Impression Reference Technique for the Open Flap Digital Workflow in the Immediate Loading Rehabilitation of the Upper and Lower Jaws
Abstract
1. Introduction
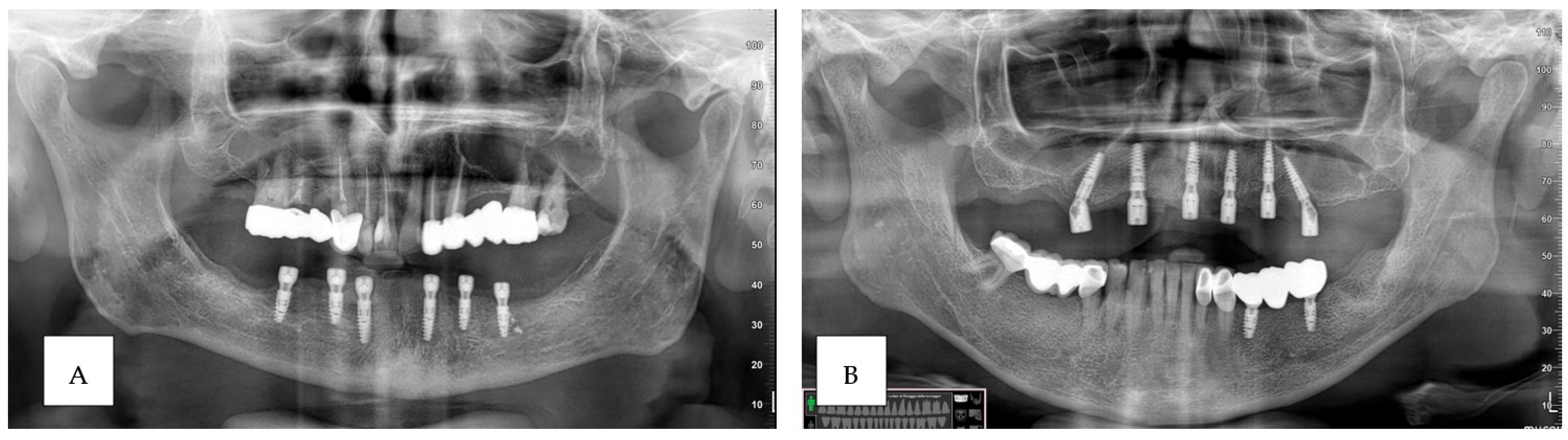
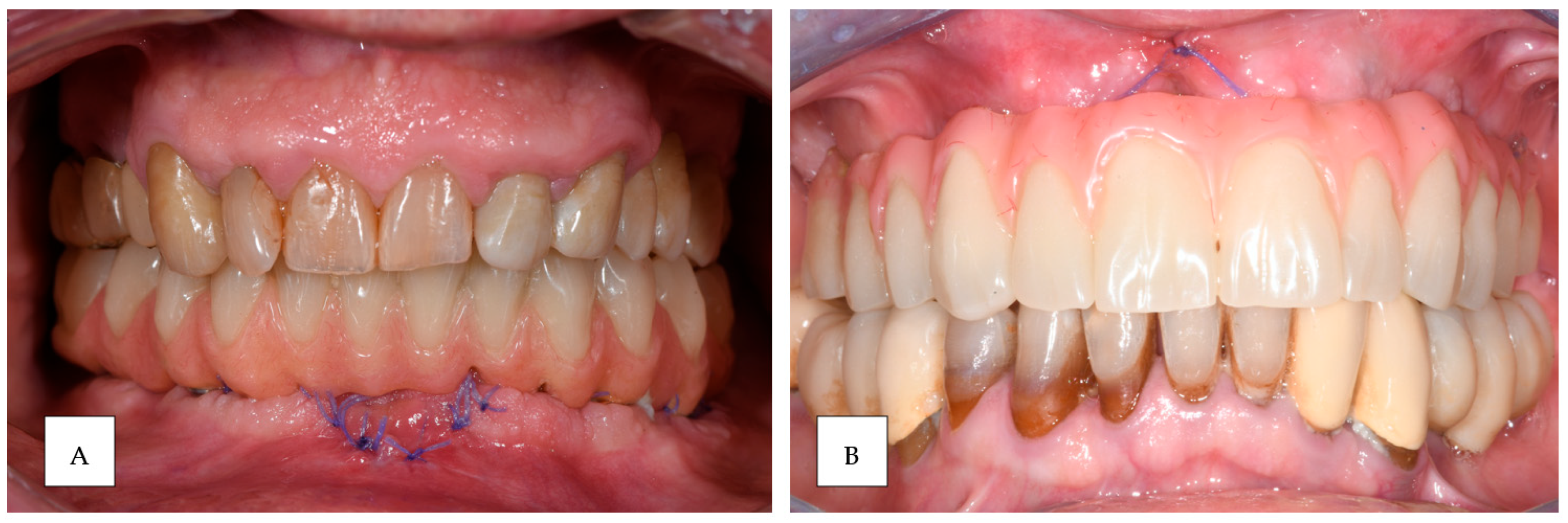
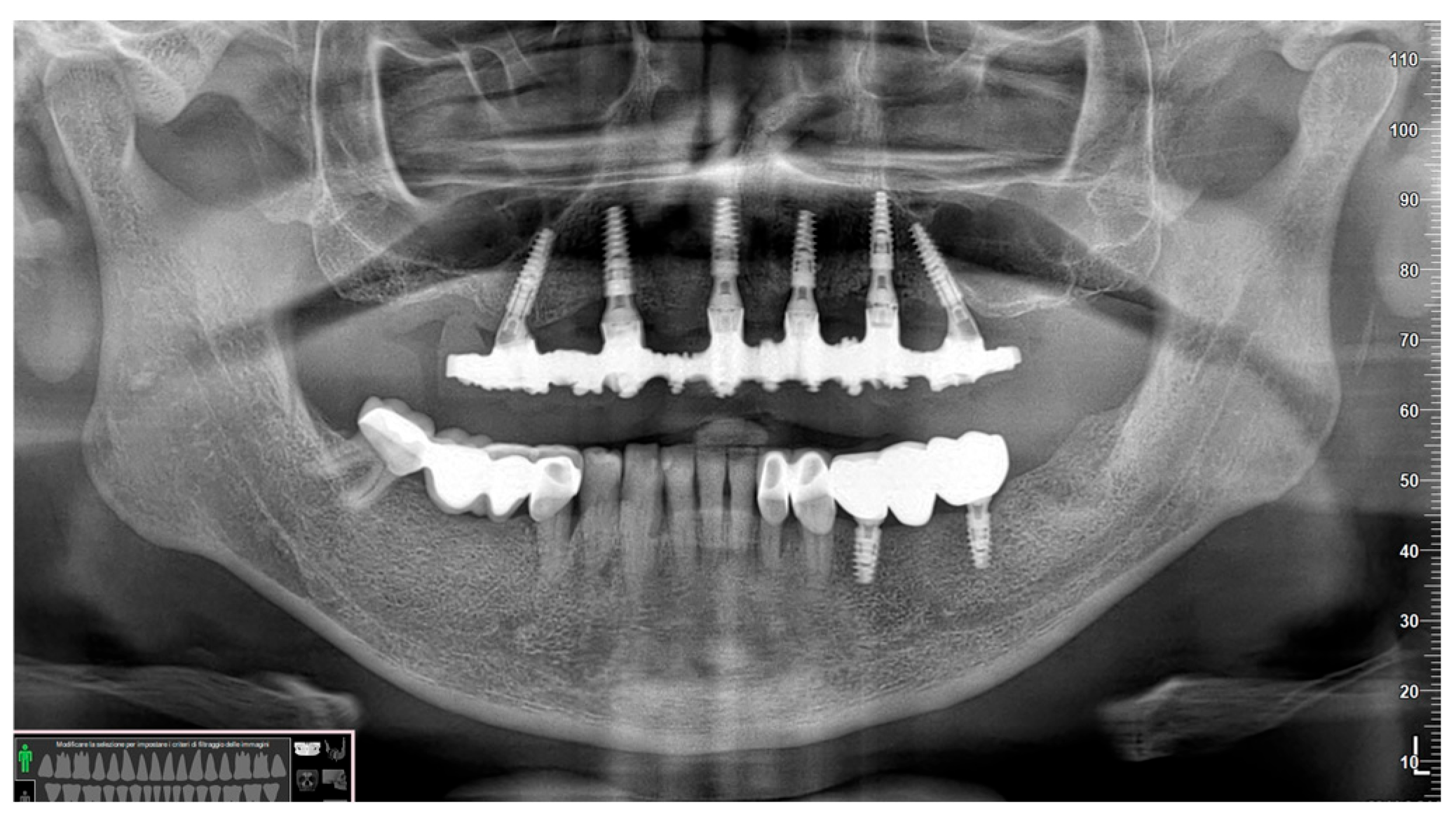
2. Materials and Methods
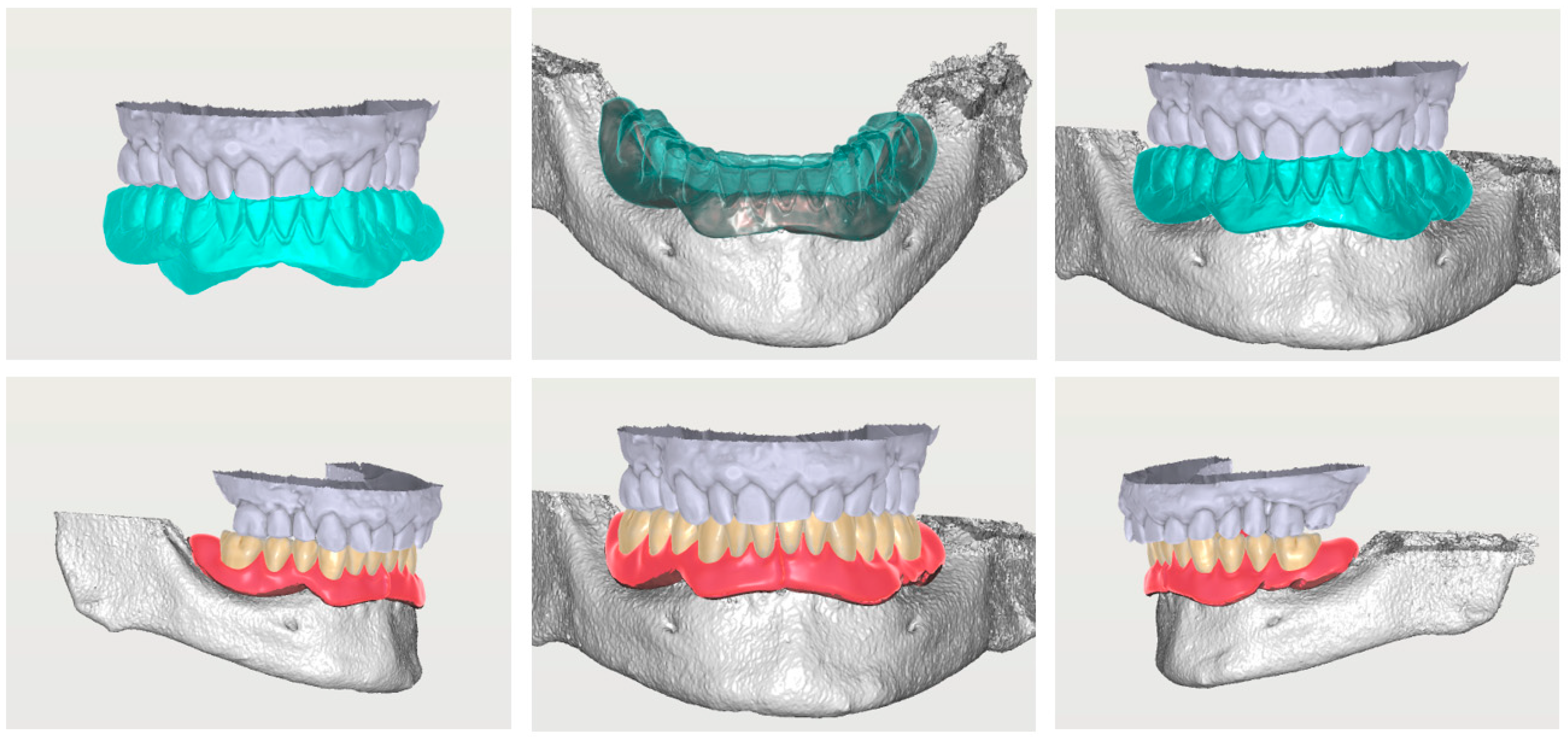
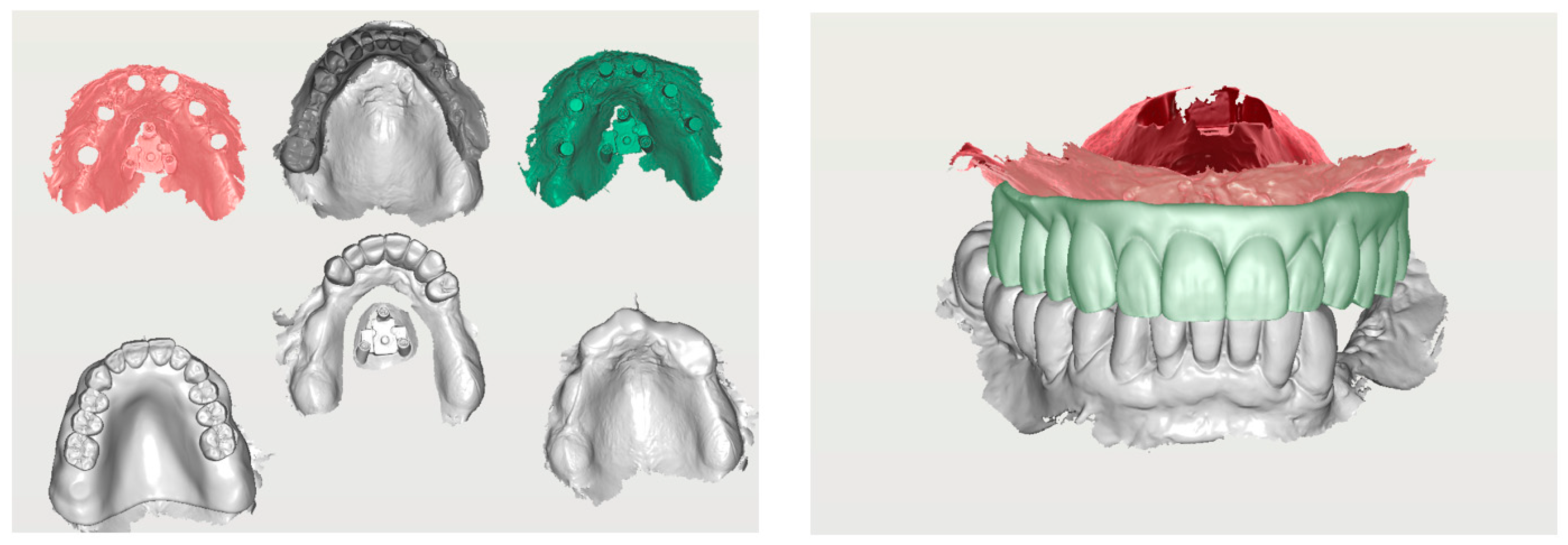
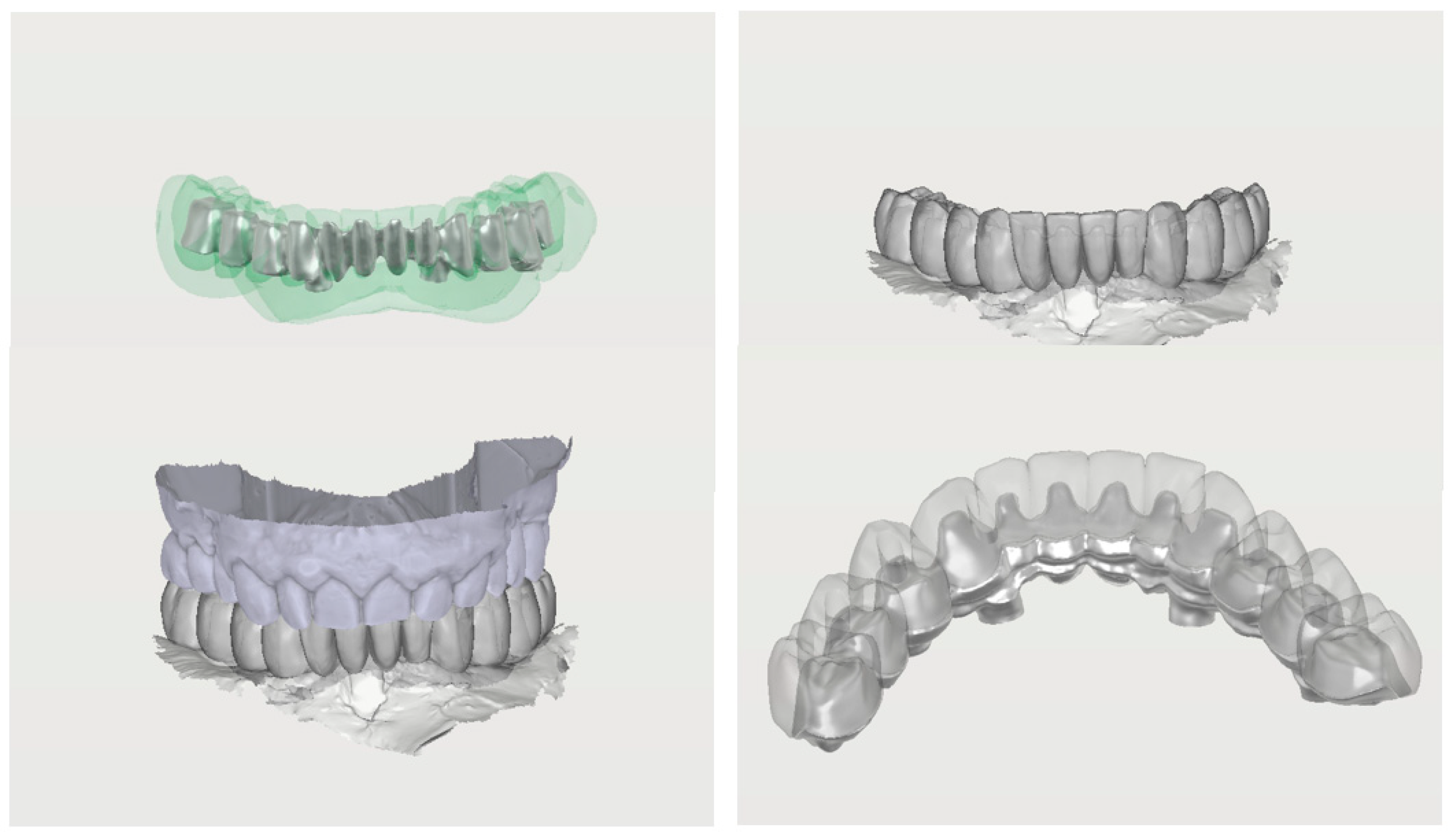
2.1. Digital Workflow
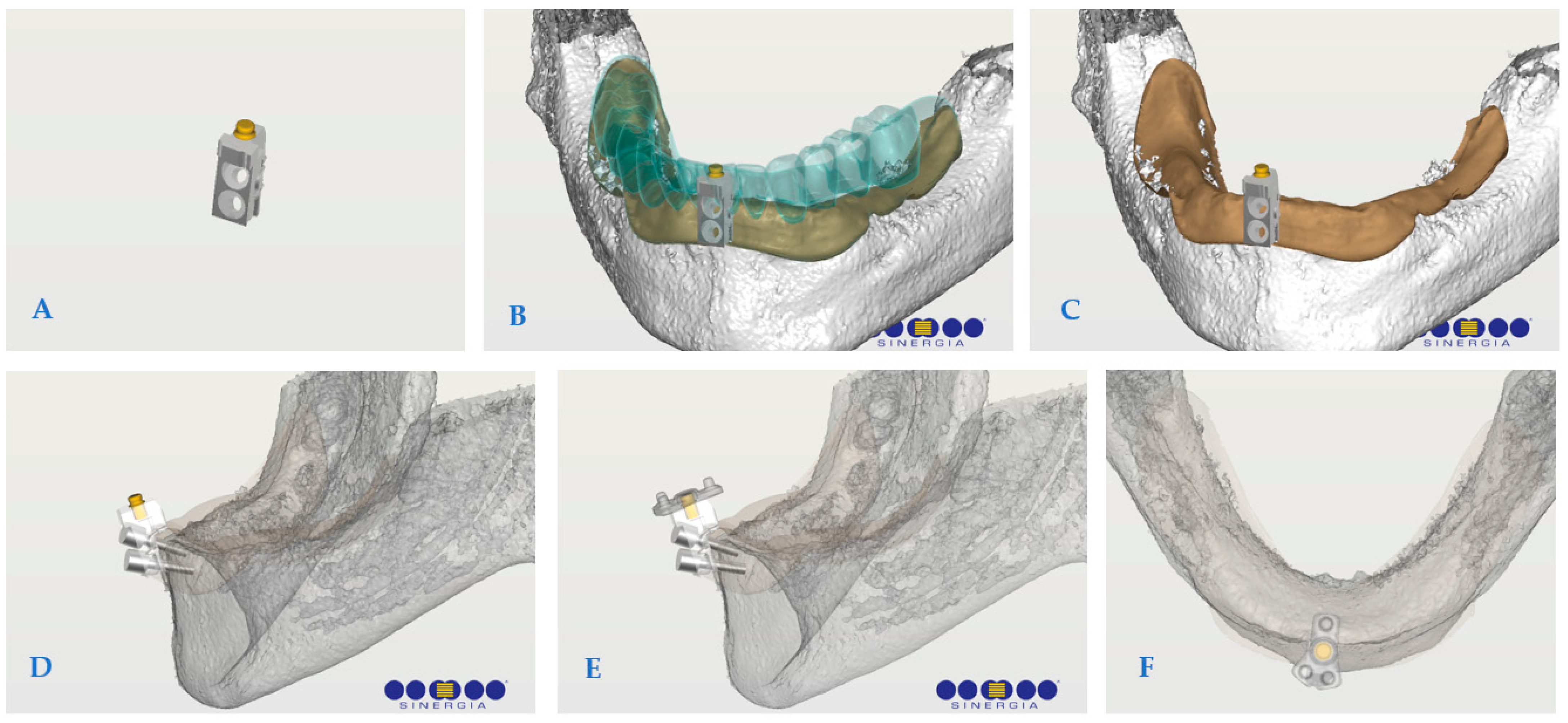
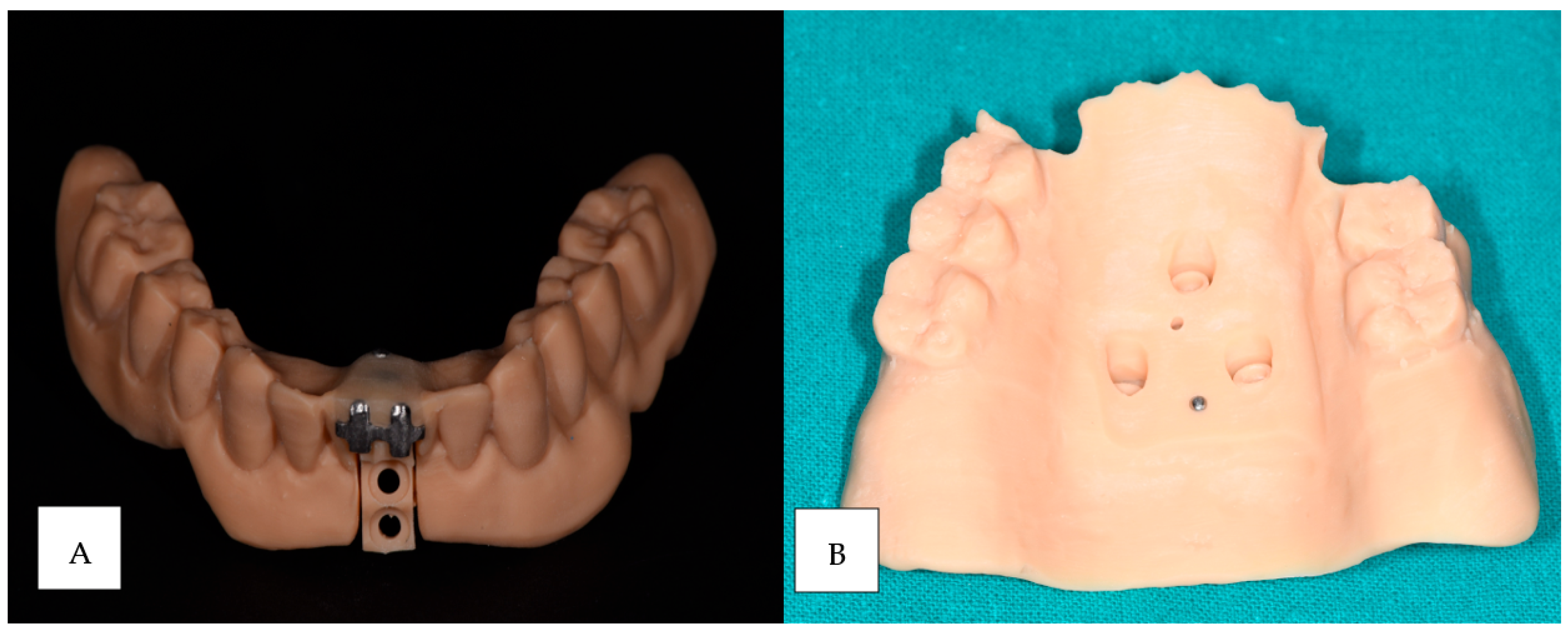
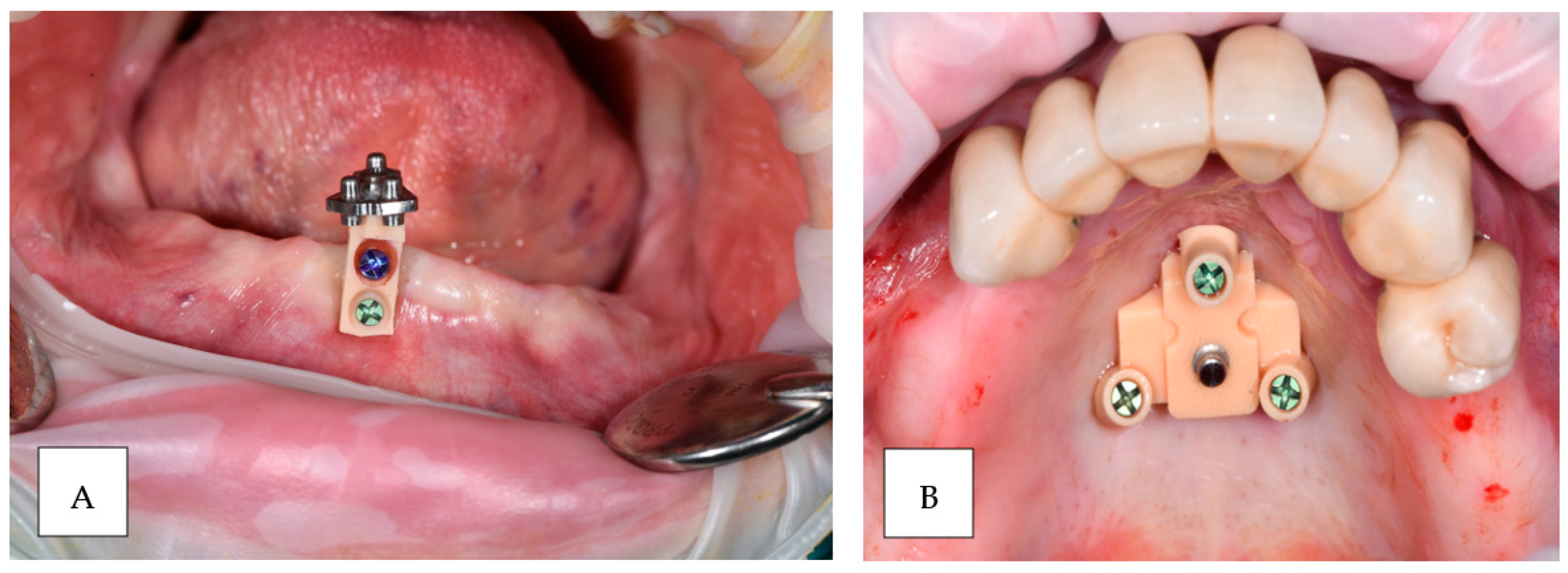
2.2. Impression Reference Technique Device
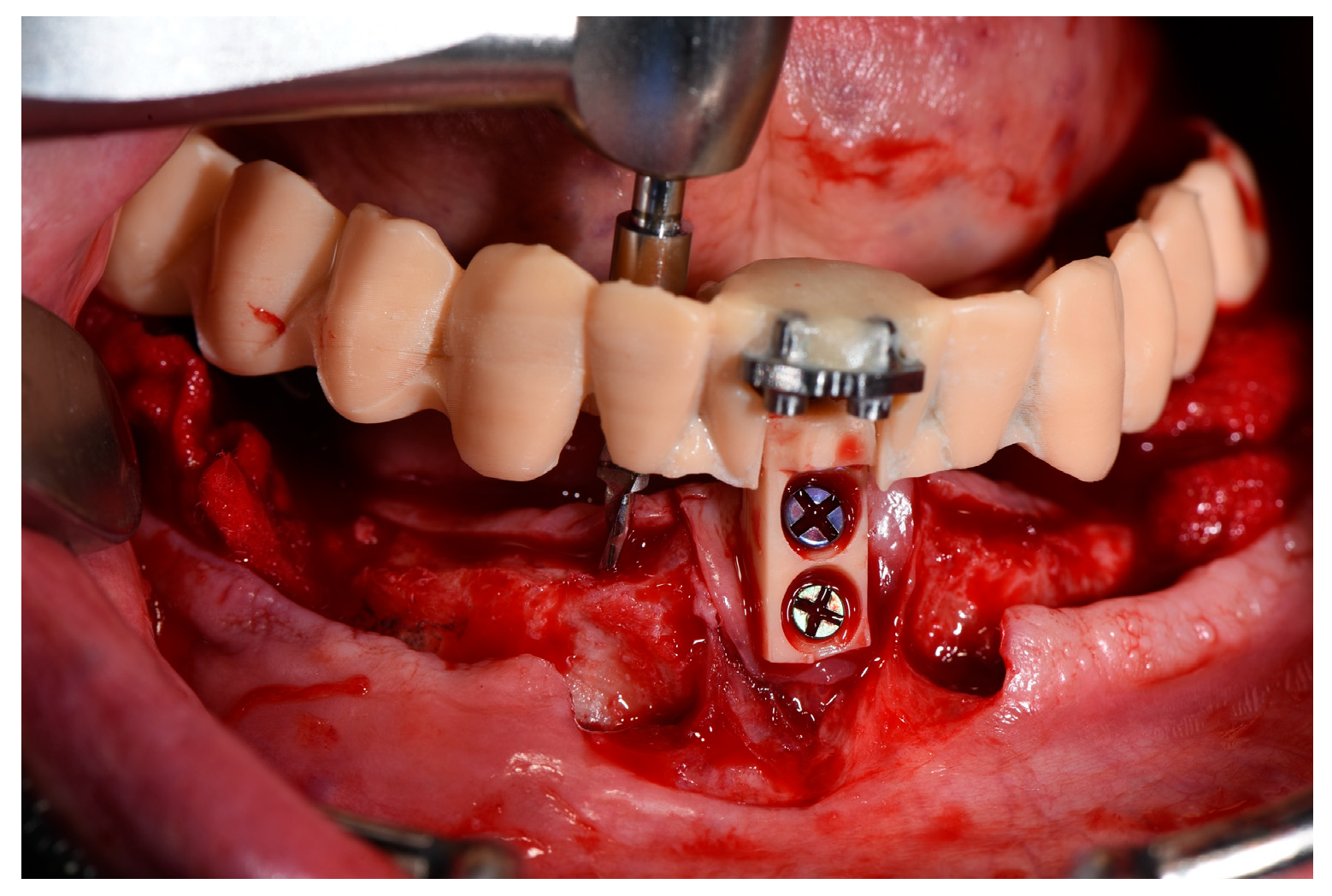
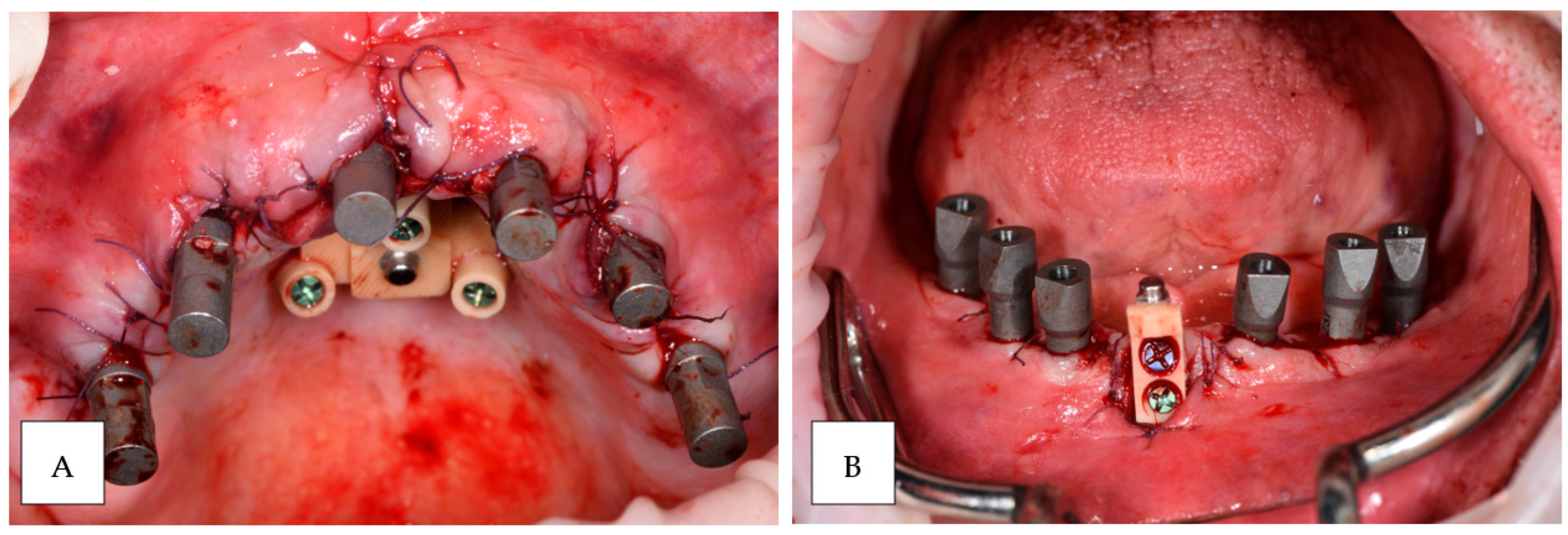
2.3. Surgical Procedure
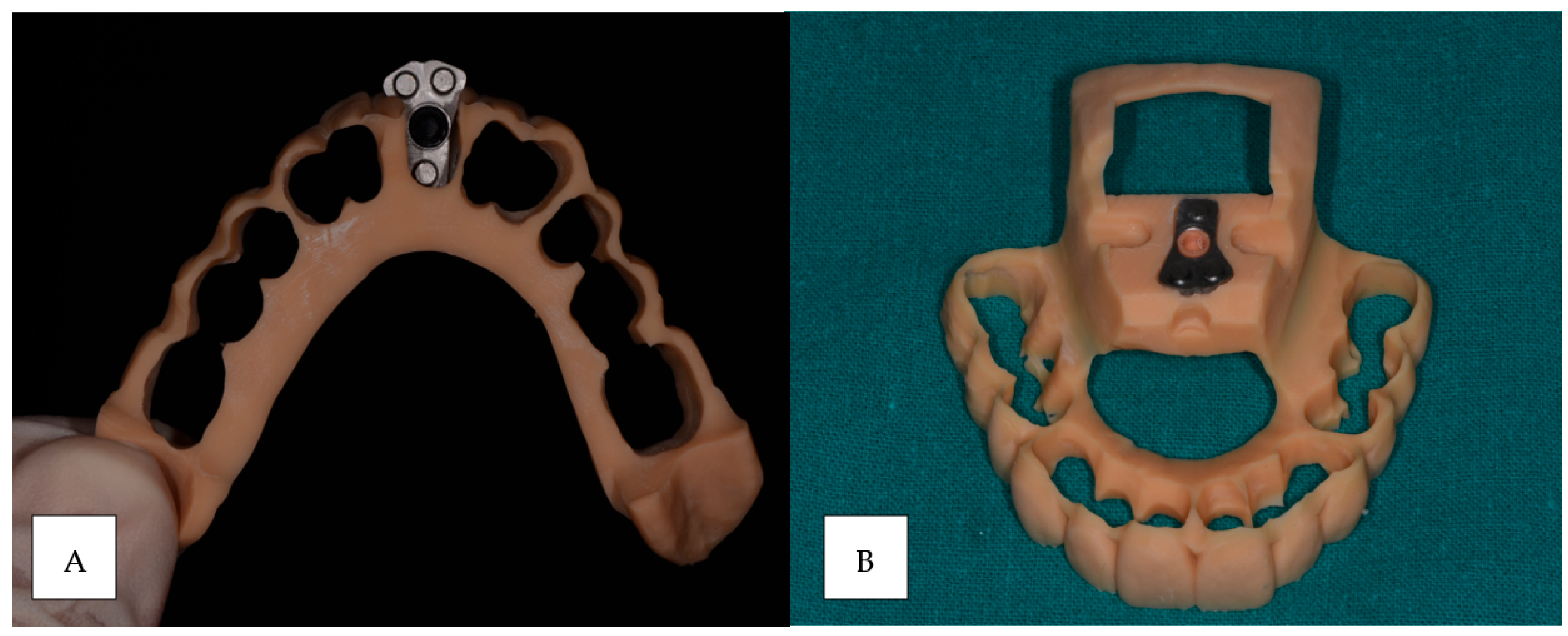
2.4. Laboratory Analysis
2.5. Prosthesis Generation
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Angelis, N.; Pesce, P.; De Lorenzi, M.; Menini, M. Evaluation of Prosthetic Marginal Fit and Implant Survival Rates for Conventional and Digital Workflows in Full-Arch Immediate Loading Rehabilitations: A Retrospective Clinical Study. J. Clin. Med. 2023, 12, 3452. [Google Scholar] [CrossRef] [PubMed]
- Cercadillo-Ibarguren, I.; Sánchez-Torres, A.; Figueiredo, R.; Valmaseda-Castellón, E. Early Complications of Immediate Loading in Edentulous Full-Arch Restorations: A Retrospective Analysis of 88 Cases. Int. J. Oral Maxillofac. Implant. 2017, 32, 1116–1122. [Google Scholar] [CrossRef]
- Mazzoni, A.; Pellegrino, G.; Breccia, C.; Di Bene, P.; Mattoli, R.; Bonifazi, L.; Barausse, C.; Felice, P. A new impression reference technique to simplify the digital workflow for immediate loading zygomatic implant-supported rehabilitation. Int. J. Oral Implantol. 2023, 16, 305–313. [Google Scholar]
- Manfredini, M.; Poli, P.P.; Maiorana, C.; Salina, F.E.; Tandurella, M.; Beretta, M. Computer Aided Full Arch Restoration by Means of One-Piece Implants and Stackable Guide: A Technical Note. Dent. J. 2023, 11, 256. [Google Scholar] [CrossRef] [PubMed]
- Menini, M.; Setti, P.; Pera, F.; Pera, P.; Pesce, P. Accuracy of multi-unit implant impression: Traditional techniques versus a digital procedure. Clin. Oral Investig. 2018, 22, 1253–1262. [Google Scholar] [CrossRef] [PubMed]
- Jung, S.W.; Fan, Y.Q.; Lee, C. Digital Workflow for Edentulous Patients with Implant-Supported Fixed Prostheses: A Fully Digital Technique. Dent. J. 2022, 10, 174. [Google Scholar] [CrossRef]
- Giménez, B.; Özcan, M.; Martínez-Rus, F.; Pradíes, G. Accuracy of a digital impression system based on active wavefront sampling technology for implants considering operator experience, implant angulation, and depth. Clin. Implant. Dent. Relat. Res. 2015, 17 (Suppl. 1), e54–e64. [Google Scholar] [CrossRef]
- Grande, F.; Celeghin, G.; Gallinaro, F.; Mobilio, N.; Catapano, S. Comparison of the accuracy between full-arch digital scans and scannable impression materials: An in vitro study. Minerva Dent. Oral. Sci. 2023, 2, 168–175. [Google Scholar] [CrossRef]
- Chochlidakis, K.; Papaspyridakos, P.; Tsigarida, A.; Romeo, D.; Chen, Y.W.; Natto, Z.; Ercoli, C. Digital Versus Conventional Full-Arch Implant Impressions: A Prospective Study on 16 Edentulous Maxillae. J. Prosthodont. 2020, 29, 281–286. [Google Scholar] [CrossRef]
- Rutkūnas, V.; Gečiauskaitė, A.; Jegelevičius, D.; Vaitiekūnas, M. Accuracy of digital implant impressions with intraoral scanners. A systematic review. Eur. J. Oral Implantol. 2017, 10 (Suppl. 1), 101–120. [Google Scholar]
- Gallo, F.; Zingari, F.; Bolzoni, A.; Barone, S.; Giudice, A. Accuracy of Zygomatic Implant Placement Using a Full Digital Planning and Custom-Made Bone-Supported Guide: A Retrospective Observational Cohort Study. Dent. J. 2023, 2, 123. [Google Scholar] [CrossRef] [PubMed]
- Franchina, A.; Stefanelli, L.V.; Ferri, A.; Pellegrino, G.; Di Carlo, S.; De Angelis, F. A Plaster Cast Contact Scan Method to Assess the Accuracy of Full-Arch Computer-Aided Implant Surgery. Int. J. Oral. Maxillofac. Implant. 2022, 2, 756–762. [Google Scholar] [CrossRef] [PubMed]
- Pellegrino, G.; Basile, F.; Relics, D.; Ferri, A.; Grande, F.; Tarsitano, A.; Marchetti, C. Computer-Aided Rehabilitation Supported by Zygomatic Implants: A Cohort Study Comparing Atrophic with Oncologic Patients after Five Years of Follow-Up. J. Clin. Med. 2020, 9, 3254. [Google Scholar] [CrossRef] [PubMed]
- Lizio, G.; Pellegrino, G.; Corinaldesi, G.; Ferri, A.; Marchetti, C.; Felice, P. Guided bone regeneration using titanium mesh to augment 3-dimensional alveolar defects prior to implant placement. A pilot study. Clin. Oral. Implant. Res. 2022, 2, 607–621. [Google Scholar] [CrossRef]
- Mangano, F.; Luongo, G.; Shibli, J.A.; Tettamanti, L.; Figliuzzi, M.; Mangano, C. Immediate loading of single and full-arch all-on-4 restorations supported by a novel implant design: 1-year results from a prospective cohort study. J. Dent. 2018, 67, 28–34. [Google Scholar]
- Joda, T.; Brägger, U. Time-efficiency analysis of the treatment with monolithic implant crowns in a digital workflow: A randomized controlled trial. Clin. Oral Implant. Res. 2016, 27, 1401–1406. [Google Scholar] [CrossRef]
- Andriessen, F.S.; Bronkhorst, E.M.; Meijer, G.J. Digital versus conventional implant impressions for edentulous patients: Accuracy outcomes. Clin. Oral Implant. Res. 2014, 25, 961–966. [Google Scholar]
- Patel, N.; Bissada, N. The digital workflow: A predictable technique for obtaining accurate impressions and maximizing efficiency. J. Prosthet. Dent. 2020, 123, 590–595. [Google Scholar]
- Bari, V. The Bari technique: A new approach to immediate loading. J. Oral Implantol. 2022, 48, 121–128. [Google Scholar]
- Rossi, M.; Ricci, A.; Ricci, S. Complete digital workflow for mandibular full-arch implant rehabilitation in 3 appointments. Int. J. Prosthodont. 2023, 36, 15–22. [Google Scholar]
- Smith, R.D.; Brown, M. Complete digital workflow for prosthesis prototype fabrication with double digital scanning: Accuracy of fit assessment. J. Prosthodont. 2022, 31, 112–119. [Google Scholar]
- Pette, G.A.; Ganeles, J.; Cranin, A.N. Digital workflow for predictable immediate loading in the mandible by using a shape memory dental implant abutment system: A clinical report. J. Prosthet. Dent. 2020, 123, 45–50. [Google Scholar]
- Turkyilmaz, I.; Suarez, J.C.; Company, A.M. Prosthetic requirements for immediate implant loading: A review. J. Prosthet. Dent. 2018, 119, 698–704. [Google Scholar]
- Holst, S.; Blatz, M.B. Conversion of digital dentures for immediate loading of complete arch implant prostheses. J. Prosthodont. 2021, 30, 325–332. [Google Scholar]
- De Santis, D.; Sinigaglia, S.; Pancera, P.; Faccioni, P.; Luciano, U.; Setti, A.P.; Bursi, P.; Nocini, R.; Nocini, P.F.; Bertossi, D. An overview of guided bone regeneration. J. Biol. Regul. Homeost. Agents, 2019; 33, 49–53. [Google Scholar]
- Pietrabissa, R.; Galli, A.; Casu, G. Update on the accuracy of digital implant impression in 2023: A coordinate-based analysis. Int. J. Prosthodont. 2023, 36, 465–472. [Google Scholar]
- Lee, J.H.; Park, J.S. Digital workflow for full-arch immediate implant placement using a stackable surgical guide fabricated using SLM technology. J. Prosthet. Dent. 2021, 126, 220–228. [Google Scholar]
- Mangano, F.G.; Veronesi, G. Stackable guide in implantology: A technical note. Int. J. Comput. Dent. 2020, 23, 261–267. [Google Scholar]
- Bianchi, A.E.; Fabbro, M. 3D virtual patient—Magnetically retained printed stackable system for implant guided placement: Case report. J. Oral Implantol. 2023, 49, 25–30. [Google Scholar]
- Scherer, M.D.; Lubelski, W. Current knowledge about stackable guides: A scoping review. Int. J. Oral Maxillofac. Implant. 2021, 36, 1217–1226. [Google Scholar]
- Lin, W.S.; Harris, B.T. A novel digital technique for maintaining maxillomandibular relations in fixed prosthetic rehabilitations. J. Prosthet. Dent. 2022, 127, 12–18. [Google Scholar]
- Chochlidakis, K.M.; Ercoli, C. Use of intraoral scanners for full dental arches: Could different strategies or overlapping software affect accuracy? J. Prosthodont. 2021, 30, 497–503. [Google Scholar]
- Pesce, P.; Pera, F.; Setti, P.; Menini, M. Precision and accuracy of a digital impression scanner in full-arch implant rehabilitation. J. Prosthet. Dent. 2018, 128, 276–283. [Google Scholar] [CrossRef] [PubMed]
- Buser, D.; Chen, S. Indications for immediate loading of implants and implant success. Periodontol. 2000 2014, 66, 205–215. [Google Scholar]
- Testori, T.; Taschieri, S. Cone beam computed tomography in implantology: Review of the literature and clinical recommendations. Clin. Oral Implant. Res. 2019, 30, 377–386. [Google Scholar]
- Al-Helal, A.; Rezaei, M. Three-dimensional printing and digital workflows in implant dentistry. J. Prosthet. Dent. 2022, 127, 573–580. [Google Scholar]
- Caputo, A.; Morimoto, S. The use of shape memory dental implant abutments in immediate loading protocols: A systematic review. J. Oral Implantol. 2020, 46, 277–284. [Google Scholar]
- Ferreira, J.J.; Carrara, H.M. Influence of 3D printed stackable guides on the accuracy of implant placement: A clinical and radiographic study. Int. J. Oral Maxillofac. Implant. 2021, 36, 950–957. [Google Scholar]
- Ercoli, C.; Xie, Z. Comparing traditional and digital methods for the fabrication of implant-supported fixed prostheses. J. Prosthet. Dent. 2022, 127, 693–700. [Google Scholar]
- Taşdemir, S.; Kuru, S. Hybrid workflows in implant prosthetics: Benefits and limitations of digital and analog techniques. Clin. Oral Implant. Res. 2023, 34, 12–19. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pellegrino, G.; Anselmo, G.; Barausse, C.; Ratti, S.; Breccia, C.; Mancuso, E.; Giudice, A.; Di Bene, P.; Felice, P. Impression Reference Technique for the Open Flap Digital Workflow in the Immediate Loading Rehabilitation of the Upper and Lower Jaws. Prosthesis 2024, 6, 1479-1490. https://doi.org/10.3390/prosthesis6060107
Pellegrino G, Anselmo G, Barausse C, Ratti S, Breccia C, Mancuso E, Giudice A, Di Bene P, Felice P. Impression Reference Technique for the Open Flap Digital Workflow in the Immediate Loading Rehabilitation of the Upper and Lower Jaws. Prosthesis. 2024; 6(6):1479-1490. https://doi.org/10.3390/prosthesis6060107
Chicago/Turabian StylePellegrino, Gerardo, Gabriele Anselmo, Carlo Barausse, Stefano Ratti, Cristiana Breccia, Edoardo Mancuso, Amerigo Giudice, Pietro Di Bene, and Pietro Felice. 2024. "Impression Reference Technique for the Open Flap Digital Workflow in the Immediate Loading Rehabilitation of the Upper and Lower Jaws" Prosthesis 6, no. 6: 1479-1490. https://doi.org/10.3390/prosthesis6060107
APA StylePellegrino, G., Anselmo, G., Barausse, C., Ratti, S., Breccia, C., Mancuso, E., Giudice, A., Di Bene, P., & Felice, P. (2024). Impression Reference Technique for the Open Flap Digital Workflow in the Immediate Loading Rehabilitation of the Upper and Lower Jaws. Prosthesis, 6(6), 1479-1490. https://doi.org/10.3390/prosthesis6060107








