Infection and Burn Injury
Abstract
:1. Introduction
2. Risk Factors for Infection
3. Pathophysiology of the Burn Wound
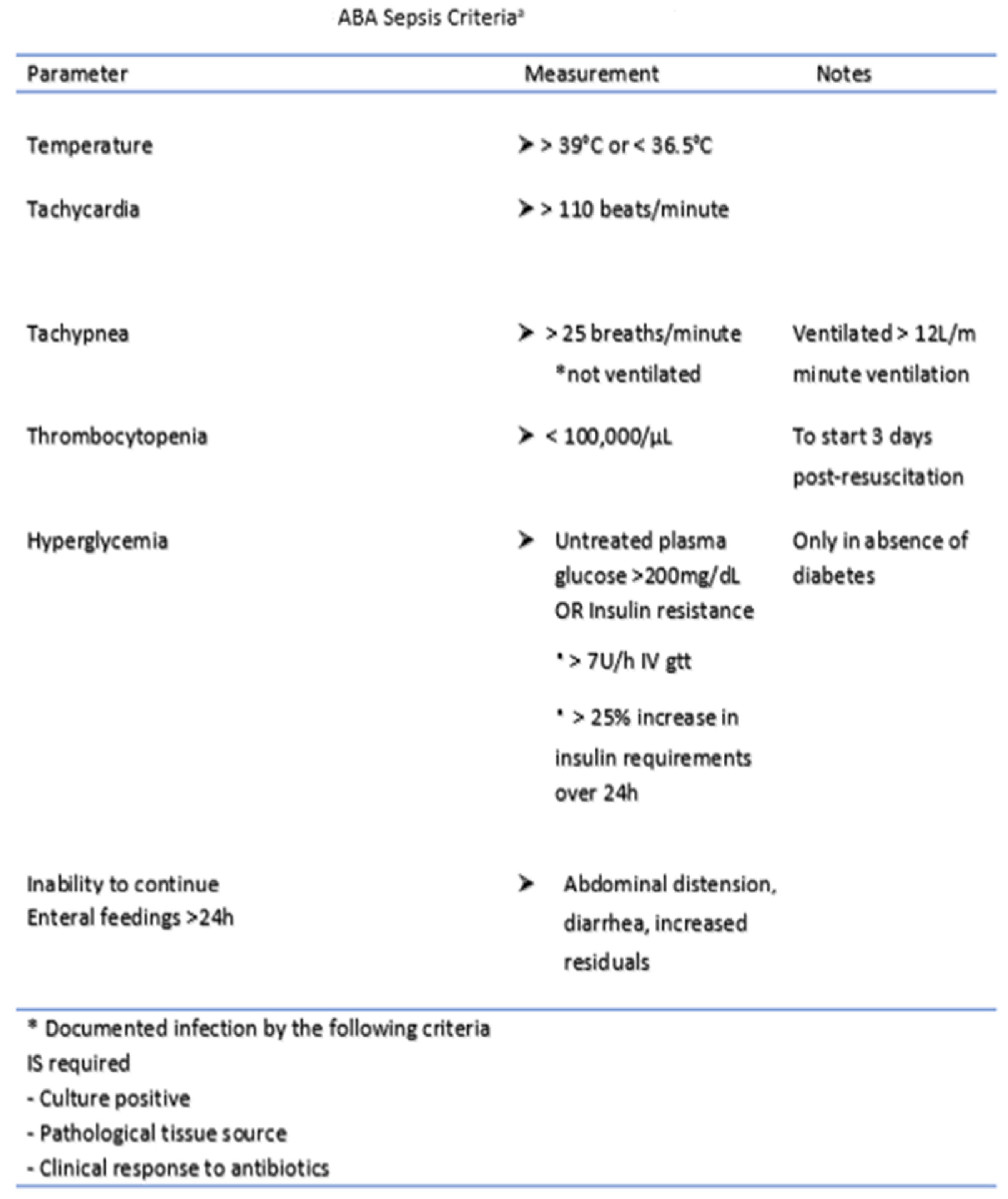
4. Diagnosis of Infection and Sepsis
5. Evolution of the Burn Infection
6. Agents of Infection
6.1. Gram-Positive Bacteria
6.1.1. Staphylococcus
6.1.2. Streptococcus
6.1.3. Enterococcus
6.2. Gram-Negative Bacteria
6.2.1. Pseudomonas
6.2.2. Acinetobacter
6.2.3. Enterobacter
6.3. Fungi and Yeasts
6.4. Viruses
7. Specific Infections in the Burn Patient
7.1. Pneumonia
7.2. Catheter-Associated Urinary Tract Infections (CAUTIs)
7.3. Central Line-Associated Blood Stream Infections (CLABSIs)
8. Treatment and Prevention
8.1. Pharmacokinetics and Pharmacodynamics of Antibiotics
8.2. Phage Therapy
8.3. Minimizing Contamination
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bloemsma, G.C.; Dokter, J.; Boxma, H.; Oen, I.M. Mortality and causes of death in a burn centre. Burns 2008, 34, 1103–1107. [Google Scholar] [CrossRef] [PubMed]
- Gomez, R.; Murray, C.K.; Hospenthal, D.R.; Cancio, L.C.; Renz, E.M.; Holcomb, J.B.; Wade, C.E.; Wolf, S. Causes of mortality by autopsy findings of combat casualties and civilian patients admitted to a burn unit. J. Am. Coll. Surg. 2009, 208, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, M.G.; van Baar, M.E.; Choudhry, M.A.; Chung, K.K.; Gibran, N.S.; Logsetty, S. Burn injury. Nat. Rev. Dis. Primers 2020, 6, 11. (In English) [Google Scholar] [CrossRef] [PubMed]
- Church, D.; Elsayed, S.; Reid, O.; Winston, B.; Lindsay, R. Burn wound infections. Clin. Microbiol. Rev. 2006, 19, 403–434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rowan, M.P.; Cancio, L.C.; Elster, E.A.; Burmeister, D.M.; Rose, L.F.; Natesan, S.; Chan, R.K.; Christy, R.J.; Chung, K.K. Burn wound healing and treatment: Review and advancements. Crit. Care 2015, 19, 243. [Google Scholar] [CrossRef] [Green Version]
- Evers, L.H.; Bhavsar, D.; Mailänder, P. The biology of burn injury. Exp. Dermatol. 2010, 19, 777–783. (In English) [Google Scholar] [CrossRef]
- Lachiewicz, A.M.; Hauck, C.G.; Weber, D.J.; Cairns, B.A.; van Duin, D. Bacterial Infections After Burn Injuries: Impact of Multidrug Resistance. Clin. Infect. Dis. 2017, 65, 2130–2136. [Google Scholar] [CrossRef]
- American Burn Association. National Burn Repository 2019 Update. Report of Data from 2008–2018. Available online: https://sk75w2kudjd3fv2xs2cvymrg-wpengine.netdna-ssl.com/wp-content/uploads/2020/05/2019-ABA-Annual-Report_FINAL.pdf (accessed on 18 October 2021).
- Schultz, L.; Walker, S.A.; Elligsen, M.; Walker, S.E.; Simor, A.; Mubareka, S.; Daneman, N. Identification of predictors of early infection in acute burn patients. Burns 2013, 39, 1355–1366. [Google Scholar] [CrossRef] [PubMed]
- Lopez, O.N.; Cambiaso-Daniel, J.; Branski, L.K.; Norbury, W.B.; Herndon, D.N. Predicting and managing sepsis in burn patients: Current perspectives. Ther. Clin. Risk Manag. 2017, 13, 1107–1117. (In English) [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vinaik, R.; Barayan, D.; Shahrokhi, S.; Jeschke, M.G. Management and prevention of drug resistant infections in burn patients. Expert Rev. Anti. Infect. Ther. 2019, 17, 607–619. [Google Scholar] [CrossRef] [PubMed]
- Jones, S.W.; Williams, F.N.; Cairns, B.A.; Cartotto, R. Inhalation Injury: Pathophysiology, Diagnosis, and Treatment. Clin. Plast. Surg. 2017, 44, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Nielson, C.B.; Duethman, N.C.; Howard, J.M.; Moncure, M.; Wood, J.G. Burns: Pathophysiology of Systemic Complications and Current Management. J. Burn. Care Res. 2017, 38, e469–e481. [Google Scholar] [CrossRef] [PubMed]
- Zhang, P.; Zou, B.; Liou, Y.C.; Huang, C. The pathogenesis and diagnosis of sepsis post burn injury. Burn. Trauma 2021, 9, tkaa047. [Google Scholar] [CrossRef] [PubMed]
- Tiwari, V.K. Burn wound: How it differs from other wounds? Indian J. Plast. Surg. 2012, 45, 364–373. [Google Scholar] [CrossRef] [PubMed]
- Shakespeare, P. Burn wound healing and skin substitutes. Burns 2001, 27, 517–522. (In English) [Google Scholar] [CrossRef]
- Dvorak, J.E.; Ladhani, H.A.; Claridge, J.A. Review of Sepsis in Burn Patients in 2020. Surg. Infect. 2021, 22, 37–43. [Google Scholar] [CrossRef]
- Dastagir, K.; Krezdorn, N.; Bingoel, A.S.; Mett, T.R.; Radtke, C.; Jokuszies, A.; Vogt, P.M. Application of critical care scores in severely burned patients. J. Burn Care Res. 2021, 42, 1176–1180. [Google Scholar] [CrossRef]
- Torres, M.J.M.; Peterson, J.M.; Wolf, S.E. Detection of Infection and Sepsis in Burns. Surg. Infect. 2021, 22, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Tejiram, S.; Shupp, J.W. Innovations in Infection Prevention and Treatment. Surg. Infect. 2021, 22, 12–19. [Google Scholar] [CrossRef]
- Hogan, B.K.; Wolf, S.; Hospenthal, D.R.; D’Avignon, L.C.; Chung, K.K.; Yun, H.C.; Mann, E.A.; Murray, C.K. Correlation of American Burn Association sepsis criteria with the presence of bacteremia in burned patients admitted to the intensive care unit. J. Burn Care Res. 2012, 33, 371–378. [Google Scholar] [CrossRef]
- Mann-Salinas, E.A.; Baun, M.M.; Meininger, J.C.; Murray, C.K.; Aden, J.K.; Wolf, S.; Wade, C.E. Novel predictors of sepsis outperform the American Burn Association sepsis criteria in the burn intensive care unit patient. J. Burn Care Res. 2013, 34, 31–43. [Google Scholar] [CrossRef] [PubMed]
- Barati, M.; Alinejad, F.; Bahar, M.A.; Tabrisi, M.S.; Shamshiri, A.R.; Bodouhi, N.-O.; Karimi, H. Comparison of WBC, ESR, CRP and PCT serum levels in septic and non-septic burn cases. Burns 2008, 34, 770–774. [Google Scholar] [CrossRef]
- Farhan, N.; Jeffery, S. Diagnosing Burn Wounds Infection: The Practice Gap & Advances with MolecuLight Bacterial Imaging. Diagnostics 2021, 11, 268. [Google Scholar] [CrossRef]
- Ren, H.; Li, Y.; Han, C.; Hu, H. Serum procalcitonin as a diagnostic biomarker for sepsis in burned patients: A meta-analysis. Burns 2015, 41, 502–509. [Google Scholar] [CrossRef] [PubMed]
- Gille, J.; Jocovic, J.; Kremer, T.; Sablotzki, A. The predictive role of Interleukin 6 in burn patients with positive blood cultures. Int. J. Burn. Trauma 2021, 11, 123–130. Available online: https://www.ncbi.nlm.nih.gov/pubmed/34094705 (accessed on 8 November 2021).
- Niggemann, P.; Rittirsch, D.; Buehler, P.; Schweizer, R.; Giovanoli, P.; Reding, T.; Graf, R.; Plock, J.; Klein, H. Incidence and Time Point of Sepsis Detection as Related to Different Sepsis Definitions in Severely Burned Patients and Their Accompanying Time Course of Pro-Inflammatory Biomarkers. J. Pers. Med. 2021, 11, 701. [Google Scholar] [CrossRef] [PubMed]
- Moins-Teisserenc, H.; Cordeiro, D.J.; Audigier, V.; Ressaire, Q.; Benyamina, M.; Lambert, J.; Maki, G.; Homyrda, L.; Toubert, A.; Legrand, M. Severe Altered Immune Status After Burn Injury Is Associated With Bacterial Infection and Septic Shock. Front. Immunol. 2021, 12, 586195. [Google Scholar] [CrossRef]
- Miller, R.R., III; Lopansri, B.K.; Burke, J.P.; Levy, M.; Opal, S.; Rothman, R.E.; D’Alessio, F.R.; Sidhaye, V.K.; Aggarwal, N.R.; Balk, R.; et al. Validation of a Host Response Assay, SeptiCyte LAB, for Discriminating Sepsis from Systemic Inflammatory Response Syndrome in the ICU. Am. J. Respir. Crit. Care Med. 2018, 198, 903–913. [Google Scholar] [CrossRef]
- Sweeney, T.E.; Khatri, P. Comprehensive Validation of the FAIM3:PLAC8 Ratio in Time-matched Public Gene Expression Data. Am. J. Respir. Crit. Care Med. 2015, 192, 1260–1261. [Google Scholar] [CrossRef] [Green Version]
- Gunsolus, I.L.; Sweeney, T.E.; Liesenfeld, O.; Ledeboer, N.A. Diagnosing and Managing Sepsis by Probing the Host Response to Infection: Advances, Opportunities, and Challenges. J. Clin. Microbiol. 2019, 57. [Google Scholar] [CrossRef] [Green Version]
- Maslove, D.M.; Shapira, T.; Tyryshkin, K.; Veldhoen, R.A.; Marshall, J.C.; Muscedere, J. Validation of diagnostic gene sets to identify critically ill patients with sepsis. J. Crit. Care 2018, 49, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Grenga, L.; Pible, O.; Armengaud, J. Pathogen proteotyping: A rapidly developing application of mass spectrometry to address clinical concerns. Clin. Mass Spectrom. 2019, 14 Pt A, 9–17. [Google Scholar] [CrossRef]
- Schubert, S.; Kostrzewa, M. MALDI-TOF MS in the Microbiology Laboratory: Current Trends. Curr. Issues Mol. Biol. 2017, 23, 17–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dingle, T.C.; Butler-Wu, S.M. Maldi-tof mass spectrometry for microorganism identification. Clin. Lab. Med. 2013, 33, 589–609. [Google Scholar] [CrossRef] [PubMed]
- Ladhani, H.A.; Yowler, C.J.; Claridge, J.A. Burn Wound Colonization, Infection, and Sepsis. Surg. Infect. 2021, 22, 44–48. (In English) [Google Scholar] [CrossRef]
- Norbury, W.; Herndon, D.N.; Tanksley, J.; Jeschke, M.G.; Finnerty, C.C. Infection in Burns. Surg. Infect. 2016, 17, 250–255. (In English) [Google Scholar] [CrossRef] [Green Version]
- Stanojcic, M.; Vinaik, R.; Jeschke, M.G. Status and Challenges of Predicting and Diagnosing Sepsis in Burn Patients. Surg. Infect. 2018, 19, 168–175. [Google Scholar] [CrossRef]
- Hidalgo, F.; Mas, D.; Rubio, M.; Garcia-Hierro, P. Infections in critically ill burn patients. Med. Intensiv. 2016, 40, 179–185. [Google Scholar] [CrossRef]
- Moussa, A.; Lo, C.H.; Cleland, H. Burn wound excision within 24 h: A 9-year review. Burns 2021, 47, 1300–1307. [Google Scholar] [CrossRef]
- Reese, A.D.; Keyloun, J.W.; Garg, G.; McLawhorn, M.M.; Moffatt, L.T.; Travis, T.E.; Johnson, L.S.; Shupp, J.W. Compounded Cerium Nitrate-Silver Sulfadiazine Cream is Safe and Effective for the Treatment of Burn Wounds: A Burn Center’s Four-Year Experience. J. Burn Care Res. 2021. [Google Scholar] [CrossRef]
- Cambiaso-Daniel, J.; Boukovalas, S.; Bitz, G.H.; Branski, L.K.; Herndon, D.N.; Culnan, D.M. Topical Antimicrobials in Burn Care: Part 1-Topical Antiseptics. Ann. Plast. Surg. 2018. [Google Scholar] [CrossRef]
- Azzopardi, E.A.; Azzopardi, E.; Camilleri, L.; Villapalos, J.; Boyce, D.E.; Dziewulski, P.; Dickson, W.A.; Whitaker, I. Gram negative wound infection in hospitalised adult burn patients--systematic review and metanalysis. PLoS ONE 2014, 9, e95042. (In English) [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, B.R. Infection in patients with severe burns: Causes and prevention thereof. Infect. Dis. Clin. North Am. 2007, 21, 745–759. (In English) [Google Scholar] [CrossRef] [PubMed]
- Ellithy, M.; Mitwally, H.; Saad, M.; Mathias, R.; Shaukat, A.; Elzeer, H.; Koya, S.H.; Mahmood, Z.; Gazwi, K. Mortality incidence among critically ill burn patients infected with multidrug-resistant organisms: A retrospective cohort study. Scars Burn. Health 2021, 7, 20595131211015133. [Google Scholar] [CrossRef]
- Kooistra-Smid, M.; Nieuwenhuis, M.; van Belkum, A.; Verbrugh, H. The role of nasal carriage in Staphylococcus aureus burn wound colonization. FEMS Immunol. Med Microbiol. 2009, 57, 1–13. (In English) [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jenul, C.; Horswill, A.R. Regulation of Staphylococcus aureus Virulence. Microbiol. Spectr. 2019, 7. (In English) [Google Scholar] [CrossRef]
- Miller, M.B.; Bassler, B.L. Quorum sensing in bacteria. Annu. Rev. Microbiol. 2001, 55, 165–199. [Google Scholar] [CrossRef] [Green Version]
- Nisar, S.; Kirkpatrick, L.D.; Shupp, J.W. Bacterial Virulence Factors and Their Contribution to Pathophysiology after Thermal Injury. Surg. Infect. 2021, 22, 69–76. (In English) [Google Scholar] [CrossRef]
- Shannon, B.A.; McCormick, J.K.; Schlievert, P.M. Toxins and Superantigens of Group A Streptococci. Microbiol. Spectr. 2019, 7. (In English) [Google Scholar] [CrossRef]
- Spaulding, A.R.; Salgado-Pabón, W.; Kohler, P.L.; Horswill, A.R.; Leung, D.Y.; Schlievert, P.M. Staphylococcal and streptococcal superantigen exotoxins. Clin. Microbiol. Rev. 2013, 26, 422–447. (In English) [Google Scholar] [CrossRef] [Green Version]
- Cong, Y.; Yang, S.; Rao, X. Vancomycin resistant Staphylococcus aureus infections: A review of case updating and clinical features. J. Adv. Res. 2020, 21, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Naimi, H.M.; André, C.; Bes, M.; Tristan, A.; Gustave, C.-A.; Vandenesch, F.; Nazari, Q.A.; Laurent, F.; Dupieux, C. Antibiotic resistance profile and molecular characterization of Staphylococcus aureus strains isolated in hospitals in Kabul, Afghanistan. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 1029–1038. [Google Scholar] [CrossRef] [PubMed]
- Navarre, W.W.; Schneewind, O. Surface proteins of gram-positive bacteria and mechanisms of their targeting to the cell wall envelope. Microbiol. Mol. Biol. Rev. 1999, 63, 174–229. (In English) [Google Scholar] [CrossRef] [Green Version]
- Kleyman, R.; Cupril-Nilson, S.; Robinson, K.; Thakore, S.; Haq, F.; Chen, L.; Oyesanmi, O.; Browning, K.; Pino, J.; Mhaskar, R. Does the removal of contact precautions for MRSA and VRE infected patients change health care-associated infection rate?: A systematic review and meta-analysis. Am. J. Infect. Control 2021, 49, 784–791. (In English) [Google Scholar] [CrossRef] [PubMed]
- Cheah, A.L.; Spelman, T.; Liew, D.; Peel, T.; Howden, B.; Grayson, M.; Nation, R.; Kong, D. Enterococcal bacteraemia: Factors influencing mortality, length of stay and costs of hospitalization. Clin. Microbiol. Infect. 2013, 19, E181–E189. (In English) [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulcahy, L.R.; Isabella, V.M.; Lewis, K. Pseudomonas aeruginosa biofilms in disease. Microb. Ecol. 2014, 68, 1–12. (In English) [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lago, K.; Decker, C.F.; Chung, K.K.; Blyth, D. Difficult to Treat Infections in the Burn Patient. Surg. Infect. 2021, 22, 95–102. (In English) [Google Scholar] [CrossRef] [PubMed]
- Haghi, F.; Zeighami, H.; Monazami, A.; Toutouchi, F.; Nazaralian, S.; Naderi, G. Diversity of virulence genes in multidrug resistant Pseudomonas aeruginosa isolated from burn wound infections. Microb. Pathog. 2018, 115, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Lima, W.G.; Alves, G.C.S.; Sanches, C.; Fernandes, S.O.A.; de Paiva, M.C. Carbapenem-resistant Acinetobacter baumannii in patients with burn injury: A systematic review and meta-analysis. Burns 2019, 45, 1495–1508. (In English) [Google Scholar] [CrossRef]
- Ramirez, M.S.; Bonomo, R.A.; Tolmasky, M.E. Carbapenemases: Transforming Acinetobacter baumannii into a Yet More Dangerous Menace. Biomolecules 2020, 10, 720. (In English) [Google Scholar] [CrossRef] [PubMed]
- Azzopardi, E.A.; Boyce, D.E.; Thomas, D.W.; Dickson, W.A. Colistin in burn intensive care: Back to the future? Burns 2013, 39, 7–15. [Google Scholar] [CrossRef]
- Trottier, V.; Segura, P.G.; Namias, N.; King, D.; Pizano, L.R.; Schulman, C.I. Outcomes of Acinetobacter baumannii infection in critically ill burned patients. J. Burn Care Res. 2007, 28, 248–254. [Google Scholar] [CrossRef] [Green Version]
- Davin-Regli, A.; Lavigne, J.P.; Pagès, J.M. Enterobacter spp.: Update on Taxonomy, Clinical Aspects, and Emerging Antimicrobial Resistance. Clin. Microbiol. Rev. 2019, 32, e00002-19. (In English) [Google Scholar] [CrossRef]
- Palackic, A.; Popp, D.; Tapking, C.; Houschyar, K.S.; Branski, L.K. Fungal Infections in Burn Patients. Surg. Infect. 2021, 22, 83–87. (In English) [Google Scholar] [CrossRef] [PubMed]
- Tissot, F.; Lamoth, F.; Hauser, P.M.; Orasch, C.; Flückiger, U.; Siegemund, M.; Zimmerli, S.; Calandra, T.; Bille, J.; Eggimann, P.; et al. Beta-glucan antigenemia anticipates diagnosis of blood culture-negative intraabdominal candidiasis. Am. J. Respir. Crit. Care Med. 2013, 188, 1100–1109. [Google Scholar] [CrossRef]
- Odabasi, Z.; Mattiuzzi, G.N.; Estey, E.; Kantarjian, H.M.; Saeki, F.; Ridge, R.J.; Ketchum, P.A.; Finkelman, M.A.; Rex, J.; Ostrosky-Zeichner, L. Beta-D-glucan as a diagnostic adjunct for invasive fungal infections: Validation, cutoff development, and performance in patients with acute myelogenous leukemia and myelodysplastic syndrome. Clin. Infect. Dis. 2004, 39, 199–205. [Google Scholar] [CrossRef]
- Shupp, J.W.; Petraitiene, R.; Jaskille, A.D.; Pavlovich, A.R.; Matt, S.E.; Nguyen, D.T.; Kath, M.A.; Jeng, J.C.; Jordan, M.H.; Finkelman, M.; et al. Early serum (1-->3)-beta-D-glucan levels in patients with burn injury. Mycoses 2012, 55, 224–227. [Google Scholar] [CrossRef] [PubMed]
- Kiley, J.L.; Chung, K.K.; Blyth, D.M. Viral Infections in Burns. Surg. Infect. 2021, 22, 88–94. (In English) [Google Scholar] [CrossRef]
- Sen, S.; Johnston, C.; Greenhalgh, D.; Palmieri, T. Ventilator-Associated Pneumonia Prevention Bundle Significantly Reduces the Risk of Ventilator-Associated Pneumonia in Critically Ill Burn Patients. J. Burn Care Res. 2016, 37, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Carr, J.A.; Phillips, B.D.; Bowling, W.M. The utility of bronchoscopy after inhalation injury complicated by pneumonia in burn patients: Results from the National Burn Repository. J. Burn Care Res. 2009, 30, 967–974. [Google Scholar] [CrossRef]
- U.S. Centers for Disease Control and Prevention. The National Healthcare Safety Network (NHSN) Manual: NHSN 2015 Toolkit and Guidance for External Validation; Division of Healthcare Quality Promotion, National Center for Emerging and Zoonotic Infectious Diseases: Atlanta, GA, USA. Available online: https://www.cdc.gov/nhsn/pdfs/validation/archive/2015-nhsn-ev-guidance-p.pdf (accessed on 18 October 2021).
- Greenhalgh, D.G.; Saffle, J.R.; Holmes, J.H.; Gamelli, R.L.; Palmieri, T.L.; Horton, J.W.; Tompkins, R.G.; Traber, D.L.; Mozingo, D.W.; Deitch, E.A.; et al. American Burn Association consensus conference to define sepsis and infection in burns. J. Burn Care Res. 2007, 28, 776–790. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gould, C.V.; Umscheid, C.A.; Agarwal, R.K.; Kuntz, G.; Pegues, D.A. Healthcare Infection Control Practices Advisory, Guideline for prevention of catheter-associated urinary tract infections 2009. Infect. Control Hosp. Epidemiol. 2010, 31, 319–326. [Google Scholar] [CrossRef] [Green Version]
- Tao, L.; Zhou, J.; Gong, Y.; Liu, W.; Long, T.; Huang, X.; Luo, G.; Peng, Y.; Wu, J. Risk factors for central line-associated bloodstream infection in patients with major burns and the efficacy of the topical application of mupirocin at the central venous catheter exit site. Burns 2015, 41, 1831–1838. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Mara, M.S.; Reed, N.L.; Palmieri, T.L.; Greenhalgh, D.G. Central venous catheter infections in burn patients with scheduled catheter exchange and replacement. J. Surg. Res. 2007, 142, 341–350. [Google Scholar] [CrossRef] [PubMed]
- Goetz, A.M.; Wagener, M.M.; Miller, J.M.; Muder, R.R. Risk of infection due to central venous catheters: Effect of site of placement and catheter type. Infect. Control Hosp. Epidemiol. 1998, 19, 842–845. [Google Scholar] [CrossRef] [PubMed]
- Roham, M.; Momeni, M.; Saberi, M.; Kheirkhah, R.; Jafarian, A.; Rahbar, H. Epidemiologic analysis of central vein catheter infection in burn patients. Iran. J. Microbiol. 2017, 9, 271–276. Available online: https://www.ncbi.nlm.nih.gov/pubmed/29296271 (accessed on 18 October 2021).
- Deshpande, K.S.; Hatem, C.; Ulrich, H.L.; Currie, B.P.; Aldrich, T.K.; Bryan-Brown, C.W.; Kvetan, V. The incidence of infectious complications of central venous catheters at the subclavian, internal jugular, and femoral sites in an intensive care unit population. Crit. Care Med. 2005, 33, 13–20. [Google Scholar] [CrossRef]
- Pruskowski, K.A. Pharmacokinetics and Pharmacodynamics of Antimicrobial Agents in Burn Patients. Surg. Infect. 2021, 22, 77–82. [Google Scholar] [CrossRef]
- Robben, P.M.; Ayalew, M.D.; Chung, K.K.; Ressner, R.A. Multi-Drug-Resistant Organisms in Burn Infections. Surg. Infect. 2021, 22, 103–112. [Google Scholar] [CrossRef]
- Putra, O.N.; Saputro, I.D.; Hidayatullah, A.Y.N. A retrospective surveillance of the prophylactic antibiotics for debridement surgery in burn patients. Int. J. Burn. Trauma 2021, 11, 96–104. Available online: https://www.ncbi.nlm.nih.gov/pubmed/34094701 (accessed on 1 November 2021).
- Corcione, S.; Lupia, T.; de Rosa, F.G.; Host, M. Microbiota Interaction Study Group of the European Society of Clinical, and D. Infectious, Microbiome in the setting of burn patients: Implications for infections and clinical outcomes. Burn. Trauma 2020, 8, tkaa033. [Google Scholar] [CrossRef]
- Hill, D.M.; Guido, A.; Sultan-Ali, I.; Arif, F.; Velamuri, S.R. A non-inferiority study comparing efficacy of preoperative prophylactic antibiotics for preventing infectious complications in patients with less severe burns. Burns 2021, 47, 67–71. [Google Scholar] [CrossRef]
- Heffernan, A.J.; Lim, S.M.S.; Lipman, J.; Roberts, J.A. A personalised approach to antibiotic pharmacokinetics and pharmacodynamics in critically ill patients. Anaesth. Crit. Care Pain Med. 2021, 40, 100970. [Google Scholar] [CrossRef]
- Udy, A.A.; Roberts, J.A.; Lipman, J.; Blot, S. The effects of major burn related pathophysiological changes on the pharmacokinetics and pharmacodynamics of drug use: An appraisal utilizing antibiotics. Adv. Drug Deliv. Rev. 2018, 123, 65–74. [Google Scholar] [CrossRef]
- Dulhunty, J.M.; Roberts, J.; Davis, J.; Webb, S.A.R.; Bellomo, R.; Gomersall, C.; Shirwadkar, C.; Eastwood, G.M.; Myburgh, J.; Paterson, D.; et al. Continuous infusion of beta-lactam antibiotics in severe sepsis: A multicenter double-blind, randomized controlled trial. Clin. Infect. Dis. 2013, 56, 236–244. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fournier, A.; Eggimann, P.; Pantet, O.; Pagani, J.L.; Dupuis-Lozeron, E.; Pannatier, A.; Sadeghipour, F.; Voirol, P.; Que, Y.-A. Impact of Real-Time Therapeutic Drug Monitoring on the Prescription of Antibiotics in Burn Patients Requiring Admission to the Intensive Care Unit. Antimicrob. Agents Chemother. 2018, 62, e01818-17. [Google Scholar] [CrossRef] [Green Version]
- Kortright, K.E.; Chan, B.K.; Koff, J.L.; Turner, P.E. Phage Therapy: A Renewed Approach to Combat Antibiotic-Resistant Bacteria. Cell Host Microbe 2019, 25, 219–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, D.M.; Koskella, B.; Lin, H.C. Phage therapy: An alternative to antibiotics in the age of multi-drug resistance. World J. Gastrointest. Pharmacol. Ther. 2017, 8, 162–173. [Google Scholar] [CrossRef] [PubMed]
- Altamirano, F.L.G.; Barr, J.J. Phage Therapy in the Postantibiotic Era. Clin. Microbiol. Rev. 2019, 32, e00066-18. [Google Scholar] [CrossRef] [Green Version]
- Chadha, P.; Katare, O.P.; Chhibber, S. In vivo efficacy of single phage versus phage cocktail in resolving burn wound infection in BALB/c mice. Microb. Pathog. 2016, 99, 68–77. [Google Scholar] [CrossRef]
- Steele, A.; Stacey, H.J.; de Soir, S.; Jones, J.D. The Safety and Efficacy of Phage Therapy for Superficial Bacterial Infections: A Systematic Review. Antibiotics 2020, 9, 754. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, M.M.; Pina-Vaz, C.; Rodrigues, A. The role of phage therapy in burn wound infection management: Advantages and pitfalls. J. Burn Care Res. 2021. [Google Scholar] [CrossRef] [PubMed]
- Valente, L.; Prazak, J.; Que, Y.A.; Cameron, D.R. Progress and Pitfalls of Bacteriophage Therapy in Critical Care: A Concise Definitive Review. Crit. Care Explor. 2021, 3, e0351. [Google Scholar] [CrossRef] [PubMed]
- Phillips, L.G.; Heggers, J.P.; Robson, M.C.; Boertman, J.A.; Meltzer, T.; Smith, D.J., Jr. The effect of endogenous skin bacteria on burn wound infection. Ann. Plast. Surg. 1989, 23, 35–38. [Google Scholar] [CrossRef]
- Rafla, K.; Tredget, E.E. Infection control in the burn unit. Burns 2011, 37, 5–15. [Google Scholar] [CrossRef] [PubMed]
- Weber, D.J.; Rutala, W.A.; Sickbert-Bennett, E.E.; Kanamori, H.; Anderson, D.; Program, C.D.C.P.E. Continuous room decontamination technologies. Am. J. Infect. Control 2019, 47S, A72–A78. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, E.; Mehrabadi, J.F.; Nourani, M.; Namini, Y.N.; Mohammadi, S.; Esmaeili, D.; Abbasi, A. Evaluation of cold atmospheric-pressure plasma against burn wound infections and gene silencing. Iran. J. Microbiol. 2021, 13, 544–552. [Google Scholar] [CrossRef]
- Niedzwiedz, I.; Wasko, A.; Pawlat, J.; Polak-Berecka, M. The State of Research on Antimicrobial Activity of Cold Plasma. Pol. J. Microbiol. 2019, 68, 153–164. [Google Scholar] [CrossRef] [Green Version]
- Stratmann, B.; Costea, T.-C.; Nolte, C.; Hiller, J.; Schmidt, J.; Reindel, J.; Masur, K.; Motz, W.; Timm, J.; Kerner, W.; et al. Effect of Cold Atmospheric Plasma Therapy vs Standard Therapy Placebo on Wound Healing in Patients With Diabetic Foot Ulcers: A Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e2010411. [Google Scholar] [CrossRef]
- Angarano, V.; Smet, C.; Akkermans, S.; Watt, C.; Chieffi, A.; van Impe, J.F.M. Visible Light as an Antimicrobial Strategy for Inactivation of Pseudomonas fluorescens and Staphylococcus epidermidis Biofilms. Antibiotics 2020, 9, 171. [Google Scholar] [CrossRef] [Green Version]
- Deeter, L.; Seaton, M.; Carrougher, G.J.; McMullen, K.; Mandell, S.P.; Amtmann, D.; Gibran, N.S. Hospital-acquired complications alter quality of life in adult burn survivors: Report from a burn model system. Burns 2019, 45, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Stahmeyer, J.T.; Lutze, B.; von Lengerke, T.; Chaberny, I.F.; Krauth, C. Hand hygiene in intensive care units: A matter of time? J. Hosp. Infect. 2017, 95, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Weber, D.J.; Rutala, W.A. Self-disinfecting surfaces: Review of current methodologies and future prospects. Am. J. Infect. Control 2013, 41 (Suppl. 5), S31–S35. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kelly, E.J.; Oliver, M.A.; Carney, B.C.; Shupp, J.W. Infection and Burn Injury. Eur. Burn J. 2022, 3, 165-179. https://doi.org/10.3390/ebj3010014
Kelly EJ, Oliver MA, Carney BC, Shupp JW. Infection and Burn Injury. European Burn Journal. 2022; 3(1):165-179. https://doi.org/10.3390/ebj3010014
Chicago/Turabian StyleKelly, Edward J., Mary A. Oliver, Bonnie C. Carney, and Jeffrey W. Shupp. 2022. "Infection and Burn Injury" European Burn Journal 3, no. 1: 165-179. https://doi.org/10.3390/ebj3010014
APA StyleKelly, E. J., Oliver, M. A., Carney, B. C., & Shupp, J. W. (2022). Infection and Burn Injury. European Burn Journal, 3(1), 165-179. https://doi.org/10.3390/ebj3010014




