Barriers to Antiretroviral Medication Adherence in People Living with HIV (PLHIV) at the Time of the COVID-19 Pandemic in the Philippines
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample Size Computation
- -
- 95% confidence level;
- -
- Expected % of barriers (UNDP and UNAIDS, 2021):
- ○
- 59%—location of treatment hubs;
- ○
- 57%—checkpoints and crossing borders;
- ○
- 54%—stock of ARVS;
- -
- 20% of estimate relative precision.
2.3. Data Analysis
3. Results
3.1. Sociodemographic Characteristics
3.2. Identified HIV Treatment Barriers
3.3. HIV Treatment Barriers and Respondents by Region
“I guess lack of people or group of people that would check on you. to be honest, it’s really hard to find a support or friend that share the same situation just like mine. I know I could find them from maybe institution from a hub or even here on twitter, but, it’s really hard. I’ve been alone since I was diagnosed”(Participant 1)
“It’s kind of hard specially since I am living alone here in the metro and I am having trust issues with some of my friends about my status”(Participant 2)
3.4. HIV Treatment Barriers and Respondents by Age Group
“During the Enhanced Community Quarantine, public transportations were banned so the only way to get ARVs is through Grab Express, or Lalamove. I’m only a student without savings that time so payment for those services were kind of expensive for me”(Participant 3)
“The treatment hub is far from the place where I am staying. I’m only a student, that is why commuting is one of the hindrances why I cannot go regularly at the treatment hub to have for my check-up every 6 months”(Participant 4)
3.5. HIV Treatment Barriers and Respondents by Educational Status
“During Enhanced Community Quarantine, my hub is located in Pasay. It was hard to coordinate to the hub located in Cavite because it is not my primary hub. Also, my family doesn’t know that I have it thus it was hard to do the paper works and they ask what is the delivery is for. And since the Cavite Hub is not my primary hub, I sometimes get 2 bottles only”(Participant 5)
“All kinds of transportation have been shut off during the lockdown. The location of the treatment hub is quite far. During lockdown, I don’t get paid if I don’t go to work.”(Participant 6)
3.6. HIV Treatment Barriers and Respondents by Employment Status
“During lockdowns, you have to walk to the nearest hospital. You’ll encounter checkpoints that asked you questions if you’re the one allowed to travel to get certain items including medications. Since you’re too far from the hub, you have to get your medication to the nearest hospital hoping you’ll get one. The delivery is much trickier because you don’t have any idea what to do that’s why you have to search the net for information if it’s possible. Calling the hub was impossible back then I guess the phone to the department was busy too. Money was also a problem since my siblings stop working and its troubling time.”(Participant 7)
“I do live miles away from my treatment hub. I am employed and need to get excused to travel every refill time”(Participant 8)
“My work schedule is somehow a hindrance to go. This makes it hard for me to do testing for Viral Load and CD4 count”(Participant 9)
“All kinds of transportation have been shut off during the lockdown. The location of the treatment hub is quite far. During lockdown, I don’t get paid if I don’t go to work.”(Participant 10)
4. Discussion
4.1. Location of Treatment Hubs
4.2. Checkpoints and Crossing Borders
4.3. Financial Assistance
4.4. Psychosocial Support
4.5. Stock of ARV and Other Medicines
4.6. Study Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- ○
- Yes
- ○
- No
- <20 years old
- 21–25 years old
- 26–30 years old
- 31–35 years old
- 36–40 years old
- 41–45 years old
- 46–50 years old
- >51 years old
- National Capital Region
- Northern Luzon
- Southern Luzon
- Visayas
- Mindanao
- Male
- Female
- Homosexual
- Bisexual
- Heterosexual
- Post Graduate Studies
- College
- High school
- Elementary
- Employed
- Unemployed
- What issues did/do you encounter in accessing HIV treatment and care services, including antiretroviral therapy, in the time of COVID-19? Check all that apply.
- Transportation and delivery
- Location of treatment hubs
- Checkpoints and crossing borders
- Stock of ARVs and other medicines
- Financial assistance
- Employment
- Psychosocial support
- Verification (including ARV booklets)
- Temporary shelter and housing
- Please provide more details regarding the issues you identified in the previous question.
- You may also share other HIV-related concerns that you currently have.
Appendix B

Appendix C

Appendix D

References
- Landman, T.; Splendore, L.D.G. Pandemic democracy: Elections and COVID-19. J. Risk Res. 2020, 23, 1060–1066. [Google Scholar] [CrossRef]
- International Labour Organization. Asia-Pacific Employment and Social Outlook 2020: Navigating the Crisis towards a Human-Centered Future of Work; International Labour Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Bilon, X.J. Leaving No One Behind. Treatment and Care Concerns of People Living with HIV in the Time of COVID-19 (A Philippine Situationer); UNDP: Mandaluyong City, Philippines, 2021; pp. 1–8. [Google Scholar]
- World Health Organization. COVID-19. Available online: https://www.who.int/news-room/fact-sheets/detail/coronavirus-disease-(covid-19) (accessed on 16 September 2023).
- Epidemiology Bureau—Department of Health. Impact of the COVID-19 Pandemic to the Philippine HIV Epidemic Annual Report 2020; Epidemiology Bureau—Department of Health: Sta. Cruz, Manila, Philippines, 2020. [Google Scholar]
- Gangcuangco, L.M. HIV crisis in the Philippines: Urgent actions needed. Lancet Public Health 2019, 4, e84. [Google Scholar] [CrossRef] [PubMed]
- Arcaya, M.C.; Arcaya, A.L.; Subramanian, S.V. Inequalities in health: Definitions, concepts, and theories. Glob. Health Action 2015, 8, 27106. [Google Scholar] [CrossRef] [PubMed]
- Health Deaton, A. Inequality and Economic Development. J. Econ. Lit. 2003, XLI, 113–158. [Google Scholar] [CrossRef]
- Fauk, N.K.; Merry, M.S.; Putra, S.; Sigilipoe, M.A.; Crutzen, R.; Mwanri, L. Perceptions among transgender women of factors associated with the access to HIV/AIDS-related health services in Yogyakarta, Indonesia. PLoS ONE 2019, 14, e0221013. [Google Scholar]
- Whitehead, M. The concepts and principles of equity and health. Int. J. Health Serv. 1992, 22, 429–445. [Google Scholar] [CrossRef]
- Keleher, H.; Hagger, V. Health Literacy in Primary Health Care. Aust. J. Prim. Health 2007, 13, 24–30. [Google Scholar] [CrossRef]
- Levesque, J.F.; Harris, M.F.; Russell, G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Health 2013, 12, 18. [Google Scholar] [CrossRef]
- Choi, K.H.; Lui, H.; Guo, Y.; Han, L.; Mandel, J.S. Lack of HIV testing and awareness of HIV infection among men who have sex with men, Beijing, China. AIDS Educ. Prev. 2006, 18, 33–43. [Google Scholar] [CrossRef]
- Mohlabane, N.; Tutshana, B.; Peltzer, K.; Mwisongo, A. Barriers and facilitators associated with HIV testing uptake in South African health facilities offering HIV Counselling and Testing. Health SA Gesondheid 2016, 21, 86–95. [Google Scholar] [CrossRef]
- Nakanwagi, S.; Matovu, J.B.; Kintu, B.N.; Kaharuza, F.; Wanyenze, R.K. Facilitators and Barriers to Linkage to HIV Care among Female Sex Workers Receiving HIV Testing Services at a Community-Based Organization in Periurban Uganda: A Qualitative Study. J. Sex. Transm. Dis. 2016, 2016, 7673014. [Google Scholar] [CrossRef] [PubMed]
- Salkever, D.S. Accessibility and the demand for preventive care. Soc. Sci. Med. 1976, 10, 469–475. [Google Scholar] [CrossRef] [PubMed]
- Kretchy, I.A.; Asiedu-Danso, M.; Kretchy, J.P. Medication Management and Adherence during the COVID-19 Pandemic: Perspectives and Experiences from Low-and Middle-Income Countries; Elsevier: Amsterdam, The Netherlands, 2021; Volume 17, pp. 2023–2026. [Google Scholar]
- Collin, J.; Hadzmy, A.J.b.A. Coming out strategies on social media among young gay men in Malaysia. Youth 2022, 2, 39–52. [Google Scholar]
- Sundermann, E.E.; Erlandson, K.M.; Pope, C.N.; Rubtsova, A.; Montoya, J.; Moore, A.A.; Marzolini, C.; O’Brien, K.K.; Pahwa, S.; Payne, B.A.I.; et al. Current Challenges and Solutions in Research and Clinical Care of Older Persons Living with HIV: Findings Presented at the 9th International Workshop on HIV and Aging. AIDS Res. Hum. Retroviruses 2019, 35, 985–998. [Google Scholar] [CrossRef] [PubMed]
- Monjok, E.; Smesny, A.; Okokon, I.B.; Mgbere, O.; Essien, E.J. Adherence to antiretroviral therapy in Nigeria: An overview of research studies and implications for policy and practice. HIV/AIDS-Res. Palliat. Care 2010, 2, 69–76. [Google Scholar]
- Abaasa, A.M.; Todd, J.; Ekoru, K.; Kalyango, J.N.; Levin, J.; Odeke, E.; Karamagi, C.A.S. Good adherence to HAART and improved survival in a community HIV/AIDS treatment and care programme: The experience of The AIDS Support Organization (TASO), Kampala, Uganda. BMC Health Serv. Res. 2008, 8, 241. [Google Scholar] [CrossRef]
- World Health Organization. HIV/AIDS. Available online: https://www.who.int/news-room/fact-sheets/detail/hiv-aids (accessed on 30 November 2021).
- Center for Disease Control and Prevention. HIV and COVID 19. Available online: https://www.cdc.gov/hiv/basics/covid-19.html (accessed on 23 November 2021).
- Hargreaves, J.; Davey, C. Three Lessons for the COVID-19 Response from Pandemic HIV. Lancet HIV 2020, 7, e309–e311. [Google Scholar] [CrossRef]
- Jiang, H.; Zhou, Y.; Tang, W. Maintaining HIV Care during the COVID-19 Pandemic. Lancet HIV 2020, 7, e308–e309. [Google Scholar] [CrossRef]
- UNAIDS. Global HIV & AIDS Statistics—Fact Sheet. Available online: https://www.unaids.org/en/resources/fact-sheet (accessed on 23 November 2021).
- Karim, Q.A.; Karim, S.S.A. COVID-19 affects HIV and Tuberculosis care. Science 2020, 369, 366–368. [Google Scholar] [CrossRef]
- Dzinamarira, T.; Murewanhema, G.; Chitungo, I.; Ngara, B.; Nkambule, S.J.; Madziva, R.; Herrera, H.; Herrera, H.; Cuadros, D.F.; Cuadros, D.F.; et al. Risk of mortality in HIV-infected COVID-19 patients: A systematic review and meta-analysis. J. Infect. Public Health 2022, 15, 654–661. [Google Scholar] [CrossRef]
- Tesoriero, J.M.; Swain, C.A.E.; Pierce, J.L.; Zamboni, L.; Wu, M.; Holtgrave, D.R.; Gonzalez, C.J.; Udo, T.; Morne, J.E.; Hart-Malloy, R.; et al. COVID-19 outcomes among persons living with or without diagnosed HIV infection in New York State. JAMA Netw. Open 2014, 4, e2037069. [Google Scholar] [CrossRef] [PubMed]
- Fauk, N.K.; Gesesew, H.A.; Seran, A.L.; Ward, P.R. Barriers to access to antiretroviral therapy by people living with HIV in an Indonesian remote district during the COVID-19 pandemic: A qualitative study. BMC Infect. Dis. 2023, 23, 296. [Google Scholar] [CrossRef] [PubMed]
- Fauk, N.K.; Gesesew, H.A.; Seran, A.L.; Raymond, C.; Tahir, R.; Ward, P.R. Barriers to Accessing HIV Care Services in Host Low- and Middle-Income Countries: Views and Experiences of Indonesian Male Ex Migrant Workers Living with HIV. Int. J. Environ. Res. Public Health 2022, 19, 14377. [Google Scholar] [CrossRef]
- Fauk, N.K.; Mwanri, L.; Hawke, K.; Mohammadi, L.; Ward, P.R. Traditional Human Immunodeficiency Virus treatment and family and social influence as barriers to accessing HIV care services in Belu, Indonesia. PLoS ONE 2022, 17, e0264462. [Google Scholar] [CrossRef] [PubMed]
- Fauk, N.K.; Sukmawati, A.S.; Berek, P.A.L.; Ernawati; Kristanti, E.; Wardojo, S.S.I.; Cahaya, I.B.; Mwanri, L. Barriers to HIV testing among male clients of female sex workers in Indonesia. Int. J. Equity Health 2018, 17, 68. [Google Scholar] [CrossRef] [PubMed]
- Fauk, N.K.; Mwanri, L.; Hawke, K.; Mohammadi, L.; Ward, P.R. Psychological and Social Impact of HIV on Women Living with HIV and Their Families in Low- and Middle-Income Asian Countries: A Systematic Search and Critical Review. Int. J. Environ. Res. Public Health 2022, 19, 6668. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Weng, H.L.; Bai, H.; Liu, J.; Wei, X.N.; Zhou, K.; Sande, A. Quick Community Survey on the Impact of COVID-19 Outbreak for the Healthcare of People Living with HIV. Zhonghua Liu Xing Bing Xue Za Zhi 2020, 41, 662–666. [Google Scholar]
- Linnemayr, S.; Mayo-Wilson, L.J.; Saya, U.; Wagner, Z.; MacCarthy, S.; Walukaga, S.; Nakubulwa, S.; Karamagi, Y. HIV Care Experiences during the COVID-19 Pandemic: Mixed-Methods Telephone Interviews with Clinic-Enrolled HIV-Infected Adults in Uganda. AIDS Behav. 2020, 25, 28–39. [Google Scholar] [CrossRef]
- Ahmed, A.; Dujaili, J.A.; Jabeen, M.; Umair, M.M.; Chuah, L.-H.; Hashmi, F.K.; Awaisu, A.; Chaiyakunapruk, N. Barriers and Enablers for Adherence to Antiretroviral Therapy Among People Living with HIV/AIDS in the Era of COVID-19: A Qualitative Study from Pakistan. Front. Pharmacol. 2022, 12, 807446. [Google Scholar] [CrossRef]
- Sun, Y.; Zhan, Y.; Li, H.; Yuan, T.; Gao, Y.; Liang, B.; Feng, A.; Li, P.; Zheng, W.; Fitzpatrick, T.; et al. Stakeholder efforts to mitigate antiretroviral therapy interruption among people living with HIV during the COVID-19 pandemic in China: A qualitative study. J. Int. AIDS Soc. 2021, 24, e25781. [Google Scholar] [CrossRef]
- Fauk, N.K. Risk Factors and the Impact of HIV among Women Living with HIV and their Families in Yogyakarta and Belu District, Indonesia. Ph.D. Dissertation, Flinders University, Adelaide, Australia, 2022. [Google Scholar]
- Ballester-Arnal, R.; Gil-Llario, M.D. The Virus That Changed Spain: Impact of COVID-19 on People with HIV; Springer: Berlin/Heidelberg, Germany, 2020; Volume 24, pp. 2253–2257. [Google Scholar]
- Manchia, M.; Gathier, A.W.; Yapici-Eser, H.; Schimdt, M.V.; de Quervain, D.; van Amerlsvoort, T.; Bisson, J.I.; Cryan, J.F.; Howes, O.D.; Pinto, L.; et al. The Impact of COVID-19 Pandemic on Stress Resilience and Mental Health: A Critical Review Across Waves; Elsevier: Amsterdam, The Netherlands, 2022; Volume 55, pp. 22–83. [Google Scholar]
- Earnshaw, V.A.; Smith, L.R.; Chaudoir, S.R.; Amico, K.R.; Copenhaver, M.M. HIV Stigma Mechanisms and Well-Being among PLWH: A Test of the HIV Stigma Framework. AIDS Behav. 2013, 17, 1785–1795. [Google Scholar] [CrossRef] [PubMed]
- Ballivian, J.; Alcaide, M.L.; Cecchini, D.; Jones, D.L.; Abbamonte, J.M.; Cassetti, I. Impact of COVID–19-Related Stress and Lockdown on Mental Health among People Living with HIV in Argentina. J. Acquir. Immune Defic. Syndr. 2020, 85, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Shippy, R.A.; Karpiak, S.E. Perceptions of support among older adults with HIV. Res. Aging 2005, 27, 290–306. [Google Scholar] [CrossRef]
- Heckman, T.G.; Halkitis, P.N. Biopsychosocial aspects of HIV and aging. Behav. Med. 2014, 40, 81–84. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.C.; Fazeli, P.L.; Jeste, D.V.; Moore, D.J.; Grant, I.; Woods, S.P. Successful cognitive aging and health-related quality of life in younger and older adults infected with HIV. AIDS Behav. 2014, 18, 1186–1197. [Google Scholar] [CrossRef]
- Morgan, E.E.; Iudicello, J.E.; Weber, E.; Duarte, N.A.; Riggs, P.K.; Delano-Wood, L.; Ellis, R.; Grant, I.; Woods, S.P. Synergistic effects of HIV infection and older age on daily functioning. J. Acquir. Immune Defic. Syndr. 2012, 61, 341–348. [Google Scholar] [CrossRef]
- Valcour, V.; Paul, R.; Neuhaus, J.; Shikuma, C. The effects of age and HIV on neuropsychological performance. J. Int. Neuropsychol. Soc. 2011, 17, 190–195. [Google Scholar] [CrossRef]
- Armitage, R.; Nellums, L.B. COVID-19 and the Consequences of Isolating the Elderly. Lancet Public Health 2020, 5, e256. [Google Scholar] [CrossRef]
- Brooke, J.; Jackson, D. Older People and COVID-19: Isolation, Risk and Ageism. J. Clin. Nurs. 2020, 29, 2044–2046. [Google Scholar] [CrossRef]
- Halkitis, P.N.; Krause, K.D.; Vieira, D.L. Mental health, psychosocial challenges and resilience in older adults living with HIV. Interdiscip. Top. Gerontol. Geriatr. 2017, 42, 187–203. [Google Scholar]
- Hanghøj, S.; Boisen, K.A. Self-reported barriers to medication adherence among chronically ill adolescents: A systematic review. J. Adolesc. Health 2014, 54, 121–138. [Google Scholar] [CrossRef] [PubMed]
- Kretchy, I.A.; Owusu-Daaku, F.; Danquah, S.A. Mental health in hypertension: Assessing symptoms of anxiety, depression and stress on anti-hypertensive medication adherence. Int. J. Ment. Health Syst. 2014, 8, 25. [Google Scholar] [CrossRef] [PubMed]
- Salleh, M.R. life event, stress and illness. MJMS 2008, 15, 9–18. [Google Scholar] [PubMed]
- Hoke, T.; Bateganya, M.; Toyo, O.; Francis, C.; Shrestha, B.; Philakone, P.; Pandey, S.R.; Persaud, N.; Cassell, M.M.; Wilcher, R.; et al. How Home Delivery of antiretroviral drugs ensured uninterrupted HIV Treatment during COVID-19: Experiences from Indonesia, Laos, Nepal, and Nigeria. Glob. Health Sci. Pract. 2021, 9, 978. [Google Scholar] [CrossRef]

| Barriers | % | +/− Absolute Precision (20% of Estimate) | n |
|---|---|---|---|
| Transportation and delivery | 67% | 1.3 | 1419 |
| Location of treatment hubs | 59% | 11.8 | 67 |
| Checkpoints and crossing borders | 57% | 11.4 | 73 |
| Stock of ARVs | 54% | 10.8 | 82 |
| Financial assistance | 41% | 8.2 | 139 |
| Psychosocial support | 20% | 4.0 | 384 |
| Temporary shelter and housing | 4% | 0.8 | 2300 |
| Overseas Filipino Workers’ (OFWs’) concerns | 3% | 0.6 | 3096 |
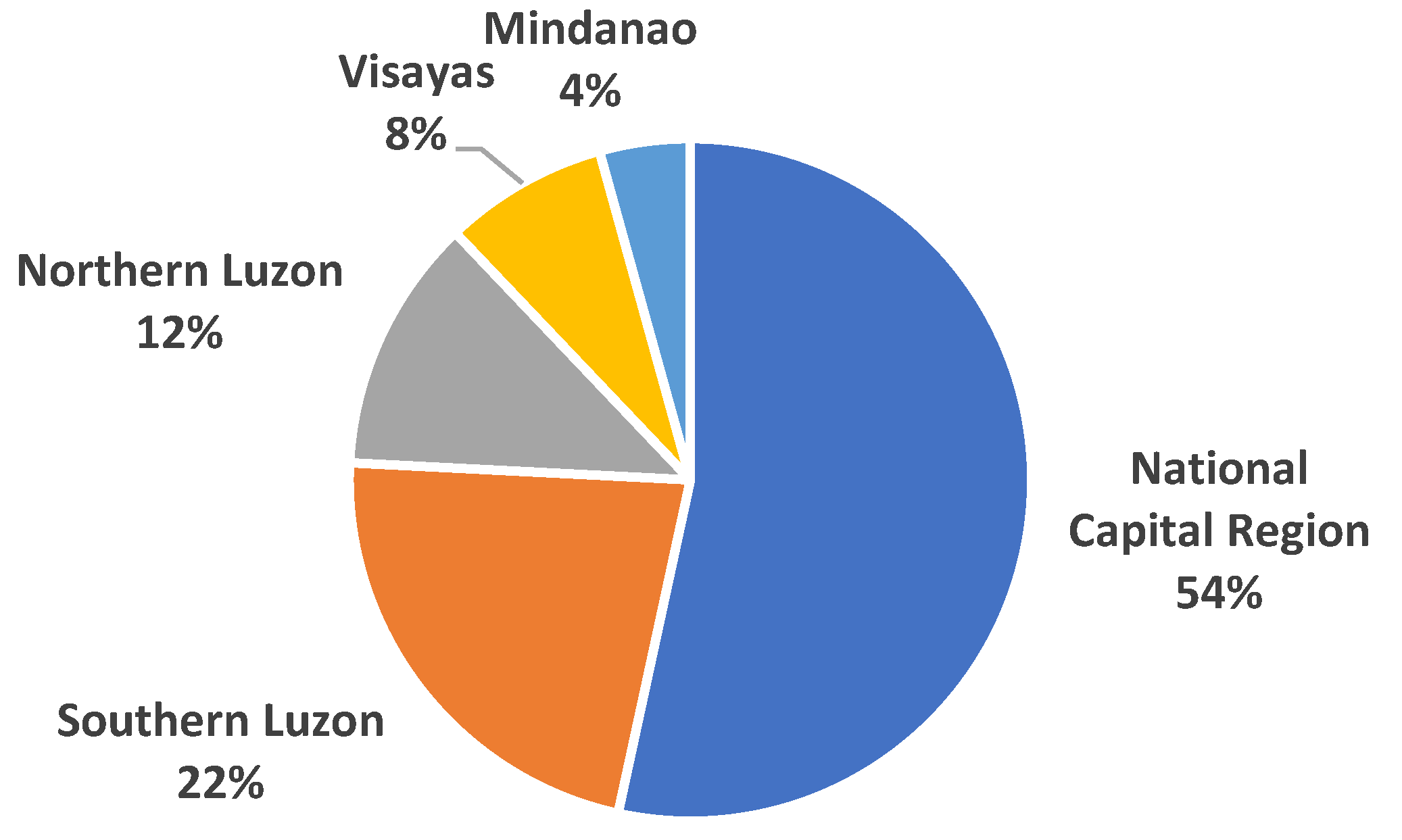
| Characteristic | No. | % |
|---|---|---|
| n | 116 | 100 |
| Region | ||
| National Capital Region (NCR) | 62 | 53.4 |
| Southern Luzon | 26 | 22.4 |
| Northern Luzon | 14 | 12.1 |
| Visayas | 9 | 7.8 |
| Mindanao | 5 | 4.3 |
| Age Group | ||
| 20 and below | 3 | 2.6 |
| 21–25 | 29 | 25.0 |
| 26–30 | 18 | 24.1 |
| 31–35 | 33 | 28.4 |
| 36–40 | 16 | 13.8 |
| 41–45 | 5 | 4.3 |
| 46–50 | 2 | 1.7 |
| Gender Identity | ||
| Male | 115 | 99.1 |
| Female | 1 | 0.9 |
| Sexual Orientation | ||
| Homosexual | 69 | 59.5 |
| Bisexual | 44 | 37.9 |
| Heterosexual | 3 | 2.6 |
| Educational Status | ||
| Elementary/High School | 15 | 12.9 |
| College/Graduate Studies | 101 | 87.1 |
| Employment Status | ||
| Employed | 82 | 70.7 |
| Unemployed | 34 | 29.3 |
| Issues | No. | % |
|---|---|---|
| n | 116 | 100 |
| Transportation and delivery | 72 | 62.1 |
| Location of treatment hubs | 61 | 52.6 |
| Financial assistance | 44 | 37.9 |
| Psychosocial support | 41 | 35.3 |
| Stock of ARVs and other medicines | 30 | 25.9 |
| Checkpoints and crossing borders | 28 | 24.1 |
| Verification (including ARV booklets) | 11 | 9.5 |
| Temporary shelter and housing | 7 | 6.0 |
| Number of Issues | ||
| 1 | 34 | 29.3 |
| 2 | 34 | 29.3 |
| 3 | 24 | 20.7 |
| 4 | 11 | 9.5 |
| 5 | 7 | 6.0 |
| 6 | 3 | 2.6 |
| 7 | 1 | 0.9 |
| 8 | 2 | 1.7 |
| Barrier | NCR (n = 62) | Northern Luzon | Southern Luzon | Visayas/Mindanao | p-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | ||
| n | 62 | 14 | 26 | 14 | |||||
| Checkpoints and crossing borders | 11 | 17.7 | 10 | 71.4 | 5 | 19.2 | 2 | 14.3 | <0.001 a |
| Financial assistance | 23 | 37.1 | 8 | 57.1 | 11 | 42.3 | 2 | 14.3 | 0.124 |
| Location of treatment hubs | 33 | 53.2 | 9 | 64.3 | 14 | 53.8 | 5 | 35.7 | 0.495 |
| Psychosocial support | 28 | 45.2 | 4 | 28.6 | 9 | 34.6 | 0 | 0 | 0.018 b |
| Stock of ARVs and other medicines | 18 | 29.0 | 2 | 14.3 | 5 | 19.2 | 5 | 35.7 | 0.456 |
| Temporary shelter and housing | 5 | 8.1 | 1 | 7.1 | 1 | 3.8 | 0 | 0 | 0.447 c |
| Transportation and delivery | 36 | 58.1 | 10 | 71.4 | 16 | 61.5 | 10 | 71.4 | 0.690 |
| Verification (including ARV booklets) | 6 | 9.7 | 2 | 14.3 | 2 | 7.7 | 1 | 7.1 | 0.939 d |
| Barrier | 18 to 25 | 26 to 30 | 31 to 35 | 36 to 50 | p-Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | ||
| n | 32 | 28 | 33 | 23 | |||||
| Checkpoints and crossing borders | 9 | 28.1 | 7 | 25.0 | 6 | 18.2 | 6 | 26.1 | 0.807 |
| Financial assistance | 17 | 53.1 | 5 | 17.9 | 12 | 36.4 | 10 | 43.5 | 0.041 |
| Location of treatment hubs | 17 | 53.1 | 16 | 57.1 | 16 | 48.5 | 12 | 52.2 | 0.927 |
| Psychosocial support | 14 | 43.8 | 15 | 53.6 | 5 | 15.2 | 7 | 30.4 | 0.011 |
| Stock of ARVs and other medicines | 7 | 21.9 | 8 | 28.6 | 6 | 18.2 | 9 | 39.1 | 0.321 |
| Transportation and delivery | 21 | 65.6 | 14 | 50.0 | 22 | 66.7 | 15 | 65.2 | 0.513 |
| 18 to 30 | 31 to 50 | ||||||||
| Temporary shelter and housing | 4 | 6.67 | 3 | 5.36 | 1.000 | ||||
| Verification (including ARV booklets) | 6 | 10.0 | 5 | 8.93 | 0.844 | ||||
| Barrier | Elementary/High School | College/Graduate Studies | p-Value | Test | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| n | 15 | 101 | ||||
| Checkpoints and crossing borders | 5 | 33.3 | 23 | 22.8 | 0.353 | Fisher’s |
| Financial assistance | 10 | 66.7 | 34 | 33.7 | 0.014 | Chi-square |
| Location of treatment hubs | 4 | 26.7 | 57 | 56.4 | 0.031 | Chi-square |
| Psychosocial support | 3 | 20.0 | 38 | 37.6 | 0.183 | Chi-square |
| Stock of ARVs and other medicines | 1 | 6.7 | 29 | 28.7 | 0.111 | Fisher’s |
| Temporary shelter and housing | 0 | 0 | 7 | 6.9 | 0.592 | Fisher’s |
| Transportation and delivery | 7 | 46.7 | 65 | 64.4 | 0.188 | Chi-square |
| Verification (including ARV booklets) | 1 | 6.7 | 10 | 9.9 | 1.000 | Fisher’s |
| Barrier | Employed | Unemployed | p-Value | Test | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| n | 82 | 34 | ||||
| Checkpoints and crossing borders | 14 | 17.1 | 14 | 41.2 | 0.006 | Chi-square |
| Financial assistance | 20 | 24.4 | 24 | 70.6 | <0.001 | Chi-square |
| Location of treatment hubs | 47 | 57.3 | 14 | 41.2 | 0.113 | Chi-square |
| Psychosocial support | 30 | 36.6 | 11 | 32.4 | 0.664 | Chi-square |
| Stock of ARVs and other medicines | 27 | 32.9 | 3 | 8.8 | 0.007 | Chi-square |
| Temporary shelter and housing | 3 | 3.7 | 4 | 11.8 | 0.192 | Fisher’s |
| Transportation and delivery | 52 | 63.4 | 20 | 58.8 | 0.643 | Chi-square |
| Verification (including ARV booklets) | 9 | 11 | 2 | 5.9 | 0.504 | Fisher’s |
| Residence of Client | Nearest HIV Facility | Distance | Travel Time by Walking |
|---|---|---|---|
| Zamboanga del Sur | Age—Healthily Wellness Hub | 405 km | 72 h |
| El Nido, Palawan | Ospital ng Palawan | 262 km | 48 h |
| Katico, Sultan Kudarat | Cotabato Regional and Medical Center | 111 km | 19 h |
| Moalboal, Cebu | Cebu City Health Center | 88 km | 17 h |
| San Joaquin, Iloilo | The Medical City Visayas | 53 km | 11 h |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Joves, P.J.M.; Matulac, M.O.; Pagcatipunan, R.S., Jr. Barriers to Antiretroviral Medication Adherence in People Living with HIV (PLHIV) at the Time of the COVID-19 Pandemic in the Philippines. Trop. Med. Infect. Dis. 2023, 8, 461. https://doi.org/10.3390/tropicalmed8100461
Joves PJM, Matulac MO, Pagcatipunan RS Jr. Barriers to Antiretroviral Medication Adherence in People Living with HIV (PLHIV) at the Time of the COVID-19 Pandemic in the Philippines. Tropical Medicine and Infectious Disease. 2023; 8(10):461. https://doi.org/10.3390/tropicalmed8100461
Chicago/Turabian StyleJoves, Philip John M., Melgar O. Matulac, and Rodolfo S. Pagcatipunan, Jr. 2023. "Barriers to Antiretroviral Medication Adherence in People Living with HIV (PLHIV) at the Time of the COVID-19 Pandemic in the Philippines" Tropical Medicine and Infectious Disease 8, no. 10: 461. https://doi.org/10.3390/tropicalmed8100461
APA StyleJoves, P. J. M., Matulac, M. O., & Pagcatipunan, R. S., Jr. (2023). Barriers to Antiretroviral Medication Adherence in People Living with HIV (PLHIV) at the Time of the COVID-19 Pandemic in the Philippines. Tropical Medicine and Infectious Disease, 8(10), 461. https://doi.org/10.3390/tropicalmed8100461






