Genetic Disorders of Calcium and Phosphorus Metabolism
Abstract
1. Physiology
1.1. Calcium-Phosphorus Metabolism
1.2. Regulation by Vitamin D
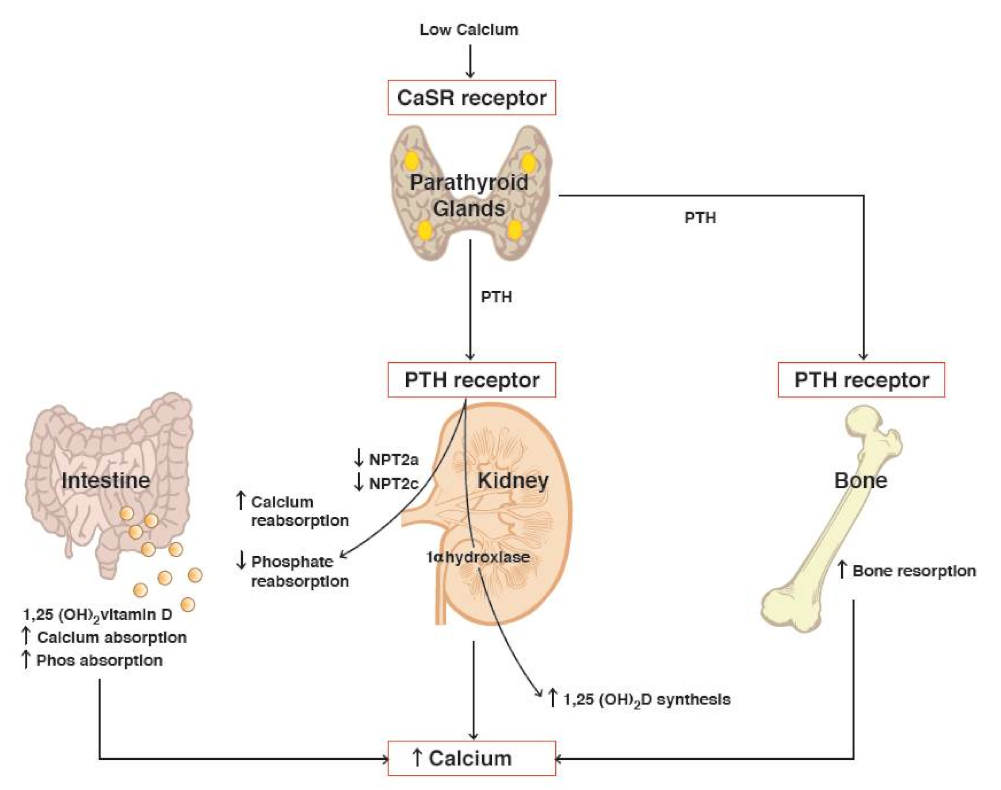
1.3. Regulation by PTH
1.4. Regulation by FGF23
2. Pathophysiology of Calcium/Phosphorus Disorders
2.1. Vitamin D Pathway Mutations-Hypercalcemia
Idiopathic Infantile Hypercalcemia (IIH)
2.2. Vitamin D Pathway Mutations–Hypocalcemia
- Vitamin D-dependent rickets type 1A is due to failure to synthesize calcitriol due to a defect in CYP27B1 encoding 1α-hydroxylase [16].
- Vitamin D–dependent rickets type 2 is the result of an impaired vitamin D receptor VDR gene (VDDR2A), or post-receptor errors (hormone response element-binding protein HNRNPC gene), that interferes with vitamin D receptor (VDDR2B) function [35]. As the defect is at the receptor level, vitamin D25(OH) levels are normal and calcitriol levels are markedly elevated. Alopecia is found in VDDR2A [34,35].
2.3. Parathyroid Hormone-Hyperparathyroidism
- A.
- Familial Hypocalciuric Hypercalcemia and Neonatal Severe Hyperparathyroidism
- FHH type 2 is due to loss-of-function mutations of GNA11 (guanine nucleotide-binding protein, alpha-11). It encodes the downstream G-protein signal of CaSR to intracellular signal transduction pathways, and its inactivation leads to hypercalcemia [46].
- FHH type 3 is due to loss-of-function mutations in AP2S1 (adaptor related protein complex 2, sigma1 subunit). Additionally, inactivating mutations lead to defective adaptor-related protein complex 2 interactions with β-arrestin (ARRB1), with a consequent defect in endocytosis of the CaSR from the cell surface. The clinical presentation comprises of hypercalcemia, low bone mineralization, and impaired cognition [46].
- Neonatal severe hyperparathyroidism (NSHPT) is a result of inactivating mutations of CaSR, however, it has a more severe presentation than FHH [47]. The NSHPT condition results from the inheritance of two abnormal CaSR alleles in either the homozygous or the compound heterozygous state, leading to severe hypercalcemia at birth. An autosomal recessive condition, it is a potentially lethal form of hyperparathyroidism that presents with life-threatening signs of acute hypercalcemia such as short QT, dysrhythmias, respiratory distress, and chronic hypercalcemia as demineralization and fractures [38,39]. Though hypercalcemia can lead to short QT intervals on ECG, arrhythmias are rare [20,37]. The time of initial presentation of NSHPT depends on the degree of hypercalcemia and varies from the first few days to several months of age [20].
- B.
- Isolated Non-Syndromic—Mutations on CDC73, CaSR, GNA11, and AP2S1 Genes Familial Isolated Hyperparathyroidism
- Type 2, known as hyperparathyroidism jaw-tumour syndrome (HPT-JT), presents as severe malignant ossifying fibromas of the maxilla and/or mandible, renal tumours, uterine tumours and an increased risk of parathyroid carcinoma [38,48]. Interestingly, these tumours are not the brown tumours typically associated with hyperparathyroidism. Both subtypes are caused by germline mutations in CDC73 on chromosome 1q31.2, encoding parafibromin, a protein intrinsic to the cell division cycle. Penetrance of this mutation is 80% [38,49].
- C.
- Multiple Endocrine Neoplasia (MEN) syndromes
- MEN1 comprises a constellation of tumours in specific locations: hyperplasia of the parathyroid glands, tumours of the adenohypophysis (prolactinoma), and pancreatic tumours (gastrinoma, insulinoma, etc) [35,41,43]. MEN1 is due to an inactivating mutation of the MEN1 or menin tumour suppressor gene, located on chromosome 11q13.1 [41]. The syndrome MEN1 rarely presents before the age of 10, and usually occurs in the second decade of life [41,50]. Hyperparathyroidism is the initial presentation [20].
- MEN2A results from activating germline mutations of RET proto-oncogene, encoding a transmembrane receptor tyrosine kinase responsible for cell growth, differentiation, and survival [2,50]. Specifically, it is associated with parathyroid adenoma, medullary thyroid carcinoma, and pheochromocytoma [2,35,50]. In addition to hypercalcemia, high calcitonin levels produced by medullary thyroid carcinoma with elevated plasma or urine catecholamines produced by pheochromocytoma are characteristic [2,50].
- MEN4 is clinically similar to MEN1. However, it is caused by an inactivating mutation of CDKN1B (cyclin-dependent kinase inhibitor 1B) on chromosome 12p13.1 [2,35]. The tumour suppressor gene CDKN1B encodes p27 which blocks the cell cycle at G0/G1 phase, regulates apoptosis and cell motility [2,50]. Similar to MEN1, MEN4 typically comprises parathyroid adenoma and pituitary adenoma, and can be associated with gastrinomas, insulinomas, or malignancy in the genitourinary tracts [2,50].
- D.
- Diagnosis
2.4. Parathyroid Hormone- Hypoparathyroidism
- A.
- Isolated Hypoparathyroidism
- Autosomal dominant hypocalcemia type 1 results from a gain of function mutations in CaSR increasing the sensitivity and response to serum concentrations of calcium leading to inappropriately low PTH production [37,50]. It may be associated with Bartter syndrome type 5 caused by poor renal tubular reabsorption of sodium chloride [50].
- B.
- Familial Isolated Hypoparathyroidism
- Mutations in GCM2 (glial cells missing 2) on 6p24.2 encodes a transcription factor essential for parathyroid gland differentiation [52].
- C.
- Diagnosis
2.5. Parathyroid Hormone-Pseudohypoparathyroidism
- Pseudohypoparathyroidism 1A (PHP1A), the most common subtype of PHP, is caused by inactivating maternal GNAS mutations. The gene GNAS encodes the alpha subunit of the stimulatory guanine nucleotide-binding protein Gsα. The maternal allele is expressed exclusively in the renal tubules while in other tissues, both maternal and paternal alleles are expressed. Other hormones such as TSH, gonadotropins, and growth hormone-releasing hormone act via G protein-coupled receptors too [2,22]. Albright Hereditary Osteodystrophy (AHO) clinical phenotype describes specific features such as short stature, developmental delay, round faces, depressed nasal bridge, brachydactyly, and dental abnormalities associated with PHP1A [22,53].
- Pseudohypoparathyroidism 1B (PHP1B) is caused by isolated renal resistance to PTH, resulting from methylation defects at differentially methylated regions (DMRs) of the GNAS maternal allele, causing decreased expression of Gsα [22,53]. These patients are usually difficult to diagnose as they lack the AHO findings, present with a normal phenotype [55], and typically have no other endocrine abnormalities [22,53]. As only the maternal allele is expressed in the kidney, renal PTH resistance manifests without the skeletal affects due to the intact paternal allele. Sporadic cases of PHP1B are most common, however, autosomal dominant transmission has also been reported [22,53]. Biochemically PHP1A and PHP1B are similar, leading to hyperphosphatemia, hypocalcemia, and elevated PTH (Table 4).
2.6. FGF23
- Loss-of-function mutation of PHEX (phosphate-regulating endopeptidase homolog) on chromosome Xp22.2-p22.1 is associated with increased expression of FGF23 and leads to X-linked dominant hypophosphatemic rickets [1,60,61]. Normally PHEX is expressed in mature osteoblasts and odontoblasts and plays a role in the down-regulation of FGF23 expression [62,63].
2.7. Hypophosphatasia
- A.
- Hypophosphatasia (HPP) is a rare inherited disorder of bone and mineral metabolism caused by loss of function mutations in the ALPL gene encoding the tissue nonspecific alkaline phosphatase (TNSALP) [65,66] (Table 6). Osteoblast synthesis of TNSALP is decreased due to monoallelic or biallelic inactivating mutations in ALPL [66,67].
- B.
- Clinical Symptoms
- The severe infantile form of hypophosphatasia is due to biallelic inactivating mutation presenting before six months and is fatal. Initial signs are failure to thrive, impaired feeding, motor delays and weakness, limb deformities and rachitic deformations of the thorax leading to respiratory failure. Vitamin B6-dependent seizures could be present as well [68].
- Mild clinical forms of HPP are due to monoallelic mutations leading to milder forms of the HPP presenting with bone pain, leg bowing, joint enlargement, and fractures. A specific and constant feature of HPP is the premature, painless, and atraumatic loss of the primary teeth with intact roots. Nephrocalcinosis due to elevated hypercalciuria could develop in older children and adolescents [66,68,69].
3. Treatment
3.1. Vitamin D Deficiency and Nutritional Rickets
3.2. Vitamin D-Dependent Rickets
3.3. Hyperparathyroidism
3.4. Hypoparathyroidism
3.5. Hypophosphatemic Rickets
3.6. Hypophosphatasia
3.7. Modifiable Factors
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Conflicts of Interest
References
- Thakker, R.V.; Richard Bringhurst, F.; Jüppner, H. Chapter 61—Regulation of Calcium Homeostasis and Genetic Disorders that Affect Calcium Metabolism. In Endocrinology: Adult and Pediatric, 7th ed.; Jameson, J.L., De Groot, L.J., de Kretser, D.M., Giudice, L.C., Grossman, A.B., Melmed, S., Potts, J.T., Jr., Weir, G.C., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2016; pp. 1063–1089.e10. [Google Scholar] [CrossRef]
- Thakker, R.V. The Parathyroid Glands, Hypercalcemia, and Hypocalcemia. In Goldman-Cecil Medicine, 26th ed.; Schafer, L.G.A.I., Ed.; Elsevier: Philadelphia, PA, USA, 2020; pp. 1611–1623.e2. [Google Scholar]
- Root, A.W.; Levine, M.A. 20—Disorders of Mineral Metabolism II. Abnormalities of Mineral Homeostasis in the Newborn, Infant, Child, and Adolescent. In Sperling Pediatric Endocrinology, 5th ed.; Sperling, M.A., Ed.; Elsevier: Philadelphia, PA, USA, 2021; pp. 705–813. [Google Scholar]
- Root, A.W. Genetic disorders of calcium, phosphorus, and bone homeostasis. Transl. Sci. Rare Dis. 2018, 3, 1–36. [Google Scholar] [CrossRef]
- Kliegman, R.M.; St. Geme, J.W.; Blum, N.J.; Shah, S.S.; Tasker, R.C.; Wilson, K.M.; Greenbaum, L.A. Electrolyte and Acid-Base Disorders. In Nelson Textbook of Pediatrics; Elsevier: Philadelphia, PA, USA, 2020; pp. 389–425. [Google Scholar]
- Moutsatsou, P.; Kassi, E.; Papavassiliou, A.G. Glucocorticoid receptor signaling in bone cells. Trends Mol. Med. 2012, 18, 348–359. [Google Scholar] [CrossRef] [PubMed]
- Uday, S.; Högler, W. Rickets and Osteomalacia. In Encyclopedia of Endocrine Diseases, 2nd ed.; Huhtaniemi, I., Martini, L., Eds.; Academic Press: Oxford, UK, 2019; pp. 339–354. [Google Scholar]
- Waller, D.G.; Sampson, A.P. Calcium metabolism and metabolic bone disease. In Medical Pharmacology and Therapeutics; Elsevier: Philadelphia, PA, USA, 2017; pp. 481–489. [Google Scholar]
- Clinical disorders of bone and mineral metabolism 5th international symposium. Calcif. Tissue Int. 1993, 52, S1–S46. [CrossRef] [PubMed]
- Watson, R.R. Handbook of Vitamin D in Human Health; Wageningen Academic Publishers: Wageningen, The Netherlands, 2013. [Google Scholar]
- Sharma, A.; Thakker, R.V.; Jüppner, H. Physiology of the Developing Kidney: Disorders and Therapy of Calcium and Phosphorous Homeostasis. In Pediatric Nephrology; Avner, E., Harmon, W., Niaudet, P., Yoshikawa, N., Emma, F., Goldstein, S., Eds.; Springer: Berlin/Heidelberg, Germany, 2016; pp. 291–339. [Google Scholar]
- Holick, M.F. Resurrection of vitamin D deficiency and rickets. J. Clin. Investig. 2006, 116, 2062–2072. [Google Scholar] [CrossRef] [PubMed]
- Schlingmann, K.P.; Konrad, M. Chapter 74—Infantile Hypercalcemia and CYP24A1 Mutations. In Vitamin D, 4th ed.; Feldman, D., Ed.; Academic Press: Oxford, UK, 2018; pp. 317–330. [Google Scholar]
- Mirea, A.-M.; Pop, R.M.; Căinap, S.S.; Trifa, A.P. Presymptomatic diagnosis of CYP24A1-related infantile idiopathic hypercalcemia: A case report. Eur. J. Med. Genet. 2020, 63, 104100. [Google Scholar] [CrossRef]
- Bikle, D.D.; Adams, J.S.; Christakos, S. Vitamin D: Production, Metabolism, Action, and Clinical Requirements. In Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism; Wiley Online Library: Hoboken, NJ, USA, 2018; pp. 230–240. [Google Scholar]
- Masi, L.; Agnusdei, D.; Bilezikian, J.; Chappard, D.; Chapurlat, R.; Cianferotti, L.; Devolgelaer, J.-P.; El Maghraoui, A.; Ferrari, S.; Javaid, M.K.; et al. Taxonomy of rare genetic metabolic bone disorders. Osteoporos. Int. 2015, 26, 2529–2558. [Google Scholar] [CrossRef]
- Gardella, T.J.; Nissenson, R.A.; Jüppner, H. Parathyroid Hormone. In Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism; Wiley Online Library: Hoboken, NJ, USA, 2018; pp. 205–211. [Google Scholar]
- Underland, L.; Markowitz, M.; Gensure, R. Calcium and Phosphate Hormones: Vitamin D, Parathyroid Hormone, and Fibroblast Growth Factor 23. Pediatr. Rev. 2020, 41, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Tfelt-Hansen, J.; Brown, E.M. The calcium-sensing receptor in normal physiology and pathophysiology: A review. Crit. Rev. Clin. Lab. Sci. 2005, 42, 35–70. [Google Scholar] [CrossRef] [PubMed]
- Moe, S.M. Disorders involving calcium, phosphorus, and magnesium. Prim. Care Clin. Off. Pract. 2008, 35, 215–237. [Google Scholar] [CrossRef] [PubMed]
- Koves, I.H.; Ness, K.D.; Nip, A.S.-Y.; Salehi, P. 95—Disorders of Calcium and Phosphorus Metabolism. In Avery’s Diseases of the Newborn, 10th ed.; Gleason, C.A., Juul, S.E., Eds.; Elsevier: Philadelphia, PA, USA, 2018; pp. 1333–1350.e4. [Google Scholar]
- Goel, N.J.; Meyers, L.L.; Frangos, M. Pseudohypoparathyroidism type 1B in a patient conceived by in vitro fertilization: Another imprinting disorder reported with assisted reproductive technology. J. Assist. Reprod. Genet. 2018, 35, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Saito, T.; Fukumoto, S. Fibroblast Growth Factor 23 (FGF23) and Disorders of Phosphate Metabolism. Int. J. Pediatr. Endocrinol. 2009, 2009, 496514. [Google Scholar] [CrossRef] [PubMed]
- McKay, C.P. Disorders of Calcium Metabolism. In Fluid and Electrolytes in Pediatrics; Feld, L.G., Kaskel, F.J., Eds.; Humana Press: Totowa, NJ, USA, 2010. [Google Scholar]
- Schlingmann, K.P.; Kaufmann, M.; Weber, S.; Irwin, A.; Goos, C.; John, U.; Misselwitz, J.; Klaus, G.; Kuwertz-Bröking, E.; Fehrenbach, H.; et al. Mutations in CYP24A1 and idiopathic infantile hypercalcemia. N. Engl. J. Med. 2011, 365, 410–421. [Google Scholar] [CrossRef] [PubMed]
- Schlingmann, K.P.; Ruminska, J.; Kaufmann, M.; Dursun, I.; Patti, M.; Kranz, B.; Pronicka, E.; Ciara, E.; Akcay, T.; Bulus, D.; et al. Autosomal-Recessive Mutations in SLC34A1 Encoding Sodium-Phosphate Cotransporter 2A Cause Idiopathic Infantile Hypercalcemia. J. Am. Soc. Nephrol. 2016, 27, 604–614. [Google Scholar] [CrossRef] [PubMed]
- Hureaux, M.; Chantot-Bastaraud, S.; Cassinari, K.; Casado, E.M.; Cuny, A.; Frébourg, T.; Vargas-Poussou, R.; Bréhin, A.-C. When a maternal heterozygous mutation of the CYP24A1 gene leads to infantile hypercalcemia through a maternal uniparental disomy of chromosome 20. Mol. Cytogenet. 2021, 14, 23. [Google Scholar] [CrossRef]
- Lodefalk, M.; Frykholm, C.; Esbjörner, E.; Ljunggren, Ö. Hypercalcaemia in a Patient with 2p13.2-p16.1 Duplication. Horm. Res. Paediatr. 2016, 85, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Schlingmann, K.P.; Cassar, W.; Konrad, M. Juvenile onset IIH and CYP24A1 mutations. Bone Rep. 2018, 9, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Jobst-Schwan, T.; Pannes, A.; Schlingmann, K.P.; Beck, B.B.; Wiesener, M.S.; Eckardt, K.-U. Discordant Clinical Course of Vitamin-D-Hydroxylase (CYP24A1) Associated Hypercalcemia in Two Adult Brothers with Nephrocalcinosis. Kidney Blood Press. Res. 2015, 40, 443–451. [Google Scholar] [CrossRef]
- Bikle, D.; Christakos, S. New aspects of vitamin D metabolism and action—Addressing the skin as source and target. Nat. Rev. Endocrinol. 2020, 16, 234–252. [Google Scholar] [CrossRef]
- Bhansali, A.; Aggarwal, A.; Parthan, G.; Gogate, Y. Rickets–Osteomalacia. In Clinical Rounds in Endocrinology; Springer: New Delhi, India, 2016; pp. 131–170. [Google Scholar]
- Ahmad, N.; Sobaihi, M.M.; Al-Jabri, M.; Al-Esaei, N.A.; Alzaydi, A. Acute respiratory failure and generalized hypotonia secondary to vitamin D dependent rickets type 1A. Int. J. Pediatr. Adolesc. Med. 2018, 5, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Khokhar, A.; Castells, S.; Perez-Colon, S. Genetic Disorders of Vitamin D Metabolism: Case Series and Literature Review. Clin. Pediatr. 2016, 55, 404–414. [Google Scholar] [CrossRef]
- National Center for Biotechnology Information. Genetic Testing Registry; U.S. National Library of Medicine: Bethesda, MD, USA, 2022. [Google Scholar]
- Gattineni, J.; Baum, M. Genetic disorders of phosphate regulation. Pediatr. Nephrol. 2012, 27, 1477–1487. [Google Scholar] [CrossRef] [PubMed]
- Root, A.W. Genetic disorders of calcium and phosphorus metabolism. Crit. Rev. Clin. Lab. Sci. 2000, 37, 217–260. [Google Scholar] [CrossRef] [PubMed]
- Bilezikian, J.P.; Bandeira, L.; Khan, A.; Cusano, N.E. Hyperparathyroidism. Lancet 2018, 391, 168–178. [Google Scholar] [CrossRef]
- Bilezikian, J.P.; Cusano, N.E.; Khan, A.A.; Liu, J.M.; Marcocci, C.; Bandeira, F. Primary hyperparathyroidism. Nat. Rev. Dis. Primers 2016, 2, 16033. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.H. Approach to the Child with Hypercalcaemia. In Calcium and Bone Disorders in Children and Adolescents; Karger: Basel, Switzerland, 2015; Volume 28, pp. 101–118. [Google Scholar] [CrossRef]
- Silva, B.C.; Cusano, N.E.; Bilezikian, J.P. Primary hyperparathyroidism. Best Pract. Res. Clin. Endocrinol. Metab. 2018, 32, 593–607. [Google Scholar] [CrossRef] [PubMed]
- Dumitru, C.; Wysolmerski, J. Chapter 66—Disorders of Calcium Metabolism. In Seldin and Giebisch’s The Kidney, 5th ed.; Alpern, R.J., Moe, O.W., Caplan, M., Eds.; Academic Press: Oxford, UK, 2013; pp. 2273–2309. [Google Scholar]
- Robinson, C. Genetics of Mineral Disorders. In Encyclopedia of Bone Biology; Zaidi, M., Ed.; Academic Press: Oxford, UK, 2020; pp. 92–107. [Google Scholar]
- Diao, J.; DeBono, A.; Josephs, T.M.; Bourke, J.E.; Capuano, B.; Gregory, K.J.; Leach, K. Therapeutic Opportunities of Targeting Allosteric Binding Sites on the Calcium-Sensing Receptor. ACS Pharmacol. Transl. Sci. 2021, 4, 666–679. [Google Scholar] [CrossRef] [PubMed]
- Warner, J.V.; Nyholt, D.; Busfield, F.; Epstein, M.; Burgess, J.; Stranks, S.; Hill, P.; Perry-Keene, D.; Learoyd, D.; Robinson, B.; et al. Familial isolated hyperparathyroidism is linked to a 1.7 Mb region on chromosome 2p13.3–14. J. Med. Genet. 2006, 43, e12. [Google Scholar] [CrossRef][Green Version]
- Shibata, Y.; Yamazaki, M.; Takei, M.; Uchino, S.; Sakurai, A.; Komatsu, M. Early-onset, severe, and recurrent primary hyperparathyroidism associated with a novel CDC73 mutation. Endocr. J. 2015, 62, 627–632. [Google Scholar] [CrossRef]
- Simonds, W.F.; James-Newton, L.A.; Agarwal, S.K.; Yang, B.; Skarulis, M.C.; Hendy, G.N.; Marx, S.J. Familial Isolated Hyperparathyroidism: Clinical and Genetic Characteristics of 36 Kindreds. Medicine 2002, 81, 1–26. [Google Scholar] [CrossRef]
- Battista, C.; Guarnieri, V.; Carnevale, V.; Baorda, F.; Pileri, M.; Garrubba, M.; Salcuni, A.S.; Chiodini, I.; Minisola, S.; Romagnoli, E.; et al. Vitamin D status in primary hyperparathyroidism: Effect of genetic background. Endocrine 2017, 55, 266–272. [Google Scholar] [CrossRef]
- Kabadi, U.M. Low 25-Hydroxyvitamin D in Primary Hyperparathyroidism: Enhanced Conversion into 1,25-Hydroxyvitamin D May Not Be “True” Deficiency. JBMR Plus 2020, 4, e10415. [Google Scholar] [CrossRef]
- Hendy, G.N.; Cole, D.E.C.; Bastepe, M. Hypoparathyroidism and Pseudohypoparathyroidism. In Endotext; Feingold, K.R., Anawalt, B., Boyce, A., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Roszko, K.L.; Bi, R.D.; Mannstadt, M. Autosomal Dominant Hypocalcemia (Hypoparathyroidism) Types 1 and 2. Front. Physiol. 2016, 7, 458. [Google Scholar] [CrossRef]
- Thomée, C.; Schubert, S.W.; Parma, J.; Lê, P.Q.; Hashemolhosseini, S.; Wegner, M.; Abramowicz, M. GCMB Mutation in Familial Isolated Hypoparathyroidism with Residual Secretion of Parathyroid Hormone. J. Clin. Endocrinol. Metab. 2005, 90, 2487–2492. [Google Scholar] [CrossRef] [PubMed]
- Gordon, R.J.; Levine, M.A. Genetic Disorders of Parathyroid Development and Function. Endocrinol. Metab. Clin. N. Am. 2018, 47, 809–823. [Google Scholar] [CrossRef] [PubMed]
- Hendy, G.N.; Bastepe, M.; Cole, D.E.C. Chapter 85—Parathyroid Disorders. In Emery and Rimoin’s Principles and Practice of Medical Genetics; Rimoin, D., Pyeritz, R., Korf, B., Eds.; Academic Press: Oxford, UK, 2013; pp. 1–34. [Google Scholar]
- Brix, B.; Werner, R.; Staedt, P.; Struve, D.; Hiort, O.; Thiele, S. Different Pattern of Epigenetic Changes of the GNAS Gene Locus in Patients with Pseudohypoparathyroidism Type Ic Confirm the Heterogeneity of Underlying Pathomechanisms in This Subgroup of Pseudohypoparathyroidism and the Demand for a New Classification of GNAS-Related Disorders. J. Clin. Endocrinol. Metab. 2014, 99, E1564–E1570. [Google Scholar] [PubMed]
- Thiele, S.; de Sanctis, L.; Werner, R.; Grötzinger, J.; Aydin, C.; Jüppner, H.; Bastepe, M.; Hiort, O. Functional characterization of GNAS mutations found in patients with pseudohypoparathyroidism type Ic defines a new subgroup of pseudohypoparathyroidism affecting selectively Gsα-receptor interaction. Hum. Mutat. 2011, 32, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, H.J.; Villarreal, H.; Klahr, S.; Slatopolsky, E. Pseudohypoparathyroidism Type II: Restoration of Normal Renal Responsiveness to Parathyroid Hormone by Calcium Administration. J. Clin. Endocrinol. Metab. 1974, 39, 693–701. [Google Scholar] [CrossRef] [PubMed]
- Linglart, A.; Menguy, C.; Couvineau, A.; Auzan, C.; Gunes, Y.; Cancel, M.; Motte, E.; Pinto, G.; Chanson, P.; Bougnères, P.; et al. Recurrent PRKAR1A mutation in acrodysostosis with hormone resistance. N. Engl. J. Med. 2011, 364, 2218–2226. [Google Scholar] [CrossRef]
- Drezner, M.; Neelon, F.A.; Lebovitz, H.E. Pseudohypoparathyroidism type II: A possible defect in the reception of the cyclic AMP signal. N. Engl. J. Med. 1973, 289, 1056–1060. [Google Scholar] [CrossRef] [PubMed]
- Al Juraibah, F.; Al Amiri, E.; Al Dubayee, M.; Al Jubeh, J.; Al Kandari, H.; Al Sagheir, A.; Al Shaikh, A.; Beshyah, S.A.; Deeb, A.; Habeb, A.; et al. Diagnosis and management of X-linked hypophosphatemia in children and adolescent in the Gulf Cooperation Council countries. Arch. Osteoporos. 2021, 16, 52. [Google Scholar] [CrossRef]
- Raimann, A.; Mehany, S.N.; Feil, P.; Weber, M.; Pietschmann, P.; Boni-Mikats, A.; Klepochova, R.; Krššák, M.; Häusler, G.; Schneider, J.; et al. Decreased Compressional Sound Velocity Is an Indicator for Compromised Bone Stiffness in X-Linked Hypophosphatemic Rickets (XLH). Front. Endocrinol. 2020, 11, 355. [Google Scholar] [CrossRef] [PubMed]
- Şıklar, Z.; Turan, S.; Bereket, A.; Baş, F.; Güran, T.; Akberzade, A.; Abacı, A.; Demir, K.; Böber, E.; Özbek, M.N.; et al. Nationwide Turkish Cohort Study of Hypophosphatemic Rickets. J. Clin. Res. Pediatr. Endocrinol. 2020, 12, 150–159. [Google Scholar] [CrossRef]
- Acar, S.; Demir, K.; Shi, Y. Genetic Causes of Rickets. J. Clin. Res. Pediatr. Endocrinol. 2017, 9 (Suppl. 2), 88–105. [Google Scholar] [CrossRef] [PubMed]
- Jagtap, V.S.; Sarathi, V.; Lila, A.R.; Bandgar, T.; Menon, P.; Shah, N.S. Hypophosphatemic rickets. Indian J. Endocrinol. Metab. 2012, 16, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Josse, R.; Kannu, P.; Villeneuve, J.; Paul, T.; Van Uum, S.; Greenberg, C.R. Hypophosphatasia: Canadian update on diagnosis and management. Osteoporos Int. 2019, 30, 1713–1722. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, C.; Girschick, H.; Mornet, E.; Schneider, D.; Jakob, F.; Mentrup, B. Unexpected high intrafamilial phenotypic variability observed in hypophosphatasia. Eur. J. Hum. Genet. 2014, 22, 1160–1164. [Google Scholar] [CrossRef] [PubMed]
- Whyte, M.P. Hypophosphatasia: An overview For 2017. Bone 2017, 102, 15–25. [Google Scholar] [CrossRef]
- Linglart, A.; Biosse-Duplan, M. Hypophosphatasia. Curr. Osteoporos Rep. 2016, 14, 95–105. [Google Scholar] [CrossRef]
- Mornet, E. Hypophosphatasia. Metabolism 2018, 82, 142–155. [Google Scholar] [CrossRef]
- Bhan, A.; Rao, A.; Bhadada, S.; Rao, S. Rickets and Osteomalacia. In Williams Textbook of Endocrinology; Elsevier: Philadelphia, PA, USA, 2020; pp. 1298–1317.e6. [Google Scholar]
- Carpenter, T. Etiology and Treatment of Calcipenic Rickets in Children. 6 February 2020. Available online: https://www.medilib.ir/uptodate/show/5804 (accessed on 25 January 2022).
- Bollerslev, J.; Schalin-Jäntti, C.; Rejnmark, L.; Siggelkow, H.; Morreau, H.; Thakker, R.; Sitges-Serra, A.; Cetani, F.; Marcocci, C.; Guistina, A.; et al. Management of Endocrine Disease: Unmet therapeutic, educational and scientific needs in parathyroid disorders. Eur. J. Endocrinol. 2019, 181, P1–P19. [Google Scholar] [CrossRef] [PubMed]
- Kellerman, R.D.; Rakel, D.; Conn, H.F.; Marcocci, C. Hyperparathyroidism and Hypoparathyroidism. In Conn’s Current Therapy; Elsevier: Philadelphia, PA, USA, 2021; pp. 330–337. [Google Scholar]
- Goltzman, D. Hypoparathyroidism; UpToDate. 2021. Available online: https://www.uptodate.com/contents/hypoparathyroidism (accessed on 25 January 2022).
- Rubin, M.R.; Levine, M.A. Chapter 75. Hypoparathyroidism and Pseudohypoparathyroidism. In Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism; Wiley Online Library: Hoboken, NJ, USA, 2008; pp. 354–361. [Google Scholar]
- Scheinman, S.J.; Carpenter, T. Hereditary Hypophosphatemic Rickets and Tumor-Induced Osteomalacia; UpToDate, 2021. Available online: https://www.uptodate.com/contents/hereditary-hypophosphatemic-rickets-and-tumor-induced-osteomalacia (accessed on 25 January 2022).
- Seefried, L.; Kishnani, P.S.; Moseley, S.; Denker, A.E.; Watsky, E.; Whyte, M.P.; Dahir, K.M. Pharmacodynamics of asfotase alfa in adults with pediatric-onset hypophosphatasia. Bone 2021, 142, 115664. [Google Scholar] [CrossRef] [PubMed]
- Seefried, L.; Rak, D.; Petryk, A.; Genest, F. Bone turnover and mineral metabolism in adult patients with hypophosphatasia treated with asfotase alfa. Osteoporos. Int. 2021, 32, 2505–2513. [Google Scholar] [CrossRef] [PubMed]
- Stokes, V.J.; Nielsen, M.F.; Hannan, F.M.; Thakker, R.V. Hypercalcemic Disorders in Children. J. Bone Miner. Res. 2017, 32, 2157–2170. [Google Scholar] [CrossRef] [PubMed]
- Vlachopapadopoulou, E.-A.; Anagnostou, E.; Dikaiakou, E.; Hanna, P.; Tsolia, M.; Michalacos, S.; Linglart, A.; Karavanaki, K. Pseudohypoparathyroidism type 1B (PHP1B), a rare disorder encountered in adolescence. J. Pediatr. Endocrinol. Metab. 2020, 33, 1475–1479. [Google Scholar] [CrossRef] [PubMed]
- Ramalho e Silva, J.D.; da Rocha, G.F.M.A.; Oliveira, M.J.M. An intricate case of sporadic pseudohypoparathyroidism type 1B with a review of literature. Arch. Endocrinol. Metab. 2021, 65, 112–116. [Google Scholar] [PubMed]
- Bouchard, G.; Laberge, C.; Scriver, C.R. Hereditary tyrosinemia and vitamin-dependent rickets in Saguenay. A genetic and demographic approach. Union Med. Can. 1985, 114, 633–636. [Google Scholar] [PubMed]
- El Kholy, M.; Elsedfy, H.; Cancio, M.F.; Hamza, R.T.; Amr, N.H.; Ahmed, A.; Toaima, N.N.; Audí, L. Nutritional rickets: Vitamin D, calcium, and the genetic make-up. Pediatr. Res. 2017, 81, 356–363. [Google Scholar] [CrossRef]
- Zittermann, A.; Pilz, S.; Berthold, H.K. Serum 25-hydroxyvitamin D response to vitamin D supplementation in infants: A systematic review and meta-analysis of clinical intervention trials. Eur. J. Nutr. 2020, 59, 359–369. [Google Scholar] [CrossRef] [PubMed]
- Irzyniec, T.; Boryń, M.; Kasztalska, J.; Nowak-Kapusta, Z.; Maciejewska-Paszek, I.; Grochowska-Niedworok, E. The effect of an oral sodium phosphate load on parathyroid hormone and fibroblast growth factor 23 secretion in normo- and hypercalciuric stone-forming patients. Clin. Nutr. 2020, 39, 3804–3812. [Google Scholar] [CrossRef]



| Disease Type of Inheritance | MIM No. | Gene/Protein | Serum 25OHD | Serum 1,25(OH)2D | Serum Ca | Plasma PTH | Serum ALP | TmP/GFR | Serum Phos | Urine Ca Excretion, Urine Ca/Cr |
|---|---|---|---|---|---|---|---|---|---|---|
| Vitamin D-Dependent rickets type 1A (VDDR1A) AR | 264700 | CYP271 1α hydroxylase 12q14.1 | N | ↓↓ | ↓↓ | ↑↑↑ | ↑↑↑ | ↓ | ↓ | ↓ |
| Vitamin D-Dependent rickets type 1B (VDDR1B) AR | 600081 | CYP2R1 25 hydroxylase 11p15.2 | ↓↓ | ↓ | ↓↓ | ↑↑↑ | ↑↑↑ | ↓ | ↓ | ↓ |
| Vitamin D-Dependent rickets type 3 (VDDR3) AD | 619073 | CYP3A4 7q22.1 | ↓↓ | ↓ | ↓↓ | ↑↑↑ | ↑↑↑ | ↓ | ↓ | ↓ |
| Vitamin D-Dependent rickets type 2A (VDDR2A) AR | 277440 | VDR Vitamin D receptor 12q13.11 | N | ↑↑↑ | ↓↓ | ↑↑↑ | ↑↑↑ | ↓ | ↓ | ↓ |
| Vitamin D-Dependent rickets type 2B (VDDR2B) AR | 164020 | HNRNC hormone response element-binding protein | N | ↑↑↑ | ↓↓ or N | ↑↑↑ | ↑↑↑ | ↓ | ↓ | ↓ |
| Disease Type of Inheritance | MIM No. | Gene Defect/Location | Plasma PTH | Serum Ca | Serum Phos | Serum 25OHD | Serum 1,25(OH)2D | Urine Ca/Cr |
|---|---|---|---|---|---|---|---|---|
| Familial isolated hyperparathyroidism AD | 145000 | MEN1/menin 11q13.1 1q31.2 CaSR 3q13.3-q21.1 GCM2 6p24 | ↑ | ↑ | ↓ | N | ↑ | ↑ |
| Hyperparathyroidsm-jaw-tumour syndrome AD | 145001 | CDC73 1q31.2 | ↑ | ↑ | ↓ | N | ↑ | ↑ |
| FHH type 1 AD | 145980 | CaSR 3q13-q21 | ↑ | ↑ | ↓ | N | ↑ | ↓ |
| FHH type 2 AD | 145981 | GNA11 19p13.3 | ↑ | ↑ | ↓ | N | ↑ | ↓ |
| FHH type 3 AD | 600740 | AP2S1 19q13.32 | ↑ | ↑ | ↓ | N | ↑ | ↓ |
| Neonatal severe hyperparathyroidism AR | 239200 | CaSR homozygous inactivating | ↑ | ↑↑↑ | ↓ | N | ↑ | ↓ |
| MEN1 AD | 131100 | MEN1 or menin 11q13.1 | ↑ | ↑ | ↓ | N | ↑ | ↓ |
| MEN2A AD | 171400 | RET 10q11.2 | ↑ | ↑ | ↓ | N | ↑ | ↓ |
| MEN4 AD | 610755 | CDKN1B | ↑ | ↑ | ↓ | N | ↑ | ↓ |
| Disease Type of Inheritance | MIM No. | Gene Defect/Protein | Plasma PTH | Serum Ca | Serum P | Serum 1,25(OH)2D | Urine Ca | Urine cAMP | TmP GFR | Additional Features |
|---|---|---|---|---|---|---|---|---|---|---|
| AD hypocalcemia type 1, (isolated hypoparathyroidism) | 601198 | CaSR 3q13.3-q21.1 | ↓↓↓ | ↓ | ↑ | ↓ | ↑↑ | ↓ | ↑ | Nephrocalcinosis Nephrolithiasis |
| AD hypocalcemia type 2 (isolated hypoparathyroidism) | 615361 | GNA11 19p13.3 | ↓ | ↓ | ↑ | ↓ | Low to mild high | N/A | ↑ | short stature, intracranial calcifications |
| Familial isolated hypoparathyroidism AD, AR | 146200 | PTH 11p15.3 | ↓ | ↓ | ↑ | ↓ | ↑ | ↓ | ↑ | N |
| Familial isolated hypoparathyroidism AD, AR | 618883 | GCM26p24.2 | ↓ | ↓ | ↑ | ↓ | ↓ | N/A | ↑ | calcifications of the basal ganglia |
| Disease Type of Inheritance | MIM No. | Gene Defect/Protein | Serum Ca | Serum P | Serum PTH | Serum 1,25(OH)2D | Urine cAMP | Urine PO4 | Associated Features |
|---|---|---|---|---|---|---|---|---|---|
| Type 1A | 103580 | GNAS Maternal allele | ↓ | ↑ | ↑ | ↓ | ↓ | ↓ | Yes TSH, LH, FSH |
| Type 1B | 603233 | GNAS-AS1, STX16, GNAS | ↓ | ↑ | ↑ | ↓ | ↓ | ↓ | Thyroid mild defects somatotropin |
| Type 1C | 612462 | GNAS | ↓ | ↑ | ↑ | ↓ | ↓ | ↓ | Yes |
| Type 2 | 203330 | PRKAR1A | ↓ | ↑ | ↑ | ↓ | ↑ | ↓ | No |
| Pseudopseudo Hypopara thyroidism | 612463 | GNAS Paternal allele | N | N | N | N | N | N | No |
| Disease Type of Inheritance | MIM No. | Gene Defect Protein | Plasma FGF23 | TmP/GFR | Serum Ca | Serum P | Serum ALP | Plasma PTH | Serum 25OHD | Serum 1,25 (OH)2D | Urine Ca Excretion, Urine Ca/Cr |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Autosomal dominant hypophosphatemic rickets (ADHR) | 193100 | FGF23 12p13.32 | ↑ | ↓ | N | ↓↓ | ↑↑ | N or ↑ | N | N or ↓ | N or ↓ |
| X-linked hypophosphatemia (XLH) X-linked dominant | 307800 | PHEX Xp22.11 | ↑ or N | ↓ | N | ↓↓ | ↑↑ | N or ↑ | N | N or ↓ | N or ↓ |
| Autosomal recessive hypophosphatemic rickets 1 (ARHR1) | 241520 | DMP1 4q22.1 | ↑or N | ↓ | N | ↓↓ | ↑↑ | N or ↑ | N | N or ↓ | N or ↓ |
| Autosomal recessive hypophosphatemic rickets 2 (ARHR2) | 613312 | ENPP1 6q23.2 | ↑or N | ↓ | N | ↓↓ | ↑↑ | N or ↑ | N | N or ↓ | N or ↓ |
| Tumour-induced osteomalacia (TIO) | N/A | N/A | ↑↑↑ | ↓ | N | ↓↓ | ↑↑ | N or ↑ | N | N or ↓ | N or ↓ |
| Hypophosphatemic rickets with hypercalciuria (HHRH) | 241530 | SLC3 4A39q34.3 | ↓ | ↓ | N | ↓ | ↑↑ | N | N | ↑↑ | ↑ |
| Disease Type of Inheritance | MIM No. | Gene Defect /Protein | Plasma FGF23 | Serum ALP | TmP GFR | Serum Ca | Serum Phos | Plasma PTH | Serum 25OHD | Serum 1,25 (OH)2D | Urine Ca Excretion, Urine Ca/Cr |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Infantile severe HypoPhosphatasia (HPP) | 171760 | ALPL geneTissue nonspecific alkaline phosphatase 1p36.12 | ↓ | N | N/A | ↑ | ↑ | ↓ | ↑ | ↓ | ↑↑↑ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miller, A.; Mathew, S.; Patel, S.; Fordjour, L.; Chin, V.L. Genetic Disorders of Calcium and Phosphorus Metabolism. Endocrines 2022, 3, 150-167. https://doi.org/10.3390/endocrines3010014
Miller A, Mathew S, Patel S, Fordjour L, Chin VL. Genetic Disorders of Calcium and Phosphorus Metabolism. Endocrines. 2022; 3(1):150-167. https://doi.org/10.3390/endocrines3010014
Chicago/Turabian StyleMiller, Assia, Serina Mathew, Sneha Patel, Lawrence Fordjour, and Vivian L. Chin. 2022. "Genetic Disorders of Calcium and Phosphorus Metabolism" Endocrines 3, no. 1: 150-167. https://doi.org/10.3390/endocrines3010014
APA StyleMiller, A., Mathew, S., Patel, S., Fordjour, L., & Chin, V. L. (2022). Genetic Disorders of Calcium and Phosphorus Metabolism. Endocrines, 3(1), 150-167. https://doi.org/10.3390/endocrines3010014





