 | 23.67 | 4.58 |
| TO | 16.13 | 11.51 | 16.12 | 4.91 | 26.11 | 8.16 |
| CK | 6.00 | 16.97 | 0.00 | 0.00 | 21.11 | 12.53 |
| NE | 6.48 | 18.03 | 0.00 | 0.00 | 31.67 | 20.35 |
| p-value | 0.721 | 0.994 | 0.898 | |||
| Overall | 17.90 | 12.78 | 9.40 | 2.55 | 41.23 | 22.11 |
| Range | 3.00–80.50 | 0.00–270.32 | 3.00–242.42 | |||
| Factors under Knowledge | Number of Participants (n = 400) | Knowledgeable (n = 33) | Proportion (%) | OR | 95% CI | p-Value |
|---|---|---|---|---|---|---|
| Months for occurrence of abortions (n = 400) *** | ||||||
| Jan, Feb, Mar | 349 | 26 | 7.45 | Ref | ||
| Apr, May, Jun | 51 | 7 | 13.73 | 3.531 | 1.40–8.90 | 0.008 |
| What causes abortion (n = 400) * | ||||||
| Diseases | 313 | 21 | 6.71 | Ref | ||
| Poor feeding | 48 | 9 | 18.75 | 1.159 | 0.32–4.07 | 0.818 |
| Misfortune | 39 | 3 | 7.69 | 3.209 | 1.37–7.50 | 0.007 |
| Do you know what causes RVF (n = 400) *** | ||||||
| No | 367 | 29 | 7.90 | Ref | ||
| Yes | 33 | 4 | 12.12 | 3.531 | 1.40–8.90 | 0.008 |
| Do you know RVF clinical signs (n = 400) | ||||||
| No | 365 | 27 | 7.40 | Ref | ||
| Yes | 35 | 6 | 17.14 | 2.590 | 1.98–6.78 | 0.053 |
| Do you know the affected species (n = 400) *** | ||||||
| No | 362 | 31 | 8.56 | Ref | ||
| Yes | 38 | 2 | 5.26 | 0.216 | 0.07–0.62 | 0.005 |
| Do you know how it is transmitted (n = 400) *** | ||||||
| No | 362 | 24 | 6.63 | Ref | ||
| Yes | 38 | 9 | 23.68 | 4.371 | 1.85–10.27 | 0.001 |
| Can mosquito transmit RVF (n = 400) *** | ||||||
| No | 362 | 23 | 6.35 | Ref | ||
| Yes | 38 | 10 | 26.32 | 5.264 | 2.28–12.15 | <0.001 |
| Do you know that it’s zoonoses (n = 400) *** | ||||||
| No | 362 | 23 | 6.35 | Ref | ||
| Yes | 38 | 10 | 26.32 | 5.264 | 2.28–12.15 | <0.001 |
| Can you suspect RVF cases in livestock (n = 400) *** | ||||||
| No | 362 | 23 | 6.35 | Ref | ||
| Yes | 38 | 10 | 26.32 | 5.264 | 2.28–12.15 | <0.001 |
| Factors under Practices | Number of Participants (n = 400) | Knowledgeable (n = 33) | Proportion (%) | OR | 95% CI | p-Value |
|---|---|---|---|---|---|---|
| Age (n = 400) * | ||||||
| ≥ 46 | 159 | 12 | 7.55 | Ref | ||
| 36–45 | 142 | 15 | 10.56 | 2.228 | 1.60–8.14 | 0.022 |
| 26–35 | 54 | 4 | 7.41 | 0.484 | 0.06–3.71 | 0.486 |
| 18–25 | 44 | 2 | 4.55 | 0.000 | 0.00–0.00 | 1.000 |
| Gender (n = 400) *** | ||||||
| Female | 269 | 18 | 6.69 | Ref | ||
| Male | 131 | 15 | 11.45 | 1.808 | 1.00–3.70 | 0.108 |
| Education (n = 400) * | ||||||
| None | 42 | 7 | 16.67 | Ref | ||
| Primary | 270 | 23 | 8.52 | 0.393 | 0.01–0.74 | 0.826 |
| Secondary | 85 | 3 | 3.53 | 0.100 | 0.00–0.42 | 0.038 |
| Tertiary | 3 | 0 | 0.00 | 5.370 | 0.0.00–0.00 | 0.177 |
| Did you experience neonatal death (n = 400) *** | ||||||
| No | 61 | 33 | 54.10 | Ref | ||
| Yes | 339 | 0 | 0.00 | 0.350 | 0.17–0.72 | 0.004 |
| Mode of night shelter (n = 400) * | ||||||
| Private | 177 | 7 | 3.95 | Ref | ||
| Communal | 216 | 26 | 12.04 | 3.323 | 1.41–7.85 | 0.006 |
| None | 7 | 0 | 0.00 | 0.000 | 0.00–0.00 | 0.999 |
| Type of grazing grounds (n = 400) *** | ||||||
| Communal | 224 | 7 | 3.13 | Ref | ||
| Stall feeding | 176 | 26 | 14.77 | 2.583 | 1.25–5.36 | 0.011 |
| Herd composition (n = 400) *** | ||||||
| Mixed species | 293 | 13 | 4.44 | Ref | ||
| Single species | 107 | 20 | 18.69 | 2.855 | 1.39–5.88 | 0.004 |
| Management of neonatal materials (n = 400) *** | ||||||
| Unprotected | 107 | 12 | 11.21 | Ref | ||
| Protected | 293 | 21 | 7.17 | 0.350 | 0.17–0.72 | 0.004 |
| Abortion management (n = 400) *** | ||||||
| Not buried | 222 | 29 | 13.06 | Ref | ||
| Buried | 178 | 4 | 2.25 | 0.190 | 0.08–0.44 | 0.001 |
| How did you handle aborted materials (n = 400) *** | ||||||
| Protected | 221 | 29 | 13.12 | Ref | ||
| Unprotected | 179 | 4 | 2.23 | 0.321 | 0.15–0.70 | 0.004 |
| Can you prevent spread of RVF? (n = 400) *** | ||||||
| Yes | 38 | 3 | 7.89 | Ref | ||
| No | 362 | 30 | 8.29 | 5.264 | 2.28–12.15 | 0.001 |
| Variable | Level | aOR | 95% CI | p-Value |
|---|---|---|---|---|
| What causes abortion (n = 400) | Diseases | Ref | ||
| Poor feeding | 1.879 | 0.47–7.52 | 0.372 | |
| Misfortune | 3.861 | 1.14–13.05 | 0.001 *** | |
| How RVF is transmitted (n = 400) | Yes | Ref | ||
| No | 5.652 | 1.76–18.12 | 0.004 *** | |
| Do you know the affected species (n = 400) | No | Ref | ||
| Yes | 0.140 | 0.03–0.62 | 0.009 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kainga, H.; Mponela, J.; Basikolo, L.; Phonera, M.C.; Mpundu, P.; Munyeme, M.; Simulundu, E.; Saasa, N. Assessment of Knowledge, Attitudes, and Practices towards Rift Valley Fever among Livestock Farmers in Selected Districts of Malawi. Trop. Med. Infect. Dis. 2022, 7, 167. https://doi.org/10.3390/tropicalmed7080167
Kainga H, Mponela J, Basikolo L, Phonera MC, Mpundu P, Munyeme M, Simulundu E, Saasa N. Assessment of Knowledge, Attitudes, and Practices towards Rift Valley Fever among Livestock Farmers in Selected Districts of Malawi. Tropical Medicine and Infectious Disease. 2022; 7(8):167. https://doi.org/10.3390/tropicalmed7080167
Chicago/Turabian StyleKainga, Henson, James Mponela, Linda Basikolo, Marvin Collen Phonera, Prudence Mpundu, Muso Munyeme, Edgar Simulundu, and Ngonda Saasa. 2022. "Assessment of Knowledge, Attitudes, and Practices towards Rift Valley Fever among Livestock Farmers in Selected Districts of Malawi" Tropical Medicine and Infectious Disease 7, no. 8: 167. https://doi.org/10.3390/tropicalmed7080167
APA StyleKainga, H., Mponela, J., Basikolo, L., Phonera, M. C., Mpundu, P., Munyeme, M., Simulundu, E., & Saasa, N. (2022). Assessment of Knowledge, Attitudes, and Practices towards Rift Valley Fever among Livestock Farmers in Selected Districts of Malawi. Tropical Medicine and Infectious Disease, 7(8), 167. https://doi.org/10.3390/tropicalmed7080167







