Effect of Health Education on Schistosomiasis Control Knowledge, Attitude, and Practice after Schistosomiasis Blocking: Results of a Longitudinal Observational Study in the Field
Abstract
:1. Introduction
2. Methods
2.1. Study Site
2.2. Study Population
2.3. Baseline Survey
2.4. Health Education
2.5. Evaluation Survey and Follow-Up Survey
2.6. Statistical Analysis
2.7. Ethical Approval and Patients’ Informed Consent
3. Results
3.1. Questionnaire Collection and Basic Information of Survey Objects
3.2. Changes in Schistosomiasis Prevention KAP among Adults
3.2.1. Changes in the Qualified Rate of Schistosomiasis Prevention KAP among Adults
3.2.2. Changes in the Qualified Rate of Schistosomiasis Prevention KAP among Adults with Different Demographic Characteristics
3.2.3. Changes in the Accuracy Rate of Schistosomiasis Prevention KAP
3.2.4. Changes in the Accuracy Rate of Schistosomiasis Prevention KAP among Adults with Different Demographic Characteristics
3.2.5. Changes in the Accuracy Rate for Different Questions among Adults
3.3. Changes in the Schistosomiasis Prevention KAP among Students
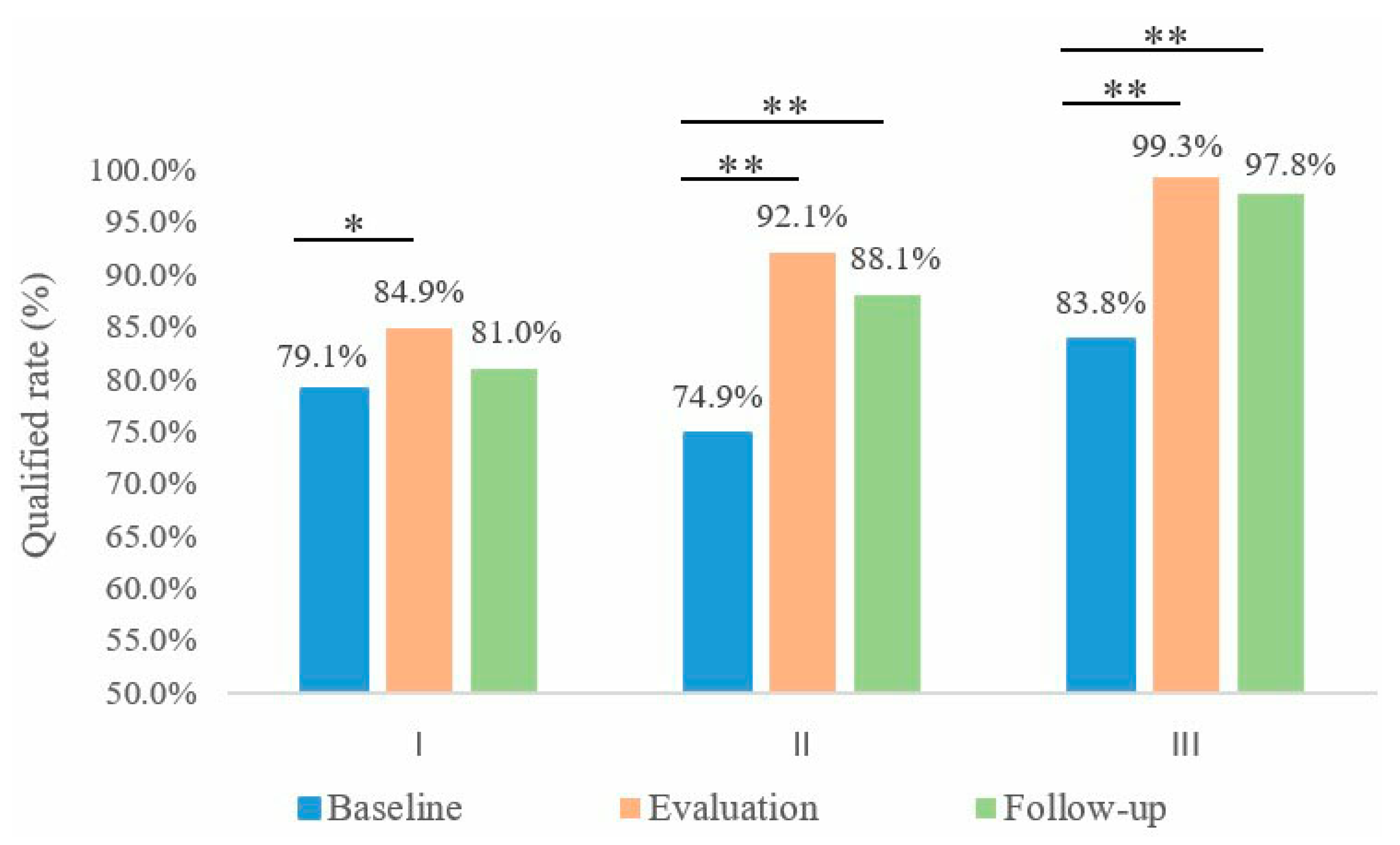
3.3.1. Changes in the Qualified Rate of Schistosomiasis Prevention KAP among Students
3.3.2. Changes in the Accuracy Rate of Schistosomiasis Prevention KAP among Students
3.3.3. Changes of Accuracy Rate of Different Questions among Students
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Loverde, P.T. Schistosomiasis. Adv. Exp. Med. Biol. 2019, 1154, 45–70. [Google Scholar] [PubMed]
- Conteh, L.; Engels, T.; Molyneux, D.H. Socioeconomic aspects of neglected tropical diseases. Lancet 2010, 375, 239–247. [Google Scholar] [CrossRef]
- Wei, O. Internal organs of a 2100-year-old female corpse. Lancet 1973, 2, 1198. [Google Scholar] [CrossRef]
- Song, L.G.; Wu, X.Y.; Sacko, M.; Wu, Z.D. History of schistosomiasis epidemiology, current status, and challenges in China: On the road to schistosomiasis elimination. Parasitol. Res. 2016, 115, 4071–4081. [Google Scholar] [CrossRef] [PubMed]
- Chuah, C.; Gobert, G.N.; Latif, B.; Heo, C.C.; Leow, C.Y. Schistosomiasis in Malaysia: A review. Acta Trop. 2019, 190, 137–143. [Google Scholar] [CrossRef]
- Gordon, C.A.; Kurscheid, J.; Williams, G.M.; Clements, A.C.A.; Li, Y.; Zhou, X.N.; Utzinger, J.; McManus, D.P.; Gray, D.J. Asian Schistosomiasis: Current Status and Prospects for Control Leading to Elimination. Trop. Med. Infect. Dis. 2019, 4, 40. [Google Scholar] [CrossRef]
- Li, S.Z.; Zheng, H.; Abe, E.M.; Yang, K.; Bergquist, R.; Qian, Y.J.; Zhang, L.J.; Xu, Z.M.; Xu, J.; Guo, J.G.; et al. Reduction patterns of acute schistosomiasis in the People’s Republic of China. PLoS Negl. Trop. Dis. 2014, 8, e2849. [Google Scholar] [CrossRef]
- Soares, M.R.; Salamat, M.S.; Leonardo, L.; Gray, D.J.; Carabin, H.; Halton, K.; McManus, D.P.; Williams, G.M.; Rivera, P.; Saniel, O.; et al. Geographical distribution of human Schistosoma japonicum infection in The Philippines: Tools to support disease control and further elimination. Int. J. Parasitol. 2014, 44, 977–984. [Google Scholar] [CrossRef]
- Satrija, F.; Ridwan, Y.; Jastal; Samarang; Rauf, A. Current status of schistosomiasis in Indonesia. Acta Trop. 2015, 141 Pt B, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Khieu, V.; Sayasone, S.; Muth, S.; Kirinoki, M.; Laymanivong, S.; Ohmae, H.; Huy, R.; Chanthapaseuth, T.; Yajima, A.; Phetsouvanh, R.; et al. Elimination of Schistosomiasis Mekongi from Endemic Areas in Cambodia and the Lao People’s Democratic Republic: Current Status and Plans. Trop. Med. Infect. Dis. 2019, 4, 30. [Google Scholar] [CrossRef]
- Gong, Y.F.; Feng, J.X.; Luo, Z.W.; Xue, J.B.; Guo, Z.Y.; Zhang, L.J.; Xia, S.; Lv, S.; Xu, J.; Li, S.Z. Spatiotemporal heterogeneity of schistosomiasis in mainland China: Evidence from a multi-stage continuous downscaling sentinel monitoring. Asian Pac. J. Trop. Med. 2022, 13, 258–265. [Google Scholar]
- Feng, J.X.; Gong, Y.F.; Luo, Z.W.; Wang, W.; Cao, C.L.; Xu, J.; Li, S.Z. Scientific basis of strategies for schistosomiasis control and prospect of the 14th Five-Year Plan in China. Chin. J. Parasit. Dis. 2022, 4, 428–435. [Google Scholar]
- Wang, L.D.; Chen, H.G.; Guo, J.G.; Zeng, X.J.; Hong, X.L.; Xiong, J.J.; Wu, X.H.; Wang, X.H.; Wang, L.Y.; Xia, G.; et al. A strategy to control transmission of Schistosoma japonicum in China. N. Engl. J. Med. 2009, 360, 121–128. [Google Scholar] [CrossRef]
- Zhang, L.J.; Xu, Z.M.; Qian, Y.J.; Dang, H.; Lv, S.; Xu, J.; Li, S.Z.; Zhou, X.N. Endemic status of schistosomiasis in People’s Republic of China in 2015. Chin. J. Schistoso. Control 2016, 28, 611–617. [Google Scholar]
- Zhang, L.J.; Xu, Z.M.; Yang, F.; Dang, H.; Li, Y.L.; Lv, S.; Cao, C.L.; Xu, J.; Li, S.Z.; Zhou, X.N. Endemic status of schistosomiasis in People’s Republic of China in 2020. Chin. J. Schistoso. Control 2021, 33, 225–233. [Google Scholar]
- Zhang, L.J.; Xu, Z.M.; Yang, F.; He, J.Y.; Dang, H.; Li, Y.L.; Cao, C.L.; Xu, J.; Li, S.Z.; Zhou, X.N. Progress of schistosomiasis control in People’s Republic of China in 2021. Chin. J. Schistoso. Control 2022, 34, 329–336. [Google Scholar]
- Feng, J.X.; Gong, Y.F.; Luo, Z.W.; Wang, X.Y.; Cao, C.L.; Zhang, X.; Zhang, J.F.; Li, H.R.; Hu, H.H.; Xu, J.; et al. Survey on the knowledge, attitude and practice towards schistosomiasis among adults in Jiangling County. Mod. Prev. Med. 2022, 49, 3426–3431. [Google Scholar]
- Lv, S.; Lv, C.; Li, Y.L.; Xu, J.; Hong, Q.B.; Zhou, J.; Zhang, J.F.; Wen, L.Y.; Zhang, J.F.; Zhang, S.Q.; et al. Expert consensus on the strategy and measures to interrupt the transmission of schistosomiasis in China. Chin. J. Schisto. Control 2021, 33, 10–14. [Google Scholar]
- Xu, J.; Hu, W.; Yang, K.; Lv, S.; Li, S.Z.; Zhou, X.N. Key points and research priorities of schistosomiasis control in China during the 14th Five-Year Plan Period. Chin. J. Schisto. Control 2021, 33, 1–6. [Google Scholar]
- Li, S.Z.; Xu, J.; Wang, T.P.; Wen, L.Y.; Yang, K.; Wang, W.; Lv, S.; Cao, C.L.; Zhou, X.N. Upholding Chinese spirit on schistosomiasis control in the new era to accelerate the progress towards schistosomiasis elimination in China. Chin. J. Schisto. Control 2019, 31, 1–13. [Google Scholar]
- Guo, Z.Y.; Feng, J.X.; Zhang, L.J.; Zhou, Y.B.; Zhou, J.; Yang, K.; Liu, Y.; Lin, D.D.; Liu, J.B.; Dong, Y.; et al. Analysis of the new WHO guideline to accelerate the progress towards elimination of schistosomiasis in China. Chin. J. Schisto. Control 2022, 34, 217–222. [Google Scholar]
- Xia, S.; Xue, J.B.; Zhang, X.; Hu, H.H.; Abe, E.M.; Rollinson, D.; Bergquist, R.; Zhou, Y.; Li, S.Z.; Zhou, X.N. Pattern analysis of schistosomiasis prevalence by exploring predictive modeling in Jiangling County, Hubei Province, P.R. China. Infect. Dis. Poverty 2017, 6, 91. [Google Scholar] [CrossRef] [PubMed]
- Gong, Y.F.; Li, Y.L.; Zhang, L.J.; Lv, S.; Xu, J.; Li, S.Z. The Potential Distribution Prediction of Oncomelania hupensis Based on Newly Emerging and Reemergent Habitats—China 2015–2019. China CDC Wkly. 2021, 3, 90–93. [Google Scholar] [CrossRef] [PubMed]
- Shi, Q.W.; Duan, L.P.; Qin, Z.Q.; Wang, W.; Shen, L.; Hua, X.; Shen, L.; Cao, J.; Zhu, F.; Wu, J.; et al. The Biosafety Evaluation for Crustaceans: A Novel Molluscicide PBQ Using against Oncomelania hupensis, the Intermediate Host of Schistosoma japonica. Trop. Med. Infect. Dis. 2022, 7, 294. [Google Scholar] [CrossRef]
- Xue, J.B.; Wang, X.Y.; Zhang, L.J.; Hao, Y.W.; Chen, Z.; Lin, D.D.; Xu, J.; Xia, S.; Li, S.Z. Potential impact of flooding on schistosomiasis in Poyang Lake regions based on multi-source remote sensing images. Parasit. Vectors 2021, 14, 116. [Google Scholar] [CrossRef]
- Xue, J.B.; Xia, S.; Zhang, L.J.; Abe, E.M.; Zhou, J.; Li, Y.Y.; Hao, Y.W.; Wang, Q.; Xu, J.; Li, S.Z.; et al. High-resolution remote sensing-based spatial modeling for the prediction of potential risk areas of schistosomiasis in the Dongting Lake area, China. Acta Trop. 2019, 198, 105077. [Google Scholar] [CrossRef]
- Takeuchi, R.; Njenga, S.M.; Ichinose, Y.; Kaneko, S.; Estrada, C.A.; Kobayashi, J. Is there a gap between health education content and practice toward schistosomiasis prevention among schoolchildren along the shores of Lake Victoria in Kenya? PLoS Negl Trop. Dis. 2019, 13, e7572. [Google Scholar] [CrossRef]
- Liu, L.; Yang, G.J.; Zhu, H.R.; Yang, K.; Ai, L. Knowledge of, attitudes towards, and practice relating to schistosomiasis in two subtypes of a mountainous region of the People’s Republic of China. Infect. Dis. Poverty 2014, 3, 16. [Google Scholar] [CrossRef]
- Hu, G.H.; Hu, J.; Song, K.Y.; Lin, D.D.; Zhang, J.; Cao, C.L.; Xu, J.; Li, D.; Jiang, W.S. The role of health education and health promotion in the control of schistosomiasis: Experiences from a 12-year intervention study in the Poyang Lake area. Acta Trop. 2005, 96, 232–241. [Google Scholar] [CrossRef]
- Zhou, X.N.; Bergquist, R.; Leonardo, L.; Yang, G.J.; Yang, K.; Sudomo, M.; Olveda, R. Schistosomiasis japonica control and research needs. Adv. Parasitol. 2010, 72, 145–178. [Google Scholar]
- Zhou, L.Y.; Deng, Y.; Steinmmann, P.; Yang, K. The effects of health education on schistosomiasis japonica prevalence and relevant knowledge in the People’s Republic of China: A systematic review and meta-analysis. Parasitol. Int. 2013, 62, 150–156. [Google Scholar] [CrossRef] [PubMed]
- The control of schistosomiasis. Report of a WHO Expert Committee. World Health Organ Tech. Rep. Ser. 1985, 728, 1–113. [Google Scholar]
- Hu, J.; Zhang, Z.S.; Hu, G.H.; Song, K.Y.; Chen, H.Y.; Hu, W.C.; Ge, J.; Peng, G.H.; Hu, Z.H.; Zhang, J.; et al. Effect of health promotion intervention on adult female residents in Schistosomiasis epidemic area of Poyang Lake for 17 years. Chin. J. Zoonoses 2010, 26, 982–985. [Google Scholar]
- Mott, K.E.; Lu, Y.; Chen, M.G. Control of schistosomiasis patients is human responsibility. Chin. J. Schisto. Control 1993, 65–74. [Google Scholar]
- Wei, Y.P. Analysis of the current situation and influencing factors of nurses’ knowledge and practice of edema in critically ill children. Chin. Gen. Pract. Nurs. 2022, 20, 3445–3447. [Google Scholar]
- Hu, G.H.; Xu, J.; Cao, C.L.; Jin, J.Y.; Lv, S.; Li, S.Z.; Zhou, X.N. Challenges and strategies of health education and health promotion in stage of schistosomiasis elimination. Chin. J. Schisto. Control 2018, 30, 117–120. [Google Scholar]
- Hata, N.; Yasukawa, A.; Sei, E.; Kawasumi, K.; Miya, N.; Yamaguchi, H.; Minai, M.; Shimogawara, R.; Ohta, N. Comparative analysis of knowledge on schistosomiasis japonica in the local people in the former endemic area in Yamanashi Prefecture, Japan: Comparisons among the background of age and occupation. J. Vet. Med. Sci. 2017, 79, 608–617. [Google Scholar] [CrossRef]

| Questionnaires | Adults | Students | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | Evaluation | Follow-Up | Baseline | Evaluation | Follow-Up | ||||
| Control Group | Intervention Group | Control Group | Intervention Group | Control Group | Intervention Group | ||||
| Distribution | 748 | 387 | 725 | 359 | 620 | 297 | 302 | 299 | 311 |
| Recovery | 738 | 382 | 717 | 353 | 609 | 295 | 302 | 298 | 311 |
| Characteristic | Baseline | Evaluation | Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control Group | Intervention Group | χ2 Value | p-Value | Control Group | Intervention Group | χ2 Value | p-Value | Control Group | Intervention Group | χ2 Value | p-Value | |
| Gender | 0.791 | 0.374 | 0.780 | 0.377 | 0.020 | 0.889 | ||||||
| Male | 52.4% (387/738) | 55.2% (211/382) | 47.8% (343/717) | 50.7% (179/353) | 53.0% (323/609) | 52.5% (155/295) | ||||||
| Female | 47.6% (351/738) | 44.76% (171/382) | 52.2% (374/717) | 49.3% (174/353) | 47.0% (286/609) | 47.5% (140/295) | ||||||
| Age, years | 5.544 | 0.063 | 2.721 | 0.257 | 0.545 | 0.762 | ||||||
| 18–44 | 11.4% (84/738) | 14.7% (56/382) | 10.5% (75/717) | 13.3% (47/353) | 11.7% (71/609) | 12.9% (38/295) | ||||||
| 45–59 | 43.1% (318/738) | 46.6% (178/382) | 39.3% (282/717) | 40.8% (144/353) | 40.6% (247/609) | 41.7% (123/295) | ||||||
| ≥60 | 45.5% (336/738) | 38.7% (148/382) | 50.2% (360/717) | 45.9% (162/353) | 47.8% (291/609) | 45.4% (134/295) | ||||||
| Education | 5.329 | 0.07 | 4.739 | 0.094 | 5.591 | 0.061 | ||||||
| Primary school and below | 57.2% (422/738) | 52.9% (202/382) | 67.4% (483/717) | 75.6% (257/353) | 54.0% (329/609) | 60.7% (179/295) | ||||||
| Junior middle school | 35.9% (265/738) | 36.4% (139/382) | 30.5% (219/717) | 21.5% (86/353) | 39.9% (243/609) | 31.9% (94/295) | ||||||
| Senior high school or above | 6.9% (51/738) | 10.7% (41/382) | 2.1% (15/717) | 2.8% (10/353) | 6.1% (37/609) | 7.5% (22/295) | ||||||
| Characteristic | Control Group | Intervention Group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Qualified Rate at Baseline (%) | Qualified Rate at Evaluation (%) | Difference in Qualified Rate (%) | Test | Qualified Rate at Follow-Up (%) | Difference in Qualified Rate (%) | Test | Qualified Rate at Baseline (%) | Qualified Rate at Evaluation (%) | Difference in Qualified Rate (%) | Test | Qualified Rate at Follow-Up (%) | Difference in Qualified Rate (%) | Test | |
| Gender | ||||||||||||||
| Male | 81.7 (316/387) | 85.7 (294/343) | 4.1 | χ2 = 2.183, p = 0.140 | 82.0 (265/323) | 0.4 | χ2 = 0.018, p = 0.893 | 76.8 (162/211) | 93.3 (167/179) | 16.5 | χ2 = 20.028, p < 0.001 | 90.3 (140/155) | 13.5 | χ2 = 11.363, p = 0.001 |
| Female | 76.4 (268/351) | 84.0 (315/374) | 7.6 | χ2 = 7.123, p = 0.008 | 79.7 (228/286) | 3.4 | χ2 = 1.307, p = 0.309 | 72.5 (124/171) | 90.8 (158/174) | 18.3 | χ2 = 19.329, p < 0.001 | 85.7 (120/140) | 13.2 | χ2 = 7.935, p = 0.005 |
| Age, years | ||||||||||||||
| 18–44 | 75.0 (63/84) | 90.7 (68/75) | 15.7 | χ2 = 6.703, p = 0.010 | 84.5 (60/71) | 9.5 | χ2 = 2.123, p = 0.145 | 91.1 (51/56) | 97.9 (46/47) | 6.8 | p = 0.216 | 100 (38/38) | 8.9 | p = 0.079 |
| 45–59 | 82.7 (263/318) | 89.4 (252/282) | 6.7 | χ2 = 5.448, p = 0.020 | 87.0 (215/247) | 4.3 | χ2 = 6.020, p = 0.014 | 77.5 (138/178) | 94.4 (136/144) | 16.9 | χ2 = 17.958, p < 0.001 | 95.9 (118/123) | 18.4 | χ2 = 19.382, p < 0.001 |
| ≥60 | 76.8 (258/336) | 80.3 (289/360) | 3.5 | χ2 = 1.260, p = 0.262 | 74.9 (218/291) | 1.9 | χ2 = 0.299, p = 0.585 | 65.5 (97/148) | 88.3 (143/162) | 22.7 | χ2 = 22.860, p < 0.001 | 77.6 (104/134) | 12.1 | χ2 = 5.006, p = 0.025 |
| Education | ||||||||||||||
| Primary school and below | 73.9 (312/422) | 82.0 (396/483) | 8.1 | χ2 = 8.579, p = 0.003 | 80.6 (265/329) | 6.6 | χ2 = 4.542, p = 0.033 | 69.3 (140/202) | 90.7 (233/257) | 21.4 | χ2 = 33.874, p < 0.001 | 81.6 (146/179) | 12.3 | χ2 = 7.618, p = 0.006 |
| Junior middle school | 84.9 (225/265) | 91.3 (200/219) | 6.4 | χ2 = 4.615, p = 0.032 | 80.3 (195/243) | 4.7 | χ2 = 1.921, p = 0.166 | 77.7 (108/139) | 95.4 (82/86) | 17.7 | χ2 = 12.601, p < 0.001 | 98.9 (93/94) | 21.2 | χ2 = 21.350, p < 0.001 |
| Senior high school or above | 92.2 (47/51) | 86.7 (13/15) | 5.5 | p = 0.612 | 89.2 (33/37) | 3.0 | p = 0.716 | 92.7 (38/41) | 100 (10/10) | 7.3 | p = 1.000 | 95.5 (21/22) | 2.8 | p = 1.000 |
| Characteristics | Difference in Qualified Rate at Evaluation (%) | Test of Difference at Evaluation | Difference in Qualified Rate at Follow-Up (%) | Test of Difference at Follow-Up |
|---|---|---|---|---|
| Gender | ||||
| Male | 7.6 | χ2 = 6.551, p = 0.010 | 8.3 | χ2 = 5.548, p = 0.018 |
| Female | 6.8 | χ2 = 4.352, p = 0.037 | 6.0 | χ2 = 2.258, p = 0.133 |
| Age, years | ||||
| 18–44 | 7.2 | p = 0.151 | 15.5 | p = 0.008 |
| 45–59 | 5.1 | χ2 = 3.031, p = 0.082 | 8.9 | χ2 = 7.211, p = 0.007 |
| ≥60 | 8.0 | χ2 = 5.003, p = 0.025 | 2.7 | χ2 = 0.364, p = 0.546 |
| Education | ||||
| Primary school and below | 8.7 | χ2 = 9.898, p = 0.002 | 1.0 | χ2 = 0.078, p = 0.781 |
| Junior middle school | 4.0 | χ2 = 1.435, p = 0.231 | 18.7 | χ2 = 19.053, p < 0.001 |
| Senior high school or above | 13.3 | p = 0.500 | 6.3 | p = 0.641 |
| Type | Control Group | Intervention Group | Difference in Accuracy Rate at Evaluation (%) | Test of Difference at Evaluation | Difference in accuracy rate at Follow-Up (%) | Test of difference in Follow-Up | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Accuracy Rate at Baseline (%) | Accuracy Rate at Evaluation (%) | Difference in Accuracy Rate (%) | Test | Accuracy Rate at Follow-Up (%) | Difference in Accuracy Rate (%) | Test | Accuracy Rate at Baseline (%) | Accuracy Rate at Evaluation (%) | Difference in Accuracy Rate (%) | Test | Accuracy Rate at Follow-Up (%) | Difference in Accuracy Rate (%) | Test | |||||
| Knowledge | 78.3 (4622/5904) | 84.6 (4855/5736) | 6.4 | χ2 = 77.662, p < 0.001 | 89.8 (4375/4872) | 11.5 | χ2 = 256.691, p < 0.001 | 79.0 (2414/3056) | 88.5 (2500/2824) | 9.5 | χ2 = 97.186, p < 0.001 | 93.7 (2212/2360) | 14.7 | χ2 = 232.119, p < 0.001 | 3.9 | χ2 = 23.626, p < 0.001 | 3.9 | χ2 = 30.228, p < 0.001 |
| Attitude | 83.0 (3674/4428) | 86.8 (3734/4302) | 3.8 | χ2 = 24.842, p < 0.001 | 87.8 (3207/3654) | 4.8 | χ2 = 36.379, p < 0.001 | 76.6 (1755/2292) | 91.6 (1940/2118) | 15.0 | χ2 = 182.935, p < 0.001 | 91.9 (1626/1770) | 15.3 | χ2 = 167.403, p < 0.001 | 4.8 | χ2 = 31.828, p < 0.001 | 4.1 | χ2 = 20.621, p < 0.001 |
| Practice | 56.6 (2505/4428) | 60.7 (2609/4302) | 4.1 | χ2 = 14.929, p < 0.001 | 60.0 (2194/3654) | 3.5 | χ2 = 9.916, p = 0.002 | 53.2 (1219/2292) | 80.6 (1706/2118) | 27.4 | χ2 = 369.015, p < 0.001 | 70.5 (1247/1770) | 17.3 | χ2 = 124.835, p < 0.001 | 19.9 | χ2 = 255.076, p < 0.001 | 10.4 | χ2 = 55.693, p < 0.001 |
| Characteristic | Accuracy Rate at Baseline (%) | Accuracy Rate at Evaluation (%) | Accuracy Rate at Follow-Up (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Knowledge | Attitude | Practice | Knowledge | Attitude | Practice | Knowledge | Attitude | Practice | |
| Gender | |||||||||
| Male | 78.8 (2441/3096) | 83.8 (1945/2322) | 56.4 (1310/2322) | 85.1 (2336/2744) | 87.2 (1794/2058) | 61.7 (1270/2058) | 90.5 (2339/2584) | 87.8 (1702/1938) | 61.0 (1182/1938) |
| Female | 77.7 (2181/2808) | 82.1 (1729/2106) | 56.7 (1195/2106) | 84.2 (2519/2992) | 86.5 (1940/2244) | 59.7 (1339/2244) | 89.0 (2036/2288) | 87.7 (1505/1716) | 59.0 (1012/1716) |
| Age | |||||||||
| 18~44 | 72.8 (489/672) | 84.7 (427/504) | 56.0 (282/504) | 86.8 (521/600) | 88.7 (399/450) | 64.0 (288/450) | 94.4 (536/568) | 87.1 (371/426) | 56.1 (239/426) |
| 45~59 | 79.9 (2032/2544) | 83.7 (1596/1908) | 56.9 (1085/1908) | 87.0 (1963/2256) | 87.9 (1488/1692) | 62.1 (1050/1692) | 89.8 (1774/1976) | 88.1 (1305/1482) | 61.5 (911/1482) |
| ≥60 | 78.2 (2101/2688) | 81.9 (1651/2016) | 56.5 (1138/2016) | 82.3 (2371/2880) | 85.5 (1847/2160) | 58.8 (1271/2160) | 88.7 (2065/2328) | 87.7 (1531/1746) | 59.8 (1044/1746) |
| Education | |||||||||
| Primary school and below | 77.1 (2603/3376) | 81.0 (2052/2532) | 54.7 (1384/2532) | 83.4 (3224/3864) | 85.9 (2489/2898) | 59.5 (1723/2898) | 86.9 (2286/2632) | 88.7 (1750/1974) | 60.7 (1199/1974) |
| Junior middle school | 79.3 (1681/2120) | 85.0 (1351/1590) | 59.1 (940/1590) | 87.0 (1525/1752) | 89.0 (1170/1314) | 63.0 (828/1314) | 92.9 (1805/1944) | 87.5 (1275/1458) | 59.5 (868/1458) |
| Senior high school or above | 82.8 (338/408) | 88.6 (271/306) | 59.2 (181/306) | 88.3 (106/120) | 83.3 (75/90) | 64.4 (58/90) | 96.0 (284/296) | 82.0 (182/222) | 57.2 (127/222) |
| Characteristic | Accuracy Rate at Baseline (%) | Accuracy Rate at Evaluation (%) | Accuracy Rate at Follow-Up (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Knowledge | Attitude | Practice | Knowledge | Attitude | Practice | Knowledge | Attitude | Practice | |
| Gender | |||||||||
| Male | 80.0 (1351/1688) | 78.2 (990/1266) | 52.3 (662/1266) | 89.9 (1287/1432) | 93.8 (1007/1074) | 81.8 (879/1074) | 94.4 (1170/1240) | 93.4 (869/930) | 70.0 (651/930) |
| Female | 77.7 (1063/1368) | 74.6 (765/1026) | 54.3 (557/1026) | 87.1 (1213/1392) | 88.8 (927/1044) | 79.2 (827/1044) | 93.0 (1042/1120) | 90.1 (757/840) | 71.0 (596/840) |
| Age | |||||||||
| 18~44 | 83.0 (372/448) | 86.0 (289/336) | 56.9 (191/336) | 94.4 (355/376) | 95.0 (268/282) | 83.3 (235/282) | 94.7 (288/304) | 98.7 (225/228) | 75.0 (171/228) |
| 45~59 | 79.4 (1130/1424) | 78.9 (843/1068) | 54.1 (578/1068) | 91.3 (1052/1152) | 94.7 (818/864) | 83.0 (717/864) | 95.2 (937/984) | 96.1 (709/738) | 74.5 (550/738) |
| ≥60 | 77.0 (912/1184) | 70.2 (623/888) | 50.7 (450/888) | 84.3 (1093/1296) | 87.9 (854/972) | 77.6 (754/972) | 92.1 (987/1072) | 86.1 (692/804) | 65.4 (526/804) |
| Education | |||||||||
| Primary school and below | 75.4 (1219/1616) | 73.8 (894/1212) | 50.4 (611/1212) | 86.7 (1782/2056) | 90.2 (1391/1542) | 78.8 (1215/1542) | 92.1 (1319/1432) | 88.2 (947/1074) | 67.6 (726/1074) |
| Junior middle school | 81.0 (901/1112) | 76.7 (640/834) | 53.6 (447/834) | 93.5 (643/688) | 95.4 (492/516) | 84.5 (436/516) | 96.0 (722/752) | 98.1 (553/564) | 74.7 (421/564) |
| Senior high school or above | 89.6 (294/328) | 89.8 (221/246) | 65.5 (161/246) | 93.8 (75/80) | 95.0 (57/60) | 91.7 (55/60) | 97.2 (171/176) | 95.5 (126/132) | 75.8 (100/132) |
| Characteristic | Knowledge | Attitude | Practice | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Difference in Accuracy Rate at Evaluation (%) | Test of Difference at Evaluation | Difference in Accuracy Rate at Follow-Up (%) | Test of Difference at Follow-Up | Difference in Accuracy Rate at Evaluation (%) | Test of Difference at Evaluation | Difference in Accuracy Rate at Follow-Up (%) | Test of Difference at Follow-Up | Difference in Accuracy Rate at Evaluation (%) | Test of Difference at Evaluation | Difference in Accuracy Rate at Follow-Up (%) | Test of Difference at Follow-Up | |
| Gender | ||||||||||||
| Male | 4.7 | χ2 = 18.426, p < 0.001 | 3.8 | χ2 = 16.314, p < 0.001 | 6.6 | χ2 = 32.423, p < 0.001 | 5.6 | χ2 = 21.369, p < 0.001 | 20.1 | χ2 = 132.833, p < 0.001 | 9.0 | χ2 = 22.115, p < 0.001 |
| Female | 3.0 | χ2 = 6.529, p = 0.011 | 4.1 | χ2 = 14.101, p < 0.001 | 2.3 | χ2 = 3.495, p = 0.062 | 2.42 | χ2 = 3.231, p = 0.072 | 19.5 | χ2 = 121.072, p < 0.001 | 12.0 | χ2 = 34.676, p < 0.001 |
| Age, years | ||||||||||||
| 18–44 | 7.6 | χ2 = 14.448, p < 0.001 | 0.4 | χ2 = 0.052, p = 0.819 | 6.4 | χ2 = 8.691, p = 0.003 | 11.6 | χ2 = 24.705, p < 0.001 | 19.3 | χ2 = 31.764, p < 0.001 | 18.9 | χ2 = 22.674, p < 0.001 |
| 45–59 | 4.3 | χ2 = 13.867, p < 0.001 | 5.4 | χ2 = 25.289, p < 0.001 | 6.7 | χ2 = 29.380, p < 0.001 | 8.0 | χ2 = 37.584, p < 0.001 | 20.9 | χ2 = 117.402, p < 0.001 | 13.1 | χ2 = 37.317, p < 0.001 |
| ≥60 | 2.0 | χ2 = 2.553, p = 0.110 | 3.4 | χ2 = 9.063, p = 0.003 | 2.4 | χ2 = 3.122, p = 0.077 | 1.6 | χ2 = 1.287, p = 0.257 | 18.7 | χ2 = 102.901, p < 0.001 | 5.6 | χ2 = 7.372, p = 0.007 |
| Education | ||||||||||||
| Primary school and below | 3.2 | χ2 = 10.766, p = 0.001 | 5.3 | χ2 = 25.561, p < 0.001 | 4.3 | χ2 = 17.047, p < 0.001 | 0.5 | χ2 = 0.156, p = 0.693 | 19.3 | χ2 = 168.155, p < 0.001 | 6.9 | χ2 = 14.060, p < 0.001 |
| Junior middle school | 6.4 | χ2 = 20.531, p < 0.001 | 3.2 | χ2 = 9.220, p = 0.002 | 6.3 | χ2 = 17.681, p < 0.001 | 10.6 | χ2 = 52.691, p < 0.001 | 21.5 | χ2 = 80.039, p < 0.001 | 15.1 | χ2 = 40.188, p < 0.001 |
| Senior high school or above | 5.4 | χ2 = 1.638, p = 0.201 | 1.2 | χ2 = 0.468, p = 0.494 | 11.7 | χ2 = 4.640, p = 0.031 | 13.5 | χ2 = 13.290, p < 0.001 | 27.2 | χ2 = 14.357, p < 0.001 | 18.6 | χ2 = 12.382, p < 0.001 |
| Question | Control Group | Intervention Group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Accuracy Rate at Baseline (%) | Accuracy Rate at Evaluation (%) | Difference in Accuracy Rate (%) | Test | Accuracy Rate at Follow-Up (%) | Difference in Accuracy Rate (%) | Test | Accuracy Rate at Baseline (%) | Accuracy Rate at Evaluation (%) | Difference in Accuracy Rate (%) | Test | Accuracy Rate at Follow-Up (%) | Difference in Accuracy Rate (%) | Test | |
| 1. Are mammals such as cattle and sheep susceptible to schistosomiasis? | 82.4 (608/738) | 89.3 (640/717) | 6.9 | χ2 = 14.090, p < 0.001 | 97.5 (594/609) | 15.2 | χ2 = 79.747, p < 0.001 | 84.8 (324/382) | 93.2 (329/353) | 8.4 | χ2 = 13.012, p < 0.001 | 99.7 (294/295) | 14.8 | χ2 = 46.105, p < 0.001 |
| 2. Is Schistosomiasis transmitted by human and animal feces? | 78.2 (577/738) | 82.6 (592/717) | 4.4 | χ2 = 4.422, p = 0.035 | 96.1 (585/609) | 17.9 | χ2 = 89.980, p < 0.001 | 84.0 (321/382) | 89.2 (315/353) | 5.2 | χ2 = 4.262, p = 0.039 | 99.0 (292/295) | 15.0 | χ2 = 43.472, p < 0.001 |
| 3. Which animal is the intermediate host of schistosomiasis? | 95.1 (702/738) | 94.6 (678/717) | 0.6 | χ2 = 0.234, p = 0.628 | 96.1 (585/609) | 0.9 | χ2 = 0.689, p = 0.407 | 94.8 (362/382) | 95.8 (338/353) | 1.0 | χ2 = 0.394, p = 0.530 | 94.2 (278/295) | 0.5 | χ2 = 0.090, p = 0.765 |
| 4. What causes schistosomiasis? | 88.6 (654/738) | 89.3 (640/717) | 0.6 | χ2 = 0.153, p = 0.696 | 96.4 (587/609) | 7.8 | χ2 = 27.782, p < 0.001 | 82.2 (314/382) | 93.8 (331/353) | 11.6 | χ2 = 22.851, p < 0.001 | 98.0 (289/295) | 15.8 | χ2 = 42.504, p < 0.001 |
| 5. When is the most susceptible time of year for schistosomiasis? | 89.8 (663/738) | 93.0 (667/717) | 3.2 | χ2 = 4.710, p = 0.030 | 94.6 (576/609) | 4.7 | χ2 = 10.182, p = 0.001 | 89.3 (341/382) | 95.2 (336/353) | 5.9 | χ2 = 8.838, p = 0.003 | 99.3 (293/295) | 10.1 | χ2 = 28.293, p < 0.001 |
| 6. What are the common symptoms of schistosomiasis? | 13.6 (100/738) | 48.1 (345/717) | 34.6 | χ2 = 204.683, p < 0.001 | 56.2 (342/609) | 42.6 | χ2 = 274.753, p < 0.001 | 19.9 (76/382) | 57.8 (204/353) | 37.9 | χ2 = 111.7183, p < 0.001 | 77.6 (229/295) | 57.7 | χ2 = 224.110, p < 0.001 |
| 7. What is the simplest and most effective way to prevent schistosomiasis? | 91.6 (676/738) | 89.3 (640/717) | 2.3 | χ2 = 2.301, p = 0.129 | 96.2 (586/609) | 4.6 | χ2 = 12.069, p = 0.001 | 89.3 (341/382) | 90.9 (321/353) | 1.7 | χ2 = 0.570, p = 0.450 | 94.6 (279/295) | 5.3 | χ2 = 6.085, p = 0.014 |
| 8. After recovering from schistosomiasis, can you get it again? | 87.0 (642/738) | 91.1 (653/717) | 4.1 | χ2 = 6.192, p = 0.013 | 85.4 (520/609) | 1.6 | χ2 = 0.726, p = 0.394 | 87.7 (335/382) | 92.4 (326/353) | 4.7 | χ2 = 4.391, p = 0.036 | 87.5 (258/295) | 0.2 | χ2 = 0.009, p = 0.926 |
| 9. What is your attitude when the department of schistosomiasis control calls for screening for schistosomiasis? | 32.7 (241/738) | 65.1 (467/717) | 32.5 | χ2 = 153.542, p < 0.001 | 94.3 (574/609) | 61.6 | χ2 = 529.775, p < 0.001 | 36.9 (141/382) | 81.3 (287/353) | 44.4 | χ2 = 148.647, p < 0.001 | 80.3 (237/295) | 43.4 | χ2 = 127.306, p < 0.001 |
| 10. When you see a place with a schistosomiasis warning sign, what do you do? | 74.1 (547/738) | 78.5 (563/717) | 4.4 | χ2 = 3.896, p = 0.048 | 93.4 (569/609) | 19.3 | χ2 = 87.589, p < 0.001 | 60.5 (231/382) | 84.7 (299/353) | 24.2 | χ2 = 53.561, p < 0.001 | 84.8 (250/295) | 24.3 | χ2 = 47.684, p < 0.001 |
| 11. Do you want to learn about schistosomiasis control? | 96.6 (713/738) | 94.0 (674/717) | 2.6 | χ2 = 5.559, p = 0.018 | 77.5 (472/609) | 19.1 | χ2 = 141.257, p < 0.001 | 84.3 (322/382) | 96.0 (339/353) | 11.7 | χ2 = 27.931, p < 0.001 | 86.1 (254/295) | 1.8 | χ2 = 0.429, p = 0.513 |
| 12. Which ways do you like to learn about schistosomiasis prevention? | 100 (738/738) | 94.0 (674/717) | 6.0 | χ2 = 45.607, p < 0.001 | 99.8 (594/609) | 0.2 | χ2 = 18.382, p < 0.001 | 94.8 (362/382) | 96.0 (339/353) | 1.3 | χ2 = 0.670, p = 0.413 | 100.0 (295/295) | 5.2 | χ2 = 15.915, p < 0.001 |
| 13. Do you want to know the current status of native snail distribution and disease detection? | 94.4 (697/738) | 94.6 (678/717) | 0.1 | χ2 = 0.009, p = 0.923 | 82.1 (500/609) | 12.3 | χ2 = 51.366, p < 0.001 | 88.0 (336/382) | 95.8 (338/353) | 7.8 | χ2 = 14.639, p < 0.001 | 100.0 (295/295) | 12.0 | χ2 = 38.113, p < 0.001 |
| 14. Which ways do you like to learn about native snail distribution and disease detection? | 100 (738/738) | 94.6 (678/717) | 5.4 | χ2 = 41.248, p < 0.001 | 79.5 (484/609) | 20.5 | χ2 = 166.973, p < 0.001 | 95.0 (363/382) | 95.8 (338/353) | 0.7 | χ2 = 0.218, p = 0.640 | 100.0 (295/295) | 5.0 | χ2 = 15.096, p < 0.001 |
| 15. Do you cooperate when testing for schistosomiasis infection? | 93.2 (688/738) | 94.7 (679/717) | 1.5 | χ2 = 1.393, p = 0.238 | 89.8 (547/609) | 3.4 | χ2 = 5.076, p = 0.024 | 96.1 (367/382) | 96.3 (340/353) | 0.3 | χ2 = 0.030, p = 0.863 | 95.9 (283/295) | 0.1 | χ2 = 0.009, p = 0.926 |
| 16. Had you ever fished or shrimped in the wild? | 78.1 (576/738) | 70.0 (502/717) | 8.0 | χ2 = 12.230, p < 0.001 | 63.7 (388/609) | 14.3 | χ2 = 33.708, p < 0.001 | 65.5 (250/382) | 86.1 (304/353) | 20.7 | χ2 = 42.246, p < 0.001 | 89.8 (265/295) | 24.4 | χ2 = 54.377, p < 0.001 |
| 17. Did you go swimming in the wild in the summer? | 95.9 (708/738) | 92.5 (663/717) | 3.5 | χ2 = 8.033, p = 0.005 | 77.7 (473/609) | 17.8 | χ2 = 103.039, p < 0.001 | 89.3 (341/382) | 98.0 (346/353) | 8.8 | χ2 = 23.011, p < 0.001 | 89.2 (263/295) | 0.1 | χ2 = 0.002, p = 0.962 |
| 18. What protective measures did you take when farming or doing activities in areas with snails? | 0.7 (5/738) | 4.5 (32/717) | 3.8 | χ2 = 21.029, p < 0.001 | 4.1 (25/609) | 3.4 | χ2 = 18.002, p < 0.001 | 0.3 (1/382) | 49.0 (173/353) | 48.8 | χ2 = 241.270, p < 0.001 | 0 (0/295) | 0.3 | p = 1.000 |
| 19. What did you do with your untreated feces? | 57.6 (425/738) | 72.9 (523/717) | 15.4 | χ2 = 37.767, p < 0.001 | 93.4 (569/609) | 35.8 | χ2 = 221.670, p < 0.001 | 47.6 (182/382) | 96.0 (339/353) | 48.4 | χ2 = 208.154, p < 0.001 | 85.1 (251/295) | 37.4 | χ2 = 101.225, p < 0.001 |
| 20. Will you cooperate with the department of schistosomiasis control when it eliminates snails? What actions will you take? | 14.0 (103/738) | 29.3 (210/717) | 15.3 | χ2 = 50.632, p < 0.001 | 31.5 (192/609) | 17.6 | χ2 = 60.224, p < 0.001 | 20.4 (78/382) | 57.8 (204/353) | 37.4 | χ2 = 108.358, p < 0.001 | 62.7 (185/295) | 42.3 | χ2 = 125.330, p < 0.001 |
| Type | Accuracy Rate at Baseline (%) | Accuracy Rate at Evaluation (%) | Difference in Accuracy Rate (%) | Test | Accuracy Rate at Follow-Up (%) | Difference in Accuracy Rate (%) | Test |
|---|---|---|---|---|---|---|---|
| Knowledge | 91.8 (2494/2718) | 99.6 (2672/2682) | 7.9 | χ2 = 201.612, p < 0.001 | 99.9 (2797/2799) | 8.2 | χ2 = 234.284, p < 0.001 |
| Attitude | 93.7 (1981/2114) | 99.5 (2075/2086) | 5.8 | χ2 = 105.358, p < 0.001 | 99.4 (2164/2177) | 5.7 | χ2 = 105.807, p < 0.001 |
| Practice | 96.7 (876/906) | 98.2 (878/894) | 1.5 | χ2 = 4.183, p = 0.041 | 99.0 (924/933) | 2.4 | χ2 = 12.194, p < 0.001 |
| Question | Accuracy Rate at Baseline (%) | Accuracy Rate at Evaluation (%) | Difference in Accuracy Rate (%) | Test | Accuracy Rate at Follow-Up (%) | Difference in Accuracy Rate (%) | Test |
|---|---|---|---|---|---|---|---|
| 1. Do you know about schistosomiasis? | 96.4 (291/302) | 99.3 (296/298) | 3.0 | χ2 = 6.247, p = 0.012 | 100.0 (311/311) | 3.6 | χ2 = 11.535, p = 0.001 |
| 2. Which aquatic animals transmit schistosomiasis? | 75.8 (229/302) | 99.0 (295/298) | 23.2 | χ2 = 72.763, p < 0.001 | 100.0 (311/311) | 24.2 | χ2 = 85.338, p < 0.001 |
| 3. Do cattle transmit schistosomiasis? | 85.4 (258/302) | 99.3 (296/298) | 13.9 | χ2 = 40.929, p < 0.001 | 100.0 (311/311) | 14.6 | χ2 = 48.815, p < 0.001 |
| 4. What are the common symptoms of schistosomiasis patients? | 95.0 (287/302) | 99.7 (297/298) | 4.6 | χ2 = 12.395, p < 0.001 | 100.0 (311/311) | 5.0 | χ2 = 15.834, p < 0.001 |
| 5. What causes schistosomiasis? | 95.7 (289/302) | 99.7 (297/298) | 4.0 | χ2 = 10.369, p = 0.001 | 100.0 (311/311) | 4.3 | χ2 = 13.677, p < 0.001 |
| 6. Is schistosomiasis harmful to human health? | 95.0 (287/302) | 100 (298/298) | 5.0 | χ2 = 15.181, p < 0.001 | 99.7 (310/311) | 4.7 | χ2 = 13.007, p < 0.001 |
| 7. What is a symptom of advanced schistosomiasis patient? | 94.7 (286/302) | 100 (298/298) | 5.3 | χ2 = 16.221, p < 0.001 | 100.0 (311/311) | 5.3 | χ2 = 16.918, p < 0.001 |
| 8. What is a symptom of children getting schistosomiasis? | 97.4 (294/302) | 100 (298/298) | 2.7 | p = 0.007 | 100.0 (311/311) | 2.7 | p = 0.003 |
| 9. Which of the following animals gets schistosomiasis? | 90.4 (273/302) | 99.7 (297/298) | 9.3 | χ2 = 27.118, p < 0.001 | 99.7 (310/311) | 9.3 | χ2 = 28.356, p < 0.001 |
| 10. Do you go to the river to catch fish or shrimp? | 97.0 (293/302) | 99.7 (297/298) | 2.6 | p = 0.020 | 97.8 (304/311) | 0.7 | χ2 = 0.321, p = 0.571 |
| 11. Where do you usually swim in summer? | 99.0 (299/302) | 100 (298/298) | 1.0 | p = 0.249 | 100.0 (311/311) | 1.0 | p = 0.119 |
| 12. Have you ever taken a health education course on schistosomiasis? | 91.4 (276/302) | 99.7 (297/298) | 8.3 | χ2 = 23.892, p < 0.001 | 100.0 (311/311) | 8.6 | χ2 = 27.961, p < 0.001 |
| 13. Would you discourage other students from playing in the water near the ditch? | 96.7 (292/302) | 100 (298/298) | 3.3 | p = 0.002 | 98.4 (306/311) | 1.7 | χ2 = 1.863, p = 0.172 |
| 14. What do you do when the department of schistosomiasis control is testing for schistosomiasis infection? | 94.7 (286/302) | 99.7 (297/298) | 5.0 | χ2 = 13.417, p < 0.001 | 99.7 (310/311) | 5.0 | χ2 = 14.073, p < 0.001 |
| 15. What is the best way to prevent schistosomiasis? | 84.1 (254/302) | 97.3 (290/298) | 13.2 | χ2 = 30.928, p < 0.001 | 100.0 (311/311) | 15.9 | χ2 = 53.630, p < 0.001 |
| 16. Can Schistosomiasis be prevented? | 93.1 (281/302) | 100 (298/298) | 7.0 | χ2 = 21.473, p < 0.001 | 100.0 (311/311) | 7.0 | χ2 = 22.393, p < 0.001 |
| 17. Have you ever been infected and treated for schistosomiasis? | 97.0 (293/302) | 98.7 (294/298) | 1.6 | χ2 = 1.898, p = 0.168 | 100.0 (311/311) | 3.0 | p = 0.002 |
| 18. Have you swam or caught fish in the river last year? | 96.0 (290/302) | 97.3 (290/298) | 1.3 | χ2 = 0.773, p = 0.379 | 97.1 (302/311) | 1.1 | χ2 = 0.540, p = 0.463 |
| 19. Have you ever defecated indiscriminately? | 97.0 (293/302) | 98.7 (294/298) | 1.6 | χ2 = 1.898, p = 0.168 | 100.0 (311/311) | 3.0 | p = 0.002 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feng, J.; Wang, X.; Zhang, X.; Hu, H.; Xue, J.; Cao, C.; Xu, J.; Yang, P.; Li, S. Effect of Health Education on Schistosomiasis Control Knowledge, Attitude, and Practice after Schistosomiasis Blocking: Results of a Longitudinal Observational Study in the Field. Trop. Med. Infect. Dis. 2023, 8, 267. https://doi.org/10.3390/tropicalmed8050267
Feng J, Wang X, Zhang X, Hu H, Xue J, Cao C, Xu J, Yang P, Li S. Effect of Health Education on Schistosomiasis Control Knowledge, Attitude, and Practice after Schistosomiasis Blocking: Results of a Longitudinal Observational Study in the Field. Tropical Medicine and Infectious Disease. 2023; 8(5):267. https://doi.org/10.3390/tropicalmed8050267
Chicago/Turabian StyleFeng, Jiaxin, Xinyi Wang, Xia Zhang, Hehua Hu, Jingbo Xue, Chunli Cao, Jing Xu, Pin Yang, and Shizhu Li. 2023. "Effect of Health Education on Schistosomiasis Control Knowledge, Attitude, and Practice after Schistosomiasis Blocking: Results of a Longitudinal Observational Study in the Field" Tropical Medicine and Infectious Disease 8, no. 5: 267. https://doi.org/10.3390/tropicalmed8050267
APA StyleFeng, J., Wang, X., Zhang, X., Hu, H., Xue, J., Cao, C., Xu, J., Yang, P., & Li, S. (2023). Effect of Health Education on Schistosomiasis Control Knowledge, Attitude, and Practice after Schistosomiasis Blocking: Results of a Longitudinal Observational Study in the Field. Tropical Medicine and Infectious Disease, 8(5), 267. https://doi.org/10.3390/tropicalmed8050267








