Thyroid and Heart: A Fatal Pathophysiological Attraction in a Controversial Clinical Liaison
Abstract
:1. History of the Relationship between Heart and Thyroid
2. Thyroid and Heart: A Tight Physiological Relation
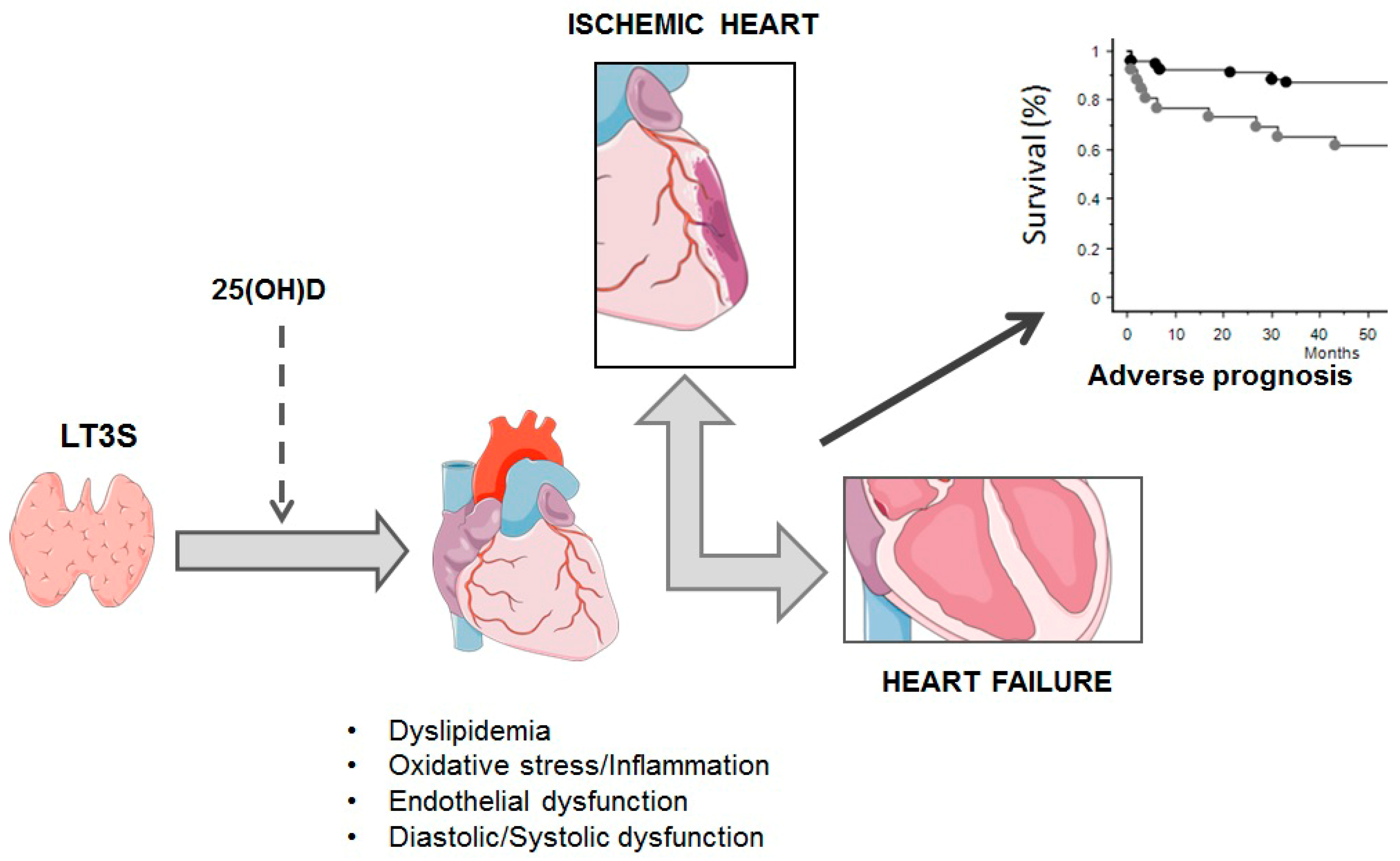
3. Hyperthyroidism, Hypothyroidism, and Subclinical Conditions
4. Thyroid and Cardioprotection
5. The Prognostic Impact of TH Abnormalities in Heart Failure and Acute Myocardial Infarction
6. TH Replacement Therapy in Heart Failure and Acute Myocardial Infarction
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wicomb, W.; Cooper, D.K.; Hassoulas, J.; Rose, A.G.; Barnard, C.N. Orthotopic transplantation of the baboon heart after 20 to 24 hours’ preservation by continuous hypothermic perfusion with an oxygenated hyperosmolar solution. J. Thorac. Cardiovasc. Surg. 1982, 83, 133–140. [Google Scholar] [CrossRef]
- Cooper, D.K.; Wicomb, W.N.; Rose, A.G.; Barnard, C.N. Orthotopic allotransplantation and autotransplantation of the baboon heart following twenty-four hours’ storage by a portable hypothermic perfusion system. Cryobiology 1983, 20, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Cushing, H. Some experimental and clinical observations concerning states of increased intracranial tension. Am. J. Med. Sci. 1902, 124, 373–400. [Google Scholar] [CrossRef]
- Kocher, A. Ueber morbus Basedowi. Mitt. Grenzgeb. Med. Chir. 1901, 1, 1–13. [Google Scholar]
- Cooper, D.K.C.; Novitzky, D.; Wicomb, W.N. The pathophysiological effects of brain death on potential donor organs, with particular reference to the heart. Ann. R. Coll. Surg. Engl. 1989, 71, 261–266. [Google Scholar]
- Novitzky, D.; Rose, A.G.; Cooper, D.K.C.; Reichart, B. Interpretation of endomyocardial biopsy after heart transplantation. Potentially confusing factors. S Afr. Med. J. 1986, 70, 789–792. [Google Scholar]
- Novitzky, D.; Cooper, D.K.C.; Rose, A.G.; Reichart, B. Prevention of myocardial injury by pretreatment with verapamil hydrochloride prior to experimental brain death: Efficacy in a baboon model. Am. J. Emerg. Med. 1987, 5, 11–18. [Google Scholar] [CrossRef]
- Novitzky, D.; Cooper, D.K.C.; Morrell, D.; Isaacs, S. Change from aerobic to anaerobic metabolism after brain death, and reversal following triiodothyronine (T3) therapy. Transplantation 1988, 45, 32–36. [Google Scholar] [CrossRef]
- Hamilton, B.E. Clinical notes on hearts in hyperthyroidism. Boston Med. Surg. J. 1922, 186, 216–218. [Google Scholar] [CrossRef]
- Pratschke, J.; Wilhelm, M.J.; Kusaka, M.; Basker, M.; Cooper, D.K.C.; Hancock, W.W.; Tilney, N.L. Brain death and its influence on donor organ quality and outcome after transplantation. Transplantation 1999, 67, 343–348. [Google Scholar] [CrossRef]
- Goetsch, E. Newer methods in the diagnosis of thyroid disorders: Pathological and clinical: B. Adrenaline hypersensitiveness in clinical states of hyperthyroidism. NY State J. Med. 1918, 18, 259–267. [Google Scholar]
- McDonald, C.H.; Shepeard, W.L.; Green, M.F.; DeGroat, A.F. Response of the hyperthyroid heart to epinephrine. Am. J. Phys. 1935, 112, 227–230. [Google Scholar] [CrossRef]
- Gaffney, T.E.; Braunwald, E.; Kahler, R.L. Effects of guanethidine on triiodothyronine-induced hyperthyroidism in man. New Eng. J. Med. 1961, 265, 16–20. [Google Scholar] [CrossRef] [PubMed]
- Levey, G.S. The adrenergic nervous system in hyperthyroidism: Therapeutic role of beta adrenergic blocking drugs. Pharmacol. Ther. 1976, 1, 431–443. [Google Scholar] [CrossRef]
- The coronary drug project. Findings leading to further modifi cations of its protocol with respect to dextrothyroxine. The coronary drug project research group. JAMA 1972, 220, 996–1008. [CrossRef]
- Pilo, A.; Iervasi, G.; Vitek, F.; Ferdeghini, M.; Cazzuola, F.; Bianchi, R. Thyroidal and peripheral production of 3,5,3′—Triiodothyronine in humans by multicompartmental analysis. Am. J. Physiol. 1990, 258, E715–E726. [Google Scholar] [CrossRef]
- Young, W.F., Jr.; Gorman, C.A.; Jiang, N.S.; Machacek, D.; Hay, I.D. L-thyroxine contamination of pharmaceutical D-thyroxine: Probable cause of therapeutic effect. Clin. Pharmacol. Ther. 1984, 36, 781–787. [Google Scholar] [CrossRef]
- Papp, C. The heart in thyroid dysfunction. Postgrad. Med. J. 1945, 21, 45–51. [Google Scholar] [CrossRef]
- Tata, J.R.; Ernster, L.; Lindberg, O.; Arrhenius, E.; Pedersen, S.; Hedman, R. The action of thyroid hormones at the cell level. Biochem. J. 1963, 86, 408–428. [Google Scholar] [CrossRef]
- Dillmann, W.H. Hormonal influences on cardiac myosin ATPase activity and myosin isoenzyme distribution. Mol. Cell Endocrinol. 1984, 34, 169–181. [Google Scholar] [CrossRef]
- Oppenheimer, J.H.; Koerner, D.; Schwartz, H.L.; Surks, M.I. Specific nuclear triiodothyronine binding sites in rat liver and kidney. J. Clin. Endocrinol. Metab. 1972, 35, 330–333. [Google Scholar] [CrossRef] [PubMed]
- Fazio, S.; Palmieri, E.A.; Lombardi, G.; Biondi, B. Effects of thyroid hormone on the cardiovascular system. Recent Prog. Horm. Res. 2004, 59, 31–50. [Google Scholar] [CrossRef] [PubMed]
- Razvi, S.; Jabbar, A.; Pingitore, A.; Danzi, S.; Biondi, B.; Klein, I.; Peeters, R.; Zaman, A.; Iervasi, G. Thyroid hormones and cardiovascular function and diseases. J. Am. Coll. Cardiol. 2018, 24, 1781–1796. [Google Scholar] [CrossRef] [PubMed]
- Klein, I. Thyroid hormone and the cardiovascular system. Am. J. Med. 1990, 88, 631–637. [Google Scholar] [CrossRef]
- Jabbar, A.; Pingitore, A.; Pearce, S.H.; Zaman, A.; Iervasi, G.; Razvi, S. Thyroid hormones and cardiovascular disease. Nat. Rev. Cardiol. 2017, 14, 39–55. [Google Scholar] [CrossRef]
- Hartong, R.; Wang, N.; Kurokawa, R.; Lazar, M.A.; Glass, C.K.; Apriletti Dillmann, W.H. Delineation of three different thyroid hormone-response elements in promoter of rat sarcoplasmic reticulum Ca2_-ATPase gene. J. Biol. Chem. 1994, 269, 13021–13029. [Google Scholar] [CrossRef]
- Klein, I. Chapter 81: Endocrine disorders and cardiovascular disease. In Braunwald’s Heart Disease, 10th ed.; Elsevier: Philadelphia, PA, USA, 2014; pp. 1793–1808. [Google Scholar]
- Mastorci, F.; Sabatino, L.; Vassalle, C.; Pingitore, A. Cardioprotection and Thyroid Hormones in the Clinical Setting of Heart Failure. Front. Endocrinol. 2020, 10, 927. [Google Scholar] [CrossRef]
- Sun, Z.; Ojamaa, K.; Coetzee, W.A.; Artman, M.; Klein, I. Effects of thyroid hormone on action potential and repolarization currents in rat ventricular myocytes. Am. J. Physiol. Endocrinol. Metab. 2000, 278, E302–E307. [Google Scholar] [CrossRef]
- Pachucki, J.; Burmeister, L.A.; Larsen, P.R. Thyroid hormone regulates hyperpolarization-activated cyclic nucleotide-gated channel (HCN2) mRNA in the rat heart. Circ. Res. 1999, 85, 498–503. [Google Scholar] [CrossRef]
- Danzi, S.; Klein, I. Thyroid hormone and blood pressure regulation. Curr. Hypertens. Rep. 2003, 5, 513–520. [Google Scholar] [CrossRef]
- Klein, I.; Ojamaa, K. Thyroid hormone and the cardiovascular system. N. Engl. J. Med. 2001, 344, 501–509. [Google Scholar] [CrossRef] [PubMed]
- Biondi, B.; Palmieri, E.A.; Lombardi, G.; Fazio, S. Effects of thyroid hormone on cardiac function: The relative importance of heart rate, loading conditions, and myocardial contractility in the regulation of cardiac performance in human hyperthyroidism. J. Clin. Endocrinol. Metab. 2002, 87, 968–974. [Google Scholar] [CrossRef] [PubMed]
- Volpe, R. Immunoregulation in autoimmune thyroid disease. Thyroid 1994, 4, 373–377. [Google Scholar] [CrossRef]
- Cooper, D.S.; Biondi, B. Subclinical thyroid disease. Lancet 2012, 379, 1142–1154. [Google Scholar] [CrossRef]
- Kahaly, G.J.; Dillmann, W.H. Thyroid hormone action in the heart. Endocr. Rev. 2005, 26, 704–728. [Google Scholar] [CrossRef]
- Mohr-Kahaly, S.; Kahaly, G.; Meyer, J. [Cardiovascular effects of thyroid hormones]. Z. Kardiol. 1996, 85 (Suppl. S6), 219–231. [Google Scholar]
- Weltman, N.Y.; Wang, D.; Redetzke, R.A.; Gerdes, A.M. Longstanding hyperthyroidism is associated with normal or enhanced intrinsic cardiomyocyte function despite decline in global cardiac function. PLoS ONE 2012, 7, e46655. [Google Scholar] [CrossRef] [PubMed]
- Klein, I. Endocrine disorders and cardiovascular disease. In Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine, 7th ed.; Zipes, D.P., Libby, P., Bonow, R., Braunwald, E., Eds.; Saunders: Philadelphia, PA, USA, 2005; pp. 2051–2065. [Google Scholar]
- Fredlund, B.O.; Olsson, S.B. Long QT interval and ventricular tachycardia of “torsade de pointe” type in hypothyroidism. Acta Med. Scand. 1983, 213, 231–235. [Google Scholar] [CrossRef]
- Sawin, C.T.; Geller, A.; Wolf, P.A.; Belanger, A.J.; Baker, E.; Bacharach, P.; Wilson, P.W.; Benjamin, E.J.; D’Agostino, R.B. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N. Engl. J. Med. 1994, 331, 1249–1252. [Google Scholar] [CrossRef]
- Parle, J.V.; Maisonneuve, P.; Sheppard, M.C.; Boyle, P.; Franklyn, J.A. Prediction of all-cause and cardiovascular mortality in elderly people from one low serum thyrotropin result: A 10-year cohort study. Lancet 2001, 358, 861–865. [Google Scholar] [CrossRef] [PubMed]
- Iervasi, G.; Molinaro, S.; Landi, P.; Taddei, M.C.; Galli, E.; Mariani, F.; L’abbate, A.; Pingitore, A. Association between increased mortality and mild thyroid dysfunction in cardiac patients. Arch. Intern. Med. 2007, 167, 1526–1532. [Google Scholar] [CrossRef] [PubMed]
- Cappola, A.R.; Fried, L.P.; Arnold, A.M.; Danese, M.D.; Kuller, L.H.; Burke, G.L.; Tracy, R.P.; Ladenson, P.W. Thyroid status, cardiovascular risk, and mortality in older adults. JAMA 2006, 295, 1033–1041. [Google Scholar] [CrossRef]
- Rodondi, N.; Bauer, D.C.; Cappola, A.R.; Cornuz, J.; Robbins, J.; Fried, L.P.; Ladenson, P.W.; Vittinghoff, E.; Gottdiener, J.S.; Newman, A.B. Subclinical thyroid dysfunction, cardiac function, and the risk of heart failure. The Cardiovascular Health study. J. Am. Coll. Cardiol. 2008, 52, 1152–1159. [Google Scholar] [CrossRef]
- Rodondi, N.; Aujesky, D.; Vittinghoff, E.; Cornuz, J.; Bauer, D.C. Subclinical hypothyroidism and the risk of coronary heart disease: A meta-analysis. Am. J. Med. 2006, 119, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Monzani, F.; Di Bello, V.; Caraccio, N.; Bertini, A.; Giorgi, D.; Giusti, C.; Ferrannini, E. Effect of levothyroxine on cardiac function and structure in subclinical hypothyroidism: A double blind, placebo-controlled study. J. Clin. Endocrinol. Metab. 2001, 86, 1110–1115. [Google Scholar] [CrossRef]
- Ripoli, A.; Pingitore, A.; Favilli, B.; Bottoni, A.; Turchi, S.; Osman, N.F.; De Marchi, D.; Lombardi, M.; L’Abbate, A.; Iervasi, G. Does subclinical hypothyroidism affect cardiac pump performance? Evidence from a magnetic resonance imaging study. J. Am. Coll. Cardiol. 2005, 45, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Hak, A.E.; Pols, H.A.; Visser, T.J.; Drexhage, H.A.; Hofman, A.; Witteman, J.C. Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: The Rotterdam Study. Ann. Intern. Med. 2000, 132, 270–278. [Google Scholar] [CrossRef]
- Kübler, W.; Haass, M. Cardioprotection: Definition, classification, and fundamental principles. Heart 1996, 75, 330–333. [Google Scholar] [CrossRef]
- Pingitore, A.; Nicolini, G.; Kusmic, C.; Iervasi, G.; Grigolini, P.; Forini, F. Cardioprotection and thyroid hormones. Heart Fail. Rev. 2016, 21, 391–399. [Google Scholar] [CrossRef]
- Forini, F.; Pitto, L.; Nicolini, G. Thyroid hormone, mitochondrial function and cardioprotection. In Thyroid and Heart; Iervasi, G., Pingitore, A., Gerdes, A.M., Razvi, A., Eds.; Springer Nature: Cham, Switzerland, 2020; Chapter 9. [Google Scholar]
- Goldenthal, M.J.; Ananthakrishnan, R.; Marín-García, J. Nuclear-mitochondrial cross-talk in cardiomyocyte T3 signaling: A time-course analysis. J. Mol. Cell Cardiol. 2005, 39, 319–326. [Google Scholar] [CrossRef]
- Galli, E.; Pingitore, A.; Iervasi, G. The role of thyroid hormone in the pathophysiology of heart failure: Clinical evidence. Heart Fail. Rev. 2010, 15, 155–169. [Google Scholar] [CrossRef] [PubMed]
- Garber, J.R.; Cobin, R.H.; Gharib, H.; Hennessey, J.V.; Klein, I.; Mechanick, J.I.; Pessah-Pollack, R.; Singer, P.A.; Woeber for the American Association of Clinical Endocrinologists; American Association of Clinical Endocrinologists; et al. Clinical practice guidelines for hypothyroidism in adults: Cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid 2012, 22, 1200–1235. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Wang, Y.; Shi, W.; Liu, Y.; Cao, S.; Yu, T. Mitochondrial proteomics alterations in rat hearts following ischemia/reperfusion and diazoxide post conditioning. Mol. Med. Rep. 2021, 23, 161. [Google Scholar] [CrossRef]
- Canale, P.; Nicolini, G.; Pitto, L.; Kusmic, C.; Rizzo, M.; Balzan, S.; Iervasi, G.; Forini, F. Role of miR-133/Dio3 Axis in the T3-Dependent Modulation of Cardiac mitoK-ATP Expression. Int. J. Mol. Sci. 2022, 23, 6549. [Google Scholar] [CrossRef]
- Sabatino, L. Nrf2-Mediated Antioxidant Defense and Thyroid Hormone Signaling: A Focus on Cardioprotective Effects. Antioxidants 2023, 12, 1177. [Google Scholar] [CrossRef] [PubMed]
- Della Nera, G.; Sabatino, L.; Gaggini, M.; Gorini, F.; Vassalle, C. Vitamin D Determinants, Status, and Antioxidant/Anti-inflammatory-Related Effects in Cardiovascular Risk and Disease: Not the Last Word in the Controversy. Antioxidants 2023, 18, 948. [Google Scholar] [CrossRef]
- Al-Oanzi, Z.H.; Alenazy, F.O.; Alhassan, H.H.; Alruwaili, Y.; Alessa, A.I.; Alfarm, N.B.; Alanazi, M.O.; Alghofaili, S.I. The Role of Vitamin D in Reducing the Risk of Metabolic Disturbances That Cause Cardiovascular Diseases. J. Cardiovasc. Dev. Dis. 2023, 10, 209. [Google Scholar] [CrossRef]
- Alrefaie, Z.; Awad, H. Effect of vitamin D3 on thyroid function and deiodinase 2 expression in diabetic rats. Arch. Physiol. Biochem. 2015, 121, 206–209. [Google Scholar] [CrossRef]
- Miura, M.; Tanaka, K.; Komatsu, Y.; Suda, M.; Yasoda, A.; Sakuma, Y.; Ozasa, A.; Nakao, K. A novel interaction between thyroid hormones and 1,25(OH)(2)D(3) in osteoclast formation. Biochem. Biophys. Res. Commun. 2002, 291, 987–994. [Google Scholar] [CrossRef]
- Gouveia, C.H.; Christoffolete, M.A.; Zaitune, C.R.; Dora, J.M.; Harney, J.W.; Maia, A.L.; Bianco, A.C. Type 2 iodothyronine selenodeiodinase is expressed throughout the mouse skeleton and in the MC3T3-E1 mouse osteoblastic cell line during differentiation. Endocrinology 2005, 146, 195–200. [Google Scholar] [CrossRef]
- Berg, J.P.; Liane, K.M.; Bjørhovde, S.B.; Bjøro, T.; Torjesen, P.A.; Haug, E. Vitamin D receptor binding and biological effects of cholecalciferol analogues in rat thyroid cells. J. Steroid Biochem. Mol. Biol. 1994, 50, 145–150. [Google Scholar] [CrossRef]
- D’Emden, M.C.; Wark, J.D. 1,25-Dihydroxyvitamin D3 enhances thyrotropin releasing hormone induced thyrotropin secretion in normal pituitary cells. Endocrinology 1987, 121, 1192–1194. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, Q.; Dong, H.; Feng, Y.; Raguthu, C.; Liang, X.; Liu, C.; Zhang, Z.; Yao, X. The protective effect of iodide intake adjustment and 1,25(OH)2D3 supplementation in rat offspring following excess iodide intake. Ther. Adv. Endocrinol. Metab. 2020, 11, 2042018820958295. [Google Scholar] [CrossRef] [PubMed]
- Vassalle, C.; Parlanti, A.; Pingitore, A.; Berti, S.; Iervasi, G.; Sabatino, L. Vitamin D, Thyroid Hormones and Cardiovascular Risk: Exploring the Components of This Novel Disease Triangle. Front. Physiol. 2021, 12, 722912. [Google Scholar] [CrossRef] [PubMed]
- Babić Leko, M.; Jureško, I.; Rozić, I.; Pleić, N.; Gunjača, I.; Zemunik, T. Vitamin D and the Thyroid: A Critical Review of the Current Evidence. Int. J. Mol. Sci. 2023, 24, 3586. [Google Scholar] [CrossRef] [PubMed]
- Pingitore, A.; Mastorci, F.; Berti, S.; Sabatino, L.; Palmieri, C.; Iervasi, G.; Vassalle, C. Hypovitaminosis D and Low T3 Syndrome: A Link for Therapeutic Challenges in Patients with Acute Myocardial Infarction. J. Clin. Med. 2021, 10, 5267. [Google Scholar] [CrossRef]
- Mirhosseini, N.; Brunel, L.; Muscogiuri, G.; Kimball, S. Physiological serum 25-hydroxyvitamin D concentrations are associated with improved thyroid function-observations from a community-based program. Endocrine 2017, 58, 563–573. [Google Scholar] [CrossRef]
- Iervasi, G.; Pingitore, A.; Landi, P.; Raciti, M.; Ripoli, A.; Scarlattini, M.; L’Abbate, A.; Donato, L. Low-T3 syndrome: A strong prognostic predictor of death in patients with heart disease. Circulation 2003, 107, 708–713. [Google Scholar] [CrossRef]
- Pingitore, A.; Iervasi, G.; Barison, A.; Prontera, C.; Pratali, L.; Emdin, M.; Giannessi, D.; Neglia, D. Early activation of an altered thyroid hormone profile in asymptomatic or mildly symptomatic idiopathic left ventricular dysfunction. J. Card. Fail. 2006, 12, 520–526. [Google Scholar] [CrossRef]
- Molinaro, S.; Iervasi, G.; Lorenzoni, V.; Coceani, M.; Landi, P.; Srebot, V.; Mariani, F.; L’Abbate, A.; Pingitore, A. Persistence of mortality risk in patients with acute cardiac diseases and mild thyroid dysfunction. Am. J. Med. Sci. 2012, 343, 65–70. [Google Scholar] [CrossRef]
- De Matteis, G.; Covino, M.; Burzo, M.L.; Della Polla, D.A.; Petti, A.; Bruno, C.; Franceschi, F.; Mancini, A.; Gambassi, G. Prognostic role of hypothyroidism and low free-triiodothyronine levels in patients hospitalized with acute heart failure. Intern. Emerg. Med. 2021, 16, 1477–1486. [Google Scholar] [CrossRef]
- Zhou, P.; Huang, L.Y.; Zhai, M.; Huang, Y.; Zhuang, X.F.; Liu, H.H.; Zhang, Y.H.; Zhang, J. The prognostic value of free triiodothyronine/free thyroxine ratio in patients hospitalized with heart failure. Zhonghua Yi Xue Za Zhi. 2023, 103, 1679–1684. (In Chinese) [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Han, S.; Li, Y.; Tong, F.; Li, Z.; Sun, Z. Value of FT3/FT4 Ratio in Prognosis of Patients with Heart Failure: A Propensity-Matched Study. Front. Cardiovasc. Med. 2022, 9, 859608. [Google Scholar] [CrossRef]
- Samuel, N.A.; Cuthbert, J.J.; Brown, O.I.; Kazmi, S.; Cleland, J.G.F.; Rigby, A.S.; Clark, A.L. Relation Between Thyroid Function and Mortality in Patients with Chronic Heart Failure. Am. J. Cardiol. 2021, 139, 57–63. [Google Scholar] [CrossRef]
- Iacoviello, M.; Parisi, G.; Gioia, M.I.; Grande, D.; Rizzo, C.; Guida, P.; Lisi, F.; Giagulli, V.A.; Licchelli, B.; Di Serio, F.; et al. Thyroid Disorders and Prognosis in Chronic Heart Failure: A Long-Term Follow-Up Study. Endocr. Metab. Immune Disord. Drug Targets. 2020, 20, 437–445. [Google Scholar] [CrossRef]
- Li, X.; Yao, Y.; Chen, Z.; Fan, S.; Hua, W.; Zhang, S.; Fan, X. Thyroid-stimulating hormone within the normal range and risk of major adverse cardiovascular events in nonischemic dilated cardiomyopathy patients with severe left ventricular dysfunction. Clin. Cardiol. 2019, 42, 120–128. [Google Scholar] [CrossRef]
- Sato, Y.; Yoshihisa, A.; Kimishima, Y.; Kiko, T.; Kanno, Y.; Yokokawa, T.; Abe, S.; Misaka, T.; Sato, T.; Oikawa, M.; et al. Low T3 Syndrome Is Associated with High Mortality in Hospitalized Patients With Heart Failure. J. Card. Fail. 2019, 25, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Kannan, L.; Shaw, P.A.; Morley, M.P.; Brandimarto, J.; Fang, J.C.; Sweitzer, N.K.; Cappola, T.P.; Cappola, A.R. Thyroid dysfunction in heart failure and cardiovascular outcomes. Circ. Heart Fail. 2018, 11, e005266. [Google Scholar] [CrossRef] [PubMed]
- Sato, Y.; Yoshihisa, A.; Kimishima, Y.; Kiko, T.; Watanabe, S.; Kanno, Y.; Abe, S.; Miyata, M.; Sato, T.; Suzuki, S.; et al. Subclinical hypothyroidism is associated with adverse prognosis in heart failure patients. Can. J. Cardiol. 2018, 34, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.Y.; Shu, X.R.; Su, Z.Z.; Lin, R.J.; Zhang, H.F.; Yuan, W.L.; Wang, J.F.; Xie, S.L. A low-normal free triiodothyronine level is associated with adverse prognosis in euthyroid patients with heart failure receiving cardiac resynchronization therapy. Int. Heart J. 2017, 58, 908–914. [Google Scholar] [CrossRef]
- Hayashi, T.; Hasegawa, T.; Kanzaki, H.; Funada, A.; Amaki, M.; Takahama, H.; Ohara, T.; Sugano, Y.; Yasuda, S.; Ogawa, H.; et al. Subclinical hypothyroidism is an independent predictor of adverse cardiovascular outcomes in patients with acute decompensated heart failure. ESC Heart Fail. 2016, 3, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Guan, H.; Fang, W.; Zhang, K.; Gerdes, A.M.; Iervasi, G.; Tang, Y.-D. Free triiodothyronine level correlates with myocardial injury and prognosis in idiopathic dilated cardiomyopathy: Evidence from cardiac MRI and SPECT/PET imaging. Sci. Rep. 2016, 6, 39811. [Google Scholar] [CrossRef] [PubMed]
- Okayama, D.; Minami, Y.; Kataoka, S.; Shiga, T.; Hagiwara, N. Thyroid function on admission and outcome in patients hospitalized for acute decompensated heart failure. J. Cardiol. 2015, 66, 205–211. [Google Scholar] [CrossRef]
- Wang, W.; Guan, H.; Gerdes, M.; Iervasi, G.; Yang, Y.; Tang, Y. Thyroid status, cardiac function and mortality in patients with idiopathic dilated cardiomyopathy. J. Clin. Endocrinol. Metab. 2015, 100, 3210–3218. [Google Scholar] [CrossRef]
- Chen, S.; Shauer, A.; Zwas, D.R.; Lotan, C.; Keren, A.; Gotsman, I. The effect of thyroid function on clinical outcome in patients with heart failure. Eur. J. Heart Fail. 2014, 16, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Chuang, C.P.; Jong, Y.S.; Wu, C.Y.; Lo, H.M. Impact of triiodothyronine and N-terminal pro-B-type natriuretic peptide on the long term survival of critically ill patients with acute heart failure. Am. J. Cardiol. 2014, 113, 845–850. [Google Scholar] [CrossRef]
- Li, X.; Yang, X.; Wang, Y.; Ding, L.; Wang, J.; Hua, W. The prevalence and prognostic effects of subclinical thyroid dysfunction in dilated cardiomyopathy patients: A single-center cohort study. J. Card. Fail. 2014, 20, 506–512. [Google Scholar] [CrossRef]
- Perez, A.C.; Jhund, P.S.; Stott, D.J.; Gullestad, L.; Cleland, J.G.; van Veldhuisen, D.J.; Wikstrand, J.; Kjekshus, J.; McMurray, J.J. Thyroid-stimulating hormone and clinical outcomes: The CORONA trial (controlled rosuvastatin multinational study in heart failure). JACC Heart Fail. 2014, 2, 35–40. [Google Scholar] [CrossRef]
- Frey, A.; Kroiss, M.; Berliner, D.; Seifert, M.; Allolio, B.; Güder, G.; Ertl, G.; Angermann, C.E.; Störk, S.; Fassnacht, M. Prognostic impact of subclinical thyroid dysfunction in heart failure. Int. J. Cardiol. 2013, 168, 300–305. [Google Scholar] [CrossRef]
- Mitchell, J.E.; Hellkamp, A.S.; Mark, D.B.; Anderson, J.; Johnson, G.W.; Poole, J.E.; Lee, K.L.; Bardy, G.H. Thyroid function in heart failure and impact on mortality. JACC Heart Fail. 2013, 1, 48–55. [Google Scholar] [CrossRef]
- Passino, C.; Pingitore, A.; Landi, P.; Fontana, M.; Zyw, L.; Clerico, A.; Emdin, M.; Iervasi, G. Prognostic value of combined measurement of brain natriuretic peptide and triiodothyronine in heart failure. J. Card. Fail. 2009, 15, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Iacoviello, M.; Guida, P.; Guastamacchia, E.; Triggiani, V.; Forleo, C.; Catanzaro, R.; Cicala, M.; Basile, M.; Sorrentino, S.; Favale, S. Prognostic role of sub-clinical hypothyroidism in chronic heart failure outpatients. Curr. Pharm. Des. 2008, 14, 2686–2692. [Google Scholar] [CrossRef] [PubMed]
- Kozdag, G.; Ural, D.; Vural, A.; Agacdiken, A.; Kahraman, G.; Sahin, T.; Ural, E.; Komsuoglu, B. Relation between free triiodothyronine/free thyroxine ratio, echocardiographic parameters and mortality in dilated cardiomyopathy. Eur. J. Heart Fail. 2005, 7, 113–118. [Google Scholar] [CrossRef] [PubMed]
- Pingitore, A.; Landi, P.; Taddei, M.C.; Ripoli, A.; L’Abbate, A.; Iervasi, G. Triiodothyronine levels for risk stratification of patients with chronic heart failure. Am. J. Med. 2005, 118, 132136. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M.A.; Stevenson, L.W.; Luu, M.; Walden, J.A. Altered thyroid hormone metabolism in advanced heart failure. J. Am. Coll. Cardiol. 1990, 16, 91–95. [Google Scholar] [CrossRef]
- Lubrano, V.; Pingitore, A.; Carpi, A.; Iervasi, G. Relationship between triiodothyronine and proinflammatory cytokines in chronic heart failure. Biomed. Pharmacother. 2010, 64, 165–169. [Google Scholar] [CrossRef]
- Shen, Y.; Chen, G.; Su, S.; Zhao, C.; Ma, H.; Xiang, M. Independent Association of Thyroid Dysfunction and Inflammation Predicts Adverse Events in Patients with Heart Failure via Promoting Cell Death. J. Cardiovasc. Dev. Dis. 2022, 9, 290. [Google Scholar] [CrossRef]
- Cittadini, A.; Salzano, A.; Iacoviello, M.; Triggiani, V.; Rengo, G.; Cacciatore, F.; Maiello, C.; Limongelli, G.; Masarone, D.; Perticone, F.; et al. Multiple hormonal and metabolic deficiency syndrome predicts outcome in heart failure: The T.O.S.CA. Registry. Eur. J. Prev. Cardiol. 2021, 28, 1691–1700. [Google Scholar] [CrossRef] [PubMed]
- Mahal, S.; Datta, S.; Ravat, V.; Patel, P.; Saroha, B.; Patel, R.S. Does subclinical hypothyroidism affect hospitalization outcomes and mortality in congestive cardiac failure patients? Cureus 2018, 10, e2766. [Google Scholar] [CrossRef]
- Fontes, R.; Coeli, C.R.; Aguiar, F.; Vaisman, M. Reference interval of thyroid stimulating hormone and free thyroxine in a reference population over 60 years old and in very old subjects (over 80 years): Comparison to young subjects. Thyroid. Res. 2013, 6, 13. [Google Scholar] [CrossRef]
- Silva-Tinoco, R.; Castillo-Martínez, L.; Orea-Tejeda, A.; Orozco-Gutiérrez, J.J.; Vázquez-Díaz, O.; Montaño-Hernández, P.; Flores-Rebollar, A.; Reza-Albarrán, A. Developing thyroid disorders is associated with poor prognosis factors in patient with stable chronic heart failure. Int. J. Cardiol. 2011, 147, e24–e25. [Google Scholar] [CrossRef] [PubMed]
- Merla, R.; Martinez, J.D.; Martinez, M.A.; Khalife, W.; Bionat, S.; Bionat, J.; Barbagelata, A. Hypothyroidism and renal function in patients with systolic heart failure. Tex. Heart Inst. J. 2010, 37, 66–69. [Google Scholar]
- Drechsler, C.; Schneider, A.; Gutjahr-Lengsfeld, L.; Kroiss, M.; Carrero, J.J.; Krane, V.; Allolio, B.; Wanner, C.; Fassnacht, M. Thyroid function, cardiovascular events, and mortality in diabetic hemodialysis patients. Am. J. Kidney Dis. 2014, 63, 988–996. [Google Scholar] [CrossRef]
- Friberg, L.; Werner, S.; Eggertsen, G.; Ahnve, S. Rapid down-regulation of thyroid hormones in acute myocardial infarction: Is it cardioprotective in patients with angina? Arch. Intern. Med. 2002, 162, 1388–1394. [Google Scholar] [CrossRef]
- Wang, W.Y.; Tang, Y.D.; Yang, M.; Cui, C.; Mu, M.; Qian, J.; Yang, Y.J. Free triiodothyronine level indicates the degree of myocardial injury in patients with acute ST-elevation myocardial infarction. Chin. Med. J. 2013, 126, 3926–3929. [Google Scholar] [PubMed]
- Ceremuzyński, L.; Górecki, A.; Czerwosz, L.; Chamiec, T.; Bartoszewicz, Z. Herbaczyńska-Cedro Low serum triiodothyronine in acute myocardial infarction indicates major heart injury. K. Kardiol. Pol. 2004, 60, 468–480. [Google Scholar]
- Lymvaios, I.; Mourouzis, I.; Cokkinos, D.V.; Dimopoulos, M.A.; Toumanidis, S.T.; Pantos, C. Thyroid hormone and recovery of cardiac function in patients with acute myocardial infarction: A strong association? Eur. J. Endocrinol. 2011, 165, 107–114. [Google Scholar] [CrossRef]
- Reindl, M.; Feistritzer, H.J.; Reinstadler, S.J.; Mueller, L.; Tiller, C.; Brenner, C.; Mayr, A.; Henninger, B.; Mair, J.; Klug, G.; et al. Thyroid-stimulating hormone and adverse left ventricular remodeling following ST-segment elevation myocardial infarction. Eur. Heart J. Acute Cardiovasc. Care. 2019, 8, 717–726. [Google Scholar] [CrossRef]
- Han, C.; Xu, K.; Wang, L.; Zhang, Y.; Zhang, R.; Wei, A.; Dong, L.; Hu, Y.; Xu, J.; Li, W.; et al. Impact of persistent subclinical hypothyroidism on clinical outcomes in non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention. Clin. Endocrinol. 2022, 96, 70–81. [Google Scholar] [CrossRef]
- Brozaitiene, J.; Mickuviene, N.; Podlipskyte, A.; Burkauskas, J.; Bunevicius, R. Relationship and prognostic importance of thyroid hormone and N-terminal pro-B-Type natriuretic peptide for patients after acute coronary syndromes: A longitudinal observational study. Cardiovasc. Disord. 2016, 16, 45. [Google Scholar] [CrossRef]
- Yu, T.; Tian, C.; Song, J.; He, D.; Wu, J.; Wen, Z.; Sun, Z.; Sun, Z. Value of the fT3/fT4 ratio and its combination with the GRACE risk score in predicting the prognosis in euthyroid patients with acute myocardial infarction undergoing percutaneous coronary intervention: A prospective cohort study. BMC Cardiovasc. Disord. 2018, 18, 181. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Ma, W.; Huang, S.; Lin, X.; Yu, M. Impact of low triiodothyronine syndrome on long-term outcomes in patients with myocardial infarction with nonobstructive coronary arteries. Ann. Med. 2021, 53, 741–749. [Google Scholar] [CrossRef] [PubMed]
- Pingitore, A.; Chen, Y.; Gerdes, A.M.; Iervasi, G. Acute myocardial infarction and thyroid function: New pathophysiological and therapeutic perspectives. Ann. Medicine. Ann. Med. 2012, 44, 745–757. [Google Scholar] [CrossRef] [PubMed]
- Amin, A.; Chitsazan, M.; Taghavi, S.; Ardeshiri, M. Effects of triiodothyronine replacement therapy in patietns with chronic stable heart failure and low-triidotrhyronine syndrome: A randomized, double-blind, placebo-controlled study. ESC Heart Fail. 2015, 2, 5–11. [Google Scholar] [CrossRef]
- Holmager, P.; Schmidt, U.; Mark, P.; Andersen, U.; Dominguez, H.; Raymond, I.; Zerahn, B.; Nygaard, B.; Kistorp, C.; Faber, J. Long-term L-Triiodothyronine (T3) treatment in stable systolic heart failure patients: A randomised, double-blind, cross-over, placebo-controlled intervention study. Clin. Endocrinol. 2015, 83, 931–937. [Google Scholar] [CrossRef]
- Curotto Grasiosi, J.C.; Peressotti, B.; Machado, R.A.; Filipini, E.C.; Angel, A.; Delgado, J.; Quiroga, G.A.C.; Mansilla, C.R.; Quesada, M.D.M.M.; Degregorio, A.; et al. Improvement in functional capacity after levothyroxine treatment in patients with chronic heart failure and sublinical hypothyroidism. Endocrinol. Nutr. 2013, 60, 427–432. [Google Scholar] [CrossRef]
- Goldman, S.; McCarren, M.; Morkin, E.; Ladenson, P.W.; Edson, R.; Warren, S.; Ohm, J.; Thai, H.; Churby, L.; Barnhill, J.; et al. DITPA (3,5-Diiodothyropropionic Acid), a thyroid hormone analog to treat heart failure: Phase II trial veterans affairs cooperative study. Circulation 2009, 119, 3093–3100. [Google Scholar] [CrossRef]
- Pingitore, A.; Galli, E.; Barison, A.; Iervasi, A.; Scarlattini, M.; Nucci, D.; L’Abbate, A.; Mariotti, R.; Iervasi, G. Acute effects of triiodothyronine (T3) replacement therapy in patients with chronic heart failure and low-T3 syndrome: A randomized, placebo-controlled study. J. Clin. Endocrinol. Metab. 2008, 93, 1351–1358. [Google Scholar] [CrossRef]
- Iervasi, G.; Emdin, M.; Colzani, R.M.P.; Placidi, S.; Sabatino, L.; Scarlattini, M.; Formichi, B. Beneficial effects of long-term triiodothyronine (T3) infusion in patients with advanced heart failure and low T3 syndrome. In Proceedings of the 2nd International Congress on Heart Disease—New Trends in Research, Diagnosis and Treatment, Washington, DC, USA, 21–24 July 2001; Kimchi, A., Ed.; Medimond Medical Publications: Englewood, NJ, USA, 2001; pp. 549–553. [Google Scholar]
- Malik, F.S.; Mehra, M.R.; Uber, P.A.; Park, M.H.; Scott, R.L.; Van Meter, C.H. Intravenous thyroid hormone supplementation in heart failure with cardiogenic shock. J. Card. Fail. 1999, 5, 31–37. [Google Scholar] [CrossRef]
- Hamilton, M.A.; Stevenson, L.W.; Fonarow, G.C.; Steimle, A.; Goldhaber, J.I.; Child, J.S.; Chopra, I.J.; Moriguchi, J.D.; Hage, A. Safety and hemodynamic effects of intravenous triiodothyronine in advanced congestive heart failure. Am. J. Cardiol. 1998, 81, 443–447. [Google Scholar] [CrossRef]
- Moruzzi, P.; Doria, E.; Agostoni, P.G. Medium-term effectiveness of L-thyroxine treatment in idiopathic dilated cardiomyopathy. Am. J. Med. 1996, 101, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Shi, C.; Bao, Y.; Chen, X.; Tian, L. The Effectiveness of Thyroid Hormone Replacement Therapy on Heart Failure and Low-Triiodothyronine Syndrome: An Updated Systematic Review and Meta-analysis of Randomized Controlled Trials. Endocr. Pract. 2022, 28, 1178–1186. [Google Scholar] [CrossRef]
- Chen, X.; Bao, Y.; Shi, C.; Tian, L. Effectiveness and Safety of Thyroid Hormone Therapy in Patients with Dilated Cardiomyopathy: A Systematic Review and Meta-analysis of RCTs. Am. J. Cardiovasc. Drugs. 2022, 22, 647–656. [Google Scholar] [CrossRef]
- Pingitore, A.; Mastorci, F.; Piaggi, P.; Aquaro, G.D.; Molinaro, S.; Ravani, M.; De Caterina, A.; Trianni, G.; Ndreu, R.; Berti, S.; et al. Usefulness of Triiodothyronine Replacement Therapy in Patients With ST Elevation Myocardial Infarction and Borderline/Reduced Triiodothyronine Levels (from the THIRST Study). Am. J. Cardiol. 2018, 123, 905–912. [Google Scholar] [CrossRef]
- Pantos, C.I.; Trikas, A.G.; Pissimisis, E.G.; Grigoriou, K.P.; Stougiannos, P.N.; Dimopoulos, A.K.; Linardakis, S.I.; Alexopoulos, N.A.; Evdoridis, C.G.; Gavrielatos, G.D.; et al. Effects of Acute Triiodothyronine Treatment in Patients with Anterior Myocardial Infarction Undergoing Primary Angioplasty: Evidence from a Pilot Randomized Clinical Trial (ThyRepair Study). Thyroid 2022, 32, 714–724. [Google Scholar] [CrossRef] [PubMed]
- Jabbar, A.; Ingoe, L.; Junejo, S.; Carey, P.; Addison, C.; Thomas, H.; Parikh, J.D.; Austin, D.; Hollingsworth, K.G.; Stocken, D.D.; et al. Effect of Levothyroxine on Left Ventricular Ejection Fraction in Patients With Subclinical Hypothyroidism and Acute Myocardial Infarction: A Randomized Clinical Trial. JAMA 2020, 324, 249–258. [Google Scholar] [CrossRef] [PubMed]
- Tharmapoopathy, M.; Thavarajah, A.; Kenny, R.P.W.; Pingitore, A.; Iervasi, G.; Dark, J.; Bano, A.; Razvi, S. Efficacy and Safety of Triiodothyronine Treatment in Cardiac Surgery or Cardiovascular Diseases: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Thyroid 2022, 32, 879–896. [Google Scholar] [CrossRef]
- Gerdes, A.M.; Portman, M.A.; Iervasi, G.; Pingitore, A.; Cooper, D.K.C.; Novitzky, D. Ignoring a basic pathophysiological mechanism of heart failure progression will not make it go away. Am. J. Physiol. Heart Circ. Physiol. 2021, 320, H1919–H1922. [Google Scholar] [CrossRef]

| TH Dysfunction | Events (n) | N° PTS (W,%) | Age (yy) | LVEF (%) | NYHA Class III-IV | Prognostic Weight | Ref. |
|---|---|---|---|---|---|---|---|
| fT3/fT4 ratio < 2.15 | Cardiac death, Transplantation, LV device implantation | 3257 (18) | 57 | ND | ND | HR values of FT3/FT4 ratio predicting the risk of composite endpoint in pts with LVEF <40%, 40–49%, and ≥50% were 0.91, 0.83, and 0.65, respectively | [75] |
| fT3/fT4 cutoff 0.233 | CV death (29%), Overall death (25%) | 8887 (46) | 69 | 50 | 85% | HR of all-cause mortality and CV death for pts with a high FT3/FT4 ratio was 0.841 and 0.844 times less than that in pts with a low FT3/FT4 ratio | [76] |
| TSH > 4.70 mIU/L, TSH < 0.35 mIU/L. | Overall death | 4992 (45) | 74 | ND | 34% | Hypothyroidism (HR 1.259) and hyperthyroidism (HR 1.21) had a greater risk of death compared to euthyroidism. | [77] |
| LT3, Hypothyroidism | Overall death | 762 | ND | ND | ND | Independent association with death significant in pts with TSH >10 mIU/L. LT3 was independently associated with HF hospitalization and death | [78] |
| SCH: (TSH 4–10 microUI/mL), HYPO: (TSH > 10 microUI/mL), LT3: (fT3 < 1.8 pg/mL) | In-hospital death | 1018 (55) | 81 | ND | 80% | Mortality rate was 27% among HYPO pts, 17% in SCH pts, and 11% among euthyroid pts. HYPO (HR 2.1) and fT3 levels (HR 3.4) were associated with an increased likelihood of in-hospital death. | [74] |
| TSH quartiles (≤1.3; 1.4–2.2; 2.3–3.5; ≥3.6 mlU/L) | Cardiac death (28), Non-Cardiac death (30) HF impairment (40), Cardiac transplantation (11), Ventricular arrhythmias (24) | 180 (21) | 37 | 28 | 35% | Serum TSH levels (>2.67 nIU/L) may provide help for the stratification of the risk of ventricular arrhythmias | [79] |
| LT3:fT3 ≤ 2.03 pg/mL | CV death (88), non-CV death (105) | 911 (41) | 68 | 60 | 3% | LT3 at discharge is associated with higher cardiac and all cause-mortality, accompanied by high central venous pressure, lower nutritional status, and impaired exercise capacity | [80] |
| SCH:TSH > 4.51 mlU/L; LT3: total T3 < 80 ng/dL | Cardiac transplantation (104), VAD replacement (31), Overall death (327) | 1365 (35) | 57 | 34 | No data | SCH (HR 1.82) and LT3 (HR 2.12) were associated with increased risk of composite endpoint | [81] |
| SCH:TSH > 4 µlU/mL | Worsening HF (232), CV death (108), non-CV death (128) | 1043 (41) | 67 | 42 | 3% | SCH is an independent predictor of cardiac event (HR 1.42) and all-cause mortality (1.421) after adjustment with other confounders | [82] |
| fT3 < 3.00 pmol/L | CV death (30), non-CV death (6), Hospitalization (45) | 113 (3.5) | 61 | 31 | 64% | Patients with fT3 < 3.00 pmol/L had higher overall mortality and HF hospitalization | [83] |
| SCH: TSH of 4.5 to 19.9mIU/L; SHY: TSH < 0.45 mIU/L | CV death (27), Rehospitalization (80) | 274 (70) | 70 | 39 | 100% | Higher TSH is independently associated with composite CV events. SCH is an independent predictor (HR: 2.31) of composite CV events | [84] |
| fT3 < 2.77 pg/mL | CV death (19), non-CV death (4) | 71 (34) | 54 | 26 | No data | FT3 < 2.77 pg/mL was identified as predictor of events (HR: 8.623) | [85] |
| LT3:fT3 ≤ 2.05 pg/mL | CV death (16), non-CV death (10) | 270 (31) | 68 | 67 | 100% | LT3 on admission is associated with higher in-hospital all-cause, cardiac, and non-cardiac death rates and with increased 1-year death | [86] |
| LT3:fT3 < 1.79 pg/mL; SCH: TSH > 4.78 mlU/L normal fT3 and or fT4; SHY: TSH < 0.55 mlU/L and normal fT3 and or fT4; HYPO: TSH > 4.78 mlU/L and <fT3 and or Ft4 | non-CV death (ND) | 458 (29) | 51 | 32 | ND | HYPO was the strongest predictor of death (HR 4.189), followed by LT3 (HR 3.147) and SHYPO (HR 2.869) | [87] |
| TSH quartiles (≤1.3; 1.4–2.2; 2.3–3.5; ≥3.6 mlU/L) | CV death (ND) CV hospitalization (ND) | 5599 (51) | 75 | <50 | ND | Increased risk of death in the highest TSH group (HR 1.54). TSH as an independent predictor of the combined endpoint | [88] |
| Total T3 ≤ 52.3 ng/dL | CV death (38), non-CV death (16) | 144 (49) | 71 | 42 | 100% | T3 as independent predictors for both all-cause and cardiac mortalities among critically ill patients with HF, and high NT-proBNP and low T3 levels predict a worse long-term outcome | [89] |
| SHY: TSH < 0.35 µIU/mL SCH: TSH > 5.5 µIU/mL | Overall death | 963 (26) | 52 | 32 | 72% | SHY, SCH have higher all-cause mortality rates. However, only SHY (HR 1.793), not SCH, is an independent predictor for increased risk of overall death | [90] |
| SHY: TSH < 0.3 µIU/mL SCH: TSH > 5.0 µIU/mL | CV death (1104), Hospitalization (1210), non-CV death (1402) | 4750 (22) | 73 | 31 | 63% | SCH associated with an increased risk of the composite outcome of CV death or HF hospitalization (HR: 1.29), as well as all-cause death (HR: 1.36). When NT-proBNP was added to the predictive models, the association between SCH and all outcomes was eliminated | [91] |
| LT3: fT3 < 2.7 pmol/L SHY: TSH < 0.3 mIU/L SCH: TSH > 4.0 mIU/L HYPER: TSH < 0.1 mIU/L HYPO: TSH > 4.0 mIU/L | CV death (153), non-CV death (111) | 758 (29) | 68 | 30 | ND | SCH, SHY; HYPO, HYPER are not relevant prognostic factors. LT3 is a significant indicator of poor prognosis | [92] |
| HYPO (>5.0 μU/mL), HYPER (<0.3 μU/mL) | non-CV death (ND) | 2225 (48) | 59 | 24 | ND | HYPO and HYPER were associated with 58% and 85% increases in the risk for death (HR: 1.58; HR: 1.85) | [93] |
| LT3: fT3 < 2.1 ng/L | CV death (64), non-CV death (46) | 442 (25) | 65 | 33 | 37% | Pts with LT3 and higher BNP showed the highest risk of all-cause and cardiac death | [94] |
| SCH: TSH > 5.5 mlU/L | Hospitalization (55), non-CV death (18), transplantation (6) | 338 (33) | 64 | 32 | ND | TSH levels, even slightly above normal range, are independently associated with a greater likelihood of HF progression | [95] |
| fT3/fT4 ratio ≤ 1.7 | CV death (15), VF (1) | 111 (31) | 62 | 29 | ND | fT3/fT4 ratio ≤ 1.7 was associated with an increased risk of mortality, independent of other prognostic markers. Sensitivity, specificity, positive and negative predictivity of fT3/fT4 ratio ≤ 1.7 for cardiac mortality were 100%, 71%, 36%, and 100% | [96] |
| free T3, 3.2 to 6.5 pmol/L (2 to 4.2 pg/mL); | CV death (47), non-CV death (17) | 281 (17) | 68 | 28 | ND | Low T3 levels are an independent predictor of mortality, adding prognostic information to conventional clinical (age) and functional cardiac parameters (LVEF) | [97] |
| fT3/reverseT3 ratio ≤ 4 | Cardiac death (17), Transplantation (6) | 84 (16) | 50 | 18 | 100% | A low fT3/reverse T3 ratio was a predictor of cardiac events, with a survival rate of 37%. The lowest ratio was associated with the poorest prognosis | [98] |
| Patients (N) | Study Design | LVEF (%) | TH Dose Treatment | Main Findings | Ref. |
|---|---|---|---|---|---|
| 39 ischemic and non-ischemic HF and LT3 | Randomized, prospective, double-blind, placebo-controlled | 31 ± 6 | T3 0.025 mg/day, OS | Improvement in NYHA class, ↑ LVEF, ↓ LVESV, ↓ NT-proBNP, ↓ hs-C-reactive protein, ↑ 6-MWD | [117] |
| 13 ischemic and non-ischemic HF and LT3 | Randomized, double-blind, cross-over, placebo-controlled | 43 (37–52) | Oral T3 twice daily for 3 months (tablet dose 20 µg) | No clinical or functional benefit observed | [118] |
| 163 ischemic, non-ischemic HF, SCH | Uncontrolled | N/A | T4 dose necessary to normalize TSH | ↑ Physical performance at 6 min walking test | [119] |
| 86 ischemic and non-ischemic HF | Randomized (2:1) placebo-controlled | 28 ± 6 | DTPA twice daily 90 mg increments (every 2 wks to maximum 360 mg) | ↑ CI ↓ SVR, lipoproteins, and cholesterol | [120] |
| 20 ischemic and non-ischemic HF and LT3 | Randomized, placebo-controlled | 25 (18–32) | T3 3 days continuously infused (initial dose 20 g/m2) | ↑ LVSV, LVEDV, ↓ NT-proBNP, Aldosterone, NA | [121] |
| 6 ischemic and non-ischemic HF | Uncontrolled | 24 ± 3 | T3 initial dose 20 mg/m2bs/d Continuous infusion (4 d) | ↓SVR ↑ CO and UO | [122] |
| 10 cardiogenic shock | Uncontrolled | N/A | T4 20 mg/h bolus + continuous infusion (36 h) | ↑ CI, PCWP, and MAP | [123] |
| 23 ischemic and non-ischemic HF | Uncontrolled | 22 ± 1 | T3 cumulative dose 0.15–2.7 mg/kg bolus + continuous infusion (6–12 h) | ↓ SVR ↑ CO | [124] |
| 10 non-ischemic HF | Randomized (1:1) placebo-controlled | 29 ± 6 | T4 100 mg/d OS for 3 months | Improvement in cardiovascular performance at rest, exercise, and dobutamine stress test | [125] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pingitore, A.; Mastorci, F.; Lazzeri, M.F.L.; Vassalle, C. Thyroid and Heart: A Fatal Pathophysiological Attraction in a Controversial Clinical Liaison. Endocrines 2023, 4, 722-741. https://doi.org/10.3390/endocrines4040053
Pingitore A, Mastorci F, Lazzeri MFL, Vassalle C. Thyroid and Heart: A Fatal Pathophysiological Attraction in a Controversial Clinical Liaison. Endocrines. 2023; 4(4):722-741. https://doi.org/10.3390/endocrines4040053
Chicago/Turabian StylePingitore, Alessandro, Francesca Mastorci, Maria Francesca Lodovica Lazzeri, and Cristina Vassalle. 2023. "Thyroid and Heart: A Fatal Pathophysiological Attraction in a Controversial Clinical Liaison" Endocrines 4, no. 4: 722-741. https://doi.org/10.3390/endocrines4040053
APA StylePingitore, A., Mastorci, F., Lazzeri, M. F. L., & Vassalle, C. (2023). Thyroid and Heart: A Fatal Pathophysiological Attraction in a Controversial Clinical Liaison. Endocrines, 4(4), 722-741. https://doi.org/10.3390/endocrines4040053








