Abstract
Background Since COVID-19 was declared a pandemic on March 11, 2020, health care systems worldwide have been under significant strain. Although urology is not on the frontline of care for patients with COVID-19, every practicing urologist has been affected by the global outbreak. The objective of this review is to evaluate the impact of COVID-19 pandemic on urology residency training programs. Methods We reviewed the current evidence on urology residency training during the COVID-19 pandemic. Relevant databases (MEDLINE, Scopus, Cochrane Library) were searched for articles published to June 2021 that included residents’ or directors’ opinions on their residency training programs during the COVID-19 crisis. Results The literature search identified 72 articles. Fifteen studies including more than 2500 residents were eligible for inclusion in the analysis. During the pandemic, learning activities carried out by urology residents have been extensively affected. Worldwide, operation volume has decreased, especially for procedures in which residents were directly involved. Similarly, there has been a decline in most academic activities, and many studies have reported the negative impact on residents’ mental well-being and lifestyle. On the other hand, the lockdown provided an opportunity to review the current training system and to increase the implementation of tools such as telemedicine and smart-learning surgical skill training programs. Conclusions The COVID-19 pandemic has resulted in significant changes in urology residency programs worldwide, which have had a negative impact on surgical training and academic activities. Residents’ well-being and mental health have also been put at risk. However, this unprecedented situation has also generated new online learning modalities and technological innovations in the field of training in urology.
Introduction
The Covid-19 pandemic has led to major changes in medical training worldwide, including a massive reduction of face-to-face medical consultations and a decrease in elective surgical procedures, with many being postponed, sometimes indefinitely [1]. COVID-19 has dramatically transformed urologic training for residents and fellows, who make up a large component of expert personnel and who have been redeployed by many hospitals to provide critical care for COVID-19 patients [2,3].
The COVID-19 pandemic has had a significant effect on urology residency training programs, which have had to deal with not only the major reduction of residents’ involvement in medical visits and surgeries, but also the decrease of many educational and scientific activities [3,4]. Worldwide, urology residents have dealt with major challenges, not only in their medical training but also in their personal lives and their health and well-being. Concerns include social distancing, fear of contamination, and/or fear of transmitting the disease to relatives and patients, as well as reduction of income. Many studies indicate that, because of this, a significant proportion of urology residents have experienced anxiety and depression disorders during the pandemic [5,6]. The objective of this review is to evaluate the impact of the COVID-19 pandemic on clinical and surgical training, educational activities, health, and quality of life of urology residents worldwide, and to consider the residents’ point of view regarding these unprecedented circumstances.
Materials and Methods
This is a narrative review. Two authors (I.G., P.V.) performed a literature search independently using PubMed/MEDLINE, Scopus, and the Cochrane library for papers published to June 2021, with no language restriction. The search algorithm was constructed using the following terms and their associated MeSH terms and Boolean operators: “training,” “urology,” “residency,” “COVID-19.”
Duplicate studies were identified and removed. A review of citations within the articles identified additional relevant articles. Any disagreements were resolved by a third reviewer (C.F.).
The main inclusion criterion was the presence of residents’ or directors’ opinion on their residency training program during the COVID-19 pandemic. Therefore, all studies in which online resident and director surveys were conducted were included in the analysis.
Evidence Synthesis
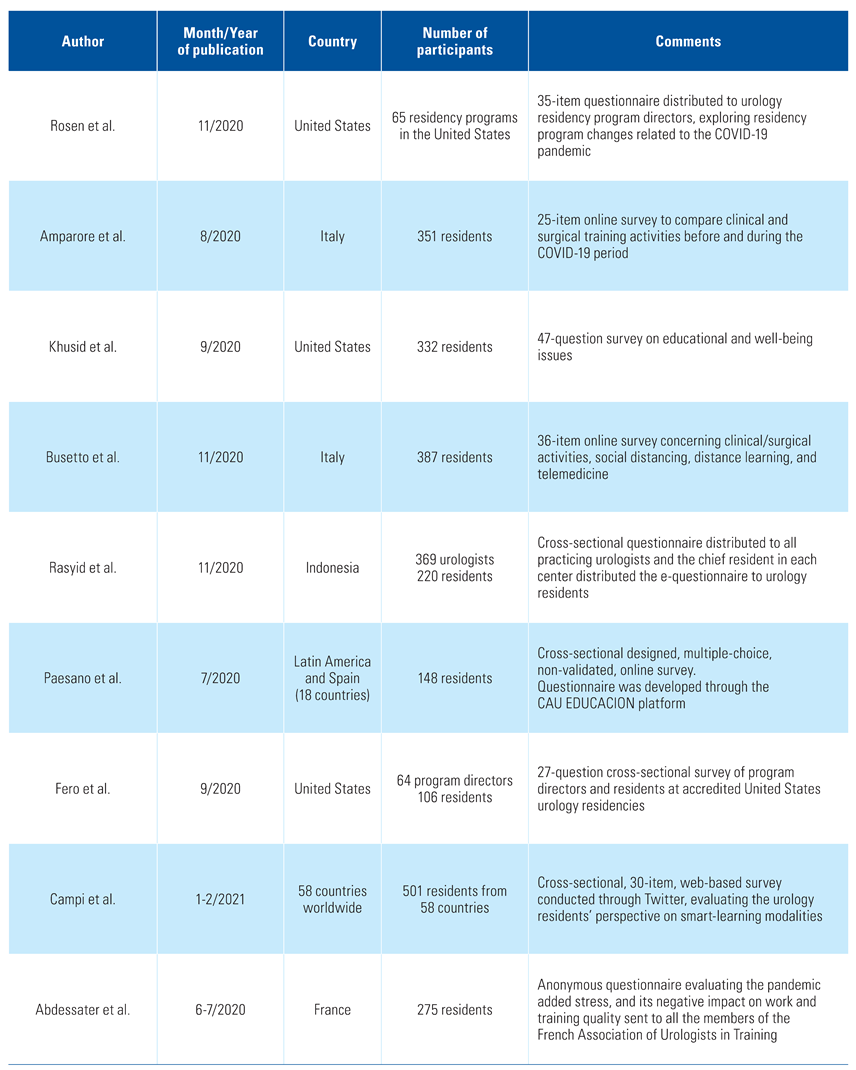
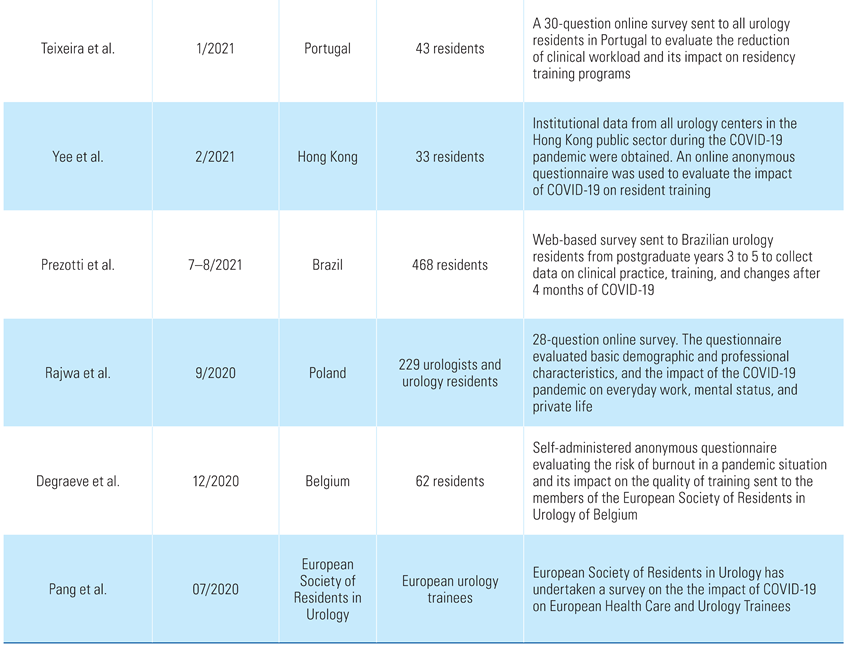
A literature search revealed a total of 72 reports. Fifteen of these (representing 2500 residents) met the inclusion criteria and were selected for analysis (Table 1).

Table 1.
Article information on urology residency training programs during the pandemic.
The study by Rosen et al. [3] was based on a 35-item questionnaire that was distributed to urology residency program directors by the Society of Academic Urologists and had a response rate of 45% (65/144). The study reported that reserve employment and redeployment had started in 80% and 26% of the training programs, respectively. Sixty percent of the programs reported concerns that residents will not meet case minimums because of COVID-19. Well-being activities focused on increased communication, while all programs had begun to use videoconferencing, and the majority planned to continue. Programs in states with a higher incidence of COVID-19 were more likely to report resident redeployment (48% versus 11%, P = 0.002) and exposure to COVID-19 positive patients (70% versus 40%, P = 0.03), and were less likely to report concerns regarding residents’ exposure (78% versus 97%, P = 0.02) and personal protective equipment availability (62% versus 89%, P = 0.02) [3].
Amparore et al. conducted a 25-item online survey sent to all Italian residents one month after the first case of COVID-19 in Italy [4]. Overall, 351 of 577 (60.8%) residents completed the questionnaire. Before the COVID-19 pandemic, the proportion of residents routinely involved in “clinical” and “surgical” activities ranged from 79.8% to 87.2% and from 49.3% to 73.5%, respectively. In the COVID-19 period, the proportion of residents experiencing a severe reduction (> 40%) or complete suppression (> 80%) of training exposure ranged between 41.1% and 81.2% for “clinical” activities and between 44.2% and 62.1% for “surgical” activities. This reduction was even more pronounced for senior residents in their final year of training [4].
The paper by Khusid et al. [7] was based on an anonymous, voluntary, 47-question survey sent to all certified urology residency programs in the United States. A total of 356 of the approximately 1800 residents in the United States (20%) responded. Results of the study showed that important risk factors regarding mental health outcomes included the perception of access to personal protective equipment, local COVID-19 severity, and perception of vulnerable household members. Respondents would be more likely to decline redeployment if given the choice if they were not currently redeployed, had children, or had concern regarding ability to reach minimum operative case numbers in urology. Respondents were more likely to have concern about reaching a surgical skill level that would allow them to operate independently after residency if elective surgeries were being cancelled and if the residents were in their final 2 years of training [7].
In the paper by Busetto et al. [8], 387 of the 577 Italian urology residents (67.1%) participated in an anonymous 36-item online survey. Participants were categorized as those working only in COVID-19 hospitals (and furthermore as “junior” and “senior” residents) and those working in any of the 3 geographical areas created according to the prevalence of COVID-19. The study reported that clinical and learning activities were significantly reduced for the overall group, while working in a COVID-19 hospital and having “senior” resident status were independent factors associated with a greater decrease in outpatient activity. Despite these facts, the study presented an optimistic point of view, reporting that the COVID-19 era can offer an opportunity to implement innovative solutions that may be part of future urology training [8].
Rasyid et al. designed a cross-sectional study based on a web questionnaire [9]. A link was sent to all practicing urologists in Indonesia, and the chief residents in each urology center distributed it to urology residents. Among residents, the response rate was 220/220 (100%). Results showed that 26.8% of the urology residents had been COVID-19 patients. Meanwhile, trainees reported high rates regarding the availability and use of personal protective equipment. The study concluded that the COVID-19 pandemic caused a decline in both outpatient clinic and surgery services [9].
Paesano et al. [10] conducted a multiple-choice, online, non-validated survey that was answered by 148 residents from 18 countries in Latin America and Spain. Eighty-two percent of the residents mentioned that their urology department’s activity was significantly reduced, while 15% stated that the urology activity had been completely terminated. Only 3% of the participants continued their regular clinical activities. At the same time, 75% of the participants stated that their surgical training had been “completely affected,” and 65% stated that their academic training had been “partially” or “completely affected.” Most of the residents supported an extension of their residency period [10].
A cross-sectional survey conducted by Fer et al. [11] was distributed among program chiefs and residents at accredited United States urology residency training centers. The responses were reported and compared between those in high versus low COVID-19 contamination geographic regions and between program leaders and residents. The response rate was 43% from program leaders and 18% from residents. Most residents (83%) claimed that they were participating in the care of COVID-19 patients while the majority of participants reported decreased surgical volume (83% to 100%) and decreased size of inpatient resident teams (99%). Regarding new technologies, 99% and 95% of participants reported increased use of telemedicine and a transition to virtual educational models, respectively. Nevertheless, the article drew attention to the downstream effects of the COVID-19 pandemic on urology residents’ training [11].
On the other hand, smart-learning modalities and contents were evaluated in detail by Campi et al. [12] in a 30-item, web-based survey conducted through Twitter. A total of 501 urology residents from 58 countries participated. More than half of the participants considered pre-recorded videos (78.4%), interactive webinars (78.2%), podcasts (56.9%) and social media (51.9%) as highly useful tools of smart learning. Similarly, updates on guidelines and surgical videos were rated highly useful modalities by the 84.8% and 81.0% of the surveyed trainees, respectively. The preferred combination of smart learning included pre-recorded surgical videos, interactive webinars, and pre-recorded videos on guidelines [12].
Teixeira et al. [13] evaluated the impact of COVID-19 pandemic on urology residents in Portugal. A 30-question online survey was sent to all urology trainees, and 54.4% responded to it. In all, 81% stated there had been a significant decrease (more than 75%) in outpatient clinical activity as well as (by 48.8%) diagnostic procedures. Participants reported that laparoscopic/robotic, endoscopic, and major open surgeries were decreased by 67.5%, 29.3%, and 17.5%, respectively. As a result, COVID-19 had a major impact on urology residency, and many residents (32.6%) considered the need to extend their residency [13].
Similarly, Yee et al. [14] examined the changes in urology practice and residency during the COVID-19 pandemic with a perspective from the authors’ experience of SARS in 2003. Authors declared reduced numbers of operating sessions (by 40.5%), clinical attendance (by 28.5%), cystoscopy sessions (by 49.6%), prostate biopsy (by 44.8%), and shockwave lithotripsy sessions (by 38.5%). Benign prostatic hyperplasia-related surgeries and ureteric stone related procedures were the most commonly delayed, while all centers gave priority to cancer-related procedures. The residents’ survey had a response rate of 48.5% and revealed that training and academic activities were heavily affected by the COVID-19 pandemic. Urology residents’ surgical exposure was significantly hindered, while 53.3% of the respondents had their professional examinations cancelled because of COVID-19 [14].
A 28-question online national survey designed by Rajwa et al. [15] to examine the impact of the COVID-19 pandemic on Polish urologists had a response rate of 28.63% (229 participants). Most of the residents (62.0%) claimed that the pandemic had harmed their training. A proportion of participants (38.9%) wanted telemedicine to permanently replace some of the consultations after the pandemic, with residents being significantly more positive about it than urologists (51.4% versus 33.1%). Furthermore, the study showed that there was a significantly negative impact on the work, mental health, and private lives of Polish urologists [15].
From another point of view, Abdessater et al. [5] assessed the psychological impact of the pandemic on young French urologists in training. A self-administered anonymous questionnaire was sent to the members of the French Association of Urologists in Training (AFUF) via email. A total of 275 members (55.5%) responded. The study concluded that the COVID-19 pandemic had a negative impact on the psychosocial well-being of the participants as more than 90% of the responders felt more stressed during the pandemic. Independent factors associated with worsening of psychological condition were past medical history of respiratory disease and caring for COVID-19 patients [5].
Similarly, Prezotti et al. [6] showed that COVID-19 has had a significant impact on Brazilian urology residents. A web-based survey was sent to 468 urology trainees in postgraduate years 3 to 5. Major reductions in patient consultations, diagnostic procedures, and surgeries were reported, while the median damage to urological training was 6.0 (on a scale from 0 to 10). Changes in health and lifestyle included weight gain (43.8%), reduced physical activity (68.6%), increased alcoholic intake (44.9%) and cigarette consumption (53.6%), decreased sexual satisfaction (25.2%), and feelings of sadness or depression (48.2%) [6].
A different perspective is highlighted in a survey by Degraeve et al. [16]. A self-administered anonymous questionnaire based on the Copenhagen Burnout Inventory score was emailed to the members of the European Society of Residents in Urology of Belgium (ESRU-B) with a response rate of 50% (62 participants). Even though 93% of the responders mentioned a negative impact of the crisis on their practical training, most of the participants reported a positive impact on their life (56%) and their theoretical training (61.7%), with a significantly reduced burnout risk score. The authors report, therefore, that the lockdown did not have negative psychological impact on Belgian residents in urology [16].
Finally, a survey undertaken by the European Society of Residents in Urology indicates that the pandemic has negatively affected the training of urology residents because of the loss of surgical exposure and inability to complete core surgical procedures. It was noted that smart-learning modalities are valuable in maintaining the learning curve of residents [17].
Discussion
The unprecedented scenario of COVID-19 has affected residency training conditions worldwide, forming a challenging environment for both trainers and residents, exacerbated by uncertainty about the duration of the pandemic [18].
The most obvious impact of COVID-19 on urology practice has been the reduction of diagnostic procedures and training operations [5,19]. Several urological associations and societies have therefore released recommendations to guide the daily clinical and surgical activities of urologists. Overall, the recommendations are based on the urgency of each procedure, the available resources of each clinic, and the risks of deferring elective interventions [20]. At the same time, recommendations from a panel of experts from the United States and Europe have been published, suggesting a list of surgeries that should be prioritized [21]. As a result, many centers reserved operating room time for cancer cases and complicated stone surgeries, while the number of cystoscopy sessions and prostate biopsies was reduced [10,22]. In addition to the decrease in urological surgical procedures, the European Association of Urology clinical recommendations suggested that the few non-deferrable surgical procedures (oncological and for life-threatening conditions) that are performed during the pandemic must be carried out by surgeons experienced in each procedure. This resulted in further decrease of resident participation in surgical operations [23]. The common goal of these measurements, as noted by Pang et al., was to reduce surgical times and risk of infection and complications, as well as to minimize spread and to free up nursing staff, anesthesiologists, ventilators, personal protective equipment, and beds [24]. With the proper use of personal protective equipment and nasopharyngeal swabs, controlled hospital access, and prompt management of suspected/positive cases, oncological and urgent cases can be managed during the COVID-19 pandemic [25].
Clinical rounds, inpatient, and outpatient care, as well as curricular and face-to-face academic activities were put on hold [18]. Residents and fellows were redeployed to pathology and intensive care units [26]. It has also been reported that in some countries, residents have been advised to stay at home if there were no clinical or ward duties to be fulfilled [27]. This had significant impact on residents’ case diaries, with mandatory training require-ments at risk of being unfulfilled [28]. Meanwhile, many university laboratories were closed, as, for example, in the United Kingdom, where those in PhD programs had been asked to return to clinical practice [24]. These delays are likely to have consequences for both clinical and basic science research [13]. Moreover, because of the suspension of non-urgent elective surgeries and the limitation of training activities, many residency examinations were postponed, as were many congresses, meetings, and national conferences [18]. Fellow of the European Board of Urology (FEBU) 2020 and the UK postgraduate fellowship examinations, as well as the European Urology Residents Education Program course 2020 were either postponed or cancelled. Extending residency programs to meet educational targets is another popular solution to the problem. Residents from the last year had their consultant examinations postponed while residency admission examinations were deferred [6].
At the same time, studies reported several independent factors associated with worsening of residents’ mental health during the COVID-19 pandemic. Inadequate access to personal protective equipment and the redeployment to a “frontline” COVID-19 service were associated with higher rates of anxiety among trainees [1]. Additionally, a past medical history of respiratory disease, as well as the presence of a household member who was susceptible to COVID-19 were associated with a higher degree of reported stress [5]. Finally, changes in trainees’ lifestyle during the pandemic included increased alcohol intake and cigarette consumption and decreased sexual satisfaction [6].
Another point of view was presented in a Belgian study by Degraeve et al., which reported a positive impact on residents’ lives and on their theoretical training during the pandemic, with a significantly reduced burnout risk score [16]. Furthermore, the pandemic has brought virtual learning options to the fore, as well as alternative resident educational activities in which applications such as Zoom and Skype enable interaction between residents and experienced physicians [19]. Initially, most urologic residency programs converted their standard conferences to digital platforms [29], and urologic educators worldwide have created daily didactic lectures, presented difficult cases on expert panels, and discussed innovative research [30]. Several urologic oncologists have held interactive virtual viewings of their robotic surgeries, serving as alternative opportunities for trainees to learn basic surgical techniques [22]. As a result, telemedicine, pre-recorded surgical videos, interactive webinars on clinical cases, and pre-recorded videos on guidelines were implemented and considered as highly useful smart-learning modalities during the pandemic [12]. These modalities do not replace the learning process in an operating room, but they encourage a new educational technology strategy that could be incorporated into educational programs in the future. The combination of the collective virtual resources of institutions worldwide may expose residents to a higher quality and more varied education [31]. In addition to maintaining resident training, telemedicine provides the opportunity of counseling patients, thus reducing unnecessary hospital visits and empowering patient self-care [32]. The use of laparoscopic and robotic simulators and 3D printing of models enables experts in surgical simulation to lead residents through guided surgeries. This can not only help residents develop their surgical skills but also learn techniques or procedures not be performed at their institutions [33]. Although distance teaching is still not considered routine, laparoscopic and robotic simulators are especially valuable because of the surgical volume is limited at most academic centers, and the likely duration of the pandemic remains uncertain [30]. These simulators also offer the chance of virtual surgical training in countries where laparoscopy and robot assisted surgery are not currently implemented in the urology residency training programs [34].
Conclusions
COVID-19 may be the greatest challenge health care systems all over the world have faced in the modern era. The COVID-19 pandemic has resulted in significant changes with negative impact in the heterogenous field of urology residency training programs worldwide. Residents’ concerns are mainly focused on their surgical training, but their well-being and mental health are also at risk. The findings of studies in this paper offer some insight into the development of best practices such as the online training modalities that are now a fundamental tool for continuous updating.
Conflicts of Interest
None declared.
References
- Ficarra, V.; Novara, G.; Abrate, A.; Bartoletti, R.; Crestani, A.; De Nunzio, C.; et al. Urology practice during the COVID-19 pandemic. Minerva Urol. Nefrol. 2020, 72, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Stock, J.A. I was deployed to a COVID unit. J. Pediatr. Urol. 2020, 16, 297–298. [Google Scholar] [CrossRef] [PubMed]
- Rosen, G.H.; Murray, K.S.; Greene, K.L.; Pruthi, R.S.; Richstone, L.; Mirza, M. Effect of COVID-19 on Urology residency training: A nationwide survey of program directors by the Society of Academic Urologists. J. Urol. 2020, 204, 1039–1045. [Google Scholar] [CrossRef] [PubMed]
- Amparore, D.; Claps, F.; Cacciamani, G.E.; Esperto, F.; Fiori, C.; Liguori, G.; et al. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol. Nefrol. 2020, 72, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Abdessater, M.; Rouprêt, M.; Misrai, V.; Matillon, X.; Gondran-Tellier, B.; Freton, L.; et al. COVID-19 pandemic impacts on anxiety of French urologist in training: Outcomes from a national survey. Prog. Urol. 2020, 30, 448–455. [Google Scholar] [CrossRef] [PubMed]
- Prezotti, J.A.; Henriques, J.V.T.; Favorito, L.A.; Canalini, A.F.; Machado, M.G.; Brandão, T.B.V.; et al. Impact of COVID-19 on education, health and lifestyle behaviour of Brazilian urology residents. Int. Braz. J. Urol. 2021, 47, 753–776. [Google Scholar] [CrossRef] [PubMed]
- Khusid, J.A.; Weinstein, C.S.; Becerra, A.Z.; Kashani, M.; Robins, D.J.; Fink, L.E.; et al. Well-being and education of urology residents during the COVID-19 pandemic: Results of an American National Survey. Int. J. Clin. Pract. 2020, 74, e13559. [Google Scholar] [CrossRef] [PubMed]
- Busetto, G.M.; Del Giudice, F.; Mari, A.; Sperduti, I.; Longo, N.; Antonelli, A.; et al. How can the COVID-19 pandemic lead to positive changes in urology residency? Front. Surg. 2020, 7, 563006. [Google Scholar] [CrossRef] [PubMed]
- Rasyid, N.; Birowo, P.; Parikesit, D.; Rahman, F. The impact of the COVID-19 pandemic on urology practice in Indonesia: A nationwide survey. Urol. J. 2020, 17, 677–679. [Google Scholar] [CrossRef] [PubMed]
- Paesano, N.; Santomil, F.; Tobia, I. Impact of COVID-19 Pandemic on Ibero-American Urology Residents: Perspective of American Confederation of Urology (CAU). Int Braz J. Urol. 2020, 46 (Suppl. 1), 165–169. [Google Scholar] [CrossRef]
- Fero, K.E.; Weinberger, J.M.; Lerman, S.; Bergman, J. Perceived impact of urologic surgery training program modifications due to COVID-19 in the United States. Urology 2020, 143, 62–67. [Google Scholar] [CrossRef] [PubMed]
- Campi, R.; Amparore, D.; Checcucci, E.; Claps, F.; Teoh, J.Y.-C.; Serni, S.; et al. Exploring the residents’ perspective on smart learning modalities and contents for virtual urology education: Lesson learned during the COVID-19 pandemic. Actas Urol. Esp. (Engl. Ed.) 2021, 45, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, B.L.; Cabral, J.; Mendes, G.; Madenelo, M.; Rocha, M.A.; Mesquita, S.; et al. How the COVID-19 pandemic changed urology residency - a nationwide survey from the Portuguese resident’s perspective. Cent. European J. Urol. 2021, 74, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Yee, C.H.; Wong, H.F.; Tam, M.H.M.; Yuen, S.K.K.; Chan, H.C.; Cheung, M.H.; et al. Effect of SARS and COVID-19 outbreaks on urology practice and training. Hong Kong Med. J. 2021, 27, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Rajwa, P.; Przydacz, M.; Zapala, P. How has the COVID-19 pandemic impacted Polish urologists? Results from a national survey. Cent. Eur. J. Urol. 2020, 73, 252–259. [Google Scholar] [CrossRef]
- Degraeve, A.; Lejeune, S.; Muilwijk, T.; Poalaert, F.; Piraprez, M.; Svistakov, I.; et al. When residents work less, they feel better: Lessons learned from an unprecedent context of lockdown. Prog. Urol. 2020, 30, 1060–1066. [Google Scholar] [CrossRef] [PubMed]
- Pang, K.H.; Carrion, D.M.; Rivas, J.G.; Mantica, G.; Mattigk, A.; Pradere, B.; On behalf of The European Society of Residents in Urology; et al. The Impact of COVID-19 on European Health Care and Urology Trainees. Eur. Urol. 2020, 78, 6–8. [Google Scholar] [CrossRef]
- Puliatti, S.; Eissa, A.; Eissa, R.; Amato, M.; Mazzone, E.; Dell’Oglio, P.; et al. COVID-19 and urology: A comprehensive review of the literature. BJU Int. 2020, 125, E7–E14. [Google Scholar] [CrossRef] [PubMed]
- Porpiglia, F.; Checcucci, E.; Amparore, D.; Verri, P.; Campi, R.; Claps, F.; et al. Slowdown of urology residents’ learning curve during the COVID-19 emergency. BJU Int. 2020, 125, E15–E17. [Google Scholar] [CrossRef] [PubMed]
- Amparore, D.; Campi, R.; Checcucci, E.; Sessa, F.; Pecoraro, A.; Minervini, A.; et al. Forecasting the future of urology practice: A comprehensive review of the recommendations by international and European associations on priority procedures during the COVID-19 pandemic. Eur. Urol. Focus 2020, 6, 1032–1048. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.Q.; Lu, J.; Chiong, E. Re: Kristian D. Stensland, Todd M. Morgan, Alireza Moinzadeh; et al. Considerations in the Triage of Urologic Surgeries During the COVID-19 Pandemic. Eur. Urol. 2020, 77, 663–666: The Forgotten Urological Patient During the COVID-19 Pandemic: Patient Safety Safeguards. Eur. Urol. 2020, 78, e135–e136. [Google Scholar] [PubMed]
- Westerman, M.E.; Tabakin, A.L.; Sexton, W.J.; Chapin, B.F.; Singer, E.A. Impact of COVID-19 on resident and fellow education: Current guidance and future opportunities for urologic oncology training programs. Urol. Oncol. 2021, 39, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.; Grüllich, C.; Erb, H.H. Re: Ribal MJ, Cornford P, Briganti A, Knoll T, Gravas S, Babjuk M; et al. European Association of Urology Guidelines Office Rapid Reaction Group: An organisation-wide collaborative effort to adapt the European Association of Urology guidelines recommendations to the coronavirus disease 2019 Era. Eur. Urol. Focus 2020, 78, 21–28. https://doi.org/10.1016/j.eururo.2020.04.056: Metastatic prostate cancer and COVID-19: Do current data allow modification of established treatment recommendations? Eur. Urol. Focus 2020, 6, 1135–1136. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.; Kaulfuss, J.; Grange, P. Re: Karl H. Pang, Diego M. Carrion, Juan Gomez Rivas; et al. The Impact of COVID-19 on European Health Care and Urology Trainees. Eur. Urol. 2020, 78, 6–8. Eur. Urol. 2020, 78, e236. [Google Scholar] [CrossRef] [PubMed]
- Esperto, F.; Prata, F.; Civitella, A.; Pang, K.H.; Marchioni, M.; Tuzzolo, P.; et al. Implementation and strategies to ensure adequate coordination within a Urology Department during the COVID-19 pandemic. Int. Braz. J. Urol. 2020, 46 (Suppl. 1), 170–180. [Google Scholar] [CrossRef] [PubMed]
- Diokno, A.C.; Devries, J.M. The impact of COVID-19 on urologic practice, medical education, and training. Int. Urol. Nephrol. 2020, 52, 1195–1198. [Google Scholar] [CrossRef] [PubMed]
- Esperto, F.; Papalia, R.; Pang, K.H.; Cataldo, R.; Scarpa, R.M. What is the role of residents during a pandemic? Minerva Urol. Nefrol. 2020, 72, 387–388. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.Q.; Wang, Z.; Tiong, H.Y.; Chiong, E. The good, the bad, and the ugly of the COVID-19 pandemic in a urology residency program in Singapore. Urology 2020, 142, 244–245. [Google Scholar] [CrossRef] [PubMed]
- Smigelski, M.; Movassaghi, M.; Small, A. Urology virtual education programs during the COVID-19 pandemic. Curr. Urol. Rep. 2020, 21, 50. [Google Scholar] [CrossRef] [PubMed]
- Claps, F.; Amparore, D.; Esperto, F.; Cacciamani, G.; Fiori, C.; Minervini, A.; et al. Smart learning for urology residents during the COVID-19 pandemic and beyond: Insights from a nationwide survey in Italy. Minerva Urol. Nefrol. 2020, 72, 647–649. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.S.; Tabakin, A.L.; Patel, H.V.; Backstrand, J.R.; Jang, T.L.; Kim, I.Y.; et al. Adapting urology residency training in the COVID-19 era. Urology 2020, 141, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Papalia, R.; Cataldo, R.; Alloni, R.; Pang, K.H.; Alcini, A.; Flammia, G.; et al. Urologic surgery in a safe hospital during the COVID-19 pandemic scenario. Minerva Urol. Nefrol. 2021, 73, 384–391. [Google Scholar] [CrossRef]
- Tabakin, A.; Patel, H.V.; Singer, E.A. Lessons learned from the COVID-19 pandemic: A call for a national video-based curriculum for urology residents. J. Surg. Educ. 2021, 78, 324–326. [Google Scholar] [CrossRef] [PubMed]
- Tzelves, L.; Glykas, I.; Lazarou, L.; Zabaftis, C.; Fragkoulis, C.; Leventi, A.; et al. Urology residency training in Greece. Results from the first national resident survey. Actas Urol. Esp. 2021, 45, 537–544. [Google Scholar] [CrossRef] [PubMed]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2022 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.