Knowledge Production on Congenital Chagas Disease across Time, Borders and Disciplines: A Comprehensive Scoping Review
Abstract
:1. Introduction
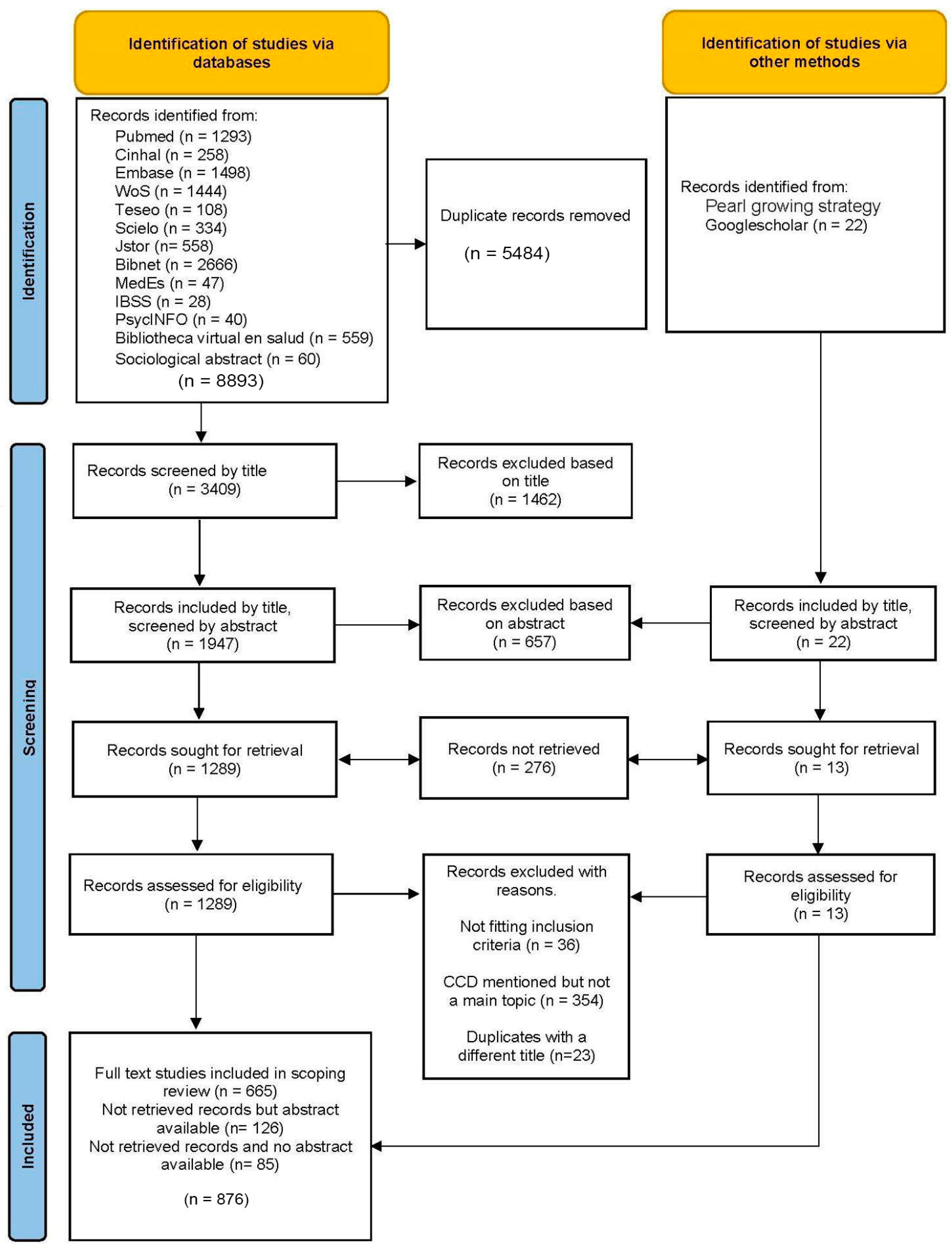
2. Materials and Methods
2.1. Research Question
- How is the current literature on CCD distributed geographically, thematically and by discipline?
- What are the gaps within the scientific literature on CCD?
- What is the geopolitical configuration of the research teams?
- What is the geopolitical configuration of the research sites and which population/countries are most studied?
- What changes can be observed through time in terms of the volume of research, themes and political geographical distribution?
- In which journals is Chagas-related research being published?
- Who are the most prolific authors?
- How do research domains co-create knowledge (translational research and bedside-to-benchtop research)?
- What problems emerge through the classification of countries and areas as endemic/non-endemic?
- How is “congenital Chagas” defined?
2.2. Data Source and Search Strategy
2.3. Study Selection
2.4. Eligibility Criteria
2.5. Data Coding
- We identified the country and city where the research was conducted in a column called “research location”;
- We identified whether the country is endemic or non-endemic;
- We then subclassified endemic countries into whether the area of research is endemic or not (NEA—non-endemic area);
- We considered whether the endemicity status has changed through time.
3. Results
3.1. Publications by Language
3.2. Publication by Year
3.3. Publication by Disciplines
3.4. Publication by Source Type
3.5. Publications by Research Locations
3.6. Publications by Subject of Study (Animal/Human/Body Part)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Maguire, B.J.; Dahal, P.; Rashan, S.; Ngu, R.; Boon, A.; Forsyth, C.; Strub-Wourgaft, N.; Chatelain, E.; Barreira, F.; Sosa-Estani, S.; et al. The Chagas disease study landscape: A systematic review of clinical and observational antiparasitic treatment studies to assess the potential for establishing an individual participant-level data platform. PLoS Negl. Trop. Dis. 2021, 15, e0009697. [Google Scholar] [CrossRef]
- Bern, C.; Kjos, S.; Yabsley, M.J.; Montgomery, S.P. Trypanosoma cruzi and Chagas’ disease in the United States. Clin. Microbiol. Rev. 2011, 24, 655–681. [Google Scholar] [CrossRef] [PubMed]
- WHO. Chagas Disease: Key Facts. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/chagas-disease-(american-trypanosomiasis)#:~:text=It%20is%20transmitted%20by%20the,is%20initiated%20soon%20after%20infection (accessed on 12 July 2023).
- Carlier, Y.; Altcheh, J.; Angheben, A.; Freilij, H.; Luquetti, A.O.; Schijman, A.G.; Segovia, M.; Wagner, N.; Vinas, P.A. Congenital Chagas disease: Updated recommendations for prevention, diagnosis, treatment, and follow-up of newborns and siblings, girls, women of childbearing age, and pregnant women. PLoS Negl. Trop. Dis. 2019, 13, e0007694. [Google Scholar] [CrossRef]
- Basile, L.; Jansá, J.M.; Carlier, Y.; Salamanca, D.D.; Angheben, A.; Bartoloni, A.; Seixas, J.; Van Gool, T.; Cañavate, C.; Flores-Chávez, M.; et al. Chagas disease in European countries: The challenge of a surveillance system. Eurosurveillance 2011, 16, 19968. [Google Scholar] [CrossRef]
- Manne-Goehler, J.; Umeh, C.A.; Montgomery, S.P.; Wirtz, V.J. Estimating the burden of Chagas Disease in the United States. PLoS Negl. Trop. Dis. 2016, 10, e0005033. [Google Scholar] [CrossRef]
- Jackson, Y.; Pinto, A.; Pett, S. Chagas disease in Australia and New Zealand: Risks and needs for public health interventions. Trop. Med. Int. Health 2014, 19, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, J.; Coll, O.; Juncosa, T.; Vergés, M.; del Pino, M.; Fumado, V.; Bosch, J.; Posada, E.J.; Hernandez, S.; Fisa, R.; et al. Prevalence and vertical transmission of Trypanosoma cruzi infection among pregnant Latin American women attending 2 maternity clinics in Barcelona, Spain. Clin. Infect. Dis. 2009, 48, 1736–1740. [Google Scholar] [CrossRef]
- Alarcón, A.; Morgan, M.; Montgomery, S.P.; Scavo, L.; Wong, E.C.; Hahn, A.; Jantausch, B. Diagnosis and treatment of congenital Chagas disease in a premature infant. J. Pediatr. Infect. Dis. Soc. 2016, 5, e28–e31. [Google Scholar] [CrossRef]
- Rodari, P.; Angheben, A.; Gennati, G.; Trezzi, L.; Bargiggia, G.; Maino, M.; Ruggeri, M.; Rampello, S.; Soavi, L.; Rizzi, M. Congenital Chagas disease in a non-endemic area: Results from a control programme in Bergamo province, Northern Italy. Travel Med. Infect. Dis. 2018, 25, 31–34. [Google Scholar] [CrossRef]
- Jackson, Y.; Myers, C.; Diana, A.; Marti, H.P.; Wolff, H.; Chappuis, F.; Loutan, L.; Gervaix, A. Congenital transmission of Chagas disease in Latin American immigrants in Switzerland. Emerg. Infect. Dis. 2009, 15, 601–603. [Google Scholar] [CrossRef] [PubMed]
- Pull, L.; Touafek, F.; Paris, L.; Le Loup, G.; Brutus, L.; Siriez, J.Y. Negativation of Trypanosoma cruzi PCR within Six Months after Treatment of a Child with Nifurtimox. PLoS Negl. Trop. Dis. 2015, 9, e0003667. [Google Scholar] [CrossRef]
- Pehrson, P.O.; Wahlgren, M.; Bengtsson, E. Intracranial calcifications probably due to congenital Chagas’ disease. Am. J. Trop. Med. Hyg. 1982, 31 Pt 1, 449–451. [Google Scholar] [CrossRef]
- Stone, R.G.M.; Gavin, P.M.; Chiodini, P.B.; Nolder, D.B.; McGettrick, P.M.; Keogh, A.B.; Mc Entagart, N.M.; Drew, R.M.; Lambert, J.M.; Ferguson, W.M. Emergence of Congenital Chagas Disease in Ireland. Pediatr. Infect. Dis. J. 2022, 41, 587–589. [Google Scholar] [CrossRef]
- Requena-Méndez, A.; Albajar-Viñas, P.; Angheben, A.; Chiodini, P.; Gascón, J.; Muñoz, J.; Chagas Disease COHEMI Working Group. Health policies to control Chagas disease transmission in European countries. PLoS Negl. Trop. Dis. 2014, 8, e3245. [Google Scholar] [CrossRef]
- Howard, E.J.; Xiong, X.; Carlier, Y.; Sosa-Estani, S.; Buekens, P. Frequency of the congenital transmission of Trypanosoma cruzi: A systematic review and meta-analysis. BJOG 2014, 121, 22–33. [Google Scholar] [CrossRef] [PubMed]
- Altcheh, J.M.; Freilij, H. (Eds.) Chagas Disease: A Clinical Approach, 1st ed.; Springer International Publishing: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Losada Galvan, I.; Alonso-Padilla, J.; Cortés-Serra, N.; Alonso-Vega, C.; Gascón, J.; Pinazo, M.J. Benznidazole for the treatment of Chagas disease. Expert Rev. Anti-Infect. Ther. 2021, 19, 547–556. [Google Scholar] [CrossRef]
- Fabbro, D.L.; Danesi, E.; Olivera, V.; Codebó, M.O.; Denner, S.; Heredia, C.; Streiger, M.; Sosa-Estani, S. Trypanocide treatment of women infected with Trypanosoma cruzi and its effect on preventing congenital Chagas. PLoS Negl. Trop. Dis. 2014, 8, e3312. [Google Scholar] [CrossRef]
- Murcia, L.; Simón, M.; Carrilero, B.; Roig, M.; Segovia, M. Treatment of infected women of childbearing age prevents congenital Trypanosoma cruzi infection by eliminating the parasitemia detected by PCR. J. Infect. Dis. 2017, 215, 1452–1458. [Google Scholar] [CrossRef]
- World Health Organization. Ending the Neglect to Attain the Sustainable Development Goals: A Road Map for Neglected Tropical Diseases 2021–2030. 2020. Available online: https://apps.who.int/iris/handle/10665/338565 (accessed on 12 July 2023).
- Kreimer, P.; Zabala, J. Producción de Conocimientos Científicos y Problemas Sociales en Países en Desarrollo. Nomadas (Colombia). 2007. Available online: https://www.proquest.com/scholarly-journals/producción-de-conocimientos-científicos-y/docview/2046696862/se-2 (accessed on 14 May 2023).
- Kreimer, P. Co-Producing Social Problems and Scientific Knowledge. Chagas Disease and the Dynamics of Research Fields in Latin America. In The Local Configuration of New Research Fields; Merz, M., Sormani, P., Eds.; Springer International Publishing: Cham, Switzerland, 2016; pp. 173–190. [Google Scholar] [CrossRef]
- Kreimer, P. Techno-Scientific Promises, Disciplinary Fields, and Social Issues in Peripheral Contexts. Sci. Cult. 2022, 32, 83–108. [Google Scholar] [CrossRef]
- Kropf, S.P.; Lima, N.T. The history of chagas disease. Reflections on science in action. Mem. Inst. Oswaldo Cruz 2021, 116. [Google Scholar] [CrossRef]
- Hassan, M.D.; Castanha, R.C.G.; Wolfram, D. Scientometric analysis of global trypanosomiasis research: 1988–2017. J. Infect. Public Health 2020, 13, 514–520. [Google Scholar] [CrossRef]
- Zabala, J.P. La Enfermedad de Chagas En La Argentina: Investigación Científica, Problemas Sociales y Políticas Sanitarias. In La Enfermedad de Chagas en la Argentina: Investigación Científica, Problemas Sociales y Políticas Sanitarias; Universidad Nacional de Quilmes: Bernal, Argentina, 2010; pp. 359–360. ISBN 978-987-558-195-1. [Google Scholar]
- Levin, L.G.; Kreimer, P.R.; Jensen, P. Chagas Disease across Contexts: Scientific Knowledge in a Globalized World. Med. Anthropol. Cross Cult. Stud. Health Illn. 2021, 40, 572–589. [Google Scholar] [CrossRef] [PubMed]
- Forsyth, C. Controlled but not cured: Structural processes and explanatory models of Chagas disease in tropical Bolivia. Soc. Sci. Med. 2015, 145, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Forsyth, C.J.; Baer, R.D. Structural Processes and Local Meaning: Explanatory Models, Political Economy, and Chagas Disease in Tropical Bolivia. Ph.D. Thesis, University of South Florida, Tampa, FL, USA, 2015. Available online: https://www.proquest.com/dissertations-theses/structural-processes-local-meaning-explanatory/docview/1767331054/se-2?accountid=138056 (accessed on 23 May 2023).
- Jimeno, I.; Mendoza, N.; Zapana, F.; de la Torre, L.; Torrico, F.; Lozano, D.; Billot, C.; Pinazo, M.J.; InSPIRES Consortium. Social determinants in the access to health care for Chagas disease: A qualitative research on family life in the “Valle Alto” of Cochabamba, Bolivia. PLoS ONE 2021, 16, e0255226. [Google Scholar] [CrossRef]
- Valdez Tah, A.R.; Huicochea Gómez, L.; Nazar Beutelspacher, A.; Ortega Canto, J.; Ramsey, J.M. La vulnerabilidad humana a la transmisión vectorial de Trypanosoma cruzi a través de los procesos de salud-enfermedad y la apropiación social del territorio. Salud Colect. 2015, 11, 191–210. [Google Scholar] [CrossRef] [PubMed]
- Ventura-Garcia, L.; Roura, M.; Pell, C.; Posada, E.; Gascón, J.; Aldasoro, E.; Muñoz, J.; Pool, R. Socio-cultural aspects of Chagas Disease: A systematic review of qualitative research. PLoS Negl. Trop. Dis. 2013, 7, e2410. [Google Scholar] [CrossRef] [PubMed]
- Mastrangelo, A. El Chagas Según Santiago: Relaciones Sociales, Ambiente, y Enfermedad de Chagas en un Paraje de Santiago del Estero. Fundación Mundo Sano, Argentina. 2009. Available online: https://www.scienceopen.com/document?vid=e9640341-13ba-4e53-8058-48100dfdac3e (accessed on 19 May 2023).
- Sanmartino, M.; Mateyca, C.; Pastorino, I.C. What are we talking about when we talk about education and Chagas? A systematic review of the issue. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165691. [Google Scholar] [CrossRef] [PubMed]
- González-Alcaide, G.; Salinas, A.; Ramos, J.M.; Dutra, W.O. Scientometrics analysis of research activity and collaboration patterns in chagas cardiomyopathy. PLoS Negl. Trop. Dis. 2018, 12, e0006602. [Google Scholar] [CrossRef]
- Dias, N.; Carvalho, B.; de Nitz, N.; Hagström, L.; Vital, T.; Hecht, M. Congenital Chagas disease: Alert of research negligence. Rev. Soc. Bras. Med. Trop. 2019, 52. [Google Scholar] [CrossRef]
- Daudt, H.M.L.; Van Mossel, C.; Scott, S.J. Enhancing the scoping study methodology: A large, inter-professional team’s experience with Arksey and O’Malley’s framework. BMC Med. Res. Methodol. 2013, 13, 48. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters MD, J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- McKeown, S.; Mir, Z.M. Considerations for conducting systematic reviews: Evaluating the performance of different methods for de-duplicating references. Syst. Rev. 2021, 10, 38. [Google Scholar] [CrossRef] [PubMed]
- Soilemezi, D.; Linceviciute, S. Synthesizing Qualitative Research: Reflections and Lessons Learnt by Two New Reviewers. Int. J. Qual. Methods 2018, 17, 1. [Google Scholar] [CrossRef]
- Canals, M.; Cáceres, D.; Alvarado, S.; Canals, A.; Cattan, P.E. Modeling Chagas disease in Chile: From vector to congenital transmission. Biosystems 2017, 156, 63–71. [Google Scholar] [CrossRef]
- Cançado, A.L.; Duarte, A.R.; Duczmal, L.H.; Ferreira, S.J.; Fonseca, C.M.; Gontijo, E.C. Penalized likelihood and multi-objective spatial scans for the detection and inference of irregular clusters. Int. J. Health Geogr. 2010, 9, 55. [Google Scholar]
- Anez, N.; Crisante, G.; Soriano, P.J. Trypanosoma cruzi congenital transmission in wild bats. Acta Trop. 2009, 109, 78–80. [Google Scholar] [CrossRef]
- Eberhard, M.; D’Alessandro, A. Congenital Trypanosoma cruzi infection in a laboratory-born squirrel monkey, Saimiri sciureus. Am. J. Trop. Med. Hyg. 1982, 31, 931–933. [Google Scholar] [CrossRef]
- Kendricks, A.L.; Gray, S.B.; Wilkerson, G.K.; Sands, C.M.; Abee, C.R.; Bernacky, B.J.; Hotez, P.J.; Bottazzi, M.E.; Craig, S.L.; Jones, K.M. Reproductive Outcomes in Rhesus Macaques (Macaca mulatta) with Naturally-acquired Trypanosoma cruzi Infection. Comp. Med. 2020, 70, 152–159. [Google Scholar] [CrossRef]
- Grieves, J.L.; Hubbard, G.B.; Williams, J.T.; VandeBerg, J.L.; Dick Edward, J.J.; López-Alvarenga, J.C.; Schlabritz-Loutsevitch, N.E. Trypanosoma cruzi in non-human primates with a history of stillbirths: A retrospective study (Papio hamadryas spp.) and case report (Macaca fascicularis). J. Med. Primatol. 2008, 37, 318–328. [Google Scholar]
- Merino, S.; Potti, J.; Moreno, J. Maternal Effort Mediates the Prevalence of Trypanosomes in the Offspring of a Passerine Bird. Proc. Natl. Acad. Sci. USA 1996, 93, 5726–5730. [Google Scholar] [CrossRef]
- Perez-Zetune, V.; Bialek, S.R.; Montgomery, S.P.; Stillwaggon, E. Congenital Chagas disease in the United States: The effect of commercially priced benznidazole on costs and benefits of maternal screening. Am. J. Trop. Med. Hyg. 2020, 102, 1086. [Google Scholar] [CrossRef]
- Stillwaggon, E.; Perez-Zetune, V.; Bialek, S.R.; Montgomery, S.P. Congenital Chagas disease in the United States: Cost savings through maternal screening. Am. J. Trop. Med. Hyg. 2018, 98, 1733. [Google Scholar] [CrossRef] [PubMed]
- Pennington, P.M.; Juárez, J.G.; Arrivillaga, M.R.; De Urioste-Stone, S.M.; Doktor, K.; Bryan, J.P.; Escobar, C.Y.; Cordón-Rosales, C. Towards Chagas disease elimination: Neonatal screening for congenital transmission in rural communities. PLoS Negl. Trop. Dis. 2017, 11, e0005783. [Google Scholar] [CrossRef] [PubMed]
- Romay-Barja, M.; Iglesias-Rus, L.; Boquete, T.; Benito, A.; Blasco-Hernández, T. Key Chagas disease missing knowledge among at-risk population in Spain affecting diagnosis and treatment. Infect. Dis. Poverty 2021, 10, 55. [Google Scholar] [CrossRef]
- Arnold, J.; Flint, J.; Casapulla, S.; Nieto, C.; Grijalva, M.J. Medical pluralism in maternal health-seeking behavior of rural women in southern Ecuador. Health Care Women Int. 2021, 42, 356–373. [Google Scholar] [CrossRef]
- Rapp, E. Chagas Congenital Screening in Switzerland: Processes of Recognition and Knowledge-Sharing. Med. Anthropol. 2021, 40, 557–571. [Google Scholar] [CrossRef] [PubMed]
- Iglesias-Rus, L.; Romay-Barja, M.; Boquete, T.; Benito, A.; Blasco-Hernandez, T. The role of the first level of health care in the approach to Chagas disease in a non-endemic country. PLoS Negl. Trop. Dis. 2019, 13, e0007937. [Google Scholar] [CrossRef]
- OPS (Organización Panamericana de la Salud). Guía Para el Diagnóstico y el Tratamiento de la Enfermedad de Chagas; OPS: Washington, DC, USA, 2018; Available online: http://iris.paho.org/xmlui/handle/123456789/49653; https://www.segib.org/programa/iniciativa-iberoamericana-sobre-chagas-congenito-ningun-bebe-con-chagas-el-camino-hacia-nuevas-generaciones-libres-de-chagas/; (accessed on 5 April 2023). [Google Scholar]
- T Junior, W.A.d.O.; Gómez i Prat, J.; Albajar-Viñas, P.; Carrazzone, C.; Kropf, S.P.; Dehousse, A.; Camargo, A.M.d.A.; Anselmi, M.; Barba, M.C.P.; Guiu, I.C.; et al. How people affected by Chagas disease have struggled with their negligence: History, associative movement and World Chagas Disease Day. Mem. Inst. Oswaldo Cruz 2022, 117. [Google Scholar] [CrossRef]
- Vanderslott, S.J. Neglect in Policy Problems: The Case of “Neglected Tropical Diseases”. Ph.D Thesis, UCL (University College London), London, UK, 2017. [Google Scholar]
- Charmillot, M. Des Maladies Comme Objets de Recherche en Sciences Sociales: Perspective Épistémologique et Éthique. Revue de l’association française de sociologie 2014. Available online: http://socio-logos.revues.org/2887 (accessed on 5 April 2023).
- Fukuoka, T.; Bessho, K.; Hosono, S.; Abukawa, D.; Mizuochi, T.; Ito, K.; Murakami, J.; Tanaka, H.; Miyoshi, Y.; Takano, T.; et al. The impact of treatment on the psychological burden of mothers of children with chronic hepatitis C virus infection: A multicenter, questionnaire survey. Sci. Rep. 2022, 12, 22116. [Google Scholar] [CrossRef]
- Tariq, S.; Elford, J.; Tookey, P.; Anderson, J.; de Ruiter, A.; O’Connell, R.; Pillen, A. “It pains me because as a woman you have to breastfeed your baby”: Decision-making about infant feeding among African women living with HIV in the UK. Sex. Transm. Infect. 2016, 92, 331–336. [Google Scholar] [CrossRef]
- Minja, A.A.; Larson, E.; Aloyce, Z.; Araya, R.; Kaale, A.; Kaaya, S.F.; Kamala, J.; Kasmani, M.N.; Komba, A.; Mwimba, A.; et al. Burden of HIV-related stigma and associated factors among women living with depression accessing PMTCT services in Dar es Salaam, Tanzania. AIDS Care 2022, 34, 1572–1579. [Google Scholar] [CrossRef]
- Rojas, M.; Noya, O.; Sosa-Estani, S.; Gascón, J. Challenges in Chagas Disease Control Through Transmission Routes. In Chagas Disease; Delgado, M.-J.P., Gascón, J., Eds.; Springer: Berlin/Heidelberg, Germany, 2020; pp. 37–55. [Google Scholar] [CrossRef]
- Castillo Riquelme, M.; Loayza Saldivia, S.; Castillo Laborde, C.; Freile Gutiérrez, B. Costo-Efectividad del Screening y Tratamiento de Mujeres Embarazadas y Recién Nacidos por Trasmisión de Chagas Congénito. Informe Preparado por los Siguientes Profesionales del DESAL 2013 Departamento de Economía de la Salud Subsecretaría de Salud Pública Ministerio de Salud de Chile. Available online: http://desal.minsal.cl/wp-content/uploads/2013/09/RE_Chagas_final_enero_2013.pdf (accessed on 14 April 2023).
- Rapp, E. Impact of Structural Barriers on Undocumented Migrants at Risk of Chagas Disease in Switzerland: A Double Burden of Neglect. In Special Edition Precarity and Health: Neglected Tropical Diseases and the Structural Inequalities Affecting Latin America(ns). Latin American Perspectives, 2023; (Forthcoming, in press). [Google Scholar]







| Inclusion Criteria | |
|---|---|
| Language | English, Spanish, French, Italian, Portuguese, German |
| Source Type | Peer-reviewed journals, theses, reports, books, policy papers, published commentaries and replies |
| Relevance | Be exclusively about congenital CD; otherwise, the section on congenital CD must be at least a significant part of the article or must provide significant or new information on the topic |
| Scope | Studies on pregnant women or women of childbearing age and studies that focus on children up to the age of 1 year (“time of general follow-up/monitoring, treatment”). Later-age studies may be included if the origin of the infection is identified as congenital. Studies with the title “congenital Chagas” even if the report concerns an adult. |
| Exclusion Criteria | Conference proceedings and paper abstracts, as we determined that we could not extract enough information from these and assumed that the worthwhile conference papers would have eventually resulted in publication. |
| Place of Research | Number of Publications | % of Production | Clinical Cases |
|---|---|---|---|
| Argentina | 164 | 24.3% | 20 |
| Brazil | 112 | 16.6% | 23 |
| Bolivia | 63 | 9.35% | 0 |
| Spain | 59 | 8.75% | 16 |
| Chile | 50 | 7.4% | 10 |
| USA | 39 | 5.8% | 7 |
| Belgium | 25 | 3.7% | 0 |
| Mexico | 24 | 3.6% | 4 |
| Venezuela | 21 | 3.1% | 1 |
| Colombia | 15 | 2.2% | 3 |
| Paraguay | 11 | 1.6% | 0 |
| Peru | 10 | 1.5% | 1 |
| Italy | 6 | 0.9% | 1 |
| Canada | 5 | 0.7% | 3 |
| Honduras | 5 | 0.7% | 1 |
| Switzerland | 5 | 0.7% | 2 |
| Ecuador | 5 | 0.7% | 0 |
| El Salvador | 4 | 0.6% | 0 |
| France | 3 | 0.45% | 1 |
| UK | 3 | 0.45% | 1 |
| Uruguay | 3 | 0.45% | 1 |
| Germany | 2 | 0.3% | 0 |
| Ireland | 2 | 0.3% | 2 |
| Sweden | 2 | 0.3% | 2 |
| Denmark | 1 | 0.15% | 0 |
| Guatemala | 1 | 0.15% | 0 |
| Japan | 1 | 0.15% | 1 |
| Americas (Systematic Review) | 1 | 0.15% | 0 |
| Worldwide Survey | 3 | 0.45% | 0 |
| Data not available | 32 | 4.75% | 11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rapp, E.; Gold, M. Knowledge Production on Congenital Chagas Disease across Time, Borders and Disciplines: A Comprehensive Scoping Review. Trop. Med. Infect. Dis. 2023, 8, 422. https://doi.org/10.3390/tropicalmed8090422
Rapp E, Gold M. Knowledge Production on Congenital Chagas Disease across Time, Borders and Disciplines: A Comprehensive Scoping Review. Tropical Medicine and Infectious Disease. 2023; 8(9):422. https://doi.org/10.3390/tropicalmed8090422
Chicago/Turabian StyleRapp, Elise, and Marina Gold. 2023. "Knowledge Production on Congenital Chagas Disease across Time, Borders and Disciplines: A Comprehensive Scoping Review" Tropical Medicine and Infectious Disease 8, no. 9: 422. https://doi.org/10.3390/tropicalmed8090422
APA StyleRapp, E., & Gold, M. (2023). Knowledge Production on Congenital Chagas Disease across Time, Borders and Disciplines: A Comprehensive Scoping Review. Tropical Medicine and Infectious Disease, 8(9), 422. https://doi.org/10.3390/tropicalmed8090422







