The Impact of COVID-19 on Burns: A Brazilian Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting, Design and Data Collection
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Rabi, F.A.; Al Zoubi, M.S.; Kasasbeh, G.A.; Salameh, D.M.; Al-Nasser, A.D. SARS-CoV-2 and Coronavirus Disease 2019: What We Know So Far. Pathogens 2020, 9, 231. [Google Scholar] [CrossRef] [PubMed]
- Farroha, A. Effects of COVID-19 pandemic on burns epidemiology. Burns 2020, 46, 1466. [Google Scholar] [CrossRef] [PubMed]
- Leão, C.E.G.; Andrade, E.S.D.; Fabrini, D.S.; Oliveira, R.A.D.; Machado, G.L.B.; Gontijo, L.C. Epidemiologia das queimaduras no estado de Minas Gerais. Rev. Bras. Cir. Plást. 2011, 26, 573–577. [Google Scholar]
- Cazumbá, M.L.B.; Buda, A.M.; Bittencourt, M.M.; Moura, C.; Braga, P.; Bowder, A.N.; Corlew, D.S.; Botelho, F.; Magalhães, L.; Pompermaier, L. The Use of Alcohol as a Disinfectant During the Pandemic and Flame Burns: A Brazilian Study. J. Burn Care Res. 2022, 43, 753–754. [Google Scholar] [CrossRef] [PubMed]
- The largest cities in Brazil. 2020. Available online: https://www.statista.com/statistics/259227/largest-cities-in-brazil/ (accessed on 20 December 2022).
- Hospital João XXIII. Available online: https://www.fhemig.mg.gov.br/atendimento/complexo-hospitalar-de-urgencia/hospital-joao-xxiii (accessed on 20 December 2022).
- R Core Team. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2012; ISBN 3-900051-07-0. Available online: https://www.r-project.org/ (accessed on 20 December 2022).
- Patel, D.D.; Rosenberg, L.; Rosenberg, M.; Leal, J.; Andersen, C.R.; Foncerrada, G.; Lee, J.O.; Jimenez, C.J.; Branski, L.; Meyer, W.J.; et al. The epidemiology of burns in young children from Mexico treated at a U.S. hospital. Burns 2016, 42, 1825–1830. [Google Scholar] [CrossRef] [PubMed]
- D’Asta, F.; Choong, J.; Thomas, C.; Adamson, J.; Wilson, Y.; Wilson, D.; Moiemen, N.; Farroha, A. Paediatric burns epidemiology during COVID-19 pandemic and ‘stay home’. Burns 2020, 46, 1471–1472. [Google Scholar] [CrossRef] [PubMed]
- Peck, M.D. Epidemiology of burns throughout the World. Part II: Intentional burns in adults. Burns 2012, 38, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Davé, D.R.; Nagarjan, N.; Canner, J.K.; Kushner, A.L.; Stewart, B.T. Rethinking burns for low & middle-income countries: Differing patterns of burn epidemiology, care seeking behavior, and outcomes across four countries. Burns 2018, 44, 1228–1234. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, R.; Sato, Y.; Matsumura, K.; Sasaki, J. Characteristics of burn injury during COVID-19 pandemic in Tokyo: A descriptive study. Burns 2021, 5, 40–45. [Google Scholar] [CrossRef] [PubMed]
- Charvillat, O.; Plancq, M.; Haraux, E.; Gouron, R.; Klein, C. Epidemiological analysis of burn injuries in children during the first COVID-19 lockdown, and a comparison with the previous five years. Ann. Chir. Plast. Esthétique 2021, 66, 285–290. [Google Scholar] [CrossRef] [PubMed]
- Rogers, A.D.; Cartotto, R. The Impact of COVID-19 on Burn Care at a Major Regional Burn Center. J. Burn Care Res. 2020, 42, 110–111. [Google Scholar] [CrossRef] [PubMed]
- Kruchevsky, D.; Arraf, M.; Levanon, S.; Capucha, T.; Ramon, Y.; Ullmann, Y. Trends in Burn Injuries in Northern Israel during the COVID-19 Lockdown. J. Burn Care Res. 2021, 42, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Salomão, K. A Corrida do álcool em Gel: Como o Produto foi da Escassez ao Excesso. 2020. Available online: https://exame.com/negocios/depois-de-corrida-por-alcool-em-gel-estoque-estabilizou-e-ha-ate-sobra/ (accessed on 20 April 2022).
- Laura, P.; José, A.; Nikki, A.; Khaled, A.; Barret, J.; Jeffery, C.; Shobha, C.; Jack, C.S.; Scott, C.; Nadia, D.; et al. Impact of COVID-19 on global burn care. Burns 2022, 48, 1301–1310. [Google Scholar] [CrossRef] [PubMed]
- Moraes, P.S.D.; Ferrari, R.A.P.; Sant’Anna, F.L.; Raniero, J.T.M.W.; Lima, L.D.S.; Santos, T.D.F.M.; Tacla, M.T.G.M. Perfil das internações de crianças em um centro de tratamento para queimados. Enferm. Bras. 2014, 16, 598–603. [Google Scholar] [CrossRef][Green Version]
- European Burns Association. European Burns Practice Guidelines for Burn Care, 4th ed.; European Burns Association: ′s-Hertogenbosch, The Netherlands, 2017. [Google Scholar]
- ISBI Practice Guidelines Committee; Steering Subcommittee; Advisory Subcommittee. ISBI Practice Guidelines for Burn Care. Burns 2016, 42, 953–1021. [Google Scholar] [CrossRef] [PubMed]


| All Patients (n = 781) | Control Group (n = 402) | Study Group (n = 379) | p | |
|---|---|---|---|---|
| Sex | 0.767 ^ | |||
| Female | 307 (40%) | 156 (39%) | 151 (40%) | |
| Male | 474 (60%) | 246 (61%) | 228 (60%) | |
| Age (years) * | 32 (9–48) | 32.5 (13.75–48) | 32 (6.25–48) | 0.342 # |
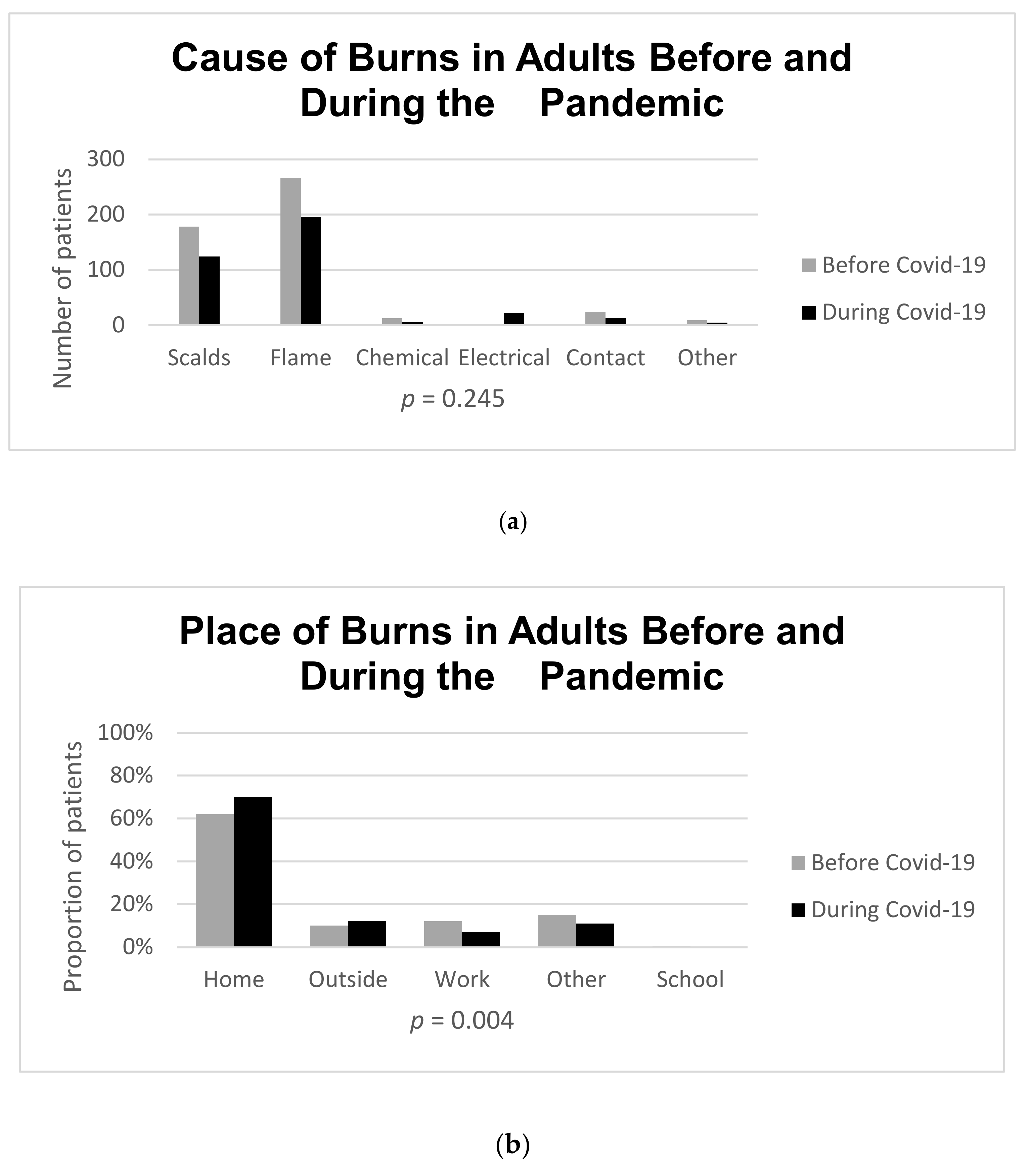
| Place of injury | 0.002 † | |||
| Outside | 81 (11%) | 38 (5%) | 43 (12%) | |
| Work | 69 (9%) | 44 (12%) | 25 (7%) | |
| School | 3 (0.4%) | 3 (0.4%) | 0 (0%) | |
| Home | 478 (65%) | 218 (29%) | 260 (35%) | |
| Other | 103 (14%) | 62 (8%) | 41 (5%) | |
| Cause of burn | 0.245 † | |||
| Scalds | 258 (33%) | 134 (34%) | 124 (33%) | |
| Flame | 397 (51%) | 202 (50%) | 195 (52%) | |
| Chemical | 23 (3%) | 7 (2%) | 16 (4%) | |
| Electrical | 56 (7%) | 34 (8%) | 22 (6%) | |
| Contact | 31 (4%) | 18 (4%) | 13 (4%) | |
| Other | 10 (2%) | 5 (2%) | 5 (1%) | |
| Mechanism of burn | 0.037 † | |||
| Accident | 603 (86%) | 341 (86%) | 322 (85%) | |
| Caused by other | 53 (6%) | 23 (5%) | 30 (8%) | |
| Self-inflicted | 58 (7%) | 31 (7%) | 27 (7%) | |
| Other | 7 (1%) | 7 (1%) | 0 | |
| Transferred from another city | 371 (46%) | 191 (50%) | 147 (40%) | 0.003 ^ |
| Time to admission the at the João XXIII | ||||
| Hospital (days) * | 1 (0–4) | 1 (0–4) | 1 (0–3.5) | 0.828 # |
| TBSA% * | 15 (8–28) | 15 (9–30) | 13.5 (7–25) | 0.038 # |
| Location of the Burn | 0.928 ^ | |||
| Head and neck | 470 (51%) 571 (62%) | 284 (53%) 345 (64%) | 186 (49%) 226 (60%) | |
| Core (Thorax, Abdomen, and Back) | ||||
| Arms | 577 (63%) | 345 (64%) | 232 (61%) | |
| Hands | 188 (21%) | 96 (18%) | 92 (24%) | |
| Genitalia | 86 (9%) | 50 (9%) | 36 (9%) | |
| Legs | 427 (47%) | 257 (48%) | 170 (45%) | |
| Feet | 107 (12%) | 60 (11%) | 47 (12%) | |
| Presence of FTB | 312 (40%) | 164 (41%) | 148 (37%) | 0.415 ^ |
| In-patient status | 770 (95%) | 376 (95%) | 370 (97%) | 0.149 ^ |
| Presence of inhalation injury | 117 (15%) | 59(15%) | 58 (16%) | 0.812 ^ |
| Need for mechanical ventilation | 142 (16%) | 86 (16%) | 56 (15%) | 0.360 ^ |
| In-hospital mortality | 72 (8%) | 39 (7%) | 33 (9%) | 0.696 ^ |
| Length of stay (days) * | 23 (15-41) | 24 (15-45.75) | 21 (14-35) | 0.014 # |
| All Pediatric Burns (n = 277) | Control Group (n = 147) | Study Group (n = 130) | p | |
|---|---|---|---|---|
| Burn mechanism | 1 † | |||
| Accident | 271 (97%) | 144 (97%) | 127 (97%) | |
| Caused by other | 4 (2%) | 2 (2%) | 2 (1%) | |
| Self-inflicted | 2 (1%) | 1 (1%) | 1 (1%) | |
| Burn cause | 0.10 † | |||
| Scald | 172 (62%) | 92 (62%) | 80 (62%) | |
| Flame | 67 (24%) | 36 (24%) | 31 (24%) | |
| Chemical | 4 (0%) | 2 (0%) | 2 (0%) | |
| Electrical | 15 (0.5%) | 8 (0.5%) | 7 (0.5%) | |
| Contact | 14 (0.5%) | 8 (0.5%) | 6 (0.5%) | |
| Other | 3 (0%) | 1 (0%) | 2 (0%) | |
| Place of injury | 0.16 † | |||
| Outside | 17 (1%) | 10 (0.7%) | 7 (0.7%) | |
| Work | 2 (0.1%) | 0 (0%) | 2 (0%) | |
| School | 3 (0.1%) | 3 (0.2%) | 0 (0%) | |
| Home | 225 (81%) | 111 (75%) | 113 (86%) | |
| Other | 17(1%) | 11 (0.7%) | 6 (0.7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moura, C.; Bittencourt, M.; Cazumbá, M.L.; Buda, A.; Bowder, A.; Corlew, D.S.; Filho, F.M.B.; Barboza, L.; Pompermaier, L. The Impact of COVID-19 on Burns: A Brazilian Study. Eur. Burn J. 2023, 4, 1-8. https://doi.org/10.3390/ebj4010001
Moura C, Bittencourt M, Cazumbá ML, Buda A, Bowder A, Corlew DS, Filho FMB, Barboza L, Pompermaier L. The Impact of COVID-19 on Burns: A Brazilian Study. European Burn Journal. 2023; 4(1):1-8. https://doi.org/10.3390/ebj4010001
Chicago/Turabian StyleMoura, Carolina, Marcela Bittencourt, Maria Luíza Cazumbá, Alexandra Buda, Alexis Bowder, Daniel Scott Corlew, Fábio Mendes Botelho Filho, Lucas Barboza, and Laura Pompermaier. 2023. "The Impact of COVID-19 on Burns: A Brazilian Study" European Burn Journal 4, no. 1: 1-8. https://doi.org/10.3390/ebj4010001
APA StyleMoura, C., Bittencourt, M., Cazumbá, M. L., Buda, A., Bowder, A., Corlew, D. S., Filho, F. M. B., Barboza, L., & Pompermaier, L. (2023). The Impact of COVID-19 on Burns: A Brazilian Study. European Burn Journal, 4(1), 1-8. https://doi.org/10.3390/ebj4010001








