Endoscopic Salvage of Gastrointestinal Anastomosis Leaks—Past, Present, and Future—A Narrated Review
Abstract
:1. Introduction
2. Results
2.1. History of Endoscopic Sealing
The Cuffed Stent
2.2. Current Technology
2.2.1. Tissue Adhesives
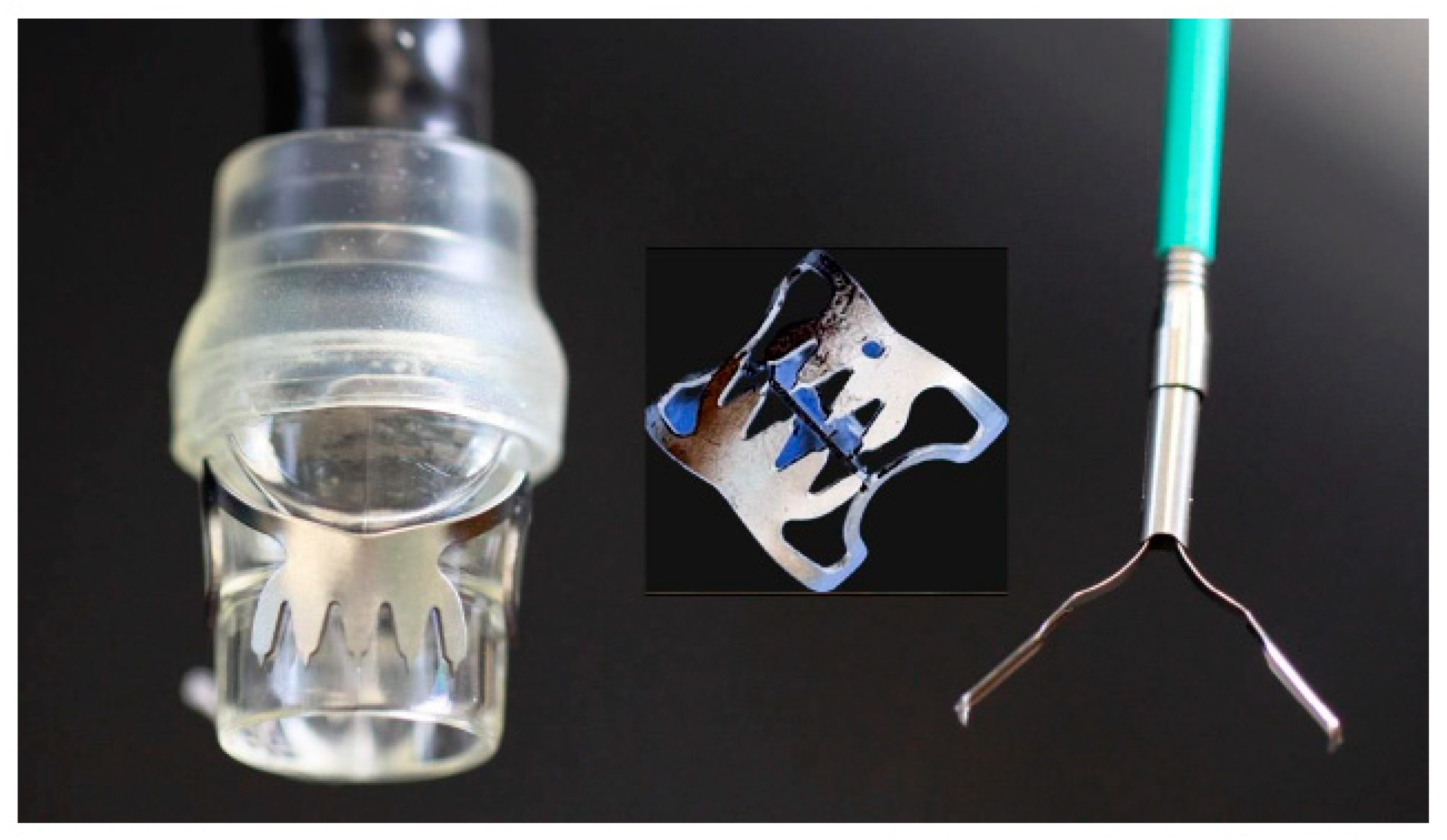
2.2.2. Endoclips and Over-the-Scope Clips
2.2.3. Stents
2.2.4. Endoscopic Vacuum Therapy (EVT)
2.2.5. Endoscopic Internal Drainage (EID)
2.2.6. Vac-Stent Technique
2.2.7. The Suturing System
2.3. The Possible Future
2.3.1. Stem Cells
2.3.2. Modification of Luminal Microbiome
3. Materials and Methods
4. Discussion
4.1. Tissue Adhesives
4.2. Through-the-Scope (TTSC) and Over-the-Scope Clips (OTSC)
4.3. Stents
4.4. Endoscopic Vacuum Therapy (EVT)
4.5. Endoscopic Internal Drainage—EID
4.6. Vac-Stent Technique
4.7. Endoluminal Suturing
4.8. Stem Cells
4.9. Modification of Lumenal Microbiome
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kähler, G. Anastomotic Leakage after Upper Gastrointestinal Surgery: Endoscopic Treatment. Visc. Med. 2017, 33, 202–206. [Google Scholar] [CrossRef]
- Munshi, E.; Dahlbäck, C.; Johansson, S.; Lydrup, M.L.; Jutesten, H.; Buchwald, P. Long-term Outcomes of Endoscopic Vacuum Therapy and Transanal Drainage for Anastomotic Leakage After Anterior Resection. Vivo 2022, 36, 2275–2278. [Google Scholar] [CrossRef]
- Cereatti, F.; Grassia, R.; Drago, A.; Conti, C.B.; Donatelli, G. Endoscopic management of gastrointestinal leaks and fistulae: What option do we have? World J. Gastroenterol. 2020, 26, 4198–4217. [Google Scholar] [CrossRef]
- Rutegård, M.; Lagergren, P.; Rouvelas, I.; Lagergren, J. Intrathoracic anastomotic leakage and mortality after esophageal cancer resection: A population-based study. Ann. Surg. Oncol. 2012, 19, 99–103. [Google Scholar] [CrossRef]
- Lang, H.; Piso, P.; Stukenborg, C.; Raab, R.; Jähne, J. Management and results of proximal anastomotic leaks in a series of 1114 total gastrectomies for gastric carcinoma. Eur. J. Surg. Oncol. 2000, 26, 168–171. [Google Scholar] [CrossRef]
- Messager, M.; Warlaumont, M.; Renaud, F.; Marin, H.; Branche, J.; Piessen, G.; Mariette, C. Recent improvements in the management of esophageal anastomotic leak after surgery for cancer. Eur. J. Surg. Oncol. 2017, 43, 258–269. [Google Scholar] [CrossRef]
- Scognamiglio, P.; Reeh, M.; Melling, N.; Kantowski, M.; Eichelmann, A.-K.; Chon, S.-H.; El-Sourani, N.; Schön, G.; Höller, A.; Izbicki, J.R.; et al. Management of intra-thoracic anastomotic leakages after esophagectomy: Updated systematic review and meta-analysis of endoscopic vacuum therapy versus stenting. BMC Surg. 2022, 22, 309. [Google Scholar] [CrossRef]
- Blencowe, N.S.; Strong, S.; Mcnair, A.G.; Brookes, S.T.; Crosby, T.; Griffin, S.M.; Blazeby, J.M. Reporting of short-term clinical outcomes after esophagectomy: A systematic review. Ann. Surg. 2012, 255, 658–666. [Google Scholar] [CrossRef]
- Kuppusamy, M.K.; Low, D.E. Evaluation of International Contemporary Operative Outcomes and Management Trends Associated With Esophagectomy: A 4-Year Study of >6000 Patients Using ECCG Definitions and the Online Esodata Database. Ann. Surg. 2022, 275, 515–525. [Google Scholar] [CrossRef]
- Aiolfi, A.; Asti, E.; Rausa, E.; Bonavina, G.; Bonitta, G.; Bonavina, L. Use of C-reactive protein for the early prediction of anastomotic leak after esophagectomy: Systematic review and Bayesian meta-analysis. PLoS ONE 2018, 13, e0209272. [Google Scholar] [CrossRef]
- Low, D.E.; Kuppusamy, M.K.; Alderson, D.; Cecconello, I.; Chang, A.C.; Darling, G.; Davies, A.; D’journo, X.B.; Gisbertz, S.S.; Griffin, S.M.; et al. Benchmarking Complications Associated with Esophagectomy. Ann. Surg. 2019, 269, 291–298. [Google Scholar] [CrossRef]
- Watanabe, M.; Miyata, H.; Gotoh, M.; Baba, H.; Kimura, W.; Tomita, N.; Nakagoe, T.; Shimada, M.; Kitagawa, Y.; Sugihara, K.; et al. Total gastrectomy risk model: Data from 20,011 Japanese patients in a nationwide internet-based database. Ann. Surg. 2014, 260, 1034–1039. [Google Scholar] [CrossRef]
- Van Der Werf, L.R.; Busweiler, L.a.D.; Van Sandick, J.W.; Van Berge Henegouwen, M.I.; Wijnhoven, B.P.L. Reporting National Outcomes After Esophagectomy and Gastrectomy According to the Esophageal Complications Consensus Group (ECCG). Ann. Surg. 2020, 271, 1095–1101. [Google Scholar] [CrossRef] [PubMed]
- Vermeer, T.A.; Orsini, R.G.; Daams, F.; Nieuwenhuijzen, G.A.; Rutten, H.J. Anastomotic leakage and presacral abscess formation after locally advanced rectal cancer surgery: Incidence, risk factors and treatment. Eur. J. Surg. Oncol. 2014, 40, 1502–1509. [Google Scholar] [CrossRef] [PubMed]
- Clifford, R.E.; Fowler, H.; Govindarajah, N.; Vimalachandran, D.; Sutton, P.A. Early anastomotic complications in colorectal surgery: A systematic review of techniques for endoscopic salvage. Surg. Endosc. 2019, 33, 1049–1065. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.H.; Huang, X.W.; Song, Y.C.; Lin, H.Z.; Zheng, F.W. Analysis of Prevention and Treatment of Anastomotic Leakage after Sphincter-Preserving Surgery for Middle- and Low-Grade Rectal Cancer under Laparoscopy. Int. J. Clin. Pract. 2022, 2022, 6231880. [Google Scholar] [CrossRef]
- Penna, M.; Hompes, R.; Arnold, S.; Wynn, G.; Austin, R.; Warusavitarne, J.; Moran, B.; Hanna, G.B.; Mortensen, N.J.; Tekkis, P.P. Incidence and Risk Factors for Anastomotic Failure in 1594 Patients Treated by Transanal Total Mesorectal Excision: Results From the International TaTME Registry. Ann. Surg. 2019, 269, 700–711. [Google Scholar] [CrossRef]
- Okoshi, K.; Masano, Y.; Hasegawa, S.; Hida, K.; Kawada, K.; Nomura, A.; Kawamura, J.; Nagayama, S.; Yoshimura, T.; Sakai, Y. Efficacy of transanal drainage for anastomotic leakage after laparoscopic low anterior resection of the rectum. Asian J. Endosc. Surg. 2013, 6, 90–95. [Google Scholar] [CrossRef]
- Yang, L.; Huang, X.E.; Zhou, J.N. Risk assessment on anastomotic leakage after rectal cancer surgery: An analysis of 753 patients. Asian Pac. J. Cancer Prev. 2013, 14, 4447–4453. [Google Scholar] [CrossRef]
- Marshall, J.S.; Srivastava, A.; Gupta, S.K.; Rossi, T.R.; Debord, J.R. Roux-en-Y gastric bypass leak complications. Arch. Surg. 2003, 138, 520–523; discussion 523–524. [Google Scholar] [CrossRef]
- Csendes, A.; Burgos, A.M.; Braghetto, I. Classification and management of leaks after gastric bypass for patients with morbid obesity: A prospective study of 60 patients. Obes. Surg. 2012, 22, 855–862. [Google Scholar] [CrossRef]
- Morales, M.P.; Miedema, B.W.; Scott, J.S.; De La Torre, R.A. Management of postsurgical leaks in the bariatric patient. Gastrointest. Endosc. Clin. N. Am. 2011, 21, 295–304. [Google Scholar] [CrossRef]
- Gonzalez, R.; Sarr, M.G.; Smith, C.D.; Baghai, M.; Kendrick, M.; Szomstein, S.; Rosenthal, R.; Murr, M.M. Diagnosis and contemporary management of anastomotic leaks after gastric bypass for obesity. J. Am. Coll. Surg. 2007, 204, 47–55. [Google Scholar] [CrossRef] [PubMed]
- Abou Rached, A.; Basile, M.; El Masri, H. Gastric leaks post sleeve gastrectomy: Review of its prevention and management. World J. Gastroenterol. 2014, 20, 13904–13910. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, R.J.; Diaz, A.A.; Arvidsson, D.; Baker, R.S.; Basso, N.; Bellanger, D.; Boza, C.; El Mourad, H.; France, M.; Gagner, M.; et al. International Sleeve Gastrectomy Expert Panel Consensus Statement: Best practice guidelines based on experience of >12,000 cases. Surg. Obes. Relat. Dis. 2012, 8, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Bashah, M.; Khidir, N.; El-Matbouly, M. Management of leak after sleeve gastrectomy: Outcomes of 73 cases, treatment algorithm and predictors of resolution. Obes. Surg. 2020, 30, 515–520. [Google Scholar] [CrossRef] [PubMed]
- Mandarino, F.V.; Barchi, A.; Fanti, L.; D’amico, F.; Azzolini, F.; Esposito, D.; Biamonte, P.; Lauri, G.; Danese, S. Endoscopic vacuum therapy for post-esophagectomy anastomotic dehiscence as rescue treatment: A single center case series. Esophagus 2022, 19, 417–425. [Google Scholar] [CrossRef]
- Binda, C.; Jung, C.F.M.; Fabbri, S.; Giuffrida, P.; Sbrancia, M.; Coluccio, C.; Gibiino, G.; Fabbri, C. Endoscopic Management of Postoperative Esophageal and Upper GI Defects-A Narrative Review. Medicina 2023, 59, 136. [Google Scholar] [CrossRef]
- Lux, G.; Wilson, D.; Wilson, J.; Demling, L. A cuffed tube for the treatment of oesophago-bronchial fistulae. Endoscopy 1987, 19, 28–30. [Google Scholar] [CrossRef]
- Irving, J.D.; Simson, J.N. A new cuffed oesophageal prosthesis for the management of malignant oesophago-respiratory fistula. Ann. R. Coll. Surg. Engl. 1988, 70, 13–15. [Google Scholar]
- Hordijk, M.L.; Dees, J.; Van Blankenstein, M. The management of malignant esophago-respiratory fistulas with a cuffed prosthesis. Endoscopy 1990, 22, 241–244. [Google Scholar] [CrossRef]
- Sargeant, I.R.; Thorpe, S.; Bown, S.G. Cuffed esophageal prosthesis: A useful device in desperate situations in esophageal malignancy. Gastrointest. Endosc. 1992, 38, 669–675. [Google Scholar] [CrossRef]
- Kotzampassi, K.; Eleftheriadis, E. Tissue sealants in endoscopic applications for anastomotic leakage during a 25-year period. Surgery 2015, 157, 79–86. [Google Scholar] [CrossRef]
- Shehab, H. Endoscopic management of postsurgical leaks. Int. J. Gastrointest. Interv. 2016, 5, 6–14. [Google Scholar] [CrossRef]
- Hua, F.; Sun, D.; Zhao, X.; Song, X.; Yang, W. Update on therapeutic strategy for esophageal anastomotic leak: A systematic literature review. Thorac. Cancer 2023, 14, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Truong, S.; Böhm, G.; Klinge, U.; Stumpf, M.; Schumpelick, V. Results after endoscopic treatment of postoperative upper gastrointestinal fistulas and leaks using combined Vicryl plug and fibrin glue. Surg. Endosc. 2004, 18, 1105–1108. [Google Scholar] [CrossRef]
- Blumetti, J.; Abcarian, H. Management of low colorectal anastomotic leak: Preserving the anastomosis. World J. Gastrointest. Surg. 2015, 7, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Binmoeller, K.F.; Grimm, H.; Soehendra, N. Endoscopic closure of a perforation using metallic clips after snare excision of a gastric leiomyoma. Gastrointest. Endosc. 1993, 39, 172–174. [Google Scholar] [CrossRef]
- Li, C.; Zhao, Y.; Han, Z.; Zhou, Y. Anastomotic leaks following gastrointestinal surgery: Updates on diagnosis and interventions. Int. J. Clin. Exp. Med. 2016, 9, 7031–7040. [Google Scholar]
- Cho, S.B.; Lee, W.S.; Joo, Y.E.; Kim, H.R.; Park, S.W.; Park, C.H.; Kim, H.S.; Choi, S.K.; Rew, J.S. Therapeutic options for iatrogenic colon perforation: Feasibility of endoscopic clip closure and predictors of the need for early surgery. Surg. Endosc. 2012, 26, 473–479. [Google Scholar] [CrossRef]
- Al Ghossaini, N.; Lucidarme, D.; Bulois, P. Endoscopic treatment of iatrogenic gastrointestinal perforations: An overview. Dig. Liver Dis. 2014, 46, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, S.; Barth, B.A.; Bhat, Y.M.; Desilets, D.J.; Gottlieb, K.T.; Maple, J.T.; Pfau, P.R.; Pleskow, D.K.; Siddiqui, U.D.; Tokar, J.L.; et al. Endoscopic closure devices. Gastrointest. Endosc. 2012, 76, 244–251. [Google Scholar] [CrossRef] [PubMed]
- Goenka, M.K.; Rodge, G.A.; Tiwary, I.K. Endoscopic Management with a Novel Over-The-Scope Padlock Clip System. Clin. Endosc. 2019, 52, 574–580. [Google Scholar] [CrossRef]
- Von Renteln, D.; Denzer, U.W.; Schachschal, G.; Anders, M.; Groth, S.; Rösch, T. Endoscopic closure of GI fistulae by using an over-the-scope clip (with videos). Gastrointest. Endosc. 2010, 72, 1289–1296. [Google Scholar] [CrossRef]
- Kobara, H.; Mori, H.; Nishiyama, N.; Fujihara, S.; Okano, K.; Suzuki, Y.; Masaki, T. Over-the-scope clip system: A review of 1517 cases over 9 years. J. Gastroenterol. Hepatol. 2019, 34, 22–30. [Google Scholar] [CrossRef] [PubMed]
- D’alessandro, A.; Galasso, G.; Zito, F.P.; Giardiello, C.; Cereatti, F.; Arienzo, R.; Pacini, F.; Chevallier, J.-M.; Donatelli, G. Role of Endoscopic Internal Drainage in Treating Gastro-Bronchial and Gastro-Colic Fistula After Sleeve Gastrectomy. Obes. Surg. 2022, 32, 342–348. [Google Scholar] [CrossRef]
- Keller, D.S.; Talboom, K.; Van Helsdingen, C.P.M.; Hompes, R. Treatment Modalities for Anastomotic Leakage in Rectal Cancer Surgery. Clin. Colon Rectal Surg. 2021, 34, 431–438. [Google Scholar] [CrossRef]
- Evrard, S.; Le Moine, O.; Lazaraki, G.; Dormann, A.; El Nakadi, I.; Devière, J. Self-expanding plastic stents for benign esophageal lesions. Gastrointest. Endosc. 2004, 60, 894–900. [Google Scholar] [CrossRef]
- Gelbmann, C.M.; Ratiu, N.L.; Rath, H.C.; Rogler, G.; Lock, G.; Schölmerich, J.; Kullmann, F. Use of self-expandable plastic stents for the treatment of esophageal perforations and symptomatic anastomotic leaks. Endoscopy 2004, 36, 695–699. [Google Scholar] [CrossRef]
- Symonds, C.J. The Treatment of Malignant Stricture of the Œsophagus by Tubage or Permanent Catheterism. Br. Med. J. 1887, 1, 870–873. [Google Scholar] [CrossRef]
- Vanbiervliet, G.; Filippi, J.; Karimdjee, B.S.; Venissac, N.; Iannelli, A.; Rahili, A.; Benizri, E.; Pop, D.; Staccini, P.; Tran, A.; et al. The role of clips in preventing migration of fully covered metallic esophageal stents: A pilot comparative study. Surg. Endosc. 2012, 26, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Winder, J.S.; Pauli, E.M. Comprehensive management of full-thickness luminal defects: The next frontier of gastrointestinal endoscopy. World J. Gastrointest. Endosc. 2015, 7, 758–768. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.Y.; Chen, W.T. Management of anastomotic leakage after rectal surgery: A review article. J. Gastrointest. Oncol. 2019, 10, 1229–1237. [Google Scholar] [CrossRef]
- Venezia, L.; Michielan, A.; Condino, G.; Sinagra, E.; Stasi, E.; Galeazzi, M.; Fabbri, C.; Anderloni, A. Feasibility and safety of self-expandable metal stent in nonmalignant disease of the lower gastrointestinal tract. World J. Gastrointest. Endosc. 2020, 12, 60–71. [Google Scholar] [CrossRef]
- Erdmann, D.; Drye, C.; Heller, L.; Wong, M.S.; Levin, S.L. Abdominal wall defect and enterocutaneous fistula treatment with the Vacuum-Assisted Closure (V.A.C.) system. Plast. Reconstr. Surg. 2001, 108, 2066–2068. [Google Scholar] [CrossRef] [PubMed]
- Nagell, C.F.; Holte, K. Treatment of anastomotic leakage after rectal resection with transrectal vacuum-assisted drainage (VAC). A method for rapid control of pelvic sepsis and healing. Int. J. Color. Dis. 2006, 21, 657–660. [Google Scholar] [CrossRef]
- Weidenhagen, R.; Gruetzner, K.U.; Wiecken, T.; Spelsberg, F.; Jauch, K.W. Endoscopic vacuum-assisted closure of anastomotic leakage following anterior resection of the rectum: A new method. Surg. Endosc. 2008, 22, 1818–1825. [Google Scholar] [CrossRef]
- Weidenhagen, R.; Hartl, W.H.; Gruetzner, K.U.; Eichhorn, M.E.; Spelsberg, F.; Jauch, K.W. Anastomotic leakage after esophageal resection: New treatment options by endoluminal vacuum therapy. Ann. Thorac. Surg. 2010, 90, 1674–1681. [Google Scholar] [CrossRef] [PubMed]
- Reimer, S.; Seyfried, F.; Flemming, S.; Brand, M.; Weich, A.; Widder, A.; Plaßmeier, L.; Kraus, P.; Döring, A.; Hering, I.; et al. Evolution of endoscopic vacuum therapy for upper gastrointestinal leakage over a 10-year period: A quality improvement study. Surg. Endosc. 2022, 36, 9169–9178. [Google Scholar] [CrossRef] [PubMed]
- Krokowicz, L.; Borejsza-Wysocki, M.; Mackiewicz, J.; Iqbal, A.; Drews, M. 10 years of Negative Pressure Wound Therapy (NPWT): Evolution of Indications for its Use. Negat. Press. Wound Ther. 2014, 1, 27–32. [Google Scholar]
- Weidenhagen, R.; Gruetzner, K.U.; Wiecken, T.; Spelsberg, F.; Jauch, K.W. Endoluminal vacuum therapy for the treatment of anastomotic leakage after anterior rectal resection. Rozhl. Chir. 2008, 87, 397–402. [Google Scholar] [PubMed]
- Gubler, C.; Schneider, P.M.; Bauerfeind, P. Complex anastomotic leaks following esophageal resections: The new stent over sponge (SOS) approach. Dis. Esophagus 2013, 26, 598–602. [Google Scholar] [CrossRef] [PubMed]
- Bartella, I.; Mallmann, C.; Bürger, M.; Toex, U.; Goeser, T.; Bruns, C.; Chon, S.H. Stent-over-sponge (SOS): A rescue option in patients with complex postoperative anastomotic leaks after esophagectomy. Endoscopy 2019, 51, E227–E228. [Google Scholar] [CrossRef] [PubMed]
- Morell, B.; Murray, F.; Vetter, D.; Bueter, M.; Gubler, C. Endoscopic vacuum therapy (EVT) for early infradiaphragmal leakage after bariatric surgery-outcomes of six consecutive cases in a single institution. Langenbecks Arch. Surg. 2019, 404, 115–121. [Google Scholar] [CrossRef]
- Pequignot, A.; Fuks, D.; Verhaeghe, P.; Dhahri, A.; Brehant, O.; Bartoli, E.; Delcenserie, R.; Yzet, T.; Regimbeau, J.M. Is there a place for pigtail drains in the management of gastric leaks after laparoscopic sleeve gastrectomy? Obes. Surg. 2012, 22, 712–720. [Google Scholar] [CrossRef]
- Donatelli, G.; Dumont, J.L.; Cereatti, F.; Ferretti, S.; Vergeau, B.M.; Tuszynski, T.; Pourcher, G.; Tranchart, H.; Mariani, P.; Meduri, A.; et al. Treatment of Leaks Following Sleeve Gastrectomy by Endoscopic Internal Drainage (EID). Obes. Surg. 2015, 25, 1293–1301. [Google Scholar] [CrossRef]
- Gonzalez, J.M.; Lorenzo, D.; Guilbaud, T.; Bège, T.; Barthet, M. Internal endoscopic drainage as first line or second line treatment in case of postsleeve gastrectomy fistulas. Endosc. Int. Open 2018, 6, E745–E750. [Google Scholar] [CrossRef]
- Chon, S.H.; Scherdel, J.; Rieck, I.; Lorenz, F.; Dratsch, T.; Kleinert, R.; Gebauer, F.; Fuchs, H.F.; Goeser, T.; Bruns, C.J. A new hybrid stent using endoscopic vacuum therapy in treating esophageal leaks: A prospective single-center experience of its safety and feasibility with mid-term follow-up. Dis. Esophagus 2022, 35, doab067. [Google Scholar] [CrossRef]
- Chon, S.H.; Töx, U.; Lorenz, F.; Rieck, I.; Wagner, B.J.; Kleinert, R.; Fuchs, H.F.; Goeser, T.; Quaas, A.; Bruns, C.J. A Novel Hybrid Stent with Endoscopic Vacuum Therapy for Treating Leaks of the Upper Gastrointestinal Tract. Visc. Med. 2021, 37, 403–409. [Google Scholar] [CrossRef]
- Pattynama, L.M.D.; Eshuis, W.J.; Van Berge Henegouwen, M.I.; Bergman, J.; Pouw, R.E. Vacuum-stent: A combination of endoscopic vacuum therapy and an intraluminal stent for treatment of esophageal transmural defects. Front. Surg. 2023, 10, 1145984. [Google Scholar] [CrossRef]
- Mahmood, Z.; Mcmahon, B.P.; Arfin, Q.; Byrne, P.J.; Reynolds, J.V.; Murphy, E.M.; Weir, D.G. Endocinch therapy for gastro-oesophageal reflux disease: A one year prospective follow up. Gut 2003, 52, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Schiefke, I.; Neumann, S.; Zabel-Langhennig, A.; Moessner, J.; Caca, K. Use of an Endoscopic Suturing Device (the ”ESD”) to Treat Patients with Gastroesophageal Reflux Disease, After Unsuccessful EndoCinch Endoluminal Gastroplication: Another Failure. Endoscopy 2005, 37, 700–705. [Google Scholar] [CrossRef] [PubMed]
- Moran, E.A.; Gostout, C.J.; Bingener, J. Preliminary performance of a flexible cap and catheter-based endoscopic suturing system. Gastrointest. Endosc. 2009, 69, 1375–1383. [Google Scholar] [CrossRef] [PubMed]
- Muniraj, T.; Harry, R. The use of OverStitchTM for the treatment of intestinal perforation, fistulas and leaks. Int. J. Gastrointest. Interv. 2017, 6, 151–156. [Google Scholar] [CrossRef]
- Zhang, L.Y.; Bejjani, M.; Ghandour, B.; Khashab, M.A. Endoscopic through-the-scope suturing. VideoGIE 2022, 7, 46–51. [Google Scholar] [CrossRef]
- Bi, D.; Zhang, L.Y.; Alqaisieh, M.; Shrigiriwar, A.; Farha, J.; Mahmoud, T.; Akiki, K.; Almario Jose, A.; Shah-Khan, S.M.; Gordon, S.R.; et al. Novel Through-the-Scope Suture Closure of Colonic Endoscopic Mucosal Resection Defects. Gastrointest. Endosc. 2023, 98, 122–129. [Google Scholar] [CrossRef]
- Chon, S.H.; Toex, U.; Plum, P.S.; Kleinert, R.; Bruns, C.J.; Goeser, T.; Berlth, F. Efficacy and feasibility of OverStitch suturing of leaks in the upper gastrointestinal tract. Surg. Endosc. 2020, 34, 3861–3869. [Google Scholar] [CrossRef]
- Mohan, B.; Khan, S.R.; Madhu, D.; Kassab, L.; Jonnadula, S.; Chandan, S.; Facciorusso, A.; Adler, D. Clinical Outcomes of Endoscopic Suturing in Gastrointestinal Fistulas, Leaks, Perforations and Mucosal Defects: A Systematic Review and Meta-Analysis. Am. J. Gastroenterol. 2021, 116, S470–S471. [Google Scholar] [CrossRef]
- Granata, A.; Amata, M.; Ligresti, D.; Martino, A.; Tarantino, I.; Barresi, L.; Traina, M. Endoscopic management of post-surgical GI wall defects with the overstitch endosuturing system: A single-center experience. Surg. Endosc. 2020, 34, 3805–3817. [Google Scholar] [CrossRef]
- Ge, P.S.; Thompson, C.C. The Use of the Overstitch to Close Perforations and Fistulas. Gastrointest. Endosc. Clin. N. Am. 2020, 30, 147–161. [Google Scholar] [CrossRef]
- Pang, M.; Mousa, O.; Werlang, M.; Brahmbhatt, B.; Woodward, T. A hybrid endoscopic technique to close tracheoesophageal fistula. VideoGIE 2018, 3, 15–16. [Google Scholar] [CrossRef] [PubMed]
- Nachira, D.; Trivisonno, A.; Costamagna, G.; Toietta, G.; Margaritora, S.; Pontecorvi, V.; Punzo, G.; Porziella, V.; Boskoski, I. Successful Therapy of Esophageal Fistulas by Endoscopic Injection of Emulsified Adipose Tissue Stromal Vascular Fraction. Gastroenterology 2021, 160, 1026–1028. [Google Scholar] [CrossRef] [PubMed]
- Porziella, V.; Nachira, D.; Boškoski, I.; Trivisonno, A.; Costamagna, G.; Margaritora, S. Emulsified stromal vascular fraction tissue grafting: A new frontier in the treatment of esophageal fistulas. Gastrointest. Endosc. 2020, 92, 1262–1263. [Google Scholar] [CrossRef] [PubMed]
- Mongardini, F.M.; Cacciatore, C.; Catauro, A.; Maglione, F.; Picardi, F.; Lauro, A.; Gambardella, C.; Allaria, A.; Docimo, L. Stemming the Leak: A Novel Treatment for Gastro-Bronchial Fistula. Dig. Dis. Sci. 2022, 67, 5425–5432. [Google Scholar] [CrossRef]
- Shogan, B.D.; Belogortseva, N.; Luong, P.M.; Zaborin, A.; Lax, S.; Bethel, C.; Ward, M.; Muldoon, J.P.; Singer, M.; An, G.; et al. Collagen degradation and MMP9 activation by Enterococcus faecalis contribute to intestinal anastomotic leak. Sci. Transl. Med. 2015, 7, 286ra68. [Google Scholar] [CrossRef] [PubMed]
- Olivas, A.D.; Shogan, B.D.; Valuckaite, V.; Zaborin, A.; Belogortseva, N.; Musch, M.; Meyer, F.; Trimble, W.L.; An, G.; Gilbert, J.; et al. Intestinal tissues induce an SNP mutation in Pseudomonas aeruginosa that enhances its virulence: Possible role in anastomotic leak. PLoS ONE 2012, 7, e44326. [Google Scholar] [CrossRef]
- Guyton, K.; Belogortseva, N.; Levine, Z.; Kaiser, B.D.; Sangwan, N.; Hyman, N.; Shogan, B.D.; Zaborina, O.; Alverdy, J.C. Patient Acceptance of Routine Serial Postoperative Endoscopy Following Low Anterior Resection (LAR) and Its Ability to Detect Biomarkers in Anastomotic Lavage Fluid. World J. Surg. 2021, 45, 2227–2234. [Google Scholar] [CrossRef]
- Kotzampassi, K. Why Give My Surgical Patients Probiotics. Nutrients 2022, 14, 4389. [Google Scholar] [CrossRef]
- Kotzampassi, K. What Surgeon Should Know about Probiotics. Nutrients 2022, 14, 4374. [Google Scholar] [CrossRef]
- Tarapatzi, G.; Filidou, E.; Kandilogiannakis, L.; Spathakis, M.; Gaitanidou, M.; Arvanitidis, K.; Drygiannakis, I.; Valatas, V.; Kotzampassi, K.; Manolopoulos, V.G.; et al. The Probiotic Strains Bifidοbacterium lactis, Lactobacillus acidophilus, Lactiplantibacillus plantarum and Saccharomyces boulardii Regulate Wound Healing and Chemokine Responses in Human Intestinal Subepithelial Myofibroblasts. Pharmaceuticals 2022, 15, 1293. [Google Scholar] [CrossRef]
- Filidou, E.; Kolios, G. Probiotics in Intestinal Mucosal Healing: A New Therapy or an Old Friend? Pharmaceuticals 2021, 14, 1181. [Google Scholar] [CrossRef] [PubMed]
- Williamson, A.J.; Alverdy, J.C. Influence of the Microbiome on Anastomotic Leak. Clin. Colon Rectal Surg. 2021, 34, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Moysidis, M.; Stavrou, G.; Cheva, A.; Abba Deka, I.; Tsetis, J.K.; Birba, V.; Kapoukranidou, D.; Ioannidis, A.; Tsaousi, G.; Kotzampassi, K. The 3-D configuration of excisional skin wound healing after topical probiotic application. Injury 2022, 53, 1385–1393. [Google Scholar] [CrossRef]
- Kelm, M.; Anger, F. Mucosa and microbiota—The role of intrinsic parameters on intestinal wound healing. Front. Surg. 2022, 9, 905049. [Google Scholar] [CrossRef]
- Kotzampassi, K.; Stavrou, G.; Damoraki, G.; Georgitsi, M.; Basdanis, G.; Tsaousi, G.; Giamarellos-Bourboulis, E.J. A Four-Probiotics Regimen Reduces Postoperative Complications After Colorectal Surgery: A Randomized, Double-Blind, Placebo-Controlled Study. World J. Surg. 2015, 39, 2776–2783. [Google Scholar] [CrossRef] [PubMed]
- Bemelman, W.A.; Baron, T.H. Endoscopic Management of Transmural Defects, Including Leaks, Perforations, and Fistulae. Gastroenterology 2018, 154, 1938–1946.e1931. [Google Scholar] [CrossRef] [PubMed]
- Mandarino, F.V.; Barchi, A.; D’amico, F.; Fanti, L.; Azzolini, F.; Viale, E.; Esposito, D.; Rosati, R.; Fiorino, G.; Bemelman, W.A.; et al. Endoscopic Vacuum Therapy (EVT) versus Self-Expandable Metal Stent (SEMS) for Anastomotic Leaks after Upper Gastrointestinal Surgery: Systematic Review and Meta-Analysis. Life 2023, 13, 287. [Google Scholar] [CrossRef] [PubMed]
- Vargas, E.J.; Abu Dayyeh, B.K. Keep calm under pressure: A paradigm shift in managing postsurgical leaks. Gastrointest. Endosc. 2018, 87, 438–441. [Google Scholar] [CrossRef]
- Rodrigues-Pinto, E.; Morais, R.; Macedo, G.; Khashab, M.A. Choosing the Appropriate Endoscopic Armamentarium for Treatment of Anastomotic Leaks. Am. J. Gastroenterol. 2019, 114, 367–371. [Google Scholar] [CrossRef]
- Eisendrath, P.; Devière, J. Digestive leaks: An approach tailored to both indication and anatomy. Endosc. Int. Open 2016, 4, E652–E653. [Google Scholar] [CrossRef]
- Rodrigues-Pinto, E.; Repici, A.; Donatelli, G.; Macedo, G.; Devière, J.; Van Hooft, J.E.; Campos, J.M.; Galvao Neto, M.; Silva, M.; Eisendrath, P.; et al. International multicenter expert survey on endoscopic treatment of upper gastrointestinal anastomotic leaks. Endosc. Int. Open 2019, 7, E1671–E1682. [Google Scholar] [CrossRef] [PubMed]
- Hedrick, T.L.; Kane, W. Management of Acute Anastomotic Leaks. Clin. Colon Rectal Surg. 2021, 34, 400–405. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.M.; Auyeung, K.K.Y.; Lam, S.F.; Chiu, P.W.Y.; Teoh, A.Y.B. Current status in endoscopic management of upper gastrointestinal perforations, leaks and fistulas. Dig. Endosc. 2022, 34, 43–62. [Google Scholar] [CrossRef] [PubMed]
- Giraldo-Grueso, M.; Bolton, N.; Brown, R. Endoscopic Vacuum Therapy via Pharyngostomy: Novel Access for Management of Upper Gastrointestinal Defects. Am. Surg. 2022, 88, 680–685. [Google Scholar] [CrossRef]
- Groitl, H.; Scheele, J. Initial experience with the endoscopic application of fibrin tissue adhesive in the upper gastrointestinal tract. Surg. Endosc. 1987, 1, 93–97. [Google Scholar] [CrossRef]
- Eleftheriadis, E.; Tzartinoglou, E.; Kotzampassi, K.; Aletras, H. Early endoscopic fibrin sealing of high-output postoperative enterocutaneous fistulas. Acta Chir. Scand. 1990, 156, 625–628. [Google Scholar]
- Papavramidis, S.T.; Eleftheriadis, E.E.; Apostolidis, D.N.; Kotzampassi, K.E. Endoscopic fibrin sealing of high-output non-healing gastrocutaneous fistulas after vertical gastroplasty in morbidly obese patients. Obes. Surg. 2001, 11, 766–769. [Google Scholar] [CrossRef]
- Papavramidis, S.T.; Eleftheriadis, E.E.; Papavramidis, T.S.; Kotzampassi, K.E.; Gamvros, O.G. Endoscopic management of gastrocutaneous fistula after bariatric surgery by using a fibrin sealant. Gastrointest. Endosc. 2004, 59, 296–300. [Google Scholar] [CrossRef]
- Papavramidis, T.S.; Kotzampassi, K.; Kotidis, E.; Eleftheriadis, E.E.; Papavramidis, S.T. Endoscopic fibrin sealing of gastrocutaneous fistulas after sleeve gastrectomy and biliopancreatic diversion with duodenal switch. J. Gastroenterol. Hepatol. 2008, 23, 1802–1805. [Google Scholar] [CrossRef]
- Plat, V.D.; Bootsma, B.T.; Van Der Wielen, N.; Straatman, J.; Schoonmade, L.J.; Van Der Peet, D.L.; Daams, F. The role of tissue adhesives in esophageal surgery, a systematic review of literature. Int. J. Surg. 2017, 40, 163–168. [Google Scholar] [CrossRef]
- Nordentoft, T.; Pommergaard, H.C.; Rosenberg, J.; Achiam, M.P. Fibrin glue does not improve healing of gastrointestinal anastomoses: A systematic review. Eur. Surg. Res. 2015, 54, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lippert, E.; Klebl, F.H.; Schweller, F.; Ott, C.; Gelbmann, C.M.; Schölmerich, J.; Endlicher, E.; Kullmann, F. Fibrin glue in the endoscopic treatment of fistulae and anastomotic leakages of the gastrointestinal tract. Int. J. Color. Dis. 2011, 26, 303–311. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Sahakian, A.B. Endoscopic Closure of Gastrointestinal Fistulae and Leaks. Gastrointest. Endosc. Clin. N. Am. 2018, 28, 233–249. [Google Scholar] [CrossRef]
- Law, R.; Wong Kee Song, L.M.; Irani, S.; Baron, T.H. Immediate technical and delayed clinical outcome of fistula closure using an over-the-scope clip device. Surg. Endosc. 2015, 29, 1781–1786. [Google Scholar] [CrossRef] [PubMed]
- Seebach, L.; Bauerfeind, P.; Gubler, C. “Sparing the surgeon”: Clinical experience with over-the-scope clips for gastrointestinal perforation. Endoscopy 2010, 42, 1108–1111. [Google Scholar] [CrossRef]
- Barras, C.D.; Myers, K.A. Nitinol—Its use in vascular surgery and other applications. Eur. J. Vasc. Endovasc. Surg. 2000, 19, 564–569. [Google Scholar] [CrossRef]
- Zurstrassen, C.E.; Bitencourt, A.G.V.; Guimaraes, M.D.; Cavalcante, A.; Tyng, C.J.; Amoedo, M.K.; Matsushita Junior, J.P.K.; Szklaruk, J.; Marchiori, E.; Chojniak, R. Percutaneous stent placement for the treatment of malignant biliary obstruction: Nitinol versus elgiloy stents. Radiol. Bras. 2017, 50, 97–102. [Google Scholar] [CrossRef]
- Eloubeidi, M.A.; Talreja, J.P.; Lopes, T.L.; Al-Awabdy, B.S.; Shami, V.M.; Kahaleh, M. Success and complications associated with placement of fully covered removable self-expandable metal stents for benign esophageal diseases (with videos). Gastrointest. Endosc. 2011, 73, 673–681. [Google Scholar] [CrossRef]
- Mandarino, F.V.; Esposito, D.; Spelta, G.N.E.; Cavestro, G.M.; Rosati, R.; Parise, P.; Gemma, M.F.; Fanti, L. Double layer stent for the treatment of leaks and fistula after upper gastrointestinal oncologic surgery: A retrospective study. Updates Surg. 2022, 74, 1055–1062. [Google Scholar] [CrossRef]
- Larsen, M.; Kozarek, R. Therapeutic endoscopy for the treatment of post-bariatric surgery complications. World J. Gastroenterol. 2022, 28, 199–215. [Google Scholar] [CrossRef]
- Law, R.; Prabhu, A.; Fujii-Lau, L.; Shannon, C.; Singh, S. Stent migration following endoscopic suture fixation of esophageal self-expandable metal stents: A systematic review and meta-analysis. Surg. Endosc. 2018, 32, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Lamazza, A.; Sterpetti, A.V.; De Cesare, A.; Schillaci, A.; Antoniozzi, A.; Fiori, E. Endoscopic placement of self-expanding stents in patients with symptomatic anastomotic leakage after colorectal resection for cancer: Long-term results. Endoscopy 2015, 47, 270–272. [Google Scholar] [CrossRef] [PubMed]
- Lamazza, A.; Fiori, E.; Schillaci, A.; Sterpetti, A.V.; Lezoche, E. Treatment of anastomotic stenosis and leakage after colorectal resection for cancer with self-expandable metal stents. Am. J. Surg. 2014, 208, 465–469. [Google Scholar] [CrossRef] [PubMed]
- Dimaio, C.J.; Dorfman, M.P.; Gardner, G.J.; Nash, G.M.; Schattner, M.A.; Markowitz, A.J.; Chi, D.S.; Gerdes, H. Covered esophageal self-expandable metal stents in the nonoperative management of postoperative colorectal anastomotic leaks. Gastrointest. Endosc. 2012, 76, 431–435. [Google Scholar] [CrossRef]
- Puli, S.R.; Spofford, I.S.; Thompson, C.C. Use of self-expandable stents in the treatment of bariatric surgery leaks: A systematic review and meta-analysis. Gastrointest. Endosc. 2012, 75, 287–293. [Google Scholar] [CrossRef]
- Lalezari, S.; Lee, C.J.; Borovikova, A.A.; Banyard, D.A.; Paydar, K.Z.; Wirth, G.A.; Widgerow, A.D. Deconstructing negative pressure wound therapy. Int. Wound J. 2017, 14, 649–657. [Google Scholar] [CrossRef]
- Vignali, A.; De Nardi, P. Endoluminal vacuum-assisted therapy to treat rectal anastomotic leakage: A critical analysis. World J. Gastroenterol. 2022, 28, 1394–1404. [Google Scholar] [CrossRef]
- Smallwood, N.R.; Fleshman, J.W.; Leeds, S.G.; Burdick, J.S. The use of endoluminal vacuum (E-Vac) therapy in the management of upper gastrointestinal leaks and perforations. Surg. Endosc. 2016, 30, 2473–2480. [Google Scholar] [CrossRef]
- Grund, K.E.; Schweizer, U.; Zipfel, A.; Duckworth-Mothes, B. Learning of flexible endoscopy, particularly endoscopic vacuum therapy (EVT). Chirurg 2022, 93, 56–63. [Google Scholar] [CrossRef]
- Chorti, A.; Stavrou, G.; Stelmach, V.; Tsaousi, G.; Michalopoulos, A.; Papavramidis, T.S.; Kotzampassi, K. Endoscopic repair of anastomotic leakage after low anterior resection for rectal cancer: A systematic review. Asian J. Endosc. Surg. 2020, 13, 141–146. [Google Scholar] [CrossRef]
- Seika, P.; Biebl, M.; Raakow, J.; Berndt, N.; Feldbrügge, L.; Maurer, M.M.; Dobrindt, E.; Thuss-Patience, P.; Pratschke, J.; Denecke, C. The Association between Neoadjuvant Radio-Chemotherapy and Prolonged Healing of Anastomotic Leakage after Esophageal Resection Treated with EndoVAC Therapy. J. Clin. Med. 2022, 11, 4773. [Google Scholar] [CrossRef]
- Riss, S.; Stift, A.; Meier, M.; Haiden, E.; Grünberger, T.; Bergmann, M. Endo-sponge assisted treatment of anastomotic leakage following colorectal surgery. Color. Dis. 2010, 12, e104–e108. [Google Scholar] [CrossRef] [PubMed]
- Loske, G.; Müller, C.T. Tips and tricks for endoscopic negative pressure therapy. Chirurg 2019, 90, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Loske, G.; Schorsch, T.; Rucktaeschel, F.; Schulze, W.; Riefel, B.; Van Ackeren, V.; Mueller, C.T. Open-pore film drainage (OFD): A new multipurpose tool for endoscopic negative pressure therapy (ENPT). Endosc. Int. Open 2018, 6, E865–E871. [Google Scholar] [CrossRef] [PubMed]
- De Moura, D.T.H.; Hirsch, B.S.; Do Monte Junior, E.S.; Mccarty, T.R.; De Medeiros, F.S.; Thompson, C.C.; De Moura, E.G.H. Cost-effective modified endoscopic vacuum therapy for the treatment of gastrointestinal transmural defects: Step-by-step process of manufacturing and its advantages. VideoGIE 2021, 6, 523–528. [Google Scholar] [CrossRef]
- Yin, Q.; Zhou, S.; Song, Y.; Xun, X.; Liu, N.; Liu, L. Treatment of intrathoracic anastomotic leak after esophagectomy with the sump drainage tube. J. Cardiothorac. Surg. 2021, 16, 46. [Google Scholar] [CrossRef]
- Eichelmann, A.K.; Ismail, S.; Merten, J.; Slepecka, P.; Palmes, D.; Laukötter, M.G.; Pascher, A.; Mardin, W.A. Economic Burden of Endoscopic Vacuum Therapy Compared to Alternative Therapy Methods in Patients with Anastomotic Leakage After Esophagectomy. J. Gastrointest. Surg. 2021, 25, 2447–2454. [Google Scholar] [CrossRef]
- Yzet, C.; Hakim, S.; Pioche, M.; Le Mouel, J.P.; Deschepper, C.; Lafeuille, P.; Delcenserie, R.; Yzet, T.; Nguyen-Khac, E.; Fumery, M.; et al. Endoscopic treatment of large gastric leaks after gastrectomy using the combination of double pigtail drains crossing a covered stent. Surg. Endosc. 2022, 36, 9469–9475. [Google Scholar] [CrossRef]
- Donatelli, G.; Dumont, J.L.; Cereatti, F.; Dhumane, P.; Tuszynski, T.; Vergeau, B.M.; Meduri, B. Endoscopic internal drainage as first-line treatment for fistula following gastrointestinal surgery: A case series. Endosc. Int. Open 2016, 4, E647–E651. [Google Scholar] [CrossRef]
- Buerger, M.; Herbold, T.; Lange, S.; Berlth, F.; Plum, P.; Schramm, C.; Kleinert, R.; Goeser, T.; Bruns, C.; Chon, S.-H. In Vitro Evaluation of Mechanical Properties of Segmented Esophageal Self-Expandable Metal Stents: Innovative Test Methods Are Needed. J. Laparoendosc. Adv. Surg. Tech. 2019, 29, 1168–1173. [Google Scholar] [CrossRef]
- Freeman, R.K.; Ascioti, A.J.; Dake, M.; Mahidhara, R.S. An Assessment of the Optimal Time for Removal of Esophageal Stents Used in the Treatment of an Esophageal Anastomotic Leak or Perforation. Ann. Thorac. Surg. 2015, 100, 422–428. [Google Scholar] [PubMed]
- Sharaiha, R.Z.; Kumta, N.A.; Defilippis, E.M.; Dimaio, C.J.; Gonzalez, S.; Gonda, T.; Rogart, J.; Siddiqui, A.; Berg, P.S.; Samuels, P.; et al. A Large Multicenter Experience With Endoscopic Suturing for Management of Gastrointestinal Defects and Stent Anchorage in 122 Patients: A Retrospective Review. J. Clin. Gastroenterol. 2016, 50, 388–392. [Google Scholar] [CrossRef] [PubMed]
- Alam, A.; Leoni, G.; Quiros, M.; Wu, H.; Desai, C.; Nishio, H.; Jones, R.M.; Nusrat, A.; Neish, A.S. The microenvironment of injured murine gut elicits a local pro-restitutive microbiota. Nat. Microbiol. 2016, 1, 15021. [Google Scholar] [CrossRef] [PubMed]
- Hyoju, S.K.; Adriaansens, C.; Wienholts, K.; Sharma, A.; Keskey, R.; Arnold, W.; Van Dalen, D.; Gottel, N.; Hyman, N.; Zaborin, A.; et al. Low-fat/high-fibre diet prehabilitation improves anastomotic healing via the microbiome: An experimental model. Br. J. Surg. 2020, 107, 743–755. [Google Scholar] [CrossRef]
- Buttar, N.S. Minimally invasive endoscopic approaches to manage postsurgical leaks: Time to recognize the finger in the dike. Gastrointest. Endosc. 2021, 93, 1300–1303. [Google Scholar] [CrossRef] [PubMed]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menni, A.; Stavrou, G.; Tzikos, G.; Shrewsbury, A.D.; Kotzampassi, K. Endoscopic Salvage of Gastrointestinal Anastomosis Leaks—Past, Present, and Future—A Narrated Review. Gastrointest. Disord. 2023, 5, 383-407. https://doi.org/10.3390/gidisord5030032
Menni A, Stavrou G, Tzikos G, Shrewsbury AD, Kotzampassi K. Endoscopic Salvage of Gastrointestinal Anastomosis Leaks—Past, Present, and Future—A Narrated Review. Gastrointestinal Disorders. 2023; 5(3):383-407. https://doi.org/10.3390/gidisord5030032
Chicago/Turabian StyleMenni, Alexandra, George Stavrou, Georgios Tzikos, Anne D. Shrewsbury, and Katerina Kotzampassi. 2023. "Endoscopic Salvage of Gastrointestinal Anastomosis Leaks—Past, Present, and Future—A Narrated Review" Gastrointestinal Disorders 5, no. 3: 383-407. https://doi.org/10.3390/gidisord5030032





