Molecular Prevalence and Subtypes Distribution of Blastocystis spp. in Humans of Latin America: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Selection of Studies
2.5. Data Extraction and Analysis
2.6. Quality Assessment
3. Results
3.1. Literature Search
3.2. Characteristics of Included Studies
3.3. Molecular Characteristics of the Selected Articles
3.4. Prevalence of Blastocystis spp. and Subtypes
4. Discussion
4.1. Epidemiology of Blastocystis spp. in Latin America
4.2. Protocols for Blastocystis spp. Molecular Analysis
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alexeieff, A. Sur la nature des Formations Dites “Kystes de Trichomonas intestinalis”. C. R. Seances Soc. Biol. Fil. 1911, 71, 296–298. [Google Scholar]
- Stensvold, C.R.; Lewis, H.C.; Hammerum, A.M.; Porsbo, L.J.; Nielsen, S.S.; Olsen, K.E.; Arendrup, M.C.; Nielsen, H.V.; Mølbak, K. Blastocystis: Unravelling potential risk factors and clinical significance of a common but neglected parasite. Epidemiol. Infect. 2009, 137, 1655–1663. [Google Scholar] [CrossRef]
- Tan, K.S.; Mirza, H.; Teo, J.D.; Wu, B.; Macary, P.A. Current Views on the Clinical Relevance of Blastocystis spp. Curr. Infect. Dis. Rep. 2010, 12, 28–35. [Google Scholar] [CrossRef]
- Scanlan, P.D.; Stensvold, C.R.; Rajilić-Stojanović, M.; Heilig, H.G.; De Vos, W.M.; O’Toole, P.W.; Cotter, P.D. The microbial eukaryote Blastocystis is a prevalent and diverse member of the healthy human gut microbiota. FEMS Microbiol. Ecol. 2014, 90, 326–330. [Google Scholar] [CrossRef]
- Asghari, A.; Sadraei, J.; Pirestani, M.; Mohammadpour, I. First molecular identification and subtype distribution of Blastocystis sp. isolated from hooded crows (Corvus cornix) and pigeons (Columba livia) in Tehran Province, Iran. Comp. Immunol. Microbiol. Infect. Dis. 2019, 62, 25–30. [Google Scholar] [CrossRef]
- Gabrielli, S.; Palomba, M.; Furzi, F.; Brianti, E.; Gaglio, G.; Napoli, E.; Rinaldi, L.; Alburqueque, R.A.; Mattiucci, S. Molecular Subtyping of Blastocystis sp. Isolated from Farmed Animals in Southern Italy. Microorganisms 2021, 9, 1656. [Google Scholar] [CrossRef]
- Shams, M.; Shamsi, L.; Yousefi, A.; Sadrebazzaz, A.; Asghari, A.; Mohammadi-Ghalehbin, B.; Shahabi, S.; Hatam, G. Current global status, subtype distribution and zoonotic significance of Blastocystis in dogs and cats: A systematic review and meta-analysis. Parasit. Vectors 2022, 15, 225. [Google Scholar] [CrossRef]
- Scicluna, S.M.; Tawari, B.; Clark, C.G. DNA barcoding of Blastocystis. Protist 2006, 157, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Santín, M.; Gómez-Muñoz, M.T.; Solano-Aguilar, G.; Fayer, R. Development of a new PCR protocol to detect and subtype Blastocystis spp. from humans and animals. Parasitol. Res. 2011, 109, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Mohammad Rahimi, H.; Mirjalali, H.; Niyyati, M.; Haghighi, A.; Asadzadeh Aghdaei, H.; Zali, M.R. Development and evaluation of high-resolution melting curve analysis for rapid detection and subtyping of Blastocystis and comparison the results with sequencing. Parasitol. Res. 2019, 118, 3469–3478. [Google Scholar] [CrossRef] [PubMed]
- Nemati, S.; Zali, M.R.; Johnson, P.; Mirjalali, H.; Karanis, P. Molecular prevalence and subtype distribution of Blastocystis sp. in Asia and in Australia. J. Water Health 2021, 19, 687–704. [Google Scholar] [CrossRef]
- Maloney, J.G.; Molokin, A.; Santin, M. Use of Oxford Nanopore MinION to generate full-length sequences of the Blastocystis small subunit (SSU) rRNA gene. Parasit. Vectors 2020, 13, 595. [Google Scholar] [CrossRef] [PubMed]
- Public Databases for Molecular Typing and Microbial Genome Diversity (PubMLST). Blastocystis spp. Available online: https://pubmlst.org/organisms/blastocystis-spp (accessed on 17 January 2024).
- Maloney, J.G.; Molokin, A.; Seguí, R.; Maravilla, P.; Martínez-Hernández, F.; Villalobos, G.; Tsaousis, A.D.; Gentekaki, E.; Muñoz-Antolí, C.; Klisiowicz, D.R.; et al. Identification and Molecular Characterization of Four New Blastocystis Subtypes Designated ST35-ST38. Microorganisms 2022, 11, 46. [Google Scholar] [CrossRef] [PubMed]
- Paulos, S.; Köster, P.C.; de Lucio, A.; Hernández-de-Mingo, M.; Cardona, G.A.; Fernández-Crespo, J.C.; Stensvold, C.R.; Carmena, D. Occurrence and subtype distribution of Blastocystis sp. in humans, dogs and cats sharing household in northern Spain and assessment of zoonotic transmission risk. Zoonoses Public Health 2018, 65, 993–1002. [Google Scholar] [CrossRef]
- Popruk, S.; Adao, D.E.V.; Rivera, W.L. Epidemiology and subtype distribution of Blastocystis in humans: A review. Infect. Genet. Evol. 2021, 95, 105085. [Google Scholar] [CrossRef]
- Yoshikawa, H.; Wu, Z.; Pandey, K.; Pandey, B.D.; Sherchand, J.B.; Yanagi, T.; Kanbara, H. Molecular characterization of Blastocystis isolates from children and rhesus monkeys in Kathmandu, Nepal. Vet. Parasitol. 2009, 160, 295–300. [Google Scholar] [CrossRef]
- Cian, A.; El Safadi, D.; Osman, M.; Moriniere, R.; Gantois, N.; Benamrouz-Vanneste, S.; Delgado-Viscogliosi, P.; Guyot, K.; Li, L.L.; Monchy, S.; et al. Molecular Epidemiology of Blastocystis sp. in Various Animal Groups from Two French Zoos and Evaluation of Potential Zoonotic Risk. PLoS ONE 2017, 12, e0169659. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, J.D.; Sánchez, A.; Hernández, C.; Flórez, C.; Bernal, M.C.; Giraldo, J.C.; Reyes, P.; López, M.C.; García, L.; Cooper, P.J.; et al. Geographic distribution of human Blastocystis subtypes in South America. Infect. Genet. Evol. 2016, 41, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Blastocystis sp. 2019. Available online: https://www.cdc.gov/dpdx/blastocystis/index.html (accessed on 15 October 2023).
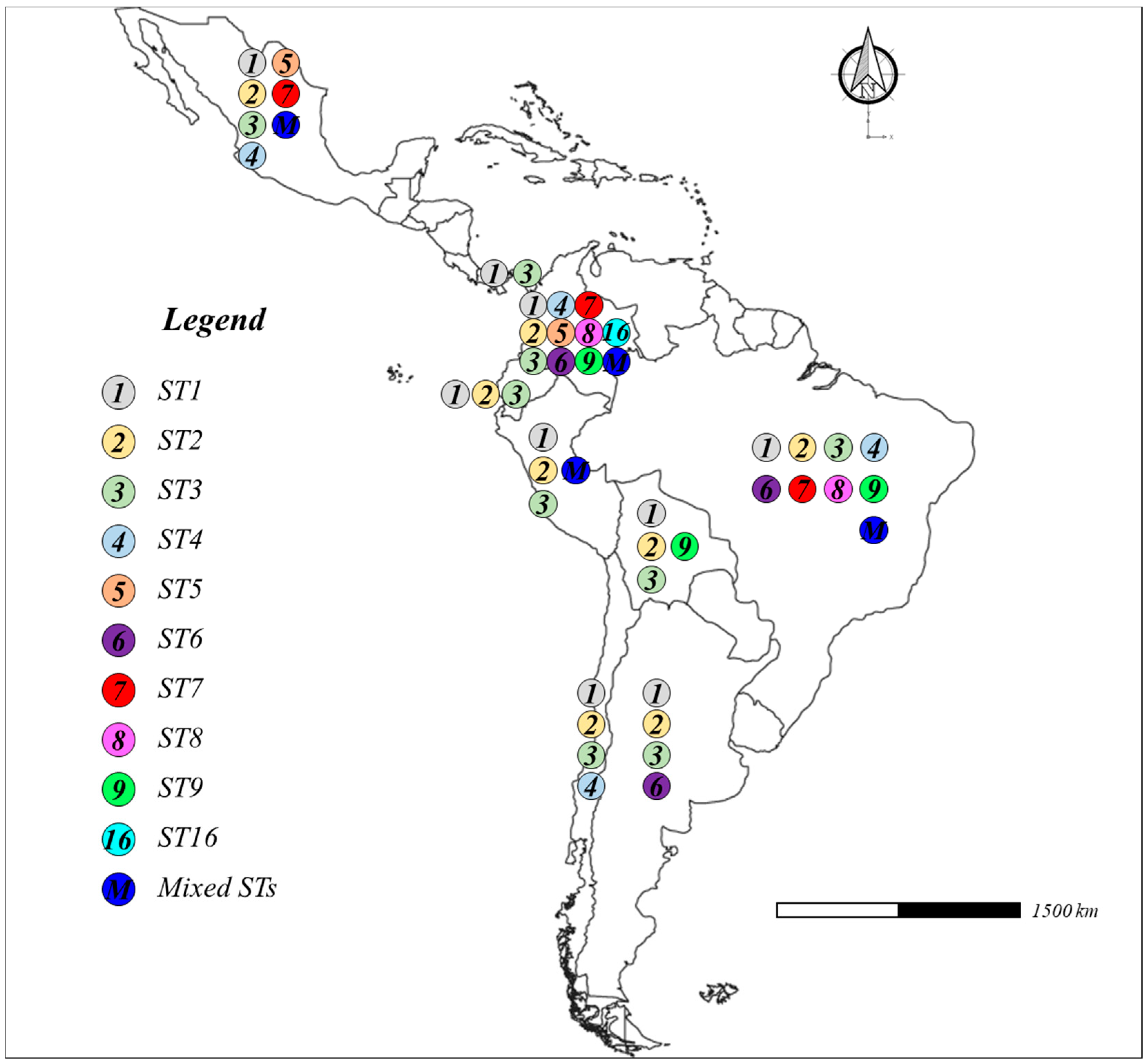
- Jiménez, P.A.; Jaimes, J.E.; Ramírez, J.D. A summary of Blastocystis subtypes in North and South America. Parasit. Vectors 2019, 12, 376. [Google Scholar] [CrossRef]
- Deng, L.; Wojciech, L.; Png, C.W.; Kioh, Y.Q.D.; Ng, G.C.; Chan, E.C.Y.; Zhang, Y.; Gascoigne, N.R.J.; Tan, K.S.W. Colonization with ubiquitous protist Blastocystis ST1 ameliorates DSS-induced colitis and promotes beneficial microbiota and immune outcomes. NPJ Biofilms Microbiomes 2023, 9, 22. [Google Scholar] [CrossRef]
- Maloney, J.G.; Molokin, A.; da Cunha, M.J.R.; Cury, M.C.; Santin, M. Blastocystis subtype distribution in domestic and captive wild bird species from Brazil using next generation amplicon sequencing. Parasite Epidemiol. Control 2020, 9, e00138. [Google Scholar] [CrossRef]
- Stensvold, C.R.; Clark, C.G. Pre-empting Pandora’s Box: Blastocystis Subtypes Revisited. Trends Parasitol. 2020, 36, 229–232. [Google Scholar] [CrossRef]
- Viesy, S.; Rezaei, Z.; Pouladi, I.; Mirzaei, A.; Abdi, J. The Prevalence of Blastocystis sp. and Its Relationship with Gastrointestinal Disorders and Risk factors. Iran. J. Parasitol. 2022, 17, 90–95. [Google Scholar]
- Abu-Madi, M.; Aly, M.; Behnke, J.M.; Clark, C.G.; Balkhy, H. The distribution of Blastocystis subtypes in isolates from Qatar. Parasit. Vectors 2015, 8, 465. [Google Scholar] [CrossRef] [PubMed]
- Poirier, P.; Wawrzyniak, I.; Vivarès, C.P.; Delbac, F.; El Alaoui, H. New insights into Blastocystis spp.: A potential link with irritable bowel syndrome. PLoS Pathog. 2012, 8, e1002545. [Google Scholar] [CrossRef] [PubMed]
- Greige, S.; El Safadi, D.; Bécu, N.; Gantois, N.; Pereira, B.; Chabé, M.; Benamrouz-Vanneste, S.; Certad, G.; El Hage, R.; Chemaly, M.; et al. Prevalence and subtype distribution of Blastocystis sp. isolates from poultry in Lebanon and evidence of zoonotic potential. Parasit. Vectors 2018, 11, 389. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Li, S.; Zou, Y.; Hong, Z.W.; Wang, P.; Zhu, X.Q.; Song, D.P.; Chen, X.Q. Prevalence and Subtype Distribution of Blastocystis sp. in Diarrheic Pigs in Southern China. Pathogens 2021, 10, 1189. [Google Scholar] [CrossRef] [PubMed]
- Nithyamathi, K.; Chandramathi, S.; Kumar, S. Predominance of Blastocystis sp. Infection among School Children in Peninsular Malaysia. PLoS ONE 2016, 11, e0136709. [Google Scholar] [CrossRef] [PubMed]
- Javanmard, E.; Niyyati, M.; Ghasemi, E.; Mirjalali, H.; Asadzadeh Aghdaei, H.; Zali, M.R. Impacts of human development index and climate conditions on prevalence of Blastocystis: A systematic review and meta-analysis. Acta Trop. 2018, 185, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Wilcox, J.J.S.; Lopez-Cotto, J.J.; Hollocher, H. Historical contingency, geography and anthropogenic patterns of exposure drive the evolution of host switching in the Blastocystis species-complex. Parasitology 2021, 148, 985–993. [Google Scholar] [CrossRef] [PubMed]
- Sarzhanov, F.; Dogruman-Al, F.; Santin, M.; Maloney, J.G.; Gureser, A.S.; Karasartova, D.; Taylan-Ozkan, A. Investigation of neglected protists Blastocystis sp. and Dientamoeba fragilis in immunocompetent and immunodeficient diarrheal patients using both conventional and molecular methods. PLoS Negl. Trop. Dis. 2021, 15, e0009779. [Google Scholar] [CrossRef]
- Deng, Y.; Zhang, S.; Ning, C.; Zhou, Y.; Teng, X.; Wu, X.; Chu, Y.; Yu, Y.; Chen, J.; Tian, L.; et al. Molecular Epidemiology and Risk Factors of Blastocystis sp. Infections among General Populations in Yunnan Province, Southwestern China. Risk Manag. Healthc. Policy 2020, 13, 1791–1801. [Google Scholar] [CrossRef]
- Matovelle, C.; Tejedor, M.T.; Monteagudo, L.V.; Beltrán, A.; Quílez, J. Prevalence and Associated Factors of Blastocystis sp. Infection in Patients with Gastrointestinal Symptoms in Spain: A Case-Control Study. Trop. Med. Infect. Dis. 2022, 7, 226. [Google Scholar] [CrossRef]
- Attah, A.O.; Sanggari, A.; Li, L.I.; Nik Him, N.A.I.I.; Ismail, A.H.; Meor Termizi, F.H. Blastocystis occurrence in water sources worldwide from 2005 to 2022: A review. Parasitol. Res. 2023, 122, 1–10. [Google Scholar] [CrossRef]
- Elseadawy, R.; Abbas, I.; Al-Araby, M.; Abu-Elwafa, S. Occurrence and molecular characterization of Acanthamoeba, Naegleria fowleri and Blastocystis in water samples from various sources in Egypt. Acta Trop. 2023, 237, 106733. [Google Scholar] [CrossRef]
- Noradilah, S.A.; Lee, I.L.; Anuar, T.S.; Salleh, F.M.; Abdul Manap, S.N.A.; Husnie, N.S.; Azrul, S.M.; Moktar, N. Blastocystis spp. contaminated water sources in aboriginal settlements. Trop. Biomed. 2017, 34, 110–117. [Google Scholar] [PubMed]
- Adamska, M. First report of Blastocystis sp. subtypes in natural water bodies in north-western Poland: A one-year monitoring. Int. J. Environ. Health Res. 2022, 32, 862–869. [Google Scholar] [CrossRef] [PubMed]
- Abdulsalam, A.M.; Ithoi, I.; Al-Mekhlafi, H.M.; Ahmed, A.; Surin, J.; Mak, J.W. Drinking water is a significant predictor of Blastocystis infection among rural Malaysian primary schoolchildren. Parasitology 2012, 139, 1014–1020. [Google Scholar] [CrossRef] [PubMed]
- Maritz, J.M.; Ten Eyck, T.A.; Elizabeth Alter, S.; Carlton, J.M. Patterns of protist diversity associated with raw sewage in New York City. ISME J. 2019, 13, 2750–2763. [Google Scholar] [CrossRef] [PubMed]
- Moreno, Y.; Moreno-Mesonero, L.; Amorós, I.; Pérez, R.; Morillo, J.A.; Alonso, J.L. Multiple identification of most important waterborne protozoa in surface water used for irrigation purposes by 18S rRNA amplicon-based metagenomics. Int. J. Hyg. Environ. Health 2018, 221, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Noradilah, S.A.; Lee, I.L.; Anuar, T.S.; Salleh, F.M.; Abdul Manap, S.N.; Mohd Mohtar, N.S.; Azrul, S.M.; Abdullah, W.O.; Moktar, N. Occurrence of Blastocystis sp. in water catchments at Malay villages and Aboriginal settlement during wet and dry seasons in Peninsular Malaysia. PeerJ 2016, 4, e2541. [Google Scholar] [CrossRef]
- Jinatham, V.; Nonebudsri, C.; Wandee, T.; Popluechai, S.; Tsaousis, A.D.; Gentekaki, E. Blastocystis in tap water of a community in northern Thailand. Parasitol. Int. 2022, 91, 102624. [Google Scholar] [CrossRef]
- Leelayoova, S.; Siripattanapipong, S.; Thathaisong, U.; Naaglor, T.; Taamasri, P.; Piyaraj, P.; Mungthin, M. Drinking water: A possible source of Blastocystis spp. subtype 1 infection in schoolchildren of a rural community in central Thailand. Am. J. Trop. Med. Hyg. 2008, 79, 401–406. [Google Scholar] [CrossRef]
- Beyhan, Y.E.; Yilmaz, H.; Cengiz, Z.T.; Ekici, A. Clinical significance and prevalence of Blastocystis hominis in Van, Turkey. Saudi Med. J. 2015, 36, 1118–1121. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Drinking Water. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/drinking-water (accessed on 15 October 2023).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Munn, Z.; Moola, S.; Lisy, K.; Riitano, D.; Tufanaru, C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int. J. Evid. Based Healthc. 2015, 13, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Candela, E.; Goizueta, C.; Periago, M.V.; Muñoz-Antoli, C. Prevalence of intestinal parasites and molecular characterization of Giardia intestinalis, Blastocystis spp. and Entamoeba histolytica in the village of Fortín Mbororé (Puerto Iguazú, Misiones, Argentina). Parasit. Vectors 2021, 14, 510. [Google Scholar] [CrossRef] [PubMed]
- Casero, R.D.; Mongi, F.; Sánchez, A.; Ramírez, J.D. Blastocystis and urticaria: Examination of subtypes and morphotypes in an unusual clinical manifestation. Acta Trop. 2015, 148, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Aruni Chura, J.; Macchioni, F.; Furzi, F.; Balboa, V.; Mercado, É.; Gómez, J.; Rojas Gonzales, P.; Poma, V.; Loup, A.; Roselli, M.; et al. Cross-sectional study on intestinal parasite infections in different ecological zones of the Department of La Paz, Bolivia. One Health 2021, 13, 100271. [Google Scholar] [CrossRef] [PubMed]
- Macchioni, F.; Segundo, H.; Totino, V.; Gabrielli, S.; Rojas, P.; Roselli, M.; Paredes, G.A.; Masana, M.; Bartoloni, A.; Cancrini, G. Intestinal parasitic infections and associated epidemiological drivers in two rural communities of the Bolivian Chaco. J. Infect. Dev. Ctries. 2016, 10, 1012–1019. [Google Scholar] [CrossRef] [PubMed]
- Macchioni, F.; Segundo, H.; Gabrielli, S.; Totino, V.; Gonzales, P.R.; Salazar, E.; Bozo, R.; Bartoloni, A.; Cancrini, G. Dramatic decrease in prevalence of soil-transmitted helminths and new insights into intestinal protozoa in children living in the Chaco region, Bolivia. Am. J. Trop. Med. Hyg. 2015, 92, 794–796. [Google Scholar] [CrossRef]
- Bertozzo, T.V.; David, É.B.; Oliveira-Arbex, A.P.; Victória, C.; Guimarães, S. Frequency, spatial distribution, and genetic diversity of Blastocystis among referred individuals to a clinical laboratory: First report of subtype 9 in Brazil. Acta Trop. 2022, 234, 106608. [Google Scholar] [CrossRef]
- Cabrine-Santos, M.; Moura, R.G.F.; Pedrosa, A.L.; Correia, D.; Oliveira-Silva, M.B. Molecular characterization of Blastocystis subtypes isolated in the city of Uberaba, Minas Gerais State, Brazil. Rev. Soc. Bras. Med. Trop. 2021, 54, e03052021. [Google Scholar] [CrossRef] [PubMed]
- Melo, G.B.; Mazzaro, M.C.; Gomes-Gouvêa, M.S.; Santos, É.A.D.; Souza, L.V.; Elias-Oliveira, J.; Gryschek, R.C.B.; Rodrigues, R.M.; Paula, F.M. Blastocystis subtypes in patients with diabetes mellitus from the Midwest region of Brazil. Rev. Inst. Med. Trop. Sao Paulo 2021, 63, e32. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.D.R.A.; Melo, G.B.; Malta, F.M.; Abdala, E.; Costa, S.F.; Pierrotti, L.C.; Gonçalves, E.M.N.; Castilho, V.L.P.; Chieffi, P.P.; Gryschek, R.C.B.; et al. Subtypes of Blastocystis sp. isolated in fecal samples from transplant candidates in São Paulo, Brazil. Parasite Epidemiol. Control 2019, 8, e00128. [Google Scholar] [CrossRef] [PubMed]
- Melo, G.B.; Malta, F.M.; Maruta, C.W.; Criado, P.R.; Castilho, V.L.P.; Gonçalves, E.M.D.N.; Espirito-Santo, M.C.C.D.; Paula, F.M.; Gryschek, R.C.B. Characterization of subtypes of Blastocystis sp. isolated from patients with urticaria, São Paulo, Brazil. Parasite Epidemiol. Control 2019, 7, e00124. [Google Scholar] [CrossRef]
- Oishi, C.Y.; Klisiowicz, D.D.R.; Seguí, R.; Köster, P.C.; Carmena, D.; Toledo, R.; Esteban, J.G.; Muñoz-Antoli, C. Reduced prevalence of soil-transmitted helminths and high frequency of protozoan infections in the surrounding urban area of Curitiba, Paraná, Brazil. Parasite Epidemiol. Control 2019, 7, e00115. [Google Scholar] [CrossRef]
- Barbosa, C.V.; Barreto, M.M.; Andrade, R.J.; Sodré, F.; d’Avila-Levy, C.M.; Peralta, J.M.; Igreja, R.P.; de Macedo, H.W.; Santos, H.L.C. Intestinal parasite infections in a rural community of Rio de Janeiro (Brazil): Prevalence and genetic diversity of Blastocystis subtypes. PLoS ONE 2018, 13, e0193860. [Google Scholar] [CrossRef] [PubMed]
- Oliveira-Arbex, A.P.; David, É.B.; Guimarães, S. Blastocystis genetic diversity among children of low-income daycare center in Southeastern Brazil. Infect. Genet. Evol. 2018, 57, 59–63. [Google Scholar] [CrossRef]
- Seguí, R.; Muñoz-Antoli, C.; Klisiowicz, D.R.; Oishi, C.Y.; Köster, P.C.; de Lucio, A.; Hernández-de-Mingo, M.; Puente, P.; Toledo, R.; Esteban, J.G.; et al. Prevalence of intestinal parasites, with emphasis on the molecular epidemiology of Giardia duodenalis and Blastocystis sp., in the Paranaguá Bay, Brazil: A community survey. Parasit. Vectors 2018, 11, 490. [Google Scholar] [CrossRef]
- Barbosa, C.V.; de Jesus Batista, R.; Pereira Igreja, R.; d’Avila Levy, C.M.; Werneck de Macedo, H.; Carneiro Santos, H.L. Distribution of Blastocystis subtypes isolated from humans from an urban community in Rio de Janeiro, Brazil. Parasit. Vectors 2017, 10, 518. [Google Scholar] [CrossRef] [PubMed]
- David, É.B.; Guimarães, S.; de Oliveira, A.P.; Goulart de Oliveira-Sequeira, T.C.; Nogueira Bittencourt, G.; Moraes Nardi, A.R.; Martins Ribolla, P.E.; Bueno Franco, R.M.; Branco, N.; Tosini, F.; et al. Molecular characterization of intestinal protozoa in two poor communities in the State of São Paulo, Brazil. Parasit. Vectors 2015, 8, 103. [Google Scholar] [CrossRef] [PubMed]
- Peña, S.; Carrasco, G.; Rojas, P.; Castillo, D.; Ozaki, L.S.; Mercado, R. Determination of subtypes of Blastocystis sp. in Chilean patients with and without inflammatory bowel syndrome, A preliminary report. Parasite Epidemiol. Control 2019, 8, e00125. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Montoya, G.M.; Galvan-Diaz, A.L.; Alzate, J.F. Metataxomics reveals Blastocystis subtypes mixed infections in Colombian children. Infect. Genet. Evol. 2023, 113, 105478. [Google Scholar] [CrossRef] [PubMed]
- Hernández, P.C.; Maloney, J.G.; Molokin, A.; George, N.S.; Morales, L.; Chaparro-Olaya, J.; Santin, M. Exploring Blastocystis genetic diversity in rural schoolchildren from Colombia using next-generation amplicon sequencing reveals significant associations between contact with animals and infection risk. Parasitol. Res. 2023, 122, 1451–1462. [Google Scholar] [CrossRef] [PubMed]
- Hernández, P.C.; Morales, L.; Chaparro-Olaya, J.; de Avila, J.; Bautista-Molano, W.; Bello-Gualtero, J.; Beltrán-Ostos, A.; Romero-Sánchez, C. Frequency and distribution of Blastocystis sp. subtypes in patients with spondyloarthritis in Bogotá, Colombia. Parasite Epidemiol. Control 2021, 15, e00227. [Google Scholar] [CrossRef]
- Osorio-Pulgarin, M.I.; Higuera, A.; Beltran-Álzate, J.C.; Sánchez-Jiménez, M.; Ramírez, J.D. Epidemiological and Molecular Characterization of Blastocystis Infection in Children Attending Daycare Centers in Medellín, Colombia. Biology 2021, 10, 669. [Google Scholar] [CrossRef]
- Castañeda, S.; Muñoz, M.; Villamizar, X.; Hernández, P.C.; Vásquez, L.R.; Tito, R.Y.; Ramírez, J.D. Microbiota characterization in Blastocystis-colonized and Blastocystis-free school-age children from Colombia. Parasit. Vectors 2020, 13, 521. [Google Scholar] [CrossRef]
- Higuera, A.; Villamizar, X.; Herrera, G.; Giraldo, J.C.; Vasquez-A, L.R.; Urbano, P.; Villalobos, O.; Tovar, C.; Ramírez, J.D. Molecular detection and genotyping of intestinal protozoa from different biogeographical regions of Colombia. PeerJ 2020, 8, e8554. [Google Scholar] [CrossRef]
- Potes-Morales, C.; Osorio-Delgado, L.A.; Carranza, J.C.; Vallejo, G.A. The first molecular detection of Blastocystis subtypes in human faecal samples from Ibague, Colombia. Parasite Epidemiol. Control 2020, 9, e00132. [Google Scholar] [CrossRef]
- Villamizar, X.; Higuera, A.; Herrera, G.; Vasquez-A, L.R.; Buitron, L.; Muñoz, L.M.; Gonzalez-C, F.E.; Lopez, M.C.; Giraldo, J.C.; Ramírez, J.D. Molecular and descriptive epidemiology of intestinal protozoan parasites of children and their pets in Cauca, Colombia: A cross-sectional study. BMC Infect. Dis. 2019, 19, 190. [Google Scholar] [CrossRef] [PubMed]
- Espinosa Aranzales, A.F.; Radon, K.; Froeschl, G.; Pinzón Rondón, Á.M.; Delius, M. Prevalence and risk factors for intestinal parasitic infections in pregnant women residing in three districts of Bogotá, Colombia. BMC Public Health 2018, 18, 1071. [Google Scholar] [CrossRef] [PubMed]
- Ramírez, J.D.; Flórez, C.; Olivera, M.; Bernal, M.C.; Giraldo, J.C. Blastocystis subtyping and its association with intestinal parasites in children from different geographical regions of Colombia. PLoS ONE 2017, 12, e0172586. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, A.; Munoz, M.; Gómez, N.; Tabares, J.; Segura, L.; Salazar, Á.; Restrepo, C.; Ruíz, M.; Reyes, P.; Qian, Y.; et al. Molecular Epidemiology of Giardia, Blastocystis and Cryptosporidium among Indigenous Children from the Colombian Amazon Basin. Front. Microbiol. 2017, 8, 248. [Google Scholar] [CrossRef] [PubMed]
- Helenbrook, W.D.; Shields, W.M.; Whipps, C.M. Characterization of Blastocystis species infection in humans and mantled howler monkeys, Alouatta palliata aequatorialis, living in close proximity to one another. Parasitol. Res. 2015, 114, 2517–2525. [Google Scholar] [CrossRef] [PubMed]
- Naceanceno, K.S.; Matamoros, G.; Gabrie, J.A.; Bottazzi, M.E.; Sanchez, A.; Mejia, R. Use of Multi-Parallel Real-Time Quantitative PCR to Determine Blastocystis Prevalence and Association with Other Gastrointestinal Parasite Infection in a Rural Honduran Location. Am. J. Trop. Med. Hyg. 2020, 102, 1373–1375. [Google Scholar] [CrossRef]
- Ramírez Pérez, M.; Yáñez, C.M.; Hernández, A.M.; Sustaita, J.J.D.; Jiménez, E.G.; Andrade, M.R.; Vargas, G.G.G.; Gómez, J.O.G. Blastocystis infection frequency and subtype distribution in university students. Heliyon 2020, 6, e05729. [Google Scholar] [CrossRef]
- Rojas-Velázquez, L.; Maloney, J.G.; Molokin, A.; Morán, P.; Serrano-Vázquez, A.; González, E.; Pérez-Juárez, H.; Ximénez, C.; Santin, M. Use of next-generation amplicon sequencing to study Blastocystis genetic diversity in a rural human population from Mexico. Parasit. Vectors 2019, 12, 566. [Google Scholar] [CrossRef]
- Nieves-Ramírez, M.E.; Partida-Rodríguez, O.; Laforest-Lapointe, I.; Reynolds, L.A.; Brown, E.M.; Valdez-Salazar, A.; Morán-Silva, P.; Rojas-Velázquez, L.; Morien, E.; Parfrey, L.W.; et al. Asymptomatic Intestinal Colonization with Protist Blastocystis Is Strongly Associated with Distinct Microbiome Ecological Patterns. mSystems 2018, 3, e00007-18. [Google Scholar] [CrossRef]
- Rojas-Velázquez, L.; Morán, P.; Serrano-Vázquez, A.; Fernández, L.D.; Pérez-Juárez, H.; Poot-Hernández, A.C.; Portillo, T.; González, E.; Hernández, E.; Partida-Rodríguez, O.; et al. Genetic Diversity and Distribution of Blastocystis Subtype 3 in Human Populations, with Special Reference to a Rural Population in Central Mexico. BioMed Res. Int. 2018, 2018, 3916263. [Google Scholar] [CrossRef]
- Perea, M.; Vásquez, V.; Pineda, V.; Samudio, F.; Calzada, J.E.; Saldaña, A. Prevalence and subtype distribution of Blastocystis sp. infecting children from a rural community in Panama. Parasite Epidemiol. Control 2020, 9, e00139. [Google Scholar] [CrossRef] [PubMed]
- Ascuña-Durand, K.; Salazar-Sánchez, R.S.; Castillo-Neyra, R.; Ballón-Echegaray, J. Relative Frequency of Blastocystis Subtypes 1, 2, and 3 in Urban and Periurban Human Populations of Arequipa, Peru. Trop. Med. Infect. Dis. 2020, 5, 178. [Google Scholar] [CrossRef] [PubMed]
- Ellwanger, J.H.; Nobre, C.A.; Chies, J.A.B. Brazilian Biodiversity as a Source of Power and Sustainable Development: A Neglected Opportunity. Sustainability 2023, 15, 482. [Google Scholar] [CrossRef]
- Saneamento Ambiental—Ministério das Cidades (Governo do Brasil). Sistema Nacional de Informações sobre Saneamento: Diagnóstico dos Serviços de água e Esgotos. Available online: https://www.gov.br/cidades/pt-br/assuntos/saneamento (accessed on 15 October 2023).
- Zanetti, A.D.S.; Malheiros, A.F.; de Matos, T.A.; Longhi, F.G.; Moreira, L.M.; Silva, S.L.; Ikeda Castrillon, S.K.; Benevides Ferreira, S.M.; Ignotti, E.; Espinosa, O.A. Prevalence of Blastocystis sp. infection in several hosts in Brazil: A systematic review and meta-analysis. Parasit. Vectors 2020, 13, 30. [Google Scholar] [CrossRef]
- Fusaro, C.; Chávez-Romero, Y.A.; Prada, S.L.G.; Serrano-Silva, N.; Bernal, J.E.; González-Jiménez, F.E.; Sarria-Guzmán, Y. Burden and Epidemiology of Human Intestinal Giardia duodenalis Infection in Colombia: A Systematic Review. Trop. Med. Infect. Dis. 2022, 7, 325. [Google Scholar] [CrossRef] [PubMed]
- Mitra, A.K.; Mawson, A.R. Neglected Tropical Diseases: Epidemiology and Global Burden. Trop. Med. Infect. Dis. 2017, 2, 36. [Google Scholar] [CrossRef]
- El-Wakil, E.S.; Zalat, R.S.; El-Badry, A.A. Mapping gut parasitism patterns in a cohort of Egyptians. Sci. Rep. 2023, 13, 9961. [Google Scholar] [CrossRef]
- Wang, J.; Gong, B.; Yang, F.; Zhang, W.; Zheng, Y.; Liu, A. Subtype distribution and genetic characterizations of Blastocystis in pigs, cattle, sheep and goats in northeastern China’s Heilongjiang Province. Infect. Genet. Evol. 2018, 57, 171–176. [Google Scholar] [CrossRef]
- Deng, L.; Chai, Y.; Zhou, Z.; Liu, H.; Zhong, Z.; Hu, Y.; Fu, H.; Yue, C.; Peng, G. Epidemiology of Blastocystis sp. infection in China: A systematic review. Parasite 2019, 26, 41. [Google Scholar] [CrossRef]
- Gureser, A.S.; Karasartova, D.; Sarzhanov, F.; Kosar, N.; Taylan-Ozkan, A.; Dogruman-Al, F. Prevalence of Blastocystis and Dientamoeba fragilis in diarrheal patients in Corum, Türkiye. Parasitol. Res. 2023, 122, 2977–2987. [Google Scholar] [CrossRef]
- Malatyalı, E.; Ertabaklar, H.; Ertuğ, S. Subtype Distribution of Blastocystis in Türkiye. Turkiye Parazitol. Derg. 2023, 47, 184–189. [Google Scholar] [CrossRef]
- Kumarasamy, V.; Rajamanikam, A.; Anbazhagan, D.; Atroosh, W.M.; Azzani, M.; Subramaniyan, V.; Abdullah, S.R. Systematic Review and Meta-Analysis: Epidemiology of Human Blastocystis spp. Infection in Malaysia. Trop. Med. Infect. Dis. 2023, 8, 415. [Google Scholar] [CrossRef]
- Karimi, P.; Shafaghi-Sisi, S.; Meamar, A.R.; Razmjou, E. Molecular identification of Cryptosporidium, Giardia, and Blastocystis from stray and household cats and cat owners in Tehran, Iran. Sci. Rep. 2023, 13, 1554. [Google Scholar] [CrossRef]
- Bachi, F.; Abidat, F.; Ghaffor, Y.; Bellili, S.; Goura, S.; Belmadani, S.A. Molecular characterization of algerian strains of Blastocysts sp. Méd. Tropicale Santé Int. 2022, 2, mtsi-v2i1. [Google Scholar]
- Dacal, E.; Saugar, J.M.; de Lucio, A.; Hernández-de-Mingo, M.; Robinson, E.; Köster, P.C.; Aznar-Ruiz-de-Alegría, M.L.; Espasa, M.; Ninda, A.; Gandasegui, J.; et al. Prevalence and molecular characterization of Strongyloides stercoralis, Giardia duodenalis, Cryptosporidium spp., and Blastocystis spp. isolates in school children in Cubal, Western Angola. Parasit. Vectors 2018, 11, 67. [Google Scholar] [CrossRef]
- Cinek, O.; Polackova, K.; Odeh, R.; Alassaf, A.; Kramná, L.; Ibekwe, M.U.; Majaliwa, E.S.; Ahmadov, G.; Elmahi, B.M.E.; Mekki, H.; et al. Blastocystis in the faeces of children from six distant countries: Prevalence, quantity, subtypes and the relation to the gut bacteriome. Parasit. Vectors 2021, 14, 399. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Owen, H.; Traub, R.J.; Cuttell, L.; Inpankaew, T.; Bielefeldt-Ohmann, H. Molecular epidemiology of Blastocystis in pigs and their in-contact humans in Southeast Queensland, Australia, and Cambodia. Vet. Parasitol. 2014, 203, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Pandey, P.K.; Verma, P.; Marathe, N.; Shetty, S.; Bavdekar, A.; Patole, M.S.; Stensvold, C.R.; Shouche, Y.S. Prevalence and subtype analysis of Blastocystis in healthy Indian individuals. Infect. Genet. Evol. 2015, 31, 296–299. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, N.A.; Al-Mekhlafi, H.M.; Anuar, T.S. Subtype distribution of Blastocystis isolated from humans and associated animals in an indigenous community with poor hygiene in Peninsular Malaysia. Trop. Biomed. 2018, 35, 849–860. [Google Scholar] [PubMed]
- Belleza, M.L.; Reyes, J.C.; Tongol-Rivera, P.N.; Rivera, W.L. Subtype analysis of Blastocystis sp. isolates from human and canine hosts in an urban community in the Philippines. Parasitol. Int. 2016, 65, 291–294. [Google Scholar] [CrossRef]
- Wakid, M.H.; Aldahhasi, W.T.; Alsulami, M.N.; El-Kady, A.M.; Elshabrawy, H.A. Identification and Genetic Characterization of Blastocystis Species in Patients from Makkah, Saudi Arabia. Infect. Drug Resist. 2022, 15, 491–501. [Google Scholar] [CrossRef]
- Khaled, S.; Gantois, N.; Ly, A.T.; Senghor, S.; Even, G.; Dautel, E.; Dejager, R.; Sawant, M.; Baydoun, M.; Benamrouz-Vanneste, S.; et al. Prevalence and Subtype Distribution of Blastocystis sp. in Senegalese School Children. Microorganisms 2020, 8, 1408. [Google Scholar] [CrossRef]
- Forsell, J.; Granlund, M.; Samuelsson, L.; Koskiniemi, S.; Edebro, H.; Evengård, B. High occurrence of Blastocystis sp. subtypes 1-3 and Giardia intestinalis assemblage B among patients in Zanzibar, Tanzania. Parasit. Vectors 2016, 9, 370. [Google Scholar] [CrossRef] [PubMed]
- van Hattem, J.M.; Arcilla, M.S.; Schultsz, C.; Bootsma, M.C.; Verhaar, N.; Rebers, S.P.; Goorhuis, A.; Grobusch, M.P.; Penders, J.; de Jong, M.D.; et al. Carriage of Blastocystis spp. in travellers—A prospective longitudinal study. Travel Med. Infect. Dis. 2019, 27, 87–91. [Google Scholar] [CrossRef]
- Rudzińska, M.; Sikorska, K. Epidemiology of Blastocystis Infection: A Review of Data from Poland in Relation to Other Reports. Pathogens 2023, 12, 1050. [Google Scholar] [CrossRef] [PubMed]
- Javanmard, E.; Rahimi, H.M.; Niyyati, M.; Aghdaei, H.A.; Sharifdini, M.; Mirjalali, H.; Zali, M.R.; Karanis, P. Molecular analysis of Blastocystis sp. and its subtypes from treated wastewater routinely used for irrigation of vegetable farmlands in Iran. J. Water Health 2019, 17, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Betts, E.L.; Gentekaki, E.; Thomasz, A.; Breakell, V.; Carpenter, A.I.; Tsaousis, A.D. Genetic diversity of Blastocystis in non-primate animals. Parasitology 2018, 145, 1228–1234. [Google Scholar] [CrossRef] [PubMed]
- Rezaei Riabi, T.; Mirjalali, H.; Haghighi, A.; Rostami Nejad, M.; Pourhoseingholi, M.A.; Poirier, P.; Delbac, F.; Wawrzyniak, I.; Zali, M.R. Genetic diversity analysis of Blastocystis subtypes from both symptomatic and asymptomatic subjects using a barcoding region from the 18S rRNA gene. Infect. Genet. Evol. 2018, 61, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, C.V.; do Bomfim, T.C.B.; Teixeira, B.R.; Gentile, R.; Neto, S.F.D.C.; Magalhães, B.S.N.; Balthazar, D.A.; da Silva, F.A.; Biot, R.; d’Avila Levy, C.M.; et al. Molecular epidemiology of Blastocystis isolated from animals in the state of Rio de Janeiro, Brazil. PLoS ONE 2019, 14, e0210740. [Google Scholar]
- Scanlan, P.D.; Knight, R.; Song, S.J.; Ackermann, G.; Cotter, P.D. Prevalence and genetic diversity of Blastocystis in family units living in the United States. Infect. Genet. Evol. 2016, 45, 95–97. [Google Scholar] [CrossRef]
- Sarria-Guzmán, Y.; Chávez-Romero, Y.; Bernal, J.E.; González-Jiménez, F.E.; Serrano-Silva, N.; Fusaro, C. Molecular identification of Giardia spp. in Latin America: An updated systematic review on reports from 2017 to 2021. J. Infect. Dev. Ctries. 2022, 16, 392–401. [Google Scholar] [CrossRef]
- Vohra, P.; Sharma, M.; Chaudhary, U. A comprehensive review of diagnostic techniques for detection of Cryptosporidium parvum in stool samples. J. Pharm. 2012, 2, 15–26. Available online: http://www.iosrphr.org/papers/v2i5/Part_7/D0251526.pdf (accessed on 20 July 2022). [CrossRef]
- Edwards, S.J.; Lilford, R.J.; Thornton, J.; Hewison, J. Informed consent for clinical trials: In search of the “best” method. Soc. Sci. Med. 1998, 47, 1825–1840. [Google Scholar] [CrossRef] [PubMed]
- O’ Sullivan, L.; Feeney, L.; Crowley, R.K.; Sukumar, P.; McAuliffe, E.; Doran, P. An evaluation of the process of informed consent: Views from research participants and staff. Trials 2021, 22, 544. [Google Scholar] [CrossRef]
- Zhang, Q.; Yin, W.; Wang, X.; Zhang, Z.; Zhang, R.; Duan, Z. Blastocystis infection and subtype distribution in domestic animals in the Qinghai-Tibetan Plateau Area (QTPA) in China: A preliminary study. Parasitol. Int. 2021, 81, 102272. [Google Scholar] [CrossRef]



| Country | Reference | Collection Period | Group Studied | Age (Years) | Number of Repeat Samples |
|---|---|---|---|---|---|
| Argentina | Candela et al., 2021 [50] | 2018 | Aboriginal Communities | 1–87 | 1 |
| Casero et al., 2015 [51] | NR | Patients (Urticaria) | 1–57 | 4 | |
| Bolivia | Aruni Chura et al., 2021 [52] | 2019 | Schoolchildren | 8–9 | 1 |
| Macchioni et al., 2016 [53] | 2013 | Rural Communities | 1–83 | NR | |
| Macchioni et al., 2015 [54] | 2011 | Children | 2–12 | NR | |
| Brazil | Bertozzo et al., 2022 [55] | 2018–2020 | Patients (Laboratory) | 0–88 | NR |
| Cabrine-Santos et al., 2021 [56] | 2011–2012 | Patients (Laboratory) | 6–10 | NR | |
| Melo et al., 2021 [57] | 2015–2016 | Patients (Diabetes Mellitus) | 18–89 | NR | |
| Silva et al., 2020 [58] | 2011–2013 | Patients (Transplant) | 19–83 | NR | |
| Melo et al., 2019 [59] | 2017–2018 | Patients (Urticaria) | 13–73 | NR | |
| Oishi et al., 2019 [60] | 2014 | Schoolchildren | 0–15 | NR | |
| Barbosa et al., 2018 [61] | 2013 | Agriculture Communities | 2–87 | 1–3 | |
| Oliveira-Arbex et al., 2018 [62] | 2012–2013 | Children | 0–6 | NR | |
| Seguí et al., 2018 [63] | 2015–2016 | General Public | 0–76 | NR | |
| Barbosa et al., 2017 [64] | NR | Patients (Psychiatric Hospital) | 1–85 | NR | |
| David et al., 2015 [65] | 2011–2013 | Poor Communities | 2–75 | 3 | |
| Chile | Peña et al., 2020 [66] | 2017–2018 | Patients (Inflammatory Bowel Syndrome) | 27–44 | NR |
| Colombia | García-Montoya, Galván-Díaz, and Alzate, 2023 [67] | NR | Children | <5 | NR |
| Hernández et al., 2023 [68] | 2017 | Schoolchildren | 4–16 | 1 | |
| Hernández et al., 2021 [69] | NR | Patients (Spondyloarthritis) | 18–65 | 1 | |
| Osorio-Pulgarin et al., 2021 [70] | 2018–2019 | Children | 0–5 | NR | |
| Castañeda et al., 2020 [71] | NR | Schoolchildren | 1–5 | NR | |
| Higuera et al., 2020 [72] | NR | General Public | 1–70 | NR | |
| Potes-Morales et al., 2020 [73] | 2017–2018 | General Public | NR | NR | |
| Villamizar et al., 2019 [74] | NR | Schoolchildren | 1–5 | NR | |
| Espinosa Aranzales et al., 2018 [75] | 2015–2016 | Pregnant Women | 14–43 | 1–2 | |
| Ramírez et al., 2017 [76] | 2012–2013 | Children | 5–14 | NR | |
| Sánchez et al., 2017 [77] | NR | Indigenous Children | 1–15 | NR | |
| Ecuador | Helenbrook et al., 2015 [78] | 2011 | Rural Communities | NR | 1 |
| Honduras | Naceanceno et al., 2020 [79] | NR | Children | 0–13 | 1 |
| Mexico | Ramírez Pérez et al., 2020 [80] | 2018 | University Students | 19–21 | 3 |
| Rojas-Velázquez et al., 2019 [81] | 2014 | General Public | 2–51 | NR | |
| Nieves-Ramírez et al., 2018 [82] | 2014 | General Public | 10–53 | NR | |
| Rojas-Velázquez et al., 2018 [83] | 2015 | General Public | 2–51 | 3 | |
| Panama | Perea et al., 2020 [84] | 2017 | Children | 1–12 | 1 |
| Perú | Ascuña-Durand et al., 2020 [85] | NR | General Public | 2–82 | NR |
| Country | Reference | Concentration Method | DNA Extraction Method | Blastocystis-Specific SSU-rDNA Primers | Product Size (bp) | Amplification | STs | dST |
|---|---|---|---|---|---|---|---|---|
| Argentina | Candela et al., 2021 [50] | Ritchie concentration technique | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | 600 | PCR | ST1 ST2 ST3 | ST3 |
| Argentina | Casero et al., 2015 [51] | Formalin-ethyl acetate Hoffman sedimentation concentration technique | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | NR | PCR | ST1 ST2 ST3 ST6 | ST3 |
| Bolivia | Aruni Chura et al., 2021 [52] | Kato–Katz | Faecal DNA kit (Bioline, UK) | RD5 BhRDr | 600 | PCR | ST1 ST2 ST3 | ST1 |
| Bolivia | Macchioni et al., 2016 [53] | Ridley concentration | NucleoSpin Tissue kit (Macherey-Nagel, Duren, Germany) | F1 R1 | 1100 | PCR | ST1 ST2 ST3 | ST3 |
| Bolivia | Macchioni et al., 2015 [54] | Ridley concentration | NucleoSpin Tissue kit (Macherey-Nagel, Duren, Germany) | F1 R1 | NR | PCR | ST2 ST9 | ST2 |
| Brazil | Bertozzo et al., 2022 [55] | Centrifugation–sedimentation method | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | 600 | PCR | ST1 ST2 ST3 ST4 ST6 ST7 ST9 | ST3 |
| Brazil | Cabrine-Santos et al., 2021 [56] | Ritchie concentration technique | Magnex DNA kit (Labtest Diagnóstica S.A., Minas Gerais, Brazil) | F1 R1 | 1100 | PCR-RFLP | ST1 ST2 ST3 | ST1 |
| SSU907 F-BH SSU907 R-BH | 907 | |||||||
| SSU850 F-BH SSU850 R-BH | 850 | |||||||
| Brazil | Melo et al., 2021 [57] | Flotation zinc sulfate | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | 600 | PCR | ST1 ST2 ST3 ST6 ST7 ST8 | ST1 |
| Brazil | Silva et al., 2020 [58] | Spontaneous sedimentation technique | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | 600 | PCR | ST1 ST2 ST3 ST7 | ST3 |
| Brazil | Melo et al., 2019 [59] | Flotation zinc sulfate | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | NR | PCR | ST1 ST2 ST3 ST4 ST6 ST1 + ST3 | ST3 |
| Brazil | Oishi et al., 2019 [60] | Ritchie concentration technique | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | 600 | PCR | ST1 ST2 ST3 ST1 + ST3 | ST3 |
| Brazil | Barbosa et al., 2018 [61] | Spontaneous sedimentation technique Flotation-saturated sodium chloride solution Pavlova’s medium | Qiamp DNA Stool mini kit (Qiagen, Valencia, CA, USA) | Blast 505–532 Blast 998–1017 | 500 | PCR | ST1 ST2 ST3 ST4 ST8 | ST3 |
| Brazil | Oliveira-Arbex et al., 2018 [62] | NR | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | 600 | PCR | ST1 ST2 ST3 ST7 | ST1 |
| Brazil | Seguí et al., 2018 [63] | Ritchie concentration technique Kato–Katz | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | 600 | PCR | ST1 ST2 ST3 ST4 ST6 ST8 | ST3 |
| Brazil | Barbosa et al., 2017 [64] | Spontaneous sedimentation technique Pavlova’s medium | Qiamp DNA Stool mini kit (Qiagen, Valencia, CA, USA) | Blast 505–532 Blast 998–1017 | 500 | PCR | ST1 ST2 ST3 ST4 ST1 + ST3 | ST3 |
| Brazil | David et al., 2015 [65] | Flotation zinc sulfate | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | 600 | PCR | ST1 ST2 ST3 ST6 ST7 ST1 + ST3 ST3 + ST7 | ST3 |
| Chile | Peña et al., 2020 [66] | PARA-PAK | QIAamp DNA Stool mini kit (QIAGEN, MD, USA) | RD5 BhRDr | 600 | PCR | ST1 ST2 ST3 ST4 | NR |
| Colombia | García-Montoya, Galván-Díaz, and Alzate, 2023 [67] | Ritchie concentration technique | Norgen Stool DNA isolation kit (Norgen Biotek Corporation, Thorold, Canada) | 18S-V4F | NR | PCR | ST1 ST2 ST3 ST1 +ST3 | ST2 |
| 18S-V4R | ||||||||
| Colombia | Hernández et al., 2023 [68] | Mini-parasep SF faecal parasite concentrator (DiaSys Ltd., Berkshire, UK) | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | Blast 505–532 Blast 998–1017 | 500 | PCR | ST1 ST2 ST3 ST4 ST5 ST1 + ST2 ST1 + ST3 ST2 + ST5 ST3 + ST5 ST1 + ST2 + ST3 ST2 + ST3 + ST4 | ST2 |
| Colombia | Hernández et al., 2021 [69] | Mini-parasep SF faecal parasite concentrator (DiaSys Ltd., Berkshire, UK) | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 Blasto18SR | 1722 | Semi-nested PCR | ST1 ST2 ST3 ST6 | ST1 |
| RD5 BhRDr | 600 | Nested PCR | ||||||
| Colombia | Osorio-Pulgarin et al., 2021 [70] | Ritchie concentration technique | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | FWD F5 R F2 | NR | PCR | ST1 ST2 ST3 ST4 ST6 ST16 | ST3 |
| RD5 BhRDr | ||||||||
| Colombia | Castañeda et al., 2020 [71] | Ritchie concentration technique Kato–Katz | Norgen Stool DNA isolation kit (Norgen Biotek Corporation, Thorold, ON, Canada) | RD5 BhRDr | 600 | PCR | NR | NR |
| Colombia | Higuera et al., 2020 [72] | NR | Norgen Stool DNA isolation kit (Norgen Biotek Corporation, Thorold, ON, Canada | RD5 BhRDr | NR | PCR | ST1 ST2 ST3 ST4 ST8 ST9 | ST1 |
| FWD F5 R F2 | ||||||||
| Colombia | Potes-Morales et al., 2020 [73] | Flotation zinc sulfate | Phenol-chloroform isoamyl alcohol | b11400ForC b11710RevC | 310 | PCR | ST1 ST2 ST3 | ST1 |
| Colombia | Villamizar et al., 2019 [74] | Ritchie concentration technique Kato–Katz | Norgen Stool DNA isolation kit (Norgen Biotek Corporation, Thorold, ON, Canada) | RD5 BhRDr | NR | PCR | ST1 ST2 ST3 ST4 | ST3 |
| Colombia | Espinosa Aranzales et al., 2018 [75] | Formol-ethyl technique | Norgen Stool DNA isolation kit (Norgen Biotek Corporation, Thorold, ON, Canada) | FWD F5 R F2 | NR | qPCR | NR | NR |
| Colombia | Ramírez et al., 2017 [76] | NR | MP FastDNA soil kit (MP Biochemicals, Solon, OH, USA) | RD5 BhRDr | NR | qPCR | ST1 ST2 ST3 ST4 ST6 ST7 | ST3 |
| Colombia | Sánchez et al., 2017 [77] | NR | Norgen Stool DNA isolation kit (Norgen Biotek Corporation, Thorold, ON, Canada) | RD5 BhRDr | NR | qPCR | ST1 ST2 ST3 ST4 ST6 | ST3 |
| Ecuador | Helenbrook et al., 2015 [78] | NR | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | BLF BLR | 260 | PCR | ST1 ST2 ST3 | ST1 |
| BH1F BhRDr | 600 | |||||||
| b11400ForC b11710RevC | NR | |||||||
| Honduras | Naceanceno et al., 2020 [79] | Kato–Katz | MP FastDNA soil kit (MP Biochemicals, Solon, OH, USA) | BL18SPPF1 BL18SR2PP | 320–340 | Multi-parallel qPCR | NR | NR |
| Mexico | Ramírez Pérez et al., 2020 [80] | Ritchie concentration technique | Commercial kit (Omega Bio-Tek Inc., Norcross, GA, USA) | F1 R1 | NR | PCR | ST1 ST2 ST3 ST4 ST5 ST7 | ST3 |
| SB82 F SB82 R | 462 | |||||||
| SB155 F SB155 R | 650 | |||||||
| SB227 F SB227 R | 526 | |||||||
| SB228 F SB228 R | 473 | |||||||
| SB229 F SB229 R | 631 | |||||||
| SB332 F SB332 R | 338 | |||||||
| SB340 F SB340 R | 704 | |||||||
| SB337 F SB337 R | 487 | |||||||
| Mexico | Rojas-Velázquez et al., 2019 [81] | NR | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | Blast 505–532 Blast 998–1017 | NR | PCR | ST1 ST2 ST3 ST1 + ST2 ST1 + ST3 ST2 + ST3 | ST3 |
| Mexico | Nieves-Ramírez et al., 2018 [82] | NR | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | NR | qPCR | ST3 | ST3 |
| Mexico | Rojas-Velázquez et al., 2018 [83] | NR | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | RD5 BhRDr | 600 | PCR | ST3 | ST3 |
| Panama | Perea et al., 2020 [84] | Formalin-ethyl acetate | QIAamp DNA Stool mini kit (QIAGEN, Hilden, Germany) | BL18SPPF1 BL18SR2PP | 320–340 | PCR | ST1 ST3 | ST1 |
| Perú | Ascuña-Durand et al., 2020 [85] | Concentration saline solution | Norgen Stool DNA isolation kit | SB83 Sub 1 F SB83 Sub 1 R | 351 | PCR | ST1 ST2 ST3 ST1 + ST3 ST1 + ST2 + ST3 | ST3 |
| STs2 F STs2 R | 1500 | |||||||
| SB227 Sub 3 F SB227 Sub 3 R | 526 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fusaro, C.; Bernal, J.E.; Baldiris-Ávila, R.; González-Cuello, R.; Cisneros-Lorduy, J.; Reales-Ruiz, A.; Castro-Orozco, R.; Sarria-Guzmán, Y. Molecular Prevalence and Subtypes Distribution of Blastocystis spp. in Humans of Latin America: A Systematic Review. Trop. Med. Infect. Dis. 2024, 9, 38. https://doi.org/10.3390/tropicalmed9020038
Fusaro C, Bernal JE, Baldiris-Ávila R, González-Cuello R, Cisneros-Lorduy J, Reales-Ruiz A, Castro-Orozco R, Sarria-Guzmán Y. Molecular Prevalence and Subtypes Distribution of Blastocystis spp. in Humans of Latin America: A Systematic Review. Tropical Medicine and Infectious Disease. 2024; 9(2):38. https://doi.org/10.3390/tropicalmed9020038
Chicago/Turabian StyleFusaro, Carmine, Jaime E. Bernal, Rosa Baldiris-Ávila, Rafael González-Cuello, Julio Cisneros-Lorduy, Arley Reales-Ruiz, Raimundo Castro-Orozco, and Yohanna Sarria-Guzmán. 2024. "Molecular Prevalence and Subtypes Distribution of Blastocystis spp. in Humans of Latin America: A Systematic Review" Tropical Medicine and Infectious Disease 9, no. 2: 38. https://doi.org/10.3390/tropicalmed9020038
APA StyleFusaro, C., Bernal, J. E., Baldiris-Ávila, R., González-Cuello, R., Cisneros-Lorduy, J., Reales-Ruiz, A., Castro-Orozco, R., & Sarria-Guzmán, Y. (2024). Molecular Prevalence and Subtypes Distribution of Blastocystis spp. in Humans of Latin America: A Systematic Review. Tropical Medicine and Infectious Disease, 9(2), 38. https://doi.org/10.3390/tropicalmed9020038






