Lean-ing Method in an Emergency Department of the Italian Epicenter of the COVID-19 Outbreak: When the Algorithm Makes Difference
Abstract
:1. Introduction
2. Materials and Methods
2.1. Humanitas Clinical and Research Hospital Emergency Department
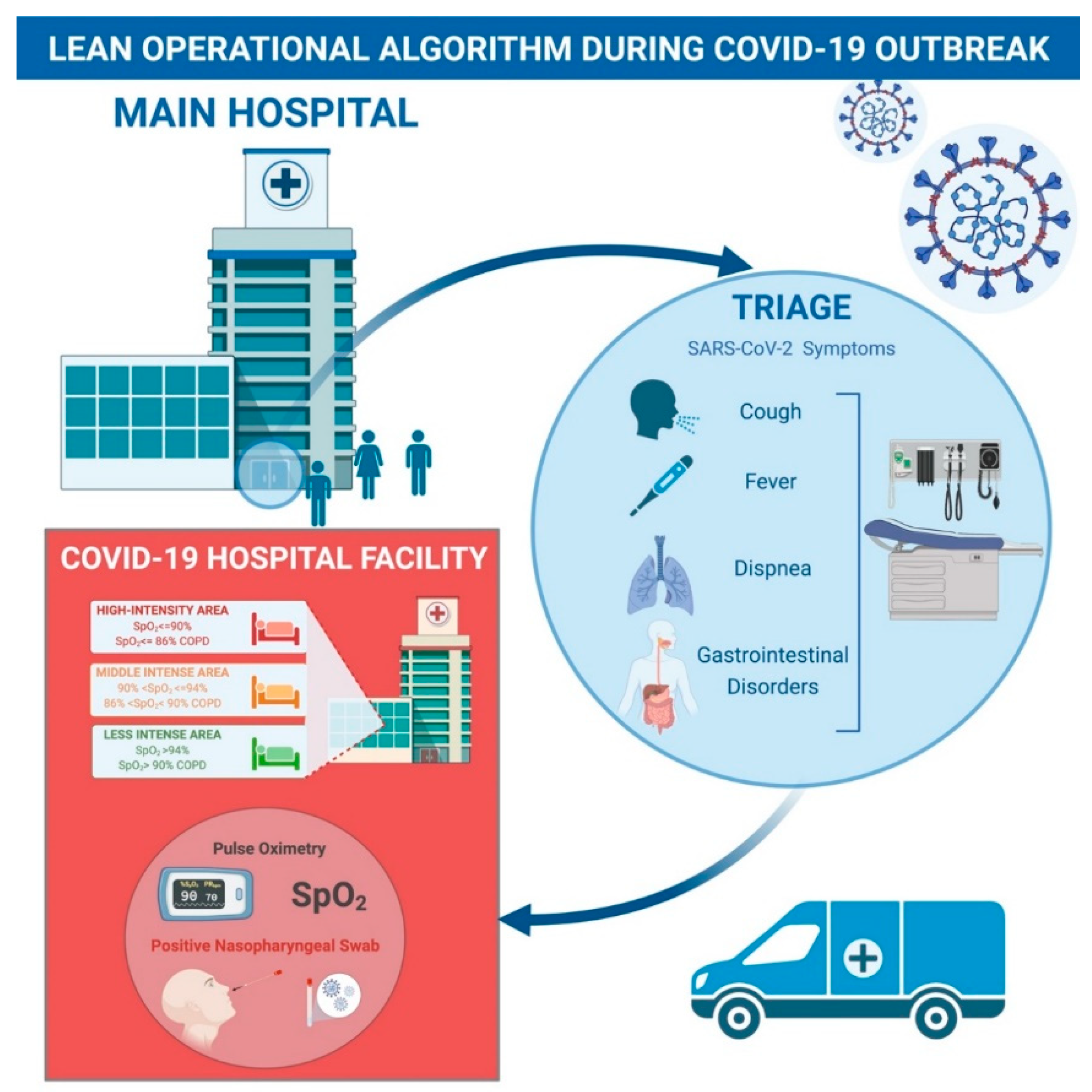
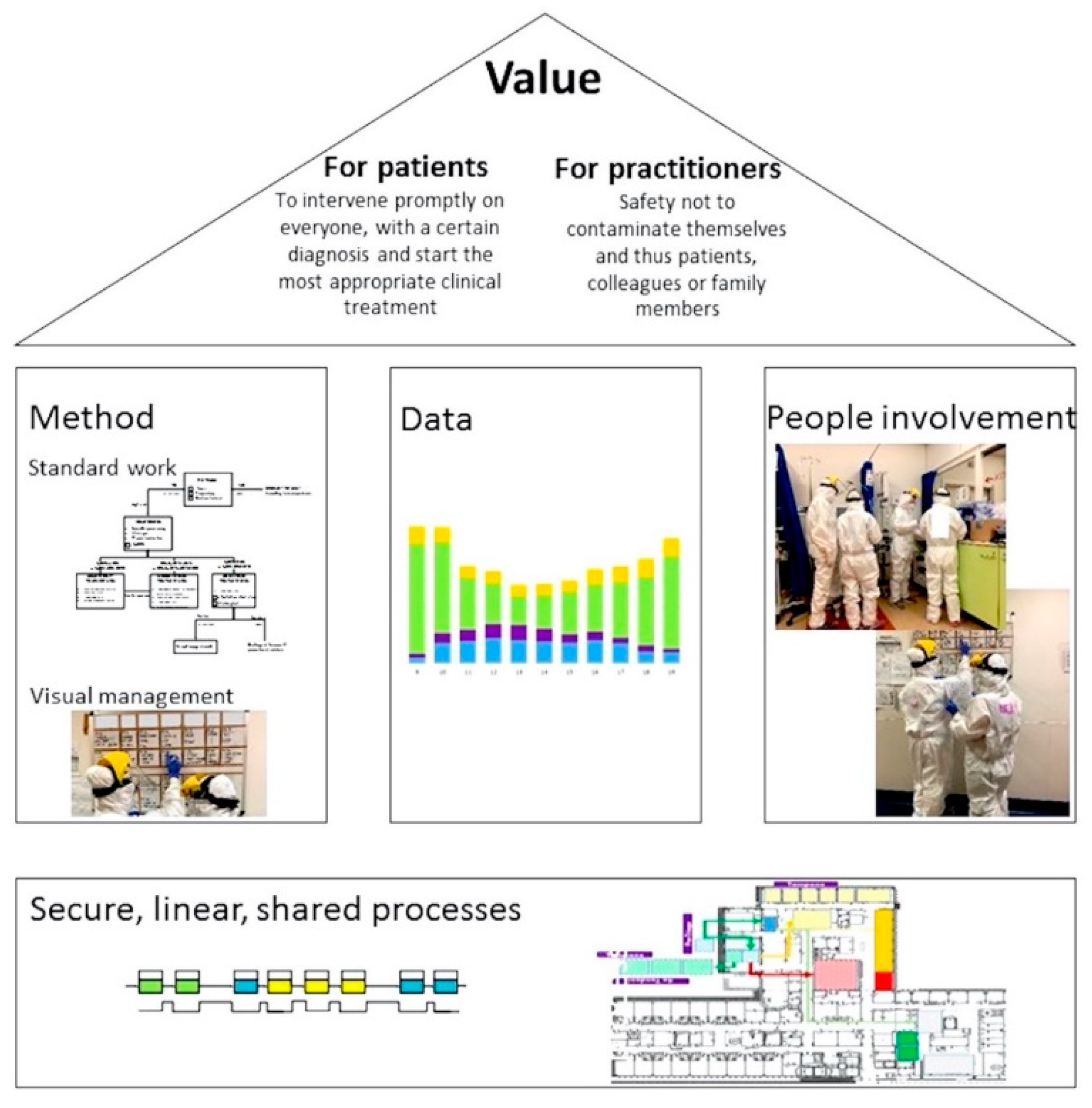
2.2. The Lean Operational Algorithm
3. System Operational Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- D’Andreamatteo, A.; Ianni, L.; Lega, F.; Sargiacomo, M. Lean in healthcare: A comprehensive review. Health Policy 2015, 119, 1197–1209. [Google Scholar] [CrossRef]
- Souza, D.L.; Korzenowski, A.L.; Alvarado, M.M.; Sperafico, J.H.; Ackermann, A.E.F.; Mareth, T.; Scavarda, A.J. A systematic review on lean applications’ in emergency departments. Healthcare 2021, 9, 763. [Google Scholar] [CrossRef]
- Chen, T.; Ma, X.; Zhou, S.; Wang, H.; Pan, Y.; Chen, L.; Lv, H.; Lu, Y. Establishing a standardized FUO emergency department: Design and practice in dealing with COVID-19. Ann. Transl. Med. 2020, 8, 749. [Google Scholar] [CrossRef]
- Patey, C.; Asghari, S.; Norman, P.; Hurley, O. Redesign of a rural emergency department to prepare for the COVID-19 pandemic. CMAJ 2020, 192, E518–E520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cecconi, M.; Piovani, D.; Brunetta, E.; Aghemo, A.; Greco, M.; Ciccarelli, M.; Angelini, C.; Voza, A.; Omodei, P.; Vespa, E.; et al. Early predictors of clinical deterioration in a cohort of 239 patients hospitalized for COVID-19 infection in Lombardy, Italy. J. Clin. Med. 2020, 9, 1548. [Google Scholar] [CrossRef] [PubMed]
- Hanft, K. Lean Hospitals: Improving Quality, Patient Safety, and Employee Engagement, 2nd ed.; Productivity Press: Seattle, WA, USA, 2013; Volume 7, pp. 124–125. [Google Scholar]
- Rotter, T.; Plishka, C.; Lawal, A.; Harrison, L.; Sari, N.; Goodridge, D.; Flynn, R.; Chan, J.; Fiander, M.; Poksinska, B.; et al. What is lean management in health care? Development of an operational definition for a cochrane systematic review. Eval. Health Prof. 2019, 42, 366–390. [Google Scholar] [CrossRef] [PubMed]
- Parkhi, S.S. Lean management practices in healthcare sector: A literature review. Benchmarking Int. J. 2019, 26, 1275–1289. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef]
- V’Kovski, P.; Kratzel, A.; Steiner, S.; Stalder, H.; Thiel, V. Coronavirus biology and replication: Implications for SARS-CoV-2. Nat. Rev. Microbiol. 2021, 19, 155–170. [Google Scholar] [CrossRef]
- Kirtipal, N.; Bharadwaj, S.; Kang, S.G. From SARS to SARS-CoV-2, insights on structure, pathogenicity and immunity aspects of pandemic human coronaviruses. Infect. Genet. Evol. 2020, 85, 104502. [Google Scholar] [CrossRef]
- Livingston, E.; Bucher, K. Coronavirus disease 2019 (COVID-19) in Italy. JAMA 2020, 323, 1335. [Google Scholar] [CrossRef] [Green Version]
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef] [PubMed]
- WHO. Clinical Management of COVID-19. Available online: https://www.who.int/publications/i/item/clinical-management-of-covid-19 (accessed on 28 January 2021).
- World Health Organization. Clinical Management of Severe Acute Respiratory Infection (SARI) when COVID-19 Disease Is Suspected: Interim Guidance, 13 March 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Percudani, M.; Corradin, M.; Moreno, M.; Indelicato, A.; Vita, A. Mental health services in lombardy during COVID-19 outbreak. Psychiatry Res. 2020, 288, 112980. [Google Scholar] [CrossRef] [PubMed]
- Odone, A.; Delmonte, D.; Scognamiglio, T.; Signorelli, C. COVID-19 deaths in Lombardy, Italy: Data in context. Lancet Public Health 2020, 5, e310. [Google Scholar] [CrossRef]
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA 2020, 323, 1574–1581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masetti, C.; Generali, E.; Colapietro, F.; Voza, A.; Cecconi, M.; Messina, A.; Omodei, P.; Angelini, C.; Ciccarelli, M.; Badalamenti, S.; et al. High mortality in COVID-19 patients with mild respiratory disease. Eur. J. Clin. Investig. 2020, 50, e13314. [Google Scholar] [CrossRef]
- Zaim, S.; Chong, J.H.; Sankaranarayanan, V.; Harky, A. COVID-19 and multiorgan response. Curr. Probl. Cardiol. 2020, 45, 100618. [Google Scholar] [CrossRef]
- Noris, M.; Benigni, A.; Remuzzi, G. The case of complement activation in COVID-19 multiorgan impact. Kidney Int. 2020, 98, 314–322. [Google Scholar] [CrossRef]
- Mokhtari, T.; Hassani, F.; Ghaffari, N.; Ebrahimi, B.; Yarahmadi, A.; Hassanzadeh, G. COVID-19 and multiorgan failure: A narrative review on potential mechanisms. J. Mol. Histol. 2020, 51, 613–628. [Google Scholar] [CrossRef]
- Bader, F.; Manla, Y.; Atallah, B.; Starling, R.C. Heart failure and COVID-19. Heart Fail. Rev. 2021, 26, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Babapoor-Farrokhran, S.; Gill, D.; Walker, J.; Rasekhi, R.T.; Bozorgnia, B.; Amanullah, A. Myocardial injury and COVID-19: Possible mechanisms. Life Sci. 2020, 253, 117723. [Google Scholar] [CrossRef]
- Ronco, C.; Reis, T.; Husain-Syed, F. Management of acute kidney injury in patients with COVID-19. Lancet Respir. Med. 2020, 8, 738–742. [Google Scholar] [CrossRef]
- Jafari-Oori, M.; Fiorentino, M.; Castellano, G.; Ebadi, A.; Rahimi-Bashar, F.; Guest, P.C.; Vahedian-Azimi, A.; Sahebkar, A. Acute kidney injury and COVID-19: A scoping review and meta-analysis. Adv. Exp. Med. Biol. 2021, 1321, 309–324. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.C.; Huo, T.I.; Huang, Y.H. Gastrointestinal and liver manifestations in patients with COVID-19. J. Chin. Med. Assoc. 2020, 83, 521–523. [Google Scholar] [CrossRef]
- Jothimani, D.; Venugopal, R.; Abedin, M.F.; Kaliamoorthy, I.; Rela, M. COVID-19 and the liver. J. Hepatol. 2020, 73, 1231–1240. [Google Scholar] [CrossRef]
- Baig, A.M. Neurological manifestations in COVID-19 caused by SARS-CoV-2. CNS Neurosci. Ther. 2020, 26, 499–501. [Google Scholar] [CrossRef] [Green Version]
- Whittaker, A.; Anson, M.; Harky, A. Neurological manifestations of COVID-19: A systematic review and current update. Acta Neurol. Scand. 2020, 142, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Aghemo, A.; Piovani, D.; Parigi, T.L.; Brunetta, E.; Pugliese, N.; Vespa, E.; Omodei, P.D.; Preatoni, P.; Lleo, A.; Repici, A.; et al. COVID-19 digestive system involvement and clinical outcomes in a large academic hospital in Milan, Italy. Clin. Gastroenterol. Hepatol. 2020, 18, 2366–2368.e2363. [Google Scholar] [CrossRef]
- Ferrante, G.; Fazzari, F.; Cozzi, O.; Maurina, M.; Bragato, R.; D’Orazio, F.; Torrisi, C.; Lanza, E.; Indolfi, E.; Donghi, V.; et al. Risk factors for myocardial injury and death in patients with COVID-19: Insights from a cohort study with chest computed tomography. Cardiovasc. Res. 2020, 116, 2239–2246. [Google Scholar] [CrossRef]
- Cocco, A.; Amami, P.; Desai, A.; Voza, A.; Ferreli, F.; Albanese, A. Neurological features in SARS-CoV-2-infected patients with smell and taste disorder. J. Neurol. 2021, 268, 1570–1572. [Google Scholar] [CrossRef]
- Desai, A.; Voza, G.; Paiardi, S.; Teofilo, F.I.; Caltagirone, G.; Pons, M.R.; Aloise, M.; Kogan, M.; Tommasini, T.; Savevski, V.; et al. The role of anti-hypertensive treatment, comorbidities and early introduction of LMWH in the setting of COVID-19: A retrospective, observational study in Northern Italy. Int. J. Cardiol. 2021, 324, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Luzzi, S.; Giotta Lucifero, A.; Marasco, S.; Del Maestro, M.; Bellantoni, G.; Gragnaniello, C. Targeting of renin-angiotensin system in COVID-19 patients affected by stroke: Emerging concerns about detrimental vs. benefit effect. Interdiscip. Neurosurg. 2020, 22, 100822. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.; Caltagirone, G.; Sari, S.; Pocaterra, D.; Kogan, M.; Azzolini, E.; Savevski, V.; Martinelli-Boneschi, F.; Voza, A. The Use of Antiviral Agents against SARS-CoV-2: Ineffective or Time and Age Dependent Result? A Retrospective, Observational Study among COVID-19 Older Adults. J. Clin. Med. 2021, 10, 686. [Google Scholar] [CrossRef]
- Desai, A.; Santonocito, O.G.; Caltagirone, G.; Kogan, M.; Ghetti, F.; Donadoni, I.; Porro, F.; Savevski, V.; Poretti, D.; Ciccarelli, M.; et al. Effectiveness of streptococcus pneumoniae urinary antigen testing in decreasing mortality of COVID-19 co-infected patients: A clinical investigation. Medicina 2020, 56, 572. [Google Scholar] [CrossRef]
- Manivel, V.; Lesnewski, A.; Shamim, S.; Carbonatto, G.; Govindan, T. CLUE: COVID-19 lung ultrasound in emergency department. Emerg. Med. Australas 2020, 32, 694–696. [Google Scholar] [CrossRef] [PubMed]
- Kilaru, A.S.; Lee, K.; Snider, C.K.; Meisel, Z.F.; Asch, D.A.; Mitra, N.; Delgado, M.K. Return hospital admissions among 1419 COVID-19 patients discharged from five U.S. emergency departments. Acad. Emerg. Med. 2020, 27, 1039–1042. [Google Scholar] [CrossRef] [PubMed]
- Gok, A.F.K.; Eryılmaz, M.; Ozmen, M.M.; Alimoglu, O.; Ertekin, C.; Kurtoglu, M.H. Recommendations for trauma and emergency general surgery practice during COVID-19 pandemic. Ulus. Travma Acil Cerrahi Derg. 2020, 26, 335–342. [Google Scholar] [CrossRef]
- De Freitas, L.; Goodacre, S.; O’Hara, R.; Thokala, P.; Hariharan, S. Interventions to improve patient flow in emergency departments: An umbrella review. Emerg. Med. J. 2018, 35, 626–637. [Google Scholar] [CrossRef] [PubMed]
- Mieiro, D.B.; Oliveira, É.B.; Fonseca, R.E.; Mininel, V.A.; Zem-Mascarenhas, S.H.; Machado, R.C. Strategies to minimize medication errors in emergency units: An integrative review. Rev. Bras. Enferm. 2019, 72, 307–314. [Google Scholar] [CrossRef] [Green Version]
- Giamberardino, M.A.; Affaitati, G.; Costantini, R.; Guglielmetti, M.; Martelletti, P. Acute headache management in emergency department. A narrative review. Intern. Emerg. Med. 2020, 15, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Cardona, M.; Lewis, E.T.; Turner, R.M.; Alkhouri, H.; Asha, S.; Mackenzie, J.; Perkins, M.; Suri, S.; Holdgate, A.; Winoto, L.; et al. Efficacy of a tool to predict short-term mortality in older people presenting at emergency departments: Protocol for a multi-centre cohort study. Arch. Gerontol. Geriatr. 2018, 76, 169–174. [Google Scholar] [CrossRef] [Green Version]
- Savioli, G.; Ceresa, I.F.; Luzzi, S.; Gragnaniello, C.; Giotta Lucifero, A.; Del Maestro, M.; Marasco, S.; Manzoni, F.; Ciceri, L.; Gelfi, E.; et al. Rates of intracranial hemorrhage in mild head trauma patients presenting to emergency department and their management: A comparison of direct oral anticoagulant drugs with vitamin k antagonists. Medicina 2020, 56, 308. [Google Scholar] [CrossRef] [PubMed]
- Savioli, G.; Ceresa, I.F.; Ciceri, L.; Sciutti, F.; Belliato, M.; Iotti, G.A.; Luzzi, S.; Del Maestro, M.; Mezzini, G.; Lafe, E.; et al. Mild head trauma in elderly patients: Experience of an emergency department. Heliyon 2020, 6, e04226. [Google Scholar] [CrossRef] [PubMed]
- Savioli, G.; Ceresa, I.F.; Macedonio, S.; Gerosa, S.; Belliato, M.; Iotti, G.A.; Luzzi, S.; Del Maestro, M.; Mezzini, G.; Giotta Lucifero, A.; et al. Trauma coagulopathy and its outcomes. Medicina 2020, 56, 205. [Google Scholar] [CrossRef] [Green Version]
- Khanna, S.; Sier, D.; Boyle, J.; Zeitz, K. Discharge timeliness and its impact on hospital crowding and emergency department flow performance. Emerg. Med. Australas 2016, 28, 164–170. [Google Scholar] [CrossRef]
- Costa, L.B.; Filho, M.G.; Rentes, A.F.; Bertani, T.M.; Mardegan, R. Lean healthcare in developing countries: Evidence from Brazilian hospitals. Int. J. Health Plann. Manag. 2017, 32, e99–e120. [Google Scholar] [CrossRef]
- Mohammadian, M.; Babaei, M.; Amin Jarrahi, M.; Anjomrouz, E. Scheduling nurse shifts using goal programming based on nurse preferences: A case study in an emergency department. Int. J. Eng. 2019, 32, 954–963. [Google Scholar] [CrossRef] [Green Version]
- Pitts, S.R.; Niska, R.W.; Xu, J.; Burt, C.W. National hospital ambulatory medical care survey: 2006 emergency department summary. In National Health Statistics Reports; U.S. Department of Health & Human Services: Washington, WA, USA, 2008; pp. 1–38. [Google Scholar]
- Klein, D.; Khan, V. Utilizing six sigma lean strategies to expedite emergency department CT scan throughput in a tertiary care facility. J. Am. Coll. Radiol. 2017, 14, 78–81. [Google Scholar] [CrossRef] [Green Version]
- Khlie, K.; Abouabdellah, A. Identification of the patient requirements using lean six sigma and data mining. Int. J. Eng. 2017, 30, 691–699. [Google Scholar]
- Sánchez, M.; Suárez, M.; Asenjo, M.; Bragulat, E. Improvement of emergency department patient flow using lean thinking. Int. J. Qual. Health Care 2018, 30, 250–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dickson, E.W.; Singh, S.; Cheung, D.S.; Wyatt, C.C.; Nugent, A.S. Application of lean manufacturing techniques in the Emergency Department. J. Emerg. Med. 2009, 37, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Holden, R.J. Lean Thinking in emergency departments: A critical review. Ann. Emerg. Med. 2011, 57, 265–278. [Google Scholar] [CrossRef] [PubMed]
- Improta, G.; Romano, M.; Di Cicco, M.V.; Ferraro, A.; Borrelli, A.; Verdoliva, C.; Triassi, M.; Cesarelli, M. Lean thinking to improve emergency department throughput at AORN Cardarelli hospital. BMC Health Serv. Res. 2018, 18, 914. [Google Scholar] [CrossRef] [PubMed]
- Aminjarahi, M.; Abdoli, M.; Fadaee, Y.; Kohan, F.; Shokouhyar, S. The prioritization of lean techniques in Emergency Departments using VIKOR and SAW approaches. Ethiop. J. Health Sci. 2021, 31, 283–292. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Desai, A.; Goretti, G.; Giordano, M.; Voza, A. Lean-ing Method in an Emergency Department of the Italian Epicenter of the COVID-19 Outbreak: When the Algorithm Makes Difference. Appl. Syst. Innov. 2021, 4, 55. https://doi.org/10.3390/asi4030055
Desai A, Goretti G, Giordano M, Voza A. Lean-ing Method in an Emergency Department of the Italian Epicenter of the COVID-19 Outbreak: When the Algorithm Makes Difference. Applied System Innovation. 2021; 4(3):55. https://doi.org/10.3390/asi4030055
Chicago/Turabian StyleDesai, Antonio, Giulia Goretti, Mauro Giordano, and Antonio Voza. 2021. "Lean-ing Method in an Emergency Department of the Italian Epicenter of the COVID-19 Outbreak: When the Algorithm Makes Difference" Applied System Innovation 4, no. 3: 55. https://doi.org/10.3390/asi4030055
APA StyleDesai, A., Goretti, G., Giordano, M., & Voza, A. (2021). Lean-ing Method in an Emergency Department of the Italian Epicenter of the COVID-19 Outbreak: When the Algorithm Makes Difference. Applied System Innovation, 4(3), 55. https://doi.org/10.3390/asi4030055






