Abstract
Background/Objectives: Penile fractures are a rare urological emergency, defined as the traumatic rupture of the tunica albuginea. They are classically diagnosed on clinical grounds, requiring urgent operative repair, most commonly by penile degloving. Magnetic resonance imaging (MRI) has emerged as a promising tool in the management of penile fractures. Often recommended in the setting of equivocal clinical diagnoses, MRI can help diagnose, as well as localise, the site of injury. Furthermore, it also holds potential in differentiating penile fractures from mimicking conditions, thereby possibly preventing unnecessary surgical procedures. This study is aimed at evaluating the diagnostic accuracy of MRI for penile fractures. Furthermore, it seeks to explore MRI’s effectiveness in guiding the surgical approach through precise localisation of the injury site. Methods: The PubMed, Embase, and Cochrane databases were searched from January 1995 to December 2022. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed, and a total of 246 cases from 32 studies were identified. Results: Pooled results for MRI use in penile fracture diagnosis resulted in a positive predictive value of 97.8%, a negative predictive value of 87.0%, a sensitivity of 98.6%, and a specificity of 80%. MRI can accurately guide localised incisions, due to its ability to accurately identify the exact site of injury, with no additional reported complications or conversions to degloving. Considerable heterogeneity was observed within MRI parameters and protocols used in the studies identified. Conclusions: This review suggests that MRI is an accurate imaging modality for penile fractures and should be considered as a first-line investigation for equivocal cases. Its application may refine clinical management by avoiding unnecessary surgeries in cases mimicking penile fractures and improve pre-operative planning through precise injury localisation. This study is limited by heterogeneity in MRI protocols and the small sample sizes and retrospective nature of many included studies. The future standardisation of MRI protocols could enhance its utility and reliability in the clinical setting. Additionally, further research is needed to evaluate the long-term outcomes following the repair of small fractures detected on MRI and following MRI-guided localised incisions during surgical repair. Level of Evidence: 2.
1. Introduction
Penile fractures are rare urological emergencies, defined as the traumatic rupture of the tunica albuginea. During erections, the tunica albuginea thins from 2 mm to 0.25–0.5 mm, increasing its susceptibility to injury [1]. Consequently, penile fractures are typically sustained in the setting of sexual activities including intercourse, masturbation, and intentional penile manipulation. A classic history of a cracking or popping sound is followed by the onset of pain, ecchymosis, swelling, and rapid detumescence. Examination commonly reveals an ‘eggplant deformity’ and penile curvature, or a palpable tunica defect may also be observed [2]. The management of penile fractures prioritises emergent surgical repair to minimise risks of long-term complications including erectile dysfunction, plaques, curvature, chronic pain, and infected haematomas [3]. However, clinical misdiagnosis rates have been reported to be as high as 15% [4,5].
In cases where the diagnosis of penile fractures is equivocal, current guidelines suggest the use of radiological investigations. In recent times, magnetic resonance imaging (MRI) has increasingly been employed for the diagnosis of common penile pathologies due to its superior soft tissue contrast, spatial resolution, large field of view, and multiplanar capabilities [6,7]. Relatively higher costs of MRI compared to other imaging modalities and poor availability in some institutions may limit its widespread use. The European Association of Urology (EAU) guidelines regard MRI to be superior to ultrasonography (USS) for penile fractures, although it does not prioritise its use over other imaging modalities [8]. Comparatively, the American Urological Association (AUA) and British Association of Urological Surgeons (BAUS) guidelines suggest the use of ultrasound (USS) imaging as an initial investigation. However, these guidelines lack clear directives on MRI’s specific use cases or its clinical and surgical implications, and they do not address the variability in MRI protocols [8,9,10]. The benefits of ultrasonography include its availability, low cost, and favourable safety profile. While USS is accessible, cost-effective, and generally safe, its efficacy may be compromised by decreased accuracy in detecting small tunica albuginea tears obscured by thrombi, discomfort during image acquisition, and limited experience of the radiographer [11,12,13].
Research on the application of MRI in the context of penile fractures is limited. A greater understanding of MRI accuracy in penile fractures is important, as it may significantly influence both diagnosis and management. MRI’s ability to exclude penile fracture and accurately diagnose benign injuries, such as dorsal vein and dartos bleeding, can lead to the safe conservative management of these penile injuries. Additionally, when surgical intervention is required, MRI insights may be able to guide operative management and inform the choice of surgical incisions [2,14]. The aim of this review is to consolidate current evidence on the accuracy of MRI for penile fractures and establish a clearer understanding of its potential applications in clinical practice.
2. Materials and Methods
2.1. Search Strategy
This systematic review was conducted with the intent to analyse the utility of MRI in the diagnosis and management of penile fractures, with the possibility of a meta-analysis if the data were sufficient. Due to the limited evidence scope, the focus was primarily on conducting a comprehensive systematic review. Our literature search encompassed databases including PubMed, Embase, and the Cochrane Central Register of Controlled Trials (CENTRAL), without restrictions on language. The time frame for the publications was set from January 1995 to December 2022, with the search terms (“penis fracture” OR “penile fracture”) AND (“magnetic resonance imaging” OR “MRI”). This review adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.
2.2. Study Selection
Titles and abstracts from the search results were initially screened by three independent reviewers (H.W., S.A., and J. Saad) to select full-text articles for detailed examination. Inclusion criteria required that the selected articles be written in English, detail the utilisation of MRI in the diagnostic work-up of penile fractures in a pre-operative setting, and include surgical exploration and operative findings. Studies not meeting these criteria were excluded. Eligible articles underwent full-text review, and where full texts were not available, abstracts were considered if they provided sufficient data for analysis. A manual search of references within selected articles and the related literature was also conducted to identify additional studies. Disagreements regarding study inclusion were resolved through consultation with a fourth reviewer (A.D.).
2.3. Data Extraction, Screening, and Appraisal
Data extraction was carried out by two reviewers (H.W. and S.A.) using a standardised form to capture study characteristics and outcomes. Extracted data included MRI protocols and sequences, characteristics of the injury (such as the location, size, and presence of concomitant urethral injury), and details of the surgical intervention (incision used, confirmation or exclusion of diagnosis, and injury description). The heterogeneity observed in reported MRI parameters and protocols was critically assessed and synthesised by a radiologist among the authors (J. Spencer).
A quality assessment of the included studies was conducted using the Newcastle–Ottawa Scale (NOS) for non-randomised studies [15]. Case reports and small series with fewer than five patients were excluded due to inherent bias and the absence of a suitable bias assessment tool for such studies. To facilitate an objective evaluation of the quality of each included study, the NOS criteria were applied through a star system. Specifically, studies were assigned a quality rating on a scale: a rating of 7 stars was interpreted as “very good” quality, indicating a high level of evidence and a low risk of bias; a rating of 5 to 6 stars was deemed “good”, suggesting moderate evidence quality with some concerns regarding bias; a rating of 3 to 4 stars was categorised as “satisfactory”, reflecting a fair level of evidence with notable bias limitations; and a rating of 2 stars or fewer was considered “unsatisfactory”, indicative of poor evidence quality with a high risk of bias.
2.4. Data Analysis
Data analysis was conducted by one reviewer (H.W.) to assess the diagnostic accuracy of MRI for penile fractures. Basic statistical analyses included the calculation of positive predictive value (PPV), negative predictive value (NPV), sensitivity, and specificity, using the true-positive (TP), true-negative (TN), false-positive (FP), and false-negative (FN) rates identified in the included studies.
3. Results
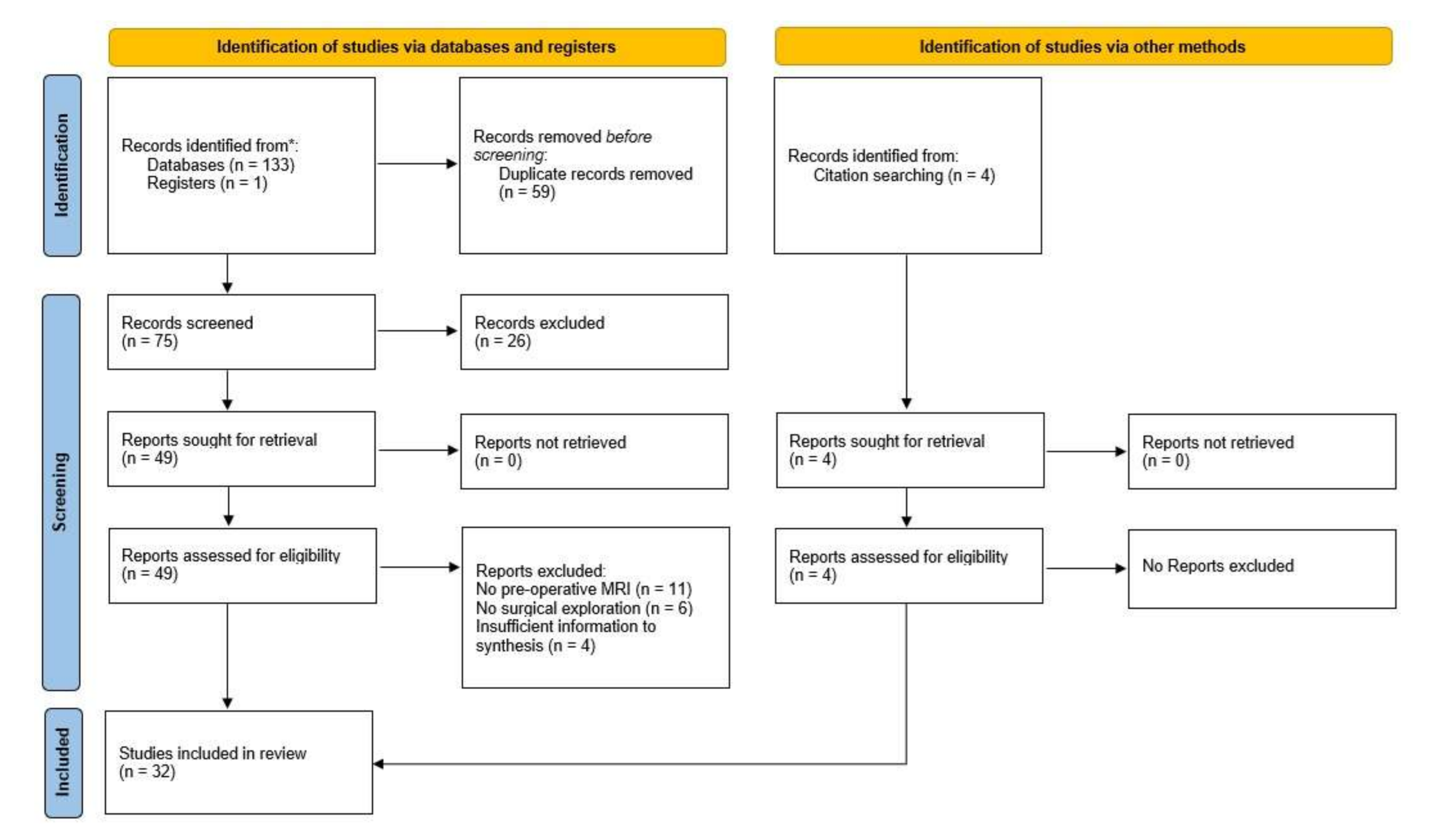
Following the defined search criteria, a total of 134 articles were initially identified. Subsequently, 59 duplicates were removed. The remaining records underwent screening based on title and abstract, resulting in the exclusion of 26 studies due to various factors such as non-English language, irrelevance of article type (e.g., reviews, editorials), and unrelated pathology. Full-text articles were retrieved for 49 studies, of which 21 were further excluded due to reasons including the absence of pre-operative MRI, lack of surgical exploration, and insufficient data for appropriate synthesis relevant to this study. Finally, 4 additional reports identified through citation review led to the inclusion of 32 studies [11,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46] in the final analysis. The screening process, including the number of studies included and excluded as well as the reasons for all exclusions, is summarised in Figure 1.
Figure 1.
PRISMA flowchart summarising the screening process for article inclusion in this systematic review. * PubMed, Embase, and Cochrane CENTRAL.
In our review, MRI use for penile fractures has been described as part of injury diagnosis, considerations for management, and pre-operative planning. Study findings including MRI parameters and protocols, MRI findings, surgical approach, surgical findings, and comparisons with ultrasonography are summarised in Tables S1 and S2 reports the pooled analysis of outcomes for MRI use in penile fractures.
In the assessment of the studies in this review, a “good” quality evaluation was consistently achieved based on the Newcastle–Ottawa Scale (NOS) criteria. The main limitation identified across these studies was the lack of a non-exposed comparison group and the absence of control for confounding variables. Detailed findings from the risk of bias evaluations, according to the NOS criteria applied, are presented in Table S3 in the Supplementary Materials.
4. Discussion
Imaging modalities considered useful in the diagnosis of penile fractures include cavernosography, ultrasound, and magnetic resonance imaging [3]. However, there are numerous benefits of MRI over alternative imaging modalities. MRI can establish penile anatomy in three orthogonal planes with excellent soft tissue contrast and is not limited by radiographer experience or pain associated with image acquisition. It is non-invasive, avoids complications that can occur with cavernosography, and does not require the routine use of contrast, mitigating risks of allergic reactions and nephropathy. Additionally, image quality is not degraded by haematomas overlying tunica defects [1,11,12,13]
Ageing blood is known to have an evolving appearance on MRI [16]. However, whether the appearance of cavernosal blood evolves in the same fashion as blood elsewhere, or whether this affects the ability to identify penile fractures on MRI, has not been reported. Thus, whether the utility of MRI is reduced in delayed presentations of penile fracture is not established. Furthermore, whether inter-reporter variability in the diagnosis of penile fractures exists has not been explored.
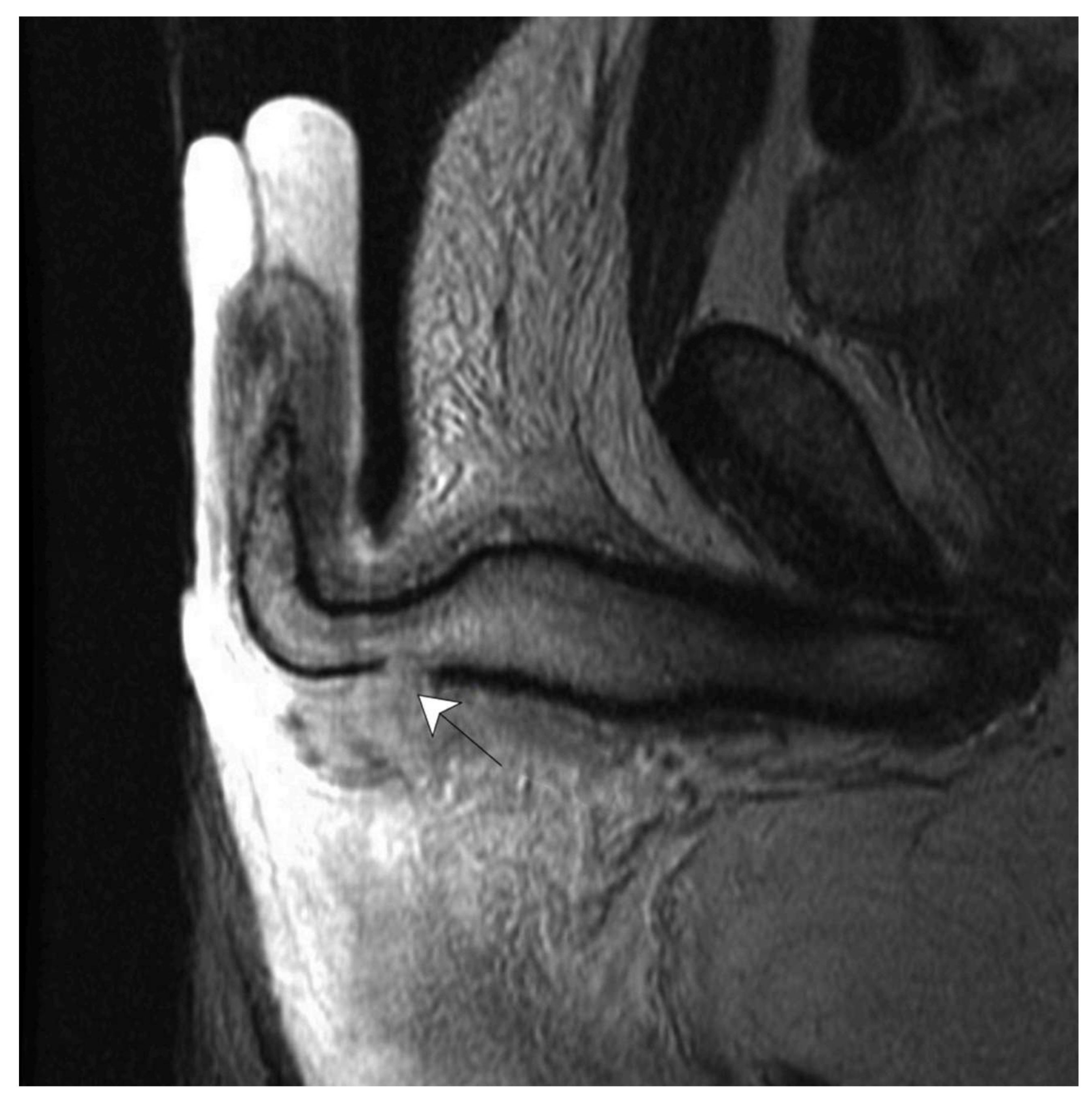
Hallmark MRI findings of penile fractures include the interruption of the low-signal tunica albuginea, evident on both T1- (T1WI) and T2-weighted imaging (T2WI) [6,47,48] [Figure 2]. When contrast is used, early focal enhancement is seen at the site of the tunica tear, with the improved delineation of acute haematomas, which are often isointense to the corpora on unenhanced sequences [6,49]. The diagnosis of penile fracture mimics such as penile contusions centres on findings including focal areas of hypointensity on a background of T2 bright corpus cavernosum and the continuity of the tunica albuginea [27,47].
Figure 2.
Penile fracture demonstrated on T2 sagittal plane. White arrow indicates the tunica albuginea defect [22].
4.1. MRI Parameters and Protocols
MRI parameters including magnet strength (Tesla), the use of coil, patient positioning, the use of contrast, and sequences were variable across the studies included in this review. The most common magnet strength used was 1.5 T, accounting for 142 out of 166 (86%) MRIs across 10 studies [11,19,24,28,30,35,37,42,43,49]. The remaining MRIs were performed with 3 T magnets in 20 patients [46], 1 T in 1 patient [11], and sub-1 T in 2 patients [34,50].
Surface coils, which maximise the signal-to-noise ratio and improve image resolution, were consistently used. For penile imaging, surface coils are generally considered favourable and should be positioned over the lower abdominopelvic wall and scrotum [6,13,50]. In this review, the use of surface coils was reported in all 13 studies that reported on this parameter [19,24,26,28,30,34,35,38,43,45,47,49,51].
Appropriate positioning is considered essential to accurate penile imaging. In all 10 studies where penile positioning was discussed, the penis was elevated, erect, or placed in the “anatomical position”, dorsiflexed against the abdominal wall, and secured in position [11,19,22,30,34,43,45,47,49,51].
The importance of slice thickness has not previously been explored within the setting of penile fractures. Penile fracture injury sizes can be as small as a focal or sub-millimetre defect, and tunica albuginea thickness typically measures 2 mm [1]. In this review, MRI slice thickness ranged from 2 mm to 6 mm for 46 patients across six studies [19,28,34,38,43,52]. All 37 penile fractures were correctly diagnosed irrespective of slice thickness dimensions. However, in a nine-patient cohort without a penile fracture on surgical exploration, Sokolakis et al. observed that 1.5 T MRI with 3 mm slices resulted in two patients being misdiagnosed with false-positive injuries [43].
Contrast was variably used in this study, with nine studies reporting either a regular or as-needed use of contrast [11,24,28,30,35,40,44,45,51], compared to six studies without contrast [18,25,42,43,46,48]. Three studies reported potential improvements in the demonstration of tunica tearing and surrounding haematoma with the use of contrast [11,30,43]. However, in a subgroup analysis of non-contrast- and contrast-enhanced MRI, Spiesecke et al. found no diagnostic benefit following contrast medium administration [44].
T1WI and T2WI are sequences utilised during MRI to generate images, and they are distinguished primarily by their tissue contrast mechanisms. T1WI provides a high spatial resolution and superior anatomical detail, allowing for differentiation between tissues with varying fat and water contents. Comparatively, T2WI excels in highlighting differences in water content among tissues, making it particularly useful in identifying pathologies such as oedema and inflammation. In almost all studies, T1WI and T2WI were performed together [11,19,22,26,27,28,30,34,35,39,43,44,45,47,49,51,52], with a single report of T1 imaging alone [37]. Most commonly, T2WI was performed in all three orthogonal planes with additional T1WI in only one or two planes. In two studies, T1WI was considered more sensitive or demonstrated penile fractures better than T2WI [11,29], attributed to the masking of haemorrhage by low signal intensity on T2WI. Uder et al. reported that for three out of four patients, T2WI alone missed the tunica tear, which was evident on T1WI, and under-appreciated the size of the tear in the remaining case [11].
While there is no established consensus on MRI protocols for penile fractures, we suggest the use of 1.5 T (or greater) MRI with a surface coil, slice thickness of ideally 3 mm or less, and the penis oriented in the anatomical position, without the routine use of contrast. Protocols should include the use of T2WI in multiple planes and additional T1W1 in one or two planes. A similar protocol recommended by Esposito et al. reported an image acquisition time of 20 min [47]. Further research is required to determine the significance of thinner slices and contrast enhancement.
4.2. MRI Accuracy
From the 32 included studies, there were a total of 246 cases of penile fractures who underwent pre-operative MRI, with 218 true-positive, 5 false-positive, 20 true-negative, and 3 false-negative cases. Pooled results include a positive predictive value of 97.8%, negative predictive value of 87.0%, sensitivity of 98.6%, and specificity of 80.0% (Table S2). MRI can accurately diagnose penile fractures as well as exclude cases of penile fracture mimics. Additionally, it can accurately map the location of injuries; however, may it underestimate the size of an injury.
Mehjardi et al. assessed the accuracy of MRI in determining the location of penile fractures. MRI was used to map the side, dorsal–ventral relation, and proximity (base, proximal, mid-shaft, and distal) of an injury, which was correlated to surgical findings following degloving [49]. The correct site was identified by MRI for 73/75 outcomes, with both incorrect outcomes being inaccurate by one order of proximity. MRI accuracy in determining the size of a tunica albuginea defect was assessed by Panella et al. in 15 patients who underwent degloving. Though penile fracture was correctly diagnosed in all 15 patients, MRI underestimated the size of injury in 9/15 (60%) patients by 5 mm or greater [35].
4.3. Use of MRI to Guide Surgical Intervention
While subcoronal degloving represents the most common incision performed for penile fracture repair in this review, 54 patients across 12 studies underwent alternative incisions including penoscrotal, perineal, ventral, lateral, and longitudinal incisions [2,11,17,18,26,27,28,38,39,40,46]. No reports of complications, secondary incisions, or conversion to subcoronal degloving were observed. The use of localised incisions for the operative repair of penile fractures was associated with improved long-term functional outcomes, including a lower mean time to sexual function, compared to patients who underwent degloving [51]. Additionally, localised incisions avoid complications unique to degloving and circumcision, including decreased penile sensation and sensitivity and decreased sexual pleasure, including lower orgasm intensity [47].
The use of MRI may change the definitive operative paradigm for penile fractures, with the potential consideration of severity and size-based decision making. Panella et al. [33] performed conservative, non-operative management in a cohort of five patients with MRI findings that demonstrated sub-5 mm injuries. On long-term follow-up, normal erectile function, as determined by the International Index of Erectile Function (IIEF-5), was observed in all five patients.
A systematic review by Wong et al. evaluated the outcomes of early surgical intervention (within 24 h of injury) versus delayed intervention in cases of penile fractures, focusing on erectile dysfunction and tunica scar formation. The study found no statistically significant differences in these outcomes between the two approaches. Early intervention did, however, slightly improve penile curvature, though the improvements were generally mild, did not impact sexual functioning, and were thus considered clinically insignificant [53]. However, Bozzini et al.’s retrospective study subsequently highlighted an association between an increased time to intervention, greater than 8.23 h from admission, and worsened erectile function [21]. Given these findings, the time taken for individual institutions to obtain MRI needs to be factored into the management of penile fractures. Nonetheless, it is important to weigh the potential advantages of using MRI, such as the avoidance of unnecessary surgeries, potentially shorter operative times, and the facilitation of precise, localised incisions, against these findings.
4.4. MRI Accuracy Compared to USS
Both MRI and USS were performed in the pre-operative setting for 60 patients across nine studies [18,26,27,29,37,42,47,50,53]. AUA and BAUS guidelines suggest the consideration of ultrasound in patients with equivocal signs and symptoms of penile fracture [9,10]. While the benefits of USS include its availability, cost profile, and safety, several diagnostic shortfalls may occur in the setting of penile fractures, including the failure to identify small tunica tears obscured by a thrombus or haematoma. Poor tolerance secondary to pain has been reported to limit image quality [11,35], and ultrasonographer experience may be lacking due to disease rarity [12,13]. When compared, MRI outperformed USS across almost all studies in this review, except for a single case where a penile fracture was identified on USS but considered inconclusive on MRI [18].
Mehjardi et al. used USS for the pre-operative mapping of penile fractures. Compared to MRI, which accurately mapped 73/75 injury location parameters, USS only correctly mapped 61/75 (81%). In the same study, USS identified 22/25 penile fractures (88%), compared to 25/25 (100%) for MRI [47]. The three fractures identified on MRI but not on USS were located at the base of the penis and could not be imaged sonographically. Alcaraz et al. reported that in 13/17 (76.5%) patients, MRI upgraded equivocal cases on USS to a diagnosis of penile fracture or demonstrated a greater extent of injury [19]. Similarly, twelve patients underwent both USS and MRI in a study by Spiesecke et al. While both imaging modalities correctly excluded seven cases negative for penile fractures, USS failed to identify three of five penile fractures seen on MRI [42].
MRI outperforms USS in penile fracture diagnosis and the mapping of injury sites. Where available, MRI should be considered the first-line investigation for equivocal cases. Additionally, the use of MRI appears capable of accurately mapping the exact site of injury, which may help facilitate localised incisions for repair.
4.5. Study Limitations
Limitations of this review include study heterogeneity and the retrospective nature of many studies, often with small sample sizes. Additionally, a degree of selection bias is introduced, as not all penile fractures would have been scanned; therefore, our statistics only apply to patients who were reviewed by a urologist or had an MRI scan performed.
The requirement for surgical confirmation to validate MRI findings also introduces a bias towards cases with positive MRI results, potentially overlooking false negatives. Variability was also seen in the reporting of MRI protocols.
Further research is needed to assess the long-term effects of imaging acquisition delays, investigate conservative treatment outcomes for minor MRI-detected fractures, explore surgical results in patients with negative MRI scans, and evaluate how MRI-guided localisation affects surgical strategies and outcomes.
5. Conclusions
MRI holds the potential to significantly change the management paradigm of penile fractures. It demonstrates high diagnostic accuracy, coupled with excellent soft tissue resolution that facilitates precise diagnosis and injury localisation. This can help guide management, particularly in equivocal cases, where it may prevent unnecessary surgeries. Additionally, accurate injury mapping can assist in surgical planning, including the use of localised incisions. This review advocates the use of MRI, when available, as a first-line radiological investigation, particularly in cases of diagnostic uncertainty.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/siuj6020029/s1: Table S1: Summary of studies utilising MRI for the diagnosis and management of penile fractures; Table S2: Summary of pooled outcomes for MRI use in penile fractures; Table S3: Quality of included studies using Newcastle–Ottawa Quality Assessment Scale.
Author Contributions
Conceptualisation, H.W., A.C., and A.D.; Methodology, H.W. and S.A.; Validation, A.C., A.D., and S.N.; Formal Analysis, A.C., A.D., and J.S. (Jeremy Saad); Data Curation, H.W., S.A., and A.C.; Writing—Original Draft Preparation, H.W.; Writing—Review and Editing, S.A., A.D., S.N., and J.S. (Jarrah Spencer); Supervision, A.D. All authors have read and agreed to the published version of the manuscript.
Funding
There was no funding for this study.
Institutional Review Board Statement
MRI images were obtained from a retrospective audit conducted with low-risk ethics approval from the author’s local health district ethics board.
Informed Consent Statement
Not applicable.
Data Availability Statement
Study materials may be considered for sharing upon reasonable request to the corresponding author.
Acknowledgments
The authors would like to thank Daniel Chia for his assistance and input in this review.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
References
- Jack, G.S.; Garraway, I.; Reznichek, R.; Rajfer, J. Current treatment options for penile fractures. Rev. Urol. 2004, 6, 114–120. [Google Scholar]
- Falcone, M.; Garaffa, G.; Castiglione, F.; Ralph, D.J. Current Management of Penile Fracture: An Up-to-Date Systematic Review. Sex. Med. Rev. 2018, 6, 253–260. [Google Scholar] [CrossRef]
- Amer, T.; Wilson, R.; Chlosta, P.; AlBuheissi, S.; Qazi, H.; Fraser, M.; Aboumarzouk, O.M. Penile Fracture: A Meta-Analysis. Urol. Int. 2016, 96, 315–329. [Google Scholar] [CrossRef] [PubMed]
- Beysel, M.; Tekin, A.; Gürdal, M.; Gürdal, M.; Sengör, F. Evaluation and treatment of penile fractures: Accuracy of clinical diagnosis and the value of corpus cavernosography. Urology 2002, 60, 492–496. [Google Scholar] [CrossRef] [PubMed]
- Karadeniz, T.; Topsakal, M.; Ariman, A.; Erton, H.; Basak, D. Penile fracture: Differential diagnosis, management and outcome. Br. J. Urol. 1996, 77, 279–281. [Google Scholar] [CrossRef] [PubMed]
- Abualruz, A.-R.; O’Malley, R.; Ponnatapura, J.; Holbert, B.L.; Whitworth, P.; Tappouni, R.; Lalwani, N. MRI of common penile pathologies and penile prostheses. Abdom. Radiol. 2020, 45, 2825–2839. [Google Scholar] [CrossRef] [PubMed]
- Parker, R.A.; Menias, C.O.; Quazi, R.; Hara, A.K.; Verma, S.; Shaaban, A.; Siegel, C.L.; Radmanesh, A.; Sandrasegaran, K. MR Imaging of the Penis and Scrotum. RadioGraphics 2015, 35, 1033–1050. [Google Scholar] [CrossRef] [PubMed]
- Serafetinidis, E.; Campos-Juanatey, F.; Hallscheidt, P.; Mahmud, H.; Mayer, E.; Schouten, N.; Sharma, D.M.; Waterloos, M.; Zimmermann, K.; Kitrey, N.D. Summary Paper of the Updated 2023 European Association of Urology Guidelines on Urological Trauma. Eur. Urol. Focus 2023, 10, 475–485. [Google Scholar] [CrossRef]
- Morey, A.F.; Broghammer, J.A.; Hollowell, C.M.P.; McKibben, M.J.; Souter, L. Urotrauma Guideline 2020: AUA Guideline. J. Urol. 2021, 205, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Rees, R.W.; Brown, G.; Dorkin, T.; Lucky, M.; Pearcy, R.; Shabbir, M.; Shukla, C.J.; Summerton, D.J.; Munner, A.; BAUS Section of Andrology and Genitourethral Surgery. British Association of Urological Surgeons (BAUS) consensus document for the management of male genital emergencies–penile fracture. BJU Int. 2018, 122, 26–28. [Google Scholar] [CrossRef]
- Uder, M.; Gohl, D.; Takahashi, M.; Derouet, H.; Defreyne, L.; Kramann, B.; Schneider, G. MRI of penile fracture: Diagnosis and therapeutic follow-up. Eur. Radiol. 2002, 12, 113–120. [Google Scholar] [CrossRef]
- Kati, B.; Akin, Y.; Demir, M.; Derouet, H.; Defreyne, L.; Kramann, B.; Schneider, G. Penile fracture and investigation of early surgical repair effects on erectile dysfunction. Urologia 2019, 86, 207–210. [Google Scholar] [CrossRef] [PubMed]
- Lindquist, C.M.; Nikolaidis, P.; Mittal, P.K.; Miller, F.H. MRI of the penis. Abdom. Radiol. 2020, 45, 2001–2017. [Google Scholar] [CrossRef] [PubMed]
- Feki, W.; Derouiche, A.; Belhaj, K.; Ouni, A.; Mouelhi, S.B.; Ben Slama, M.R.; Ayed, M.; Chebil, M. False penile fracture: Report of 16 cases. Int. J. Impot. Res. 2007, 19, 471–473. [Google Scholar] [CrossRef] [PubMed]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef]
- Swensen, S.; Keller, P.; Berquist, T.; McLeod, R.; Stephens, D. Magnetic resonance imaging of hemorrhage. Am. J. Roentgenol. 1985, 145, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Abolyosr, A.; Moneim, A.E.A.; Abdelatif, A.M.; Abdalla, M.A.; Imam, H.M.K. The management of penile fracture based on clinical and magnetic resonance imaging findings. BJU Int. 2005, 96, 373–377. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, M.M.; Singh, S.K.; Sharma, D.K.; Ranjan, P.; Kumar, S.; Chandramohan, V.; Gupta, N.; Acharya, N.C.; Bhalla, V.; Mavuduru, R.; et al. Fracture of the penis: A radiological or clinical diagnosis? A case series and literature review. Can. J. Urol. 2009, 16, 4568–4575. [Google Scholar]
- Alcaraz, A.C.; Von Stempel, C.; Ralph, D.; Lee, W.G.D. MP22-06 Ultrasonography and magnetic resonance imaging are accurate for suspected penile fracture. J. Urol. 2021, 206 (Suppl. S3), e392–e393. [Google Scholar] [CrossRef]
- Bhoopathy, S.V.; Kim, L.H. The value of pre-operative MRI in management of penile fractures. Urol. Case Rep. 2020, 31, 101185. [Google Scholar] [CrossRef]
- Bozzini, G.; Albersen, M.; Otero, J.R.; Margreiter, M.; Cruz, E.G.; Mueller, A.; Gratzke, C.; Serefoglu, E.C.; Salamanca, J.I.M.; Verze, P.; et al. Delaying Surgical Treatment of Penile Fracture Results in Poor Functional Outcomes: Results from a Large Retrospective Multicenter European Study. Eur. Urol. Focus 2018, 4, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Chaljub, G.; Ernst, R.; Rodriquez, G.; Callas, J.; Sandler, C.M. Emergent MRI utilizing a 5-inch surface coil to evaluate for acute penile fracture. Emerg. Radiol. 2002, 9, 35–37. [Google Scholar] [CrossRef] [PubMed]
- Choi, M.H.; Kim, B.; Ryu, J.A.; Lee, S.W.; Lee, K.S. MR imaging of acute penile fracture. Radiographics 2000, 20, 1397–1405. [Google Scholar] [CrossRef]
- De Lucchi, R.; Rizzo, L.; Rubino, A.; Tola, E. Magnetic resonance diagnosis of traumatic penile fracture. Radiol. Med. 2004, 107, 234–240. [Google Scholar] [PubMed]
- El-Assmy, A.; El-Tholoth, H.S.; Abou-El-Ghar, M.E.; Mohsen, T.; Ibrahiem, E.H.I. False penile fracture: Value of different diagnostic approaches and long-term outcome of conservative and surgical management. Urology 2010, 75, 1353–1356. [Google Scholar] [CrossRef]
- Fedel, M.; Venz, S.; Andreessen, R.; Loening, S.A. The value of magnetic resonance imaging in the diagnosis of suspected penile fracture with atypical clinical findings. J. Urol. 1996, 155, 1924–1927. [Google Scholar] [CrossRef] [PubMed]
- Gochenaur, L.; Osinski, T.; Wanderling, C.; Quarrier, S.O. A case report of a proximal corporal cavernosa injury presenting with butterfly perineal ecchymosis. Urol. Case Rep. 2022, 40, 101870. [Google Scholar] [CrossRef]
- Guler, I.; Ödev, K.; Kalkan, H.; Simsek, C.; Keskin, S.; Kilinç, M. The value of magnetic resonance imaging in the diagnosis of penile fracture. Int. Braz. J. Urol. 2015, 41, 325–328. [Google Scholar] [CrossRef] [PubMed]
- Harada, J.; Shida, Y.; Gono, S.; Masato, M.; Yuno, T.; Hakariya, T.; Kihara, T.; Maeda, K.; Miyata, Y.; Sakai, H. Rare case of penile fracture caused by an injury to the crus penis: Delayed repair using the transperineal approach. IJU Case Rep. 2021, 4, 36–38. [Google Scholar] [CrossRef]
- Jethwani, D.; Ooi, C.C.; Nair, T.; Omar, S. Increase the index of suspicion-atypical presentations of penile fractures. Int. J. Urol. 2019, 26 (Suppl. S2), 125. [Google Scholar] [CrossRef]
- Koifman, L.; Barros, R.; Júnior, R.A.; Cavalcanti, A.G.; Favorito, L.A. Penile fracture: Diagnosis, treatment and outcomes of 150 patients. Urology 2010, 76, 1488–1492. [Google Scholar] [CrossRef] [PubMed]
- Maubon, A.J.; Roux, J.O.; Faix, A.; Segui, B.; Ferru, J.M.; Rounet, J.P. Penile fracture: MRI demonstration of a urethral tear associated with a rupture of the corpus cavernosum. Eur. Radiol. 1998, 8, 469–470. [Google Scholar] [CrossRef] [PubMed]
- Panella, P.; Pepe, P.; Pennisi, M. Diagnosis and treatment of penile injury: Ten years experience of an emergency department. Arch. Ital. Urol. Androl. 2020, 92, 192–195. [Google Scholar] [CrossRef] [PubMed]
- Phillips, E.A.; Esposito, A.J.; Munarriz, R. Acute penile trauma and associated morbidity: 9-year experience at a tertiary care center. Andrology 2015, 3, 632–636. [Google Scholar] [CrossRef]
- Rahiman, M.; Manasa, T.; Koteshwara, D. Magnetic Resonance Imaging: An accurate diagnostic tool in the precise localization of penile fracture. Arch. Med. Health Sci. 2013, 1, 54. [Google Scholar] [CrossRef]
- Rahmouni, A.; Hoznek, A.; Duron, A.; Colombel, M.; Chopin, D.K.; Mathieu, D.; Vasile, N. Magnetic resonance imaging of penile rupture: Aid to diagnosis. J. Urol. 1995, 153, 1927–1928. [Google Scholar] [CrossRef] [PubMed]
- Rao, A.; Surendrababu, N.R. Snap sound and detumescence: Fracture penis. J. Postgrad. Med. 2007, 53, 255–256. [Google Scholar] [CrossRef] [PubMed]
- Rezaee, M.M.; Gross, M. The pelvic pop: An extremely rare case of internal penile fracture presenting with scrotal hematoma and review of the literature. Asian J. Androl. 2021, 23, 116–117. [Google Scholar] [CrossRef] [PubMed]
- Rosi, G.; Fontanella, P.; Venzi, G.; Jermini, F.; Grande, F.D. 3T MR-guided minimally-invasive penile fracture repair. Arch. Ital. Di Urol. E Androl. 2016, 88, 68–69. [Google Scholar] [CrossRef]
- Saglam, E.; Tarhan, F.; Hamarat, M.B.; Can, U.; Coskun, A.; Camur, E. Efficacy of magnetic resonance imaging for diagnosis of penile fracture: A controlled study. Investig. Clin. Urol. 2017, 58, 255–260. [Google Scholar] [CrossRef]
- Sokolakis, I.; Schubert, T.; Oelschlaeger, M.; Krebs, M.; Gschwend, J.E.; Holzapfel, K.; Kübler, H.; Gakis, G.; Hatzichristodoulou, G. The role of magnetic resonance imaging in the diagnosis of penile fracture in real-life emergency settings: Comparative analysis with intraoperative findings. J. Urol. 2019, 202, 552–557. [Google Scholar] [CrossRef]
- Spiesecke, P.; Mang, J.; Fischer, T.; Hamm, B.; Lerchbaumer, M.H. Diagnostic performance of MRI and US in suspicion of penile fracture. Transl. Androl. Urol. 2022, 11, 377–385. [Google Scholar] [CrossRef] [PubMed]
- Swain, F.R.; Udeschi, M.; Armm, M.F.; Gagliardi, J.A. Fracture of the Penis: Demonstration by MRI with Surgical Correlation. Radiol. Case Rep. 2007, 2, 75. [Google Scholar]
- Tamhankar, A.S.; Pawar, P.W.; Sawant, A.S.; Kasat, G.V.; Savaliya, A.; Mundhe, S.; Patil, S.; Narwade, S. Fractured Penis: Not So Rare! Urol. Int. 2017, 99, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Turkay, R.; Yenice, M.G.; Aksoy, S.; Şeker, G.; Şahin, S.; İnci, E.; Tuğcu, V.; Taşcı, A.I. Contribution of MRI to clinically equivocal penile fracture cases. Turk. J. Trauma. Emerg. Surg. TJTES 2016, 22, 549–552. [Google Scholar] [CrossRef] [PubMed]
- Williams, J.M.; Anderson, J.B.; Laborde, E.L. Penile Fracture Caused by Straddle Injury to a Nonerect Penis. Urology 2020, 142, e47–e48. [Google Scholar] [CrossRef]
- Esposito, A.A.; Giannitto, C.; Muzzupappa, C.; Maccagnoni, S.; Gadda, F.; Albo, G.; Biondetti, P.R. MRI of penile fracture: What should be a tailored protocol in emergency? Radiol. Med. 2016, 121, 711–718. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.X.; Zhou, Z.; Yao, H.J.; Zhang, K.; Da, J.; Zhang, M.; Wang, Z.; Lu, M.J. Comparison of different approaches to the surgical treatment of penile fractures: Quicker return to sexual function with longitudinal incisions. Int. J. Impot. Res. 2016, 28, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Zare Mehrjardi, M.; Darabi, M.; Bagheri, S.M.; Kamali, K.; Bijan, B. The role of ultrasound (US) and magnetic resonance imaging (MRI) in penile fracture mapping for modified surgical repair. Int. Urol. Nephrol. 2017, 49, 937–945. [Google Scholar] [CrossRef] [PubMed]
- Kirkham, A. MRI of the penis. Br. J. Radiol. 2012, 85, S86–S93. [Google Scholar] [CrossRef] [PubMed]
- Master, M. T1 vs T2 MRI. Available online: https://mrimaster.com/t1-vs-t2-mri/ (accessed on 5 March 2024).
- Bronselaer, G.A.; Schober, J.M.; Meyer-Bahlburg, H.F.L.; T’Sjoen, G.; Vlietinck, R.; Hoebeke, P.B. Male circumcision decreases penile sensitivity as measured in a large cohort. BJU Int. 2013, 111, 820–827. [Google Scholar] [CrossRef] [PubMed]
- Wong, N.C.; Dason, S.; Bansal, R.K.; Davies, T.O.; Braga, L.H. Can it wait? A systematic review of immediate vs. delayed surgical repair of penile fractures. Can. Urol. Assoc. J. 2017, 11, 53–60. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Société Internationale d’Urologie. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).