Current Impact and Long-Term Influence of the COVID-19 Pandemic on Iraqi Healthcare Systems: A Case Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Data Extraction
3. Case study
3.1. Case Presentation
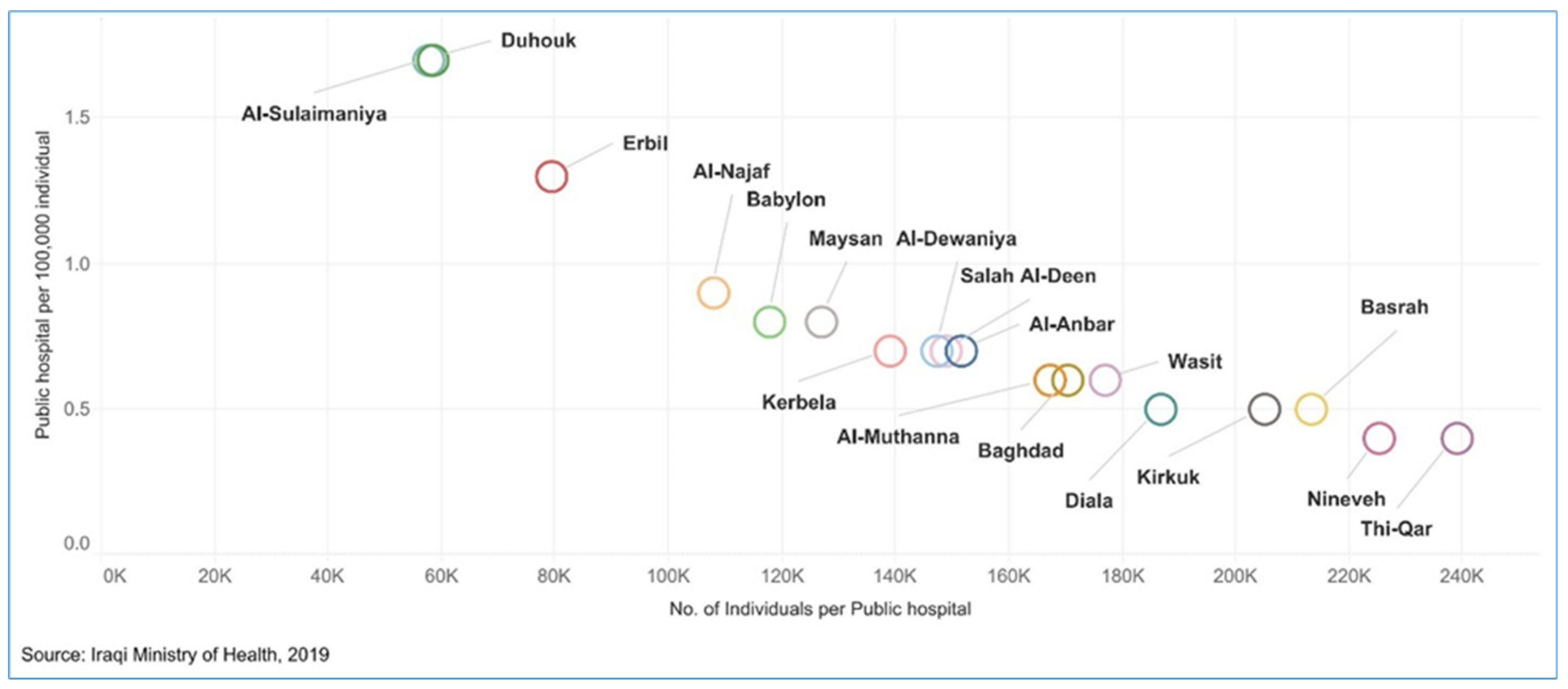
3.1.1. Service Delivery
3.1.2. Health Workforce
3.1.3. Health Information
3.1.4. Medical Products, Vaccines, and Technologies
3.1.5. Health Financing
3.1.6. Leadership and Governance
3.2. COVID-19 Case Importation
3.3. Management and Outcomes of COVID-19 in Iraq
3.4. Current Impact and Long-Term Influence of the COVID-19 Pandemic on Global and Public Health and Healthcare System
3.4.1. Vaccine-Preventable Diseases (VPDs)
3.4.2. Violence
Gender-Based Violence (GBV)
Violence against Health Care Providers (HCPs)
3.4.3. Mental Health
3.4.4. Impact of COVID-19 on Elective Medical Procedures
4. Discussion
- Immunization campaigns should be data-driven, people-centered, and flexible according to the local context. Additionally, enhancing VPDs surveillance and providing an adequate supply of PPE and vaccines are also important [117]. Moreover, planning an integrated vaccination campaign during COVID-19 vaccination is essential to avoid the accumulation of individuals with immunity gaps, as children might grow out of the target age for specific vaccines [105].
- Empowering girls and women by providing equal opportunities in the educational, economic, and political sectors; inclusion of GBV risk mitigation strategies as part of the COVID-19 response plan [118,119]; capacity building; cross-sector collaboration at all levels; scaling up of some of the local initiatives to other regions in Iraq; and increasing funding to GBV programs.
- Addressing violence against HCWs through different approaches, such as teaching de-escalation techniques; improving communication skills; limiting the number of patients’ visitors or restricting their movement within a health facility; implementing structural changes to the medical units; reducing waiting times; improving the quality of care; increasing the availability of medicines; and enhancing security and preventing the carrying of weapons inside health facilities [88,120,121].
- The implementation and expansion of telemedicine to offer mental health services, as evidence shows that telemedicine increases access to care; reduces travel and waiting times; and offers additional security measures to mental health professionals [122]. Additionally, the availability of digital applications can be used to screen for mental health disorders. The expansion and inclusion of mental health services at PHCs is another option. Mental health first aid training to HCWs, community engagement to raise awareness about mental health, and educational campaigns to normalize mental health should be considered. HCWs’ mental wellbeing should be a priority; some of the recommended strategies include setting health policies that support them financially and psychologically, such as decreasing shift hours to reduce exposure to COVID-19 patients, providing adequate PPE, ongoing education and workshops, and providing mental health resources [91,122].
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Details about the Search Methods Used in This Article
| Research Question | Databases | Limits |
|---|---|---|
| Current Impact and Long-Term Influence of the COVID-19 Pandemic on Global and Public Health, Public Policy, and Healthcare Systems: Socio-Economic Aspects—Iraq | PubMed Cochrane World Health Organization |
| Concept: COVID-19 | Concept: Iraq | Concept: Global Public Health | |
|---|---|---|---|
| Thesaurus Terms/Subheadings | “SARS-CoV-2” [MeSH] OR “COVID-19 Vaccines” [Mesh] OR “COVID-19”[Mesh] OR | “Iraq”[MeSH] OR | “Global Health” [MeSH] OR “Public Health”[MeSH] OR “Public Policy” [MeSH] OR “Delivery of Health Care”[Mesh] OR |
| Textwords | “SARS Coronavirus 2” OR “Coronavirus 2, SARS” OR “Coronavirus disease 2019 virus” OR “2019 Novel Coronavirus” OR “2019 Novel coronaviruses” OR “Coronavirus, 2019 Novel” OR “SARs-CoV-2 Virus” OR “SARS CoV 2 Virus” OR “SARS-CoV-2 Viruses” OR “Virus, SARS-CoV-2” OR “2019-nCoV” OR “COVID-19 virus” OR “COVID-19 Virus” OR “COVID 19 Virus” OR “COVID-19 Viruses” OR “Virus, COVID-19” OR “COVID-19” OR “COVID-19 vaccine” OR “COVID-19 cases” OR “COVID-19 deaths” OR “COVID-19 death” OR “COVID-19 timeline” | Iraq | “Global Health” OR “Public Health” OR “Public Policy” OR “Healthcare systems” OR “System, health care” OR “Health care system” OR “Health care systems” OR “Systems, Health Care” OR “Systems healthcare” OR “Census” OR “Population” OR “Geography” OR Demography OR Economy OR “Socioeconomic distribution” OR “Vector Ecology OR “Pandemic Response” OR “Pandemic Preparedness” OR “Pandemic Crises” OR “Anti-Science” OR “Anti-Vaccination” OR “Epidemiological curve” OR “Community strategies” OR “Social distancing” OR “Government Intervention” OR “Nonphamaceutical interventions” OR Vaccines OR “Testing capacity” OR Underreporting |
| Concept: COVID-19 | Concept: Iraq | Concept: Global Public Health | |
|---|---|---|---|
| Thesaurus Terms/ Subheadings | “SARS-CoV-2”[MeSH] OR “COVID-19 Vaccines”[MeSH] OR “COVID-19”[MeSH] OR | “Iraq”[MeSH] OR | “Global Health”[MeSH] OR “Public Health”[MeSH] OR “Public Policy” [MeSH] OR “Delivery of Health Care”[Mesh] |
| Textwords | “SARS Coronavirus 2” OR “Coronavirus 2, SARS” OR “Coronavirus disease 2019 virus” OR “2019 Novel Coronavirus” OR “2019 Novel coronaviruses” OR “Coronavirus, 2019 Novel” OR “SARS-CoV-2- Virus” OR “SARS CoV 2 Virus” OR “SARS-CoV-2 Viruses” OR “Virus, SARS-CoV-2” OR “2019-nCoV” OR “COVID-19 virus” OR “COVID-19 Virus” OR “COVID 19 Virus” OR “COVID-19 Viruses” OR “Virus, COVID-19” OR “COVID-19” OR “COVID-19 vaccine” OR “COVID-19 cases” OR “COVID-19 deaths” OR “COVID-19 death” OR “COVID-19 timeline” | Iraq | Global Health OR Public Health OR Public Policy OR Healthcare systems “System, health care” “Health care system” “Health care systems” “Systems, Health Care” “Systems healthcare” “Census” OR “Population” OR “Geography” OR Demography OR Economy OR Socioeconomic distribution OR Vector Ecology OR Pandemic Response OR Pandemic Preparedness OR Pandemic Crises OR Anti-Science OR Anti-Vaccination OR Epidemiological curve OR Community strategies OR Social distancing OR Government Intervention OR Nonphamaceutical interventions OR Vaccines OR Testing capacity OR Underreporting |
References
- Durrani, H. Healthcare and healthcare systems: Inspiring progress and future prospects. Mhealth 2016, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The World Health Report 2000: Health Systems: Improving Performance; World Health Organization: Geneva, Switzerland, 2000; pp. 23–24. [Google Scholar]
- World Health Organization. Everybody Business: Strengthening Health Systems to Improve Health Outcomes: WHO’s Framework for Action; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Manyazewal, T. Using the World Health Organization health system building blocks through survey of healthcare professionals to determine the performance of public healthcare facilities. Arch. Public Health 2017, 75, 50. [Google Scholar] [CrossRef] [PubMed]
- Henderson, A. The Coalition Provisional Authority’s Experience with Economic Reconstruction in Iraq; United States Institute of Peace: Washington, DC, USA, 2005. [Google Scholar]
- Al Hilfi, T.K.; Lafta, R.; Burnham, G. Health services in Iraq. Lancet 2013, 381, 939–948. [Google Scholar] [CrossRef]
- Khedery, A. Iraq in Pieces. Foreign Aff. 2015, 94, 33–41. [Google Scholar]
- World Health Organization. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Khidir, K.A. COVID-19 Outbreak: The Kurdistan Region Perspective. Biochem. Cell. Arch. 2021, 21, 3133–3141. [Google Scholar]
- Aslam, M.M. Decoding COVID-19: How the outbreak may impact world’s security. AIP Conf. Proc. 2021, 2339, 020097. [Google Scholar] [CrossRef]
- Al-Khuzaie, M.M. Change monitoring and assessment of health capacity of Iraq due to COVID-19 by application of GIS techniques. J. Phys. Conf. Ser. 2021, 1895, 012004. [Google Scholar] [CrossRef]
- Neogi, S.B.; Pandey, S.; Preetha, G.S.; Swain, S. The predictors of COVID-19 mortality among health systems parameters: An ecological study across 203 countries. Health Res. Policy Syst. 2022, 20, 75. [Google Scholar] [CrossRef]
- Waitzberg, R.; Hernández-Quevedo, C.; Bernal-Delgado, E.; Estupiñán-Romero, F.; Angulo-Pueyo, E.; Theodorou, M.; Kantaris, M.; Charalambous, C.; Gabriel, E.; Economou, C.; et al. Early health system responses to the COVID-19 pandemic in Mediterranean countries: A tale of successes and challenges. Health Policy 2022, 126, 465–475. [Google Scholar] [CrossRef]
- World Health Organization. Health System Strengthening. Available online: https://www.emro.who.int/iraq/priority-areas/health-system-strengthening.html (accessed on 16 July 2022).
- United Nations. Iraq Common Country Analysis (2022—Condensed Version); United Nations. 2022. Available online: https://iraq.un.org/sites/default/files/2022-07/CCA%20Iraq%20-%20Condensed.pdf (accessed on 27 July 2022).
- MoH. National Health Policy. 2014. Available online: https://extranet.who.int/countryplanningcycles/sites/default/files/planning_cycle_repository/iraq/iraqs_national_health_policy_2014-2023.pdf (accessed on 26 July 2022).
- Duran, D.; Menon, R. Mitigating the Impact of COVID-19 and Strengthening Health Systems in the Middle East and North Africa; World Bank: Washington, DC, USA, 2020. [Google Scholar]
- Bank, T.W. Data for Iraq. Available online: https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?locations=IQ (accessed on 25 July 2022).
- Mac Skelton and Abdulameer Mohsin Hussein. Medicine Under Fire: How Corruption Erodes Healthcare in Iraq; Konrad-Adenauer-Stiftung: Berlin, Germany, 2021. [Google Scholar]
- Burnham, G.; Hoe, C.; Hung, Y.W.; Ferati, A.; Dyer, A.; Hifi, T.A.; Aboud, R.; Hasoon, T. Perceptions and utilization of primary health care services in Iraq: Findings from a national household survey. BMC Int. Health Hum. Rights 2011, 11, 15. [Google Scholar] [CrossRef]
- Al Hilfi, T.K. Toward a healthier Iraq. Yale J. Biol. Med. 2014, 87, 289–297. [Google Scholar]
- Price, R.A. Iraqi State Capabilities; Institute of Development Studies: Brighton, UK, 2018. [Google Scholar]
- Fouad, F.M.; Soares, L.; Diab, J.L.; Abouzeid, A. The political economy of health in conflict: Lessons learned from three states in the Eastern Mediterranean Region during COVID-19. J. Glob. Health 2022, 12, 07001. [Google Scholar] [CrossRef]
- Karadaghi, G.; Willott, C. Doctors as the governing body of the Kurdish health system: Exploring upward and downward accountability among physicians and its influence on the adoption of coping behaviours. Hum. Resour. Health 2015, 13, 43. [Google Scholar] [CrossRef]
- KAPITA. Iraqi Health Sector Overview; KAPITA: Baghdad, Iraq, 2021. [Google Scholar]
- World Health Organization. The Global Health Observatory. Available online: https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/sdg-target-3.c-health-workforce (accessed on 16 July 2022).
- Aziz, C. Struggling to rebuild Iraq’s health-care system. War, sanctions, and mismanagement have left health system in shambles. Lancet 2003, 362, 1288–1289. [Google Scholar] [CrossRef]
- Regional Office for the Eastern Mediterranean, World Health Organization. Health Workforce Snapshot. Available online: https://rho.emro.who.int/Briefs/iraq-snapshot-2020 (accessed on 17 July 2022).
- World Health Organization. Comprehensive Assessment of Iraq’s Health Information System 2019; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Ministry of Planning. National Development Plan 2013–2017; Ministry of Planning: Baghdad, Iraq, 2013. Available online: https://planipolis.iiep.unesco.org/sites/default/files/ressources/iraq_national_development_plan_2013-2017.pdf (accessed on 12 July 2022).
- World Health Organization. Country Cooperation Strategy for World Health Organization and Iraq 2012–2017; Regional Office for the Eastern Mediterranean, World Health Organization: Cairo, Egypt, 2013. [Google Scholar]
- Al-Jumaili, A.; Younus, M.; Kannan, Y.; Nooruldeen, Z.; Al-Nuseirat, A. Pharmaceutical regulations in Iraq: From medicine approval to post-marketing. East. Mediterr. Health J. 2021, 27, 1007–1015. [Google Scholar] [CrossRef]
- Ali, A. Renal Transplantation in Iraq. Transplantation 2021, 105, 1131–1134. [Google Scholar] [CrossRef]
- Al-Mosawi, A. Iraq healthcare system: An update. LOJ Med. Sci. (LOJMS) 2020, 4, 404–411. [Google Scholar] [CrossRef]
- Karen Langhauser, K. Corruption and Political Unrest Create a Challenging—But Not Impossible—Pharma Environment. Available online: https://www.pharmamanufacturing.com/articles/2020/global-dose-focus-on-iraq/ (accessed on 28 July 2022).
- World Health Organization. The Global Health Observatory. Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/current-health-expenditure-(che)-per-capita-in-us$ (accessed on 17 July 2022).
- Akinyemi, O.O.; Popoola, O.A.; Fowotade, A.; Adekanmbi, O.; Cadmus, E.O.; Adebayo, A. Qualitative exploration of health system response to COVID-19 pandemic applying the World Health Organization health systems framework: Case study of a Nigerian state. Sci. Afr. 2021, 13, e00945. [Google Scholar] [CrossRef]
- Regional Office for the Eastern Mediterranean, World Health Organization. Iraq Health Profile 2015; World Health Organization: Geneva, Switzerland, 2017; Available online: https://rho.emro.who.int/sites/default/files/Profiles-briefs-files/EMROPUB_EN_19621_IRQ.pdf (accessed on 17 July 2022).
- Government of Iraq. Iraqi Government Announces Preventative Measures in Response to Coronavirus. 2020. Available online: https://gds.gov.iq/iraqi-government-announces-preventative-measures-in-response-to-coronavirus/ (accessed on 18 July 2022).
- Government of Iraq. Novel Coronavirus (COVID-19): Iraq’s Ministry of Health Guidance to the Public. 2020. Available online: https://gds.gov.iq/novel-coronavirus-%e2%80%aacovid-19-iraqs-ministry-of-health-guidance-to-the-public/ (accessed on 18 July 2022).
- Aziz, P.Y.; Hadi, J.M.; Sha, A.M.; Aziz, S.B.; Rahman, H.S.; Ahmed, H.A.; Abdulla, M.A.; Amine Ali, S.M. The strategy for controlling COVID-19 in Kurdistan Regional Government (KRG)/Iraq: Identification, epidemiology, transmission, treatment, and recovery. Int. J. Surg. Open 2020, 25, 41–46. [Google Scholar] [CrossRef]
- Abdulah, D.M.; Aziz Qazli, S.S.; Suleman, S.K. Response of the Public to Preventive Measures of COVID-19 in Iraqi Kurdistan. Disaster Med. Public Health Prep. 2021, 15, e17–e25. [Google Scholar] [CrossRef]
- Government of Iraq. Prime Minister Chairs First Meeting of Higher Committee for Health and National Safety. 2020. Available online: https://gds.gov.iq/prime-minister-chairs-first-meeting-of-higher-committee-for-health-and-national-safety/ (accessed on 18 July 2022).
- World Health Organization. COVID-19 Dynamic Infographic Dashboard Iraq 2020–2022; World Health Organization: Geneva, Switzerland, 2020; Available online: https://app.powerbi.com/view?r=eyJrIjoiNjljMDhiYmItZTlhMS00MDlhLTg3MjItMDNmM2FhNzE5NmM4IiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9 (accessed on 18 July 2022).
- Alatrany, S.S.; Ogden, R.; Falaiyah, A.M.; HAS, A.L.; Alatrany, A.S. The passage of time in Iraq during the COVID-19 pandemic. PLoS ONE 2022, 17, e0266877. [Google Scholar] [CrossRef] [PubMed]
- Al-Malkey, M.K.; Al-Sammak, M.A. Incidence of the COVID-19 in Iraq—Implications for travellers. Travel Med. Infect. Dis. 2020, 38, 101739. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, M.; Kolo, K.; Aspoukeh, P.; Hamad, R.; Bailey, J.R. Time Series Modelling and Simulating the Lockdown Scenarios of COVID-19 in Kurdistan Region of Iraq. J. Infect. Dev. Ctries. 2021, 15, 370–381. [Google Scholar] [CrossRef] [PubMed]
- Khalid, H.S. Newroz from Kurdish and Persian Perspectives—A Comparative Study. J. Ethn. Cult. Stud. 2020, 7, 116–130. [Google Scholar] [CrossRef]
- Mikhael, E.M.; Al-Jumaili, A.A. Can developing countries face novel coronavirus outbreak alone? The Iraqi situation. Public Health Pract. 2020, 1, 100004. [Google Scholar] [CrossRef]
- Government of Iraq. COVID-19: Higher Committee Announces Changes to Curfew Hours. 2020. Available online: https://gds.gov.iq/covid-19-higher-committee-announces-changes-to-curfew-hours/ (accessed on 11 May 2022).
- Government of Iraq. COVID-19: Higher Committee Announces ‘Odd-Even’ Rule for Vehicles. 2020. Available online: https://gds.gov.iq/covid-19-higher-committee-announces-odd-even-rule-for-vehicles/ (accessed on 19 July 2022).
- UNICEF. Iraq Receives the First Delivery of COVID-19 Vaccines through the COVAX Facility. 2021. Available online: https://www.unicef.org/iraq/press-releases/iraq-receives-first-delivery-covid-19-vaccines-through-covax-facility (accessed on 19 July 2022).
- Al-Qerem, W.; Hammad, A.; Alsajri, A.H.; Al-Hishma, S.W.; Ling, J.; Mosleh, R. COVID-19 Vaccination Acceptance and Its Associated Factors Among the Iraqi Population: A Cross Sectional Study. Patient Prefer. Adherence 2022, 16, 307–319. [Google Scholar] [CrossRef] [PubMed]
- Regional Office for the Eastern Mediterranean, World Health Organization. COVID-19 situation updates for week 27 (4–10 July 2021); World Health Organization. 2021. Available online: http://www.emro.who.int/pdf/pandemic-epidemic-diseases/covid-19/covid-19-situation-updates-for-week-27-410-july-2021.pdf?ua=1 (accessed on 19 July 2022).
- World Health Organization. Achieving 70% COVID-19 Immunization Coverage by Mid-2022. Available online: https://www.who.int/news/item/23-12-2021-achieving-70-covid-19-immunization-coverage-by-mid-2022 (accessed on 20 July 2022).
- World Health Organization. World Health Organization Coronavirus (COVID-19) Dashboard. 2020. Available online: https://covid19.who.int/ (accessed on 20 July 2022).
- IBN. Iraq Launches COVID-19 Vaccination Campaign. Available online: https://www.iraq-businessnews.com/2021/11/14/iraq-launches-covid-19-vaccination-campaign/ (accessed on 20 July 2022).
- Ritchie, H.; Mathieu, E.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Ortiz-Ospina, E.; Hasell, J.; Macdonald, B.; Dattani, S.; Roser, M. Coronavirus Pandemic (COVID-19). Our World in Data 2020. Available online: https://ourworldindata.org/coronavirus (accessed on 29 July 2022).
- Al-Qerem, W.; Jarab, A.; Hammad, A.; Alasmari, F.; Ling, J.; Alsajri, A.H.; Al-Hishma, S.W.; Abu Heshmeh, S.R. Iraqi Parents’ Knowledge, Attitudes, and Practices towards Vaccinating Their Children: A Cross-Sectional Study. Vaccines 2022, 10, 820. [Google Scholar] [CrossRef]
- Rosiello, D.F.; Anwar, S.; Yufika, A.; Adam, R.Y.; Ismaeil, M.I.; Ismail, A.Y.; Dahman, N.B.; Hafsi, M.; Ferjani, M.; Sami, F.S.; et al. Acceptance of COVID-19 vaccination at different hypothetical efficacy and safety levels in ten countries in Asia, Africa, and South America. Narra J. 2021, 1, e55. [Google Scholar] [CrossRef]
- Abu-Farha, R.; Mukattash, T.; Itani, R.; Karout, S.; Khojah, H.M.J.; Abed Al-Mahmood, A.; Alzoubi, K.H. Willingness of Middle Eastern public to receive COVID-19 vaccines. Saudi Pharm. J. 2021, 29, 734–739. [Google Scholar] [CrossRef]
- Tahir, A.I.; Ramadhan, D.S.; Piro, S.S.; Abdullah, R.Y.; Taha, A.A.; Radha, R.H. COVID-19 vaccine acceptance, hesitancy and refusal among Iraqi Kurdish population. Int. J. Health Sci. 2022, 16, 10–16. [Google Scholar]
- Abazid, H.; Basheti, I.A.; Al-Jomaa, E.E.; Abazid, A.; Kloub, W.M. Public knowledge, beliefs, psychological responses, and behavioural changes during the outbreak of COVID-19 in the Middle East. Pharm. Pract. 2021, 19, 2306. [Google Scholar] [CrossRef]
- Al-Kaabi, H.J.A.; Mohammed, H.A.; Kumait, A. Assessing knowledge and perceptions of health care workers toward novel coronavirus (COVID-19). Med.-Leg. Update 2020, 20, 2023–2030. [Google Scholar] [CrossRef]
- Hammadi, S.; AlKanan, A.K.; Fares, M.; Mohammed, N.K.; Hashim, A.R.; Habeeb, A.; Mansour, A.A. Basrah Preliminary Experience With COVID-19: A Report on 6404 Patients. Cureus 2021, 13, e13012. [Google Scholar] [CrossRef]
- Abbas, H.M.; Al-Jumaili, A.A.; Nassir, K.F.; Al-Obaidy, M.W.; Al Jubouri, A.M.; Dakhil, B.D.; Abdulelah, M.M.; Al Khames, Q.A. Assessment of COVID-19 Treatment containing both Hydroxychloroquine and Azithromycin: A natural clinical trial. Int. J. Clin. Pract. 2021, 75, e13856. [Google Scholar] [CrossRef]
- Lami, F.; Rashak, H.A.; Khaleel, H.A.; Mahdi, S.G.; Adnan, F.; Khader, Y.S.; Alhilfi, R.A.; Lehlewa, A. Iraq experience in handling the COVID-19 pandemic: Implications of public health challenges and lessons learned for future epidemic preparedness planning. J. Public Health 2021, 43, iii19–iii28. [Google Scholar] [CrossRef]
- World Health Organization. Iraq: World Health Organization Provides Support to Bridge Shortfall in Oxygen Supplies. Available online: https://www.who.int/news-room/feature-stories/detail/iraq-who-provides-support-to-bridge-shortfall-in-oxygen-supplies (accessed on 20 July 2022).
- KAPITA. Surviving the COVID-19 Crisis: Preliminary Findings of the Economic Impact on Iraq; KAPITA: Baghdad, Iraq, 2020. [Google Scholar]
- Gentilini, U.; Almenfi, M.; Orton, I.; Dale, P. Social Protection and Jobs Responses to COVID-19: A Real-Time Review of Country Measures; World Bank: Washington, DC, USA, 2020. [Google Scholar]
- Government of Iraq. COVID-19: Iraqi Government Announces New Measures. 2020. Available online: https://gds.gov.iq/covid-19-iraqi-government-announces-new-measures/ (accessed on 21 July 2022).
- Jaber, R.M.; Mafrachi, B.; Al-Ani, A.; Shkara, M. Awareness and perception of COVID-19 among the general population: A Middle Eastern survey. PLoS ONE 2021, 16, e0250461. [Google Scholar] [CrossRef]
- Al-Taweel, F.B.; Abdulkareem, A.A.; Gul, S.S.; Alshami, M.L. Evaluation of technology-based learning by dental students during the pandemic outbreak of coronavirus disease 2019. Eur. J. Dent. Educ. 2021, 25, 183–190. [Google Scholar] [CrossRef]
- Othman Abdullah, C.; Mahmood Abdulla, R. Evaluation of E-Learning in Higher Education during COVID-19 Pandemic: A Case Study in University of Sulaimani. In Proceedings of the 12th International Conference on E-Education, E-Business, E-Management, and E-Learning, IC4E 2021, Tokyo, Japan, 10–13 January 2021; pp. 68–74. [Google Scholar] [CrossRef]
- Shabila, N.P.; Alkhateeb, N.E.; Dauod, A.S.; Al-Dabbagh, A. Exploring the perspectives of medical students on application of e-learning in medical education during the COVID-19 pandemic. Work 2021, 70, 751–762. [Google Scholar] [CrossRef]
- Obaid, A.H.; Al-Husseini, K.A. The Effectiveness and Difficulties of E-Learning under Crises from the Viewpoint of the Academic Staff and Students: An Analytical Study. In Proceedings of the 2nd Annual International Conference on Information and Sciences, AiCIS 2020, Fallujah, Iraq, 24–25 November 2020; pp. 157–164. [Google Scholar] [CrossRef]
- World Health Organization. Essential Programme on Immunization. Available online: https://www.who.int/teams/immunization-vaccines-and-biologicals/essential-programme-on-immunization (accessed on 23 July 2022).
- Alhaddad, A.; Ahmadnezhad, E.; Fotouhi, A. The vaccination coverage rate in under-five children in Nasiriyah (Iraq) before and during the COVID-19 pandemic. Epidemiol. Health 2022, 44, e2022035. [Google Scholar] [CrossRef]
- Al-Mendalawi, M.D. Paediatric COVID-19 Infection in Iraq: Is it not prevalent or underestimated? Sultan Qaboos Univ. Med. J. 2020, 20, e374–e375. [Google Scholar] [CrossRef]
- USAID. National Immunization Plan of Iraq for 2015. 2015. Available online: https://pdf.usaid.gov/pdf_docs/PA00KD56.pdf (accessed on 23 July 2022).
- World Health Organization. Ministry of Health and World Health Organization Introduce Environmental Surveillance for Poliovirus in Iraq. Available online: https://www.emro.who.int/iraq/news/ministry-of-health-and-who-introduce-environmental-surveillance-for-poliovirus-in-iraq.html (accessed on 23 July 2022).
- UNAMI. For Iraq UNAMI Public Information Office 05/09/2022. 2021. Available online: https://iraq.un.org/sites/default/files/2022-05/For_Iraq_2021_2022_ENG_web.pdf (accessed on 24 July 2022).
- Mahmood, K.I.; Shabu, S.A.; KM, M.A.; Hussain, S.S.; Kako, D.A.; Hinchliff, S.; Shabila, N.P. The Impact of COVID-19 Related Lockdown on the Prevalence of Spousal Violence Against Women in Kurdistan Region of Iraq. J. Interpers. Violence 2021, 37, NP11811–NP11835. [Google Scholar] [CrossRef] [PubMed]
- Al-Atrushi, H.H.; Al-Tawil, N.G.; Shabila, N.P.; Al-Hadithi, T.S. Intimate partner violence against women in the Erbil city of the Kurdistan region, Iraq. BMC Women’s Health 2013, 13, 37. [Google Scholar] [CrossRef] [PubMed]
- United Nations Office for the Coordination of Humanitarian Affairs. Global Humanitarian Response Plan: COVID-19 (April–December 2020); United Nations Office for the Coordination of Humanitarian Affairs: New York, NY, USA; Geneva, Switzerland, 2020. [Google Scholar]
- Burnham, G.; Malik, S.; Dhari Al-Shibli, A.S.; Mahjoub, A.R.; Baqer, A.Q.; Baqer, Z.Q.; Qaraghuli, F.A.; Doocy, S. Understanding the impact of conflict on health services in Iraq: Information from 401 Iraqi refugee doctors in Jordan. Int. J. Health Plan. Manag. 2012, 27, e51–e64. [Google Scholar] [CrossRef]
- Doocy, P.; Malik, S.; Burnham, G. Experiences of Iraqi doctors in Jordan during conflict and factors associated with migration. Am. J. Disaster Med. 2010, 5, 7. [Google Scholar] [CrossRef]
- Lafta, R.; Qusay, N.; Mary, M.; Burnham, G. Violence against doctors in Iraq during the time of COVID-19. PLoS ONE 2021, 16, e0254401. [Google Scholar] [CrossRef]
- Al-Mudhaffer, R.H.; Ahjel, S.W.; Hassan, S.M.; Mahmood, A.A.; Hadi, N.R. Age Distribution of Clinical Symptoms, Isolation, Co-morbidities and Case Fatality Rate of COVID-19 Cases in Najaf City, Iraq. Med. Arch. 2020, 74, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Abdulqadir, J.N.; Glenn Ford, D.V.; Sadeq, A.L.; Hani, A.; Hossam, E.; Muna, B.; Joseph, U.A.; Ibtesam, O.J.; Hawa, A.; Nabil, E.O.; et al. Stigma towards health care providers taking care of COVID-19 patients: A multi-country study. Heliyon 2022, 8. [Google Scholar] [CrossRef]
- Al-Jumaili, A.A.; Al-Fatlawi, B.G.; Al-Jalehawi, A.K.; Al-Hamadani, F.Y.; Alsawad, O.S. Impact of COVID-19 pandemic on healthcare providers: Save the frontline fighters. Int. J. Pharm. Pract. 2021, 29, 369–375. [Google Scholar] [CrossRef]
- Abdulah, D.M.; Mohammed, A.A. The consequences of the COVID-19 pandemic on perceived stress in clinical practice: Experience of doctors in Iraqi Kurdistan. Rom. J. Intern. Med. 2020, 58, 219–227. [Google Scholar] [CrossRef]
- Saeed, B.A.; Shabila, N.P.; Aziz, A.J. Stress and anxiety among physicians during the COVID-19 outbreak in the Iraqi Kurdistan Region: An online survey. PLoS ONE 2021, 16, e0253903. [Google Scholar] [CrossRef]
- Tunescu, M.; Christodorescu, R.; Sharma, A.; Barsac, C.R.; Rogobete, A.F.; Crisan, D.C.; Popovici, S.E.; Kundnani, N.R.; Sandesc, D.; Bedreag, O. The preoperative evaluation of post-COVID-19 patients scheduled for elective surgery—What is important not to miss! Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 7607–7615. [Google Scholar] [CrossRef]
- Hoz, S.S.; Al-Sharshahi, Z.F.; Dolachee, A.A.; Matti, W.E. Letter to the Editor: “Beyond Containment: Tracking the Impact of Coronavirus Disease 2019 (COVID-19) on Neurosurgery Services in Iraq”. World Neurosurg. 2020, 143, 619–620. [Google Scholar] [CrossRef]
- Delardas, O.; Kechagias, K.S.; Pontikos, P.N.; Giannos, P. Socio-Economic Impacts and Challenges of the Coronavirus Pandemic (COVID-19): An Updated Review. Sustainability 2022, 14, 9699. [Google Scholar] [CrossRef]
- Ali, L.Q.H. Minimizing the risk of covid-19 in pediatric dialysis center in baghdad/iraq. Indian J. Public Health Res. Dev. 2020, 11, 323–325. [Google Scholar] [CrossRef]
- United Nations High Commissioner for Refugees. UNHCR Country Portfolio Evaluation: Iraq; United Nations High Commissioner for Refugees: Geneva, Switzerland, 2020; Available online: https://www.unhcr.org/en-us/research/evalreports/5f6df4a04/unhcr-iraq-country-portfolio-evaluation.html?query=Iraq (accessed on 13 July 2022).
- Albadry, A. The Security Challenges and Iraqi Parliamentary Institution. J. Basic Appl. Res. Int. 2016, 18, 28–35. [Google Scholar]
- United Nations. United Nations Sustainable Development Cooperation Framework IRAQ (UNISDCF); United Nations: New York, NY, USA, 2021. [Google Scholar]
- Farhadi, N.L.H. Forensic Analysis of COVID-19 Data from 198 Countries Two Years after the Pandemic Outbreak. COVID 2022, 2, 472–485. [Google Scholar] [CrossRef]
- El-Jardali, F.; Hemadeh, R.; Jaafar, M.; Sagherian, L.; El-Skaff, R.; Mdeihly, R.; Jamal, D.; Ataya, N. The impact of accreditation of primary healthcare centers: Successes, challenges and policy implications as perceived by healthcare providers and directors in Lebanon. BMC Health Serv. Res. 2014, 14, 86. [Google Scholar] [CrossRef]
- Bank, T.W. The World Bank in Social Protection. Available online: https://www.worldbank.org/en/topic/socialprotection/overview (accessed on 1 September 2022).
- UNICEF. Lessons Learned and Good Practices. Country-Specific Case Studies on Immunization Activities during the COVID-19 Pandemic; UNICEF: New York, NY, USA, 2020. [Google Scholar]
- Ho, L.L.; Gurung, S.; Mirza, I.; Nicolas, H.D.; Steulet, C.; Burman, A.L.; Danovaro-Holliday, M.C.; Sodha, S.V.; Kretsinger, K. Impact of the SARS-CoV-2 pandemic on vaccine-preventable disease campaigns. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2022, 119, 201–209. [Google Scholar] [CrossRef]
- Raftery, P.; Howard, N.; Palmer, J.; Hossain, M. Gender-based violence (GBV) coordination in humanitarian and public health emergencies: A scoping review. Confl. Health 2022, 16, 37. [Google Scholar] [CrossRef]
- Maureen, M.; Mary, E.; Aminat, B.; Claudia, G.M. Risk and protective factors for GBV among women and girls living in humanitarian setting: Systematic review protocol. Syst. Rev. 2021, 10, 238. [Google Scholar] [CrossRef]
- Stefano, F.; Benedetta, B.; Christian, N.; Anna Maria, G.; Giovanna, P. Managing and preventing acts of violence against health workers: Results of a review evaluating hospital control procedures. J. Aggress. Confl. Peace Res. 2022, 14, 100–111. [Google Scholar] [CrossRef]
- Hutton, S.A.; Vance, K.; Burgard, J.; Grace, S.; Van Male, L. Workplace violence prevention standardization using lean principles across a healthcare network. Int. J. Health Care Qual. Assur. 2018, 31, 464–473. [Google Scholar] [CrossRef] [PubMed]
- Dye, T.D.; Alcantara, L.; Siddiqi, S.; Barbosu, M.; Sharma, S.; Panko, T.; Pressman, E. Risk of COVID-19-related bullying, harassment and stigma among healthcare workers: An analytical cross-sectional global study. BMJ Open 2020, 10, e046620. [Google Scholar] [CrossRef]
- Devi, S. COVID-19 exacerbates violence against health workers. Lancet 2020, 396, 658. [Google Scholar] [CrossRef]
- Bhatti, O.A.; Rauf, H.; Aziz, N.; Martins, R.S.; Khan, J.A. Violence against Healthcare Workers during the COVID-19 Pandemic: A Review of Incidents from a Lower-Middle-Income Country. Ann. Glob. Health 2021, 87, 41. [Google Scholar] [CrossRef] [PubMed]
- Lafta, R.K.; Falah, N. Violence against health-care workers in a conflict affected city. Med. Confl. Surviv. 2019, 35, 65–79. [Google Scholar] [CrossRef] [PubMed]
- Seidi, P.A.M.; Ardebil, M.D.; Jaff, D. COVID-19 pandemic: New challenge to securing mental well-being in conflict settings. Asian J. Psychiatry 2020, 51, 102151. [Google Scholar] [CrossRef]
- Hashim, H.; Ramadhan, M.; Al-jarshawi, M.; Kadhim, M. Psychiatry in Iraq: Challenges and Consequences. Prim Care Companion CNS Disord. 2021, 23, 21com02922. [Google Scholar] [CrossRef]
- Sadik, S.; Al-Jadiry, A.M. Mental health services in Iraq: Past, present and future. Int. Psychiatry 2006, 3, 11–13. [Google Scholar] [CrossRef]
- World Health Organization. Immunization as an Essential Health Service: Guiding Principles for Immunization Activities during the COVID-19 Pandemic and Other Times of Severe Disruption; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Nabukeera, M. Prevention and response to gender-based violence (GBV) during novel COVID-19 lock-down in Uganda. J. Adult Prot. 2021, 23, 116–133. [Google Scholar] [CrossRef]
- Ghareeb, N.S.; El-Shafei, D.A.; Eladl, A.M. Workplace violence among healthcare workers during COVID-19 pandemic in a Jordanian governmental hospital: The tip of the iceberg. Environ. Sci. Pollut. Res. 2021, 28, 61441. [Google Scholar] [CrossRef]
- Basilua Andre, M.; Lukuke Hendrick, M.; Nlandu Roger, N.; Kaj Francoise, M.; Masamitsu, E.; Ryoji, H.; Narufumi, S. Workplace violence towards Congolese health care workers: A survey of 436 healthcare facilities in Katanga province, Democratic Republic of Congo. J. Occup. Health 2015, 57, 69–80. [Google Scholar]
- Costa, A.; Menon, V.; Phadke, R.; Dapke, K.; Miranda, A.V.; Ahmad, S.; Essar, M.Y.; Hashim, H.T. Mental health in the post COVID-19 era: Future perspectives. Einstein 2022, 20, eCE6760. [Google Scholar] [CrossRef]
- Sahebi, A.; Yousefi, A.; Abdi, K.; Jamshidbeigi, Y.; Moayedi, S.; Torres, M.; Wesemann, U.; Sheikhbardsiri, H.; Golitaleb, M. The Prevalence of Post-traumatic Stress Disorder Among Health Care Workers During the COVID-19 Pandemic: An Umbrella Review and Meta-Analysis. Front. Psychiatry 2021, 12, 764738. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Janabi, T.; Chung, S. Current Impact and Long-Term Influence of the COVID-19 Pandemic on Iraqi Healthcare Systems: A Case Study. Epidemiologia 2022, 3, 412-433. https://doi.org/10.3390/epidemiologia3040032
Al Janabi T, Chung S. Current Impact and Long-Term Influence of the COVID-19 Pandemic on Iraqi Healthcare Systems: A Case Study. Epidemiologia. 2022; 3(4):412-433. https://doi.org/10.3390/epidemiologia3040032
Chicago/Turabian StyleAl Janabi, Taysir, and Sunny Chung. 2022. "Current Impact and Long-Term Influence of the COVID-19 Pandemic on Iraqi Healthcare Systems: A Case Study" Epidemiologia 3, no. 4: 412-433. https://doi.org/10.3390/epidemiologia3040032
APA StyleAl Janabi, T., & Chung, S. (2022). Current Impact and Long-Term Influence of the COVID-19 Pandemic on Iraqi Healthcare Systems: A Case Study. Epidemiologia, 3(4), 412-433. https://doi.org/10.3390/epidemiologia3040032







