Factors Associated with Self-Reported Voice Change in the Hospitalized Burn Population: A Burn Model System National Database Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Burn Model System National Database
2.2. Demographic and Clinical Characteristics
2.3. Voice Outcomes
2.4. Data Analysis
3. Results
3.1. Study Sample and Comparison of Characteristics between Groups
3.2. Self-Reported Voice Outcomes over Time
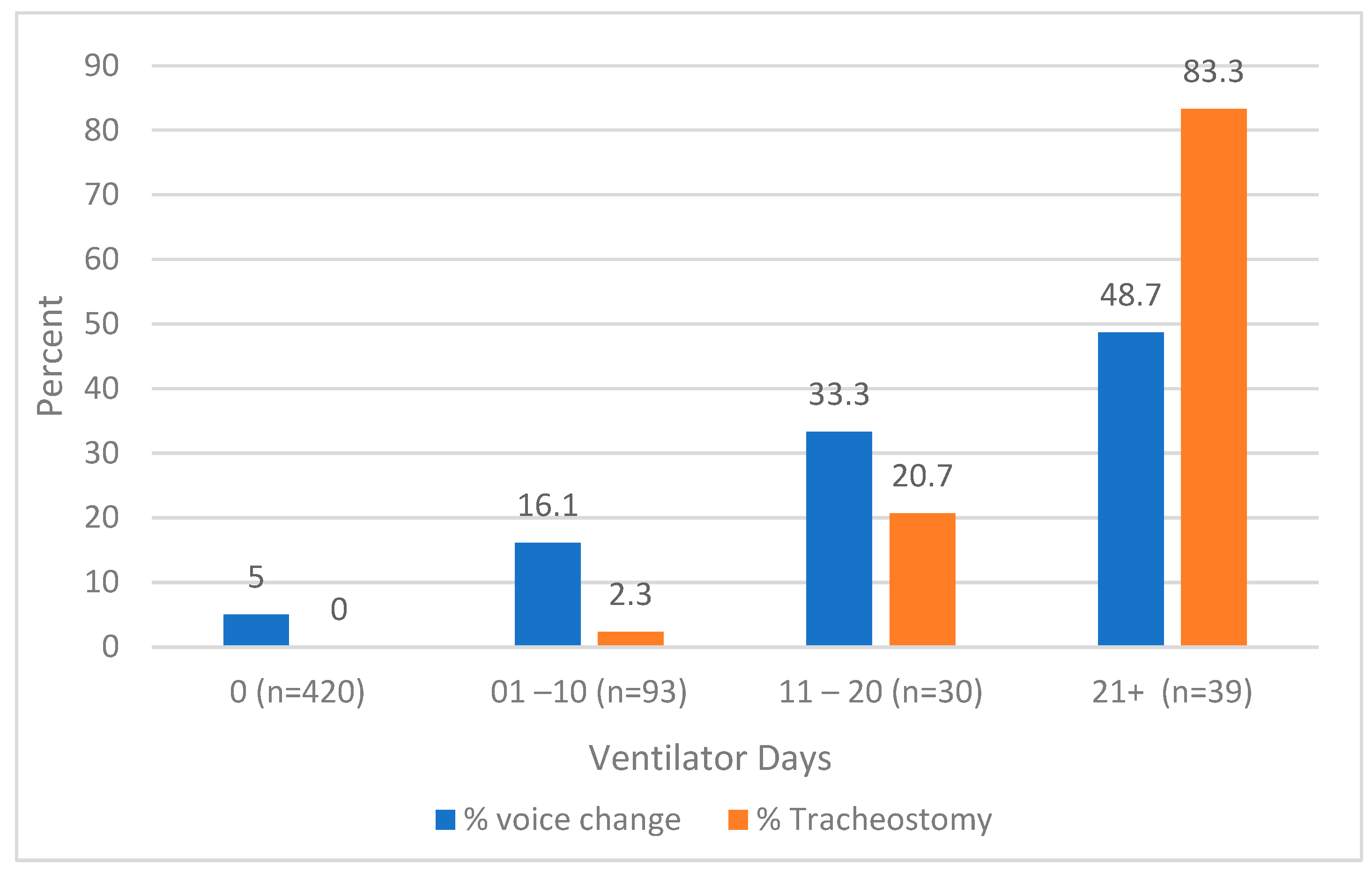
3.3. Association of Voice Changes with Ventilator Days and Tracheostomy
3.4. Factors Associated with Voice Change
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Holavanahalli, R.; Quayle, B.K. Model Systems Knowledge Translation Center. Social Interaction after Burn Injury. Model Systems Knowledge Translation Center. Available online: https://msktc.org/sites/default/files/2022-06/SI-After-Burn-508_0.pdf (accessed on 25 May 2023).
- Tiwari, M.; Tiwari, M. Voice—How humans communicate? J. Nat. Sci. Biol. Med. 2012, 3, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Jeschke, M.G.; van Baar, M.E.; Choudhry, M.A.; Chung, K.K.; Gibran, N.S.; Logsetty, S. Burn injury. Nat. Rev. Dis. Primers. 2020, 6, 11. [Google Scholar] [CrossRef] [PubMed]
- American Burn Association. 2016 National Burn Repository. Report of Data from 2006–2015 [Internet]; American Burn Association: Chicago, IL, USA, 2017; Available online: https://ameriburn.org/who-we-are/media/burn-incidence-fact-sheet/ (accessed on 1 June 2023).
- Abouzeid, C.A.; Wolfe, A.E.; Ni, P.; Carrougher, G.J.M.; Gibran, N.S.; Hammond, F.M.; Holavanahalli, R.; McMullen, K.A.; Roaten, K.; Suman, O.; et al. Are burns a chronic condition? Examining patient reported outcomes up to 20 years after burn injury—A Burn Model System National Database investigation. J. Trauma Acute Care Surg. 2022, 92, 1066–1074. [Google Scholar] [CrossRef] [PubMed]
- Kelter, B.M.; Holavanahalli, R.; Suman, O.E.; Ryan, C.M.; Schneider, J.C. Recognizing the long-term sequelae of burns as a chronic medical condition. Burns 2020, 46, 493–496. [Google Scholar] [CrossRef] [PubMed]
- Clayton, N.A.; Ward, E.C.; Rumbach, A.F.; Cross, R.R.; Kol, M.R.; Maitz, P.K. Influence of Inhalation Injury on Incidence, Clinical Profile and Recovery Pattern of Dysphagia Following Burn Injury. Dysphagia 2020, 35, 968–977. [Google Scholar] [CrossRef] [PubMed]
- Casper, J.K.; Clark, W.R.; Kelley, R.T.; Colton, R.H. Laryngeal and phonatory status after burn/inhalation injury: A long-term follow-up study. J. Burn Care Rehabil. 2002, 23, 235–243. [Google Scholar] [CrossRef]
- Clayton, N.; Kennedy, P.; Maitz, P. The severe burns patient with tracheostomy: Implications for management of dysphagia, dysphonia and laryngotracheal pathology. Burns 2010, 36, 850–855. [Google Scholar] [CrossRef] [PubMed]
- Kelly, E.; Hirschwald, J.; Clemens, J.; Regan, J. Persistent Features of Laryngeal Injury Following Endotracheal Intubation: A Systematic Review. Dysphagia 2023, 38, 1333–1341. [Google Scholar] [CrossRef] [PubMed]
- Andriolo, B.N.; Andriolo, R.B.; Saconato, H.; Atallah, Á.N.; Valente, O. Early versus late tracheostomy for critically ill patients. Cochrane Database Syst. Rev. 2015, 1, CD007271. [Google Scholar] [CrossRef]
- Khashaba, H.A.; Al-Fadhli, A.N.; Al-Tarrah, K.S.; Wilson, Y.T.; Moiemen, N. Epidemiology and outcome of burns at the Saud Al Babtain Burns, Plastic Surgery and Reconstructive Center, Kuwait: Our experience over five years (from 2006 to 2010). Ann. Burn. Fire Disasters 2012, 25, 178–187. [Google Scholar]
- Mlcak, R.P.; Suman, O.E.; Herndon, D.N. Respiratory management of inhalation injury. Burns 2007, 33, 2–13. [Google Scholar] [CrossRef] [PubMed]
- Carney, B.C.; Bailey, J.K.; Powell, H.M.; Supp, D.M.; Travis, T.E. Scar Management and Dyschromia: A Summary Report from the 2021 American Burn Association State of the Science Meeting. J. Burn Care Res. 2023, 44, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Moshrefi, S.; Sheckter, C.C.; Shepard, K.; Pereira, C.; Davis, D.J.; Karanas, Y.; Rochlin, D.H. Preventing Unnecessary Intubations: A 5-Year Regional Burn Center Experience Using Flexible Fiberoptic Laryngoscopy for Airway Evaluation in Patients with Suspected Inhalation or Airway Injury. J. Burn Care Res. 2019, 40, 341–346. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, T.L.; Caruso, D.M.; Foster, K.N.; Cairns, B.A.; Peck, M.D.; Gamelli, R.L. Effect of inhalation injury on fluid resuscitation requirements after thermal injury. Crit. Care 2009, 13, R47. [Google Scholar]
- American Burn Association. Burn Resuscitation Guidelines. 2008. Available online: https://ameriburn.org/wp-content/uploads/2017/05/burn_resuscitation.pdf (accessed on 22 December 2023).
- Brodsky, M.B.; Levy, M.J.; Jedlanek, E.; Pandian, V.P.; Blackford, B.M.; Price, C.M.; Cole, G.D.; Hillel, A.T.; Best, S.R.; Akst, L.M. Laryngeal Injury and Upper Airway Symptoms After Oral Endotracheal Intubation with Mechanical Ventilation during Critical Care: A Systematic Review. Crit. Care Med. 2018, 46, 2010–2017. [Google Scholar] [CrossRef] [PubMed]
- Gaissert, H.A.; Lofgren, R.H.; Grillo, H.C. Upper airway compromise after inhalation injury. Complex strictures of the larynx and trachea and their management. Ann. Surg. 1993, 218, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Roy, N.; Merrill, R.M.; Gray, S.D.; Smith, E.M. Voice disorders in the general population: Prevalence, risk factors, and occupational impact. Laryngoscope 2005, 115, 1988–1995. [Google Scholar] [CrossRef]
- Tracy, L.F.; Shehan, J.; Grillone, G.A. Upper Airway Burn Injury. Oper. Tech. Otolaryngol.-Head Neck Surg. 2020, 31, 295–300. [Google Scholar] [CrossRef]
- Goverman, J.; Mathews, K.; Holavanahalli, R.K.; Vardanian, A.; Herndon, D.N.; Meyer, W.J.; Kowalske, K.; Fauerbach, J.; Gibran, N.S.; Carrougher, G.J.; et al. The National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Twenty Years of Contributions to Clinical Service and Research. J. Burn Care Res. 2017, 38, e240–e253. [Google Scholar] [CrossRef]
- Amtmann, D.; McMullen, K.; Bamer, A.; Fauerbach, J.A.; Gibran, N.S.; Herndon, D.; Schneider, J.C.; Kowalske, K.; Holavanahalli, R.; Miller, A.C. National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System: Review of Program and Database. Arch. Phys. Med. Rehabil. 2020, 101, S5–S15. [Google Scholar] [CrossRef]
- Ewing, J.A. Detecting Alcoholism: The CAGE Questionnaire. JAMA 1984, 252, 1905–1907. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.L.; Rounds, L.A. Conjoint screening questionnaires for alcohol and other drug abuse: Criterion validity in a primary care practice. Wis. Med. J. 1995, 94, 135–140. [Google Scholar] [PubMed]
- Reid, A.; Ha, J.F. Inhalational injury and the larynx: A review. Burns 2019, 45, 1266–1274. [Google Scholar] [CrossRef] [PubMed]
- Behlau, M.; Madazio, G.; Oliveira, G.; Pontes, P. Evaluation of vocal abuse: Interdisciplinary analysis of 107 cases. J. Voice 2008, 22, 682–689. [Google Scholar]
- Hamdan, A.L. The effects of drugs on the larynx. J. Voice 2016, 30, 461.e13–461.e19. [Google Scholar]
- Bamer, A.M.; McMullen, K.; Gibran, N.; Holavanahalli, R.; Schneider, J.C.; Carrougher, G.J.; Wiechman, S.; Wolfe, A.; Amtmann, D. Factors Associated with Attrition of Adult Participants in a Longitudinal Database: A National Institute on Disability, Independent Living, and Rehabilitation Research Burn Model System Study. J. Burn Care Res. 2020, 41, 270–279. [Google Scholar] [CrossRef]
- American College of Chest Physicians. Guidelines for the management of adult patients with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Chest 2005, 128, 221–235. [Google Scholar]
- Beck, I.; Tapking, C.; Haug, V.; Nolte, S.; Böcker, A.; Stoppe, C.; Kneser, U.; Hirche, C.; Hundeshagen, G. Short- and long term hyposmia, hypogeusia, dysphagia and dysphonia after facial burn injury—A prospective matched cohort study. Burns 2023, 49, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Neighbors, C.; Song, S.A. Dysphonia. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK565881/ (accessed on 22 December 2023).
- Smith, E.; Taylor, M.; Mendoza, M.; Barkmeier, J.; Lemke, J.; Hoffman, H. Spasmodic dysphonia and vocal fold paralysis: Outcomes of voice problems on work-related functioning. J. Voice 1998, 12, 223–232. [Google Scholar] [CrossRef]
- Rouhani, M.J.; Clunie, G.; Thong, G.; Lovell, L.; Roe, J.; Ashcroft, M.; Holroyd, A.; Sandhu, G.; Al Yaghchi, C. A Prospective Study of Voice, Swallow, and Airway Outcomes Following Tracheostomy for COVID-19. Laryngoscope 2021, 131, E1918–E1925. [Google Scholar] [CrossRef]
- Zhen, E.; Misso, D.; Rea, S.; Vijayasekaran, S.; Fear, M.; Wood, F. Long-Term Laryngotracheal Complications After Inhalation Injury: A Scoping Review. J. Burn Care Res. 2023, 44, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Plummer, A.L.; Gracey, D.R. Consensus conference on artificial airways in patients receiving mechanical ventilation. Chest 1989, 96, 178–180. [Google Scholar] [CrossRef] [PubMed]
- Khammas, A.H.; Dawood, M.R. Timing of Tracheostomy in Intensive Care Unit Patients. Int. Arch. Otorhinolaryngol. 2018, 22, 437–442. [Google Scholar] [CrossRef]
- Lezotte, D.C.; Hills, R.A.; Heltshe, S.L.; Holavanahalli, R.K.; Fauerbach, J.A.; Blakeney, P.; Klein, M.B.; Engrav, L.H. Assets and liabilities of the Burn Model System data model: A comparison with the National Burn Registry. Arch. Phys. Med. Rehabil. 2007, 88 (Suppl. S2), S7–S17. [Google Scholar] [CrossRef] [PubMed]
| Variable | With Voice Change (n = 65) | Without Voice Change (n = 517) | p-Value |
|---|---|---|---|
| Age, mean years (SD) | 48.2 (16.3) | 46.8 (16.2) | 0.59 |
| Male, n (%) | 40 (61.5) | 359 (69.4) | 0.20 |
| Hispanic/Latino ethnicity, n (%) | 16 (25.0) | 100 (20.1) | 0.36 |
| Race, n (%) | |||
| White | 55 (87.3) | 416 (83.7) | 0.21 |
| African American/Black | 3 (4.8) | 48 (9.7) | |
| Other 1 | 5 (7.9) | 33 (6.6) | |
| Education, n greater than high school (%) | 25 (42.4) | 254 (56.3) | 0.04 |
| Burn Model System site, n (%) | |||
| Site A | 20 (30.8) | 188 (36.4) | 0.614 |
| Site B | 21 (32.3) | 174 (33.7) | |
| Site D | 24 (36.9) | 152 (29.4) | |
| Employed at time of injury, n (%) | 36 (75.0) | 333 (80.6) | 0.36 |
| Burn size, mean percent TBSA (SD) | 31.1 (24.2) | 15.5 (16.8) | <0.001 * |
| Ventilator days, mean (SD) 2 | 25.9 (25.6) | 12.9 (21.2) | <0.001 * |
| Mechanical ventilation, n (%) | 43 (67.2) | 98 (19.7) | <0.001 * |
| Alcohol misuse history, n (%) | 6 (10.0) | 64 (13.4) | 0.46 |
| Drug misuse history, n (%) | 4 (6.8) | 20 (4.3) | 0.39 |
| Burn etiology, n (%) | |||
| Fire/Flame | 54 (83.1) | 272 (52.7) | <0.001 * |
| Other 3 | 11 (16.9) | 244 (47.3) | |
| Inhalation injury, n (%) | 21 (32.8) | 45 (8.7) | <0.001 * |
| Tracheostomy, n (%) | 18 (29.0) | 20 (4.3) | <0.001 * |
| Outpatient speech services at 12 months, n (%) | 5(7.7) | 5 (1.0) | <0.001 * |
| Head/neck burn, n (%) | 51 (78.5) | 234 (45.4) | <0.001 * |
| Multiple trips to the operating room, n (%) 4 | 50 (76.9) | 252 (48.7) | <0.001 * |
| Time Point | Sample Size, n | Change in Voice, n (%) | Missing Data |
|---|---|---|---|
| Discharge | 898 | 147 (16.4) | 174 |
| 6 months | 670 | 78 (11.6) | 501 |
| 12 months | 582 | 65 (11.2) | 516 |
| 24 months | 499 | 56 (11.2) | 463 |
| 60 months | 157 | 20 (12.7) | 554 |
| Participants Who Responded to “Change in Voice” Item at Discharge and Follow-Up, n (Follow-Up Time Point) | Voice Change at Discharge, n (%) | Voice Change at Follow-Up, n (%) |
|---|---|---|
| 589 (6 months) | 93 (15.8) | 67 (11.4) |
| 481 (12 months) | 82 (17.1) | 56 (11.6) |
| 338 (24 months) | 63 (18.6) | 36 (10.7) |
| 51 (60 months) | 10 (19.6) | 9 (17.7) |
| Variable | Odds Ratio | Robust SE | Z | p-Value | 95% Cl |
|---|---|---|---|---|---|
| Age | 1.02 | 0.01 | 1.93 | 0.054 | 0.99–1.04 |
| Female | 1.87 | 0.61 | 1.92 | 0.055 | 0.99–3.54 |
| Burn Model System site | |||||
| Site B | 1.15 | 0.47 | 0.36 | 0.722 | 0.53–2.50 |
| Site D | 1.34 | 0.54 | 0.72 | 0.472 | 0.61–2.94 |
| Burn size, TBSA | 1.00 | 0.01 | 0.3 | 0.767 | 0.98–1.02 |
| Etiology of burn | |||||
| High-voltage electrical | 0.49 | 0.39 | −0.9 | 0.367 | 0.10–2.31 |
| Other 1 | 0.46 | 0.19 | −1.83 | 0.067 | 0.20–1.06 |
| Inhalation injury | 1.01 | 0.41 | 0.03 | 0.976 | 0.45–2.30 |
| Tracheostomy | 2.84 | 1.34 | 2.21 | 0.027 | 1.13–7.14 |
| Ventilator | 4.31 | 1.71 | 3.69 | <0.001 | 1.98–9.37 |
| Head/neck burn | 0.60 | 0.23 | −1.35 | 0.177 | 0.28–1.26 |
| Multiple operations | 1.01 | 0.4 | 0.04 | 0.971 | 0.47–2.18 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chacon, K.L.; Santos, E.; McMullen, K.; Shepler, L.J.; Tierney-Hendricks, C.; Clark, A.T.; Akarichi, C.; Yenikomshian, H.A.; Orton, C.M.; Ryan, C.M.; et al. Factors Associated with Self-Reported Voice Change in the Hospitalized Burn Population: A Burn Model System National Database Study. Eur. Burn J. 2024, 5, 116-125. https://doi.org/10.3390/ebj5020010
Chacon KL, Santos E, McMullen K, Shepler LJ, Tierney-Hendricks C, Clark AT, Akarichi C, Yenikomshian HA, Orton CM, Ryan CM, et al. Factors Associated with Self-Reported Voice Change in the Hospitalized Burn Population: A Burn Model System National Database Study. European Burn Journal. 2024; 5(2):116-125. https://doi.org/10.3390/ebj5020010
Chicago/Turabian StyleChacon, Kaitlyn L., Edward Santos, Kara McMullen, Lauren J. Shepler, Carla Tierney-Hendricks, Audra T. Clark, Chiaka Akarichi, Haig A. Yenikomshian, Caitlin M. Orton, Colleen M. Ryan, and et al. 2024. "Factors Associated with Self-Reported Voice Change in the Hospitalized Burn Population: A Burn Model System National Database Study" European Burn Journal 5, no. 2: 116-125. https://doi.org/10.3390/ebj5020010
APA StyleChacon, K. L., Santos, E., McMullen, K., Shepler, L. J., Tierney-Hendricks, C., Clark, A. T., Akarichi, C., Yenikomshian, H. A., Orton, C. M., Ryan, C. M., & Schneider, J. C. (2024). Factors Associated with Self-Reported Voice Change in the Hospitalized Burn Population: A Burn Model System National Database Study. European Burn Journal, 5(2), 116-125. https://doi.org/10.3390/ebj5020010








