A Novel Comprehensive Classification for Non-Prosthetic Peri-Implant Fractures
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
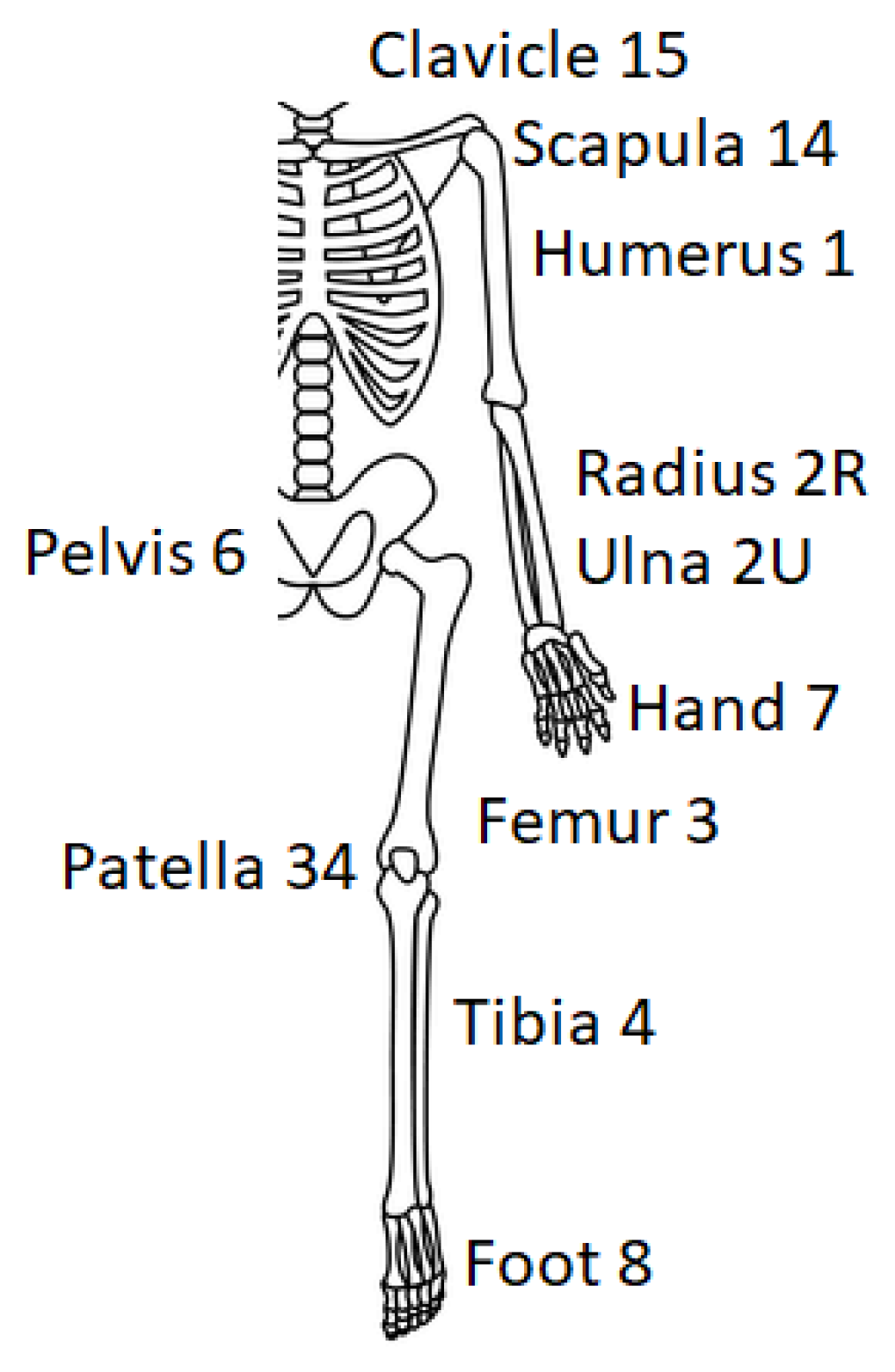
- Question about the BONE—In which bone is the fracture? Number 1–15;
- Question about the HARDWARE—What is the hardware and what is its length? A–ε and I–VI;
- Question about the FRACTURE—Where is the fracture (compared to the hardware)? A–C.
- BONE
- Number 1 identifies the humerus.
- Number 2 recognizes the forearm, and it can also be distinguished in 2R or 2U if only one bone of the forearm (radius or ulna) is considered.
- Number 3 is related to the femur, while 34 is for the patella.
- Number 4 considers the tibia (and 44, the malleoli).
- Number 5 can refer to the spine (however, this bone can be considered a little bit different).
- Number 6 is about the pelvis (same as number 5—spine).
- Number 7 characterizes the hand and consists of eight under-categories (lunate 71, scaphoid 72, capitate 73, hamate 74, trapezium 75, other carpal bones 76, metacarpals 77, phalanges 78).
- Number 8 characterizes the foot and consists of eight under-categories (talus 81, calcaneus 82, navicular 83, cuboid 84, cuneiforms 85, metatarsals 87, phalanges 88).
- Number 14 identifies the scapula.
- Number 15 refers to the clavicle.
- 2.
- HARDWARE
- α: plate and screws;
- β: screws;
- γ: nail;
- δ: K-wires;
- ε: external fixator.
- 3.
- LENGTH OF THE HARDWARE
- I: the hardware is in the proximal third of the corresponding bone;
- II: the hardware is in the middle third of the corresponding bone;
- III: the hardware is in the distal third of the corresponding bone;
- IV: the hardware is in the distal two-thirds of the bone;
- V: the hardware is in the proximal two-thirds of the bone;
- VI: the hardware lies along the entire length of the bone.
- 4.
- LEVEL OF FRACTURE
- A: the fracture is proximal to the hardware.
- B: the fracture is in correspondence of the hardware.
- ○
- B1: the fracture is in the proximal part of the hardware.
- ○
- B2: the fracture is in the middle part of the hardware.
- ○
- B3: the fracture is in the distal part of the hardware.
- C: the fracture is distal to the hardware.
References
- Seo, J.H.; Lee, B.-S.; Kim, J.-M.; Kim, J.J.; Kim, J.W. Outcomes of Dual Plating for Unstable Distal Femoral Fractures: A Subgroup Comparison between Periprosthetic and Non-Periprosthetic Fractures. Int. Orthop. 2022, 46, 2685–2692. [Google Scholar] [CrossRef] [PubMed]
- Chan, L.W.M.; Gardner, A.W.; Wong, M.K.; Chua, K.; Kwek, E.B.K. Non-Prosthetic Peri-Implant Fractures: Classification, Management and Outcomes. Arch. Orthop. Trauma Surg. 2018, 138, 791–802. [Google Scholar] [CrossRef] [PubMed]
- Barrera-Ochoa, S.; Nuñez, J.H.; Mir, X. Peri-Implant Radial and Ulnar Shaft Fractures after Volar Locking Plate Fixation of the Distal Radius. J. Hand Surg. Eur. Vol. 2018, 43, 209–210. [Google Scholar] [CrossRef]
- Al-Jabri, T.; Ridha, M.; McCulloch, R.A.; Jayadev, C.; Kayani, B.; Giannoudis, P.V. Periprosthetic Distal Femur Fractures around Total Knee Replacements: A Comprehensive Review. Injury 2023, 54, 1030–1038. [Google Scholar] [CrossRef]
- Lehmann, W.; Rupprecht, M.; Nuechtern, J.; Melzner, D.; Sellenschloh, K.; Kolb, J.; Fensky, F.; Hoffmann, M.; Püschel, K.; Morlock, M.; et al. What Is the Risk of Stress Risers for Interprosthetic Fractures of the Femur? A Biomechanical Analysis. Int. Orthop. (SICOT) 2012, 36, 2441–2446. [Google Scholar] [CrossRef]
- Ammarullah, M.I.; Afif, I.Y.; Maula, M.I.; Winarni, T.I.; Tauviqirrahman, M.; Akbar, I.; Basri, H.; van der Heide, E.; Jamari, J. Tresca Stress Simulation of Metal-on-Metal Total Hip Arthroplasty during Normal Walking Activity. Materials 2021, 14, 7554. [Google Scholar] [CrossRef]
- Ammarullah, M.I.; Hartono, R.; Supriyono, T.; Santoso, G.; Sugiharto, S.; Permana, M.S. Polycrystalline Diamond as a Potential Material for the Hard-on-Hard Bearing of Total Hip Prosthesis: Von Mises Stress Analysis. Biomedicines 2023, 11, 951. [Google Scholar] [CrossRef]
- Ammarullah, M.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Wibowo, D.; Kurdi, O.; Tauviqirrahman, M.; Jamari, J. Minimizing Risk of Failure from Ceramic-on-Ceramic Total Hip Prosthesis by Selecting Ceramic Materials Based on Tresca Stress. Sustainability 2022, 14, 13413. [Google Scholar] [CrossRef]
- Franklin, J.; Malchau, H. Risk Factors for Periprosthetic Femoral Fracture. Injury 2007, 38, 655–660. [Google Scholar] [CrossRef]
- Prieto Meré, J.A.; Barrera-Ochoa, S.; Liburd-Hernández, D.; Presas, J.P. Non-Prosthetic Peri-Implant Fracture of Both Forearm Bones. J. Surg. Case Rep. 2023, 2023, rjad300. [Google Scholar] [CrossRef] [PubMed]
- Brady, O.H.; Garbuz, D.S.; Masri, B.A.; Duncan, C.P. Classification of the hip. Orthop. Clin. N. Am. 1999, 30, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Norris, R.; Bhattacharjee, D.; Parker, M.J. Occurrence of Secondary Fracture around Intramedullary Nails Used for Trochanteric Hip Fractures: A Systematic Review of 13,568 Patients. Injury 2012, 43, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Videla-Cés, M.; Sales-Pérez, J.-M.; Sánchez-Navés, R.; Romero-Pijoan, E.; Videla, S. Proposal for the Classification of Peri-Implant Femoral Fractures: Retrospective Cohort Study. Injury 2019, 50, 758–763. [Google Scholar] [CrossRef] [PubMed]
- Müller, M.E.; Koch, P.; Nazarian, S.; Schatzker, J. The Comprehensive Classification of Fractures of Long Bones; Springer: Berlin/Heidelberg, Germany, 1990; ISBN 978-3-540-18165-1. [Google Scholar]
- Unified Classification System for Periprosthetic Fractures (UCPF). J. Orthop. Trauma 2018, 32, S141–S144. [CrossRef] [PubMed]
- Garbuz, D.S.; Masri, B.A.; Esdaile, J.; Duncan, C.P. Classification Systems in Orthopaedics. J. Am. Acad. Orthop. Surg. 2002, 10, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Marsh, J.L.; Slongo, T.F.; Agel, J.; Broderick, J.S.; Creevey, W.; DeCoster, T.A.; Prokuski, L.; Sirkin, M.S.; Ziran, B.; Henley, B.; et al. Fracture and Dislocation Classification Compendium—2007: Orthopaedic Trauma Association Classification, Database and Outcomes Committee. J. Orthop. Trauma 2007, 21, S1–S6. [Google Scholar] [CrossRef]
- Masri, B.A.; Meek, R.M.D.; Duncan, C.P. Periprosthetic Fractures Evaluation and Treatment. Clin. Orthop. Relat. Res. 2004, 420, 80–95. [Google Scholar] [CrossRef] [PubMed]
- Giannoudis, P.V.; Kanakaris, N.K.; Tsiridis, E. Principles of Internal Fixation and Selection of Implants for Periprosthetic Femoral Fractures. Injury 2007, 38, 669–687. [Google Scholar] [CrossRef] [PubMed]
- Bidolegui, F.; Pereira, S.; Munera, M.A.; Garabano, G.; Pesciallo, C.A.; Pires, R.E.; Giordano, V. Peri-Implant Femoral Fractures: Challenges, Outcomes and Proposal of a Treatment Algorithm. Chin. J. Traumatol. 2022, 26, 211–216. [Google Scholar] [CrossRef]
- Egol, K.A.; Carlock, K.D.; Kelly, E.A.; Seetharam, A.; Mullis, B.H.; Marcantonio, A.J.; Bramlett, K.J.; Nchako, C.M.; Watson, J.T.; Cannada, L.K.; et al. Previous Implant Fractures: A New Descriptive Classification System. J. Orthop. Trauma 2019, 33, 423–427. [Google Scholar] [CrossRef]
- Müller, F.; Galler, M.; Zellner, M.; Bäuml, C.; Marzouk, A.; Füchtmeier, B. Peri-Implant Femoral Fractures: The Risk Is More than Three Times Higher within PFN Compared with DHS. Injury 2016, 47, 2189–2194. [Google Scholar] [CrossRef] [PubMed]
- Kruse, M.; Mohammed, J.; Sayed-Noor, A.; Wolf, O.; Holmgren, G.; Nordström, R.; Crnalic, S.; Sköldenberg, O.; Mukka, S. Peri-Implant Femoral Fractures in Hip Fracture Patients Treated with Osteosynthesis: A Retrospective Cohort Study of 1965 Patients. Eur. J. Trauma Emerg. Surg. 2022, 48, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Liporace, F.A.; Yoon, R.S.; Collinge, C.A. Interprosthetic and Peri-Implant Fractures: Principles of Operative Fixation and Future Directions. J. Orthop. Trauma 2017, 31, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Bonnomet, F.; Favreau, H.; Bonnevialle, P.; Adam, P.; Ehlinger, M. Interimplant Femoral Fractures. Orthop. Traumatol. Surg. Res. 2022, 108, 103117. [Google Scholar] [CrossRef] [PubMed]
- Stramazzo, L.; Rovere, G.; Cioffi, A.; Vigni, G.E.; Galvano, N.; D’Arienzo, A.; Letizia Mauro, G.; Camarda, L.; D’Arienzo, M. Peri-Implant Distal Radius Fracture: Proposal of a New Classification. J. Clin. Med. 2022, 11, 2628. [Google Scholar] [CrossRef]
- Neer, C.S. Displaced Proximal Humeral Fractures. I. Classification and Evaluation. J. Bone Jt. Surg. Am. 1970, 52, 1077–1089. [Google Scholar] [CrossRef]
- Sukthankar, A.V.; Leonello, D.T.; Hertel, R.W.; Ding, G.S.; Sandow, M.J. A Comprehensive Classification of Proximal Humeral Fractures: HGLS System. J. Shoulder Elb. Surg. 2013, 22, e1–e6. [Google Scholar] [CrossRef]
- Chelli, M.; Gasbarro, G.; Lavoué, V.; Gauci, M.-O.; Raynier, J.-L.; Trojani, C.; Boileau, P. The Reliability of the Neer Classification for Proximal Humerus Fractures: A Survey of Orthopedic Shoulder Surgeons. JSES Int. 2022, 6, 331–337. [Google Scholar] [CrossRef]
- Gumina, S.; Giannicola, G.; Albino, P.; Passaretti, D.; Cinotti, G.; Postacchini, F. Comparison between Two Classifications of Humeral Head Fractures: Neer and AO-ASIF. Acta Orthop. Belg. 2011, 77, 751–757. [Google Scholar] [PubMed]
- Marongiu, G.; Leinardi, L.; Congia, S.; Frigau, L.; Mola, F.; Capone, A. Reliability and Reproducibility of the New AO/OTA 2018 Classification System for Proximal Humeral Fractures: A Comparison of Three Different Classification Systems. J. Orthop. Traumatol. 2020, 21, 4. [Google Scholar] [CrossRef]
- Stoddart, M.; Pearce, O.; Smith, J.; McCann, P.; Sheridan, B.; Al-Hourani, K. Proximal Humerus Fractures: Reliability of Neer Versus AO Classification on Plain Radiographs and Computed Tomography. Cureus 2020, 12, e8520. [Google Scholar] [CrossRef] [PubMed]
- Schatzker, J.; McBroom, R.; Bruce, D. The Tibial Plateau Fracture. The Toronto Experience 1968–1975. Clin. Orthop. Relat. Res. 1979, 138, 94–104. [Google Scholar]
- Harish, S.; Roberts, C.; Blundell, C.; Walton, N.P. AO or Schatzker? How Reliable Is Classification of Tibial Plateau Fractures? Arch. Orthop. Trauma Surg. 2003, 123, 396–398. [Google Scholar] [CrossRef] [PubMed]





| BONE | Corresponding Number |
|---|---|
| Humerus | 1 |
| Forearm | 2R 2U |
| Femur | 3 |
| Patella | 34 |
| Tibia | 4 |
| Spine | 5 |
| Pelvis | 6 |
| Hand | 7 |
| Foot | 8 |
| Scapula | 14 |
| Clavicle | 15 |
| HARDWARE | Corresponding Letter of the Greek Alphabet |
|---|---|
| Plate and screws | Alfa (α) |
| Screws | Beta (β) |
| Nail | Gamma (γ) |
| K wires | Delta (δ) |
| External fixator | Epsilon (ε) |
| HARDWARE LENGTH | Corresponding Roman Number |
|---|---|
| Proximal third | I |
| Middle third | II |
| Distal third | III |
| Proximal two-thirds of the bone | IV |
| Distal two-thirds of the bone | V |
| The entire length of the bone | VI |
| Level of Fracture Compared to the Hardware | Corresponding Capital Letter |
|---|---|
| Proximal | A |
| In correspondence | |
| ● in the proximal part | B1 |
| ● in the middle part ● in the distal part | B2 B3 |
| Distal | C |
| Bone | Hardware | Hardware Length | Site of the Fracture |
|---|---|---|---|
| 1–15 | α–ε | I–VI | A–C |
| Fleiss Kappa | Standard Error | Lower 95% CI | Upper 95% CI | p |
|---|---|---|---|---|
| 0.73 | 0.04 | 0.66 | 0.81 | <0.001 |
| Inter-Rater Reliability | ||
|---|---|---|
| Rater 1 | Rater 2 | k = 0.73 |
| Rater 1 | Rater 3 | k = 0.81 |
| Rater 1 | Rater 4 | k = 0.69 |
| Rater 1 | Rater 5 | k = 0.76 |
| Rater 2 | Rater 3 | k = 0.77 |
| Rater 2 | Rater 4 | k = 0.66 |
| Rater 2 | Rater 5 | k = 0.73 |
| Rater 3 | Rater 4 | k = 0.71 |
| Rater 3 | Rater 5 | k = 0.66 |
| Rater 4 | Rater 5 | k = 0.74 |
| Average | k = 0.73 | |
| Cohens Kappa | Standard Error | Lower 95% CI | Upper 95% CI | p |
|---|---|---|---|---|
| 0.82 | 0.07 | 0.67 | 0.96 | <0.001 |
| Intra-Rater Reliability (Weighted Kappa) | |
|---|---|
| Rater 1 | k = 0.79 |
| Rater 2 | k = 0.84 |
| Rater 3 | k = 0.96 |
| Rater 4 | k = 0.67 |
| Rater 5 | k = 0.82 |
| Average | k = 0.82 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucenti, L.; de Cristo, C.; Costarella, L.; Caldaci, A.; Sapienza, M.; Testa, G.; Pavone, V. A Novel Comprehensive Classification for Non-Prosthetic Peri-Implant Fractures. Surgeries 2023, 4, 530-543. https://doi.org/10.3390/surgeries4040052
Lucenti L, de Cristo C, Costarella L, Caldaci A, Sapienza M, Testa G, Pavone V. A Novel Comprehensive Classification for Non-Prosthetic Peri-Implant Fractures. Surgeries. 2023; 4(4):530-543. https://doi.org/10.3390/surgeries4040052
Chicago/Turabian StyleLucenti, Ludovico, Claudia de Cristo, Luciano Costarella, Alessia Caldaci, Marco Sapienza, Gianluca Testa, and Vito Pavone. 2023. "A Novel Comprehensive Classification for Non-Prosthetic Peri-Implant Fractures" Surgeries 4, no. 4: 530-543. https://doi.org/10.3390/surgeries4040052
APA StyleLucenti, L., de Cristo, C., Costarella, L., Caldaci, A., Sapienza, M., Testa, G., & Pavone, V. (2023). A Novel Comprehensive Classification for Non-Prosthetic Peri-Implant Fractures. Surgeries, 4(4), 530-543. https://doi.org/10.3390/surgeries4040052








