Abstract
Influenza poses a significant public health threat, causing millions of severe cases and hundreds of thousands of deaths annually. Vaccination remains the most effective measure to reduce transmission, complications, and the strain on healthcare systems. Despite its importance, vaccination uptake remains suboptimal among college students, a key population for infectious disease transmission and a target group for public health interventions. The primary objective of this study was to examine the psychological and contextual determinants of influenza vaccination among college students in Israel, utilizing the Theory of Planned Behavior (TPB) as the guiding framework. A cross-sectional online survey was conducted among 591 students at Ashkelon Academic College between April and May 2023. The questionnaire included validated items assessing attitudes toward vaccination, subjective norms, perceived behavioral control, and vaccination history. Hierarchical logistic regression was used to assess the predictive power of these variables in explaining actual vaccination behavior. The results indicated that prior vaccination was the strongest predictor of current influenza vaccine uptake (OR = 38.7, p < 0.001). Positive attitudes (e.g., belief in vaccine protection), strong social influences (e.g., parental vaccination behavior and trust in healthcare professionals), and high perceived behavioral control (e.g., accessibility and convenience) were all significantly associated with increased vaccination likelihood. The final model explained 68% of the variance in vaccination behavior (Nagelkerke R2 = 0.68, p < 0.001). These findings affirm the TPB as a robust framework for understanding vaccination behavior and underscore the importance of habitual vaccination, public trust, and systemic accessibility. The study contributes to the field by illustrating how national healthcare infrastructure interacts with individual-level beliefs to shape preventive health actions. Practical applications include the development of targeted interventions to promote first-time vaccination, address vaccine safety concerns, and leverage trusted social networks. Future research should investigate how digital communication, policy variation, and sociocultural context influence the components of the TPB across diverse populations.
1. Introduction
Influenza vaccination is widely regarded as one of the most effective strategies for reducing the health, social, and economic burden of the disease [1,2]. Globally, influenza is responsible for an estimated 3–5 million severe cases and between 290,000 and 650,000 respiratory-related deaths annually [3]. In the United States alone, preliminary estimates for the 2023–2024 flu season indicate approximately 40 million influenza-related illnesses, 18 million medical visits, and 470,000 hospitalizations. Since October 2023, the number of influenza-related deaths have been estimated to range between 25,000 and 72,000 [4]. In Israel, recent data indicate thousands of hospitalizations due to laboratory-confirmed influenza cases. The Israeli Ministry of Health [5] recommends annual vaccination, particularly for high-risk groups such as the elderly and individuals with chronic conditions. Nevertheless, vaccination rates remain low: only approximately 17.8% of health fund members have received the influenza vaccine, although coverage increases to 58.6% among adults aged 65 and older [5].
Despite the well-documented severity of influenza and the widespread availability of safe and effective vaccines, vaccination rates remain suboptimal. The Centers for Disease Control and Prevention (CDC) analyzed data from two nationally representative surveys to assess flu vaccination coverage for the 2023–2024 season [6]. The findings indicate that flu vaccination coverage among children aged 6 months to 17 years was 55.4%, reflecting an 8.3% decline from the pre-pandemic 2019–2020 season (63.7%). Among adults aged 18 and older, coverage stood at 44.9%, marking a 2.0% decrease from the previous season (46.9%) [6]. This decline in vaccination rates presents not only a public health challenge but also broader sustainability issue, as lower vaccine uptake can strain healthcare infrastructure, reduce workforce productivity, and increase the economic burden on health systems globally [7].
Influenza vaccination is crucial in protecting college students, who frequently interact in classrooms and social environments. Studies have shown that seasonal influenza vaccination rates among students remain relatively low, with coverage estimates ranging between 12% and 30% [8]. The dense living conditions and frequent interpersonal interactions in campus settings create an environment conducive to the rapid spread of influenza. These environments exemplify how population density, mobility patterns, and shared public spaces influence health risks and necessitate targeted interventions in high-risk social environments. Such outbreaks can disrupt academic performance, increase absenteeism, and lead to greater reliance on healthcare services and medications [9]. While influenza-related hospitalizations among college students are relatively uncommon, the overall burden of the virus in this population remains substantial [8]. Uddin et al. [10] examined factors influencing influenza vaccination uptake among college students in Michigan. Only 17.3% of students reported receiving the influenza vaccine. Students vaccinated during the previous flu season were significantly more likely to get vaccinated again. Students who consulted a doctor about flu prevention were nearly three times more likely to get vaccinated. In France, 17.9% of students from two universities were vaccinated [11]. Students who felt capable of getting vaccinated and perceived the vaccine’s benefits were associated with stronger vaccination intentions. Although these studies were conducted in different countries and healthcare systems, they converge on the importance of both internal motivators (such as self-efficacy and perceived benefit) and external enablers (such as healthcare consultation and access). However, the variation in vaccination rates suggests that cultural, systemic, and institutional differences play a critical role in shaping behavior. The findings also reveal a gap between intention and action, particularly when structural support is limited, a phenomenon widely acknowledged in health behavior literature, a pattern well-documented in health behavior literature. While Uddin et al. [10] highlight the role of professional guidance, Fall et al. [11] emphasize internal perceptions of capability, pointing to the multifaceted nature of vaccination decision-making.
These findings align with broader discussions on health equity, as accessibility and socioeconomic status may determine students’ likelihood of engaging in preventive health behaviors. They also highlight the need for context-sensitive strategies that consider both individual-level perceptions and structural barriers. The role of universities as public health stakeholders illustrates the intersection of education policy and health policy, emphasizing the need for institutional interventions that promote sustainable vaccine uptake.
The Theory of Planned Behavior (TPB), developed by Icek Ajzen [12], is a widely used framework for understanding health-related decision-making, including vaccination, as it captures individual cognitive factors and broader social influences. For example, TPB has been used to explain why individuals choose to get vaccinated or avoid vaccination in the context of influenza [13]. According to TPB, vaccination intentions are primarily driven by three key factors: attitude, subjective norms, and perceived behavioral control, each of which is influenced by broader socio-political and economic conditions.
Attitude refers to beliefs about the benefits (e.g., protection from illness, academic continuity) and perceived drawbacks (e.g., concerns about vaccine safety and effectiveness). In the context of public health sustainability, attitudes toward vaccination are influenced by access to information, media exposure, and trust in institutions, all of which can shift in response to global health crises and misinformation trends. Subjective norms encompass social influences from peers, family, and healthcare providers that either encourage or discourage vaccination. Given the increasing role of digital media and social networks in shaping public opinion, subjective norms extend beyond direct interpersonal interactions to include globalized narratives surrounding vaccination policies, governmental credibility, and social responsibility in public health efforts. Perceived behavioral control refers to an individual’s confidence in their ability to get vaccinated, including factors such as accessibility and convenience [14]. Structural barriers such as socioeconomic disparities, healthcare infrastructure, and government-led vaccination initiatives can impact perceived behavioral control, reinforcing the importance of policy-driven accessibility in shaping health behaviors. These components collectively help predict students’ likelihood of receiving the influenza vaccine. TPB can predict 60–70% of adults’ vaccination intentions [15].
Studies have identified various factors influencing vaccination decisions, including concerns about adverse effects, family influence, perceived benefits, and logistical barriers [16,17]. For instance, a systematic review highlighted that positive vaccine attitudes, self-efficacy, and healthcare workers’ recommendations significantly enhance vaccination uptake, while fear of side effects and poor access to services act as barriers [18]. Recent studies have specifically examined influenza vaccination behavior among college students, providing valuable insights into this public health concern. Due to their social engagement, university students are influenced by peer opinions and awareness campaigns, which play a critical role in shaping their vaccination intentions [19]. Findings indicate that attitudes and subjective norms significantly predict vaccination intentions, whereas perceived behavioral control has shown mixed results [20,21]. Psychological determinants such as confidence in vaccine safety and perceived susceptibility to influenza have been identified as key factors [22].
Taken together, these studies demonstrate that a complex interplay between personal beliefs, social influence, and contextual factors shapes vaccination decisions among university students. While Han et al. [18] and Schmid et al. [22] emphasize internal psychological variables such as confidence and fear, Mussetto et al. [19] highlight the growing impact of external social dynamics like peer norms and institutional messaging. This suggests that effective vaccination strategies should integrate both intrapersonal and interpersonal approaches. Moreover, the inconsistent findings regarding perceived behavioral control suggest that its predictive value may be highly context-dependent, stronger in settings where access is limited and weaker in systems offering universal availability. This underscores the need for locally tailored health behavior models that account for structural and cultural conditions. Given the critical role of influenza vaccination in disease prevention, particularly among college students, the main objective of this study is to analyze the behavioral determinants of influenza vaccination uptake among college students in Israel, using the TPB as a theoretical framework. Specifically, it investigates the influence of attitudes, subjective norms, and perceived behavioral control on students’ vaccination decisions. By framing this research within the broader context of public health sustainability, public trust, and health policy adaptation, this study contributes to understanding how individual behavior interacts with systemic and institutional forces in shaping vaccination uptake. Identifying key determinants of vaccination behavior can inform the development of targeted, sustainable, and policy-driven interventions to improve influenza vaccine uptake among college students.
2. Materials and Methods
2.1. Research Procedure
A cross-sectional online study was conducted among students at Ashkelon Academic College, Israel. This design allows for efficient data collection from a large sample at a single point in time. This approach is particularly suitable for identifying associations between behavioral factors and influenza vaccination uptake. Data collection included 4200 students enrolled in various academic programs at the college. The survey was administered between April and May 2023, coinciding with the conclusion of the influenza vaccination season in Israel. Ethical approval was obtained from the Ashkelon Academic College Ethics Committee (approval #42-2023).
The study employed a convenience sampling approach, targeting all students enrolled at Ashkelon Academic College during the 2022–2023 academic year. The survey was developed using Qualtrics (Qualtrics, Provo, UT, USA) and distributed to all students via email, with a follow-up reminder sent three weeks later. A total of 703 students participated, of whom 591 completed the questionnaire in full, yielding a completion rate of 84% among respondents and approximately 14% of the total student population. Inclusion criteria were (1) current enrollment at the college during the study period and (2) full completion of the survey items related to influenza vaccination behavior and the TPB constructs. Participants who submitted partial responses or did not provide informed consent were excluded from the final dataset. The questionnaire’s introductory page provided an overview of the study’s objectives and ensured respondent anonymity. Participation was voluntary, with students given the option to withdraw at any time without obligation to answer specific questions.
2.2. Measures
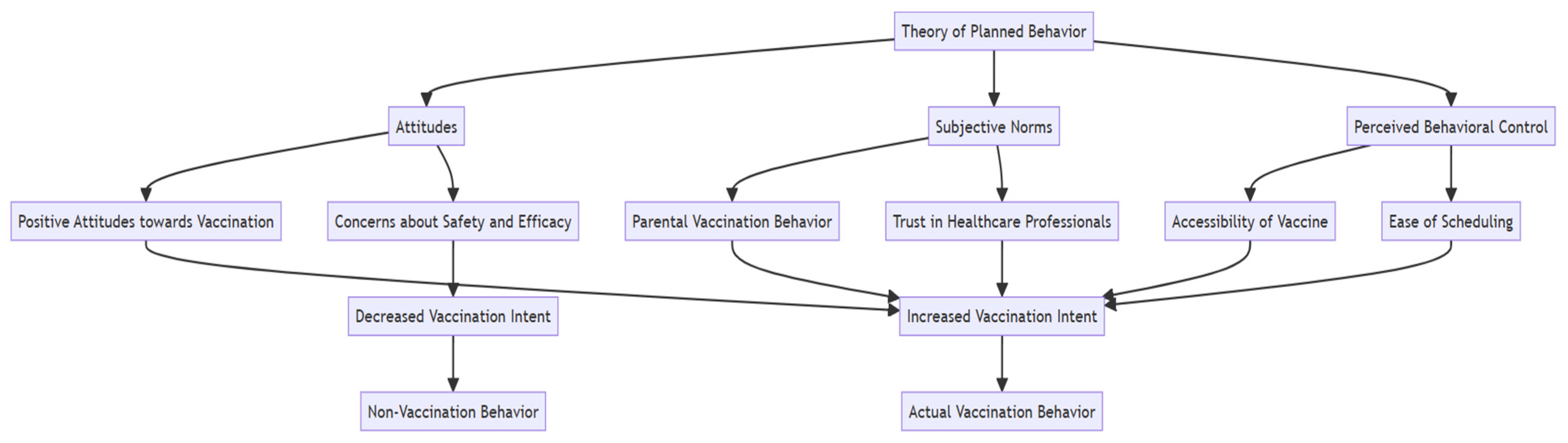
An online, closed, anonymous, self-completed questionnaire was used. It underwent content validation by an expert in public health and epidemiology and an expert in health promotion and behavior. The questionnaire comprised the following components according to the TPB. An overview of the measures and their expected associations is presented in Figure 1.
Figure 1.
Study measures and expected associations.
- Demographic information: Gender, age, religion, faculty, and year of study. The year of study was analyzed as a categorical variable (first, second, third, and fourth year) in order to capture potential differences in health awareness, institutional exposure, and vaccination behavior associated with academic progression.
- Vaccination behavior: Have you ever been vaccinated against the flu? Have you been vaccinated against influenza this year?
- Attitude: beliefs about the benefits (based on Silva et al. [23])—I believe that getting a flu shot will protect me from getting seriously ill with the flu; I believe that getting a flu shot is the best way to protect myself and others from getting the flu; Someone close to me has recently had the flu, and I want to protect myself. Cronbach’s α for reliability was 0.79.Beliefs about the drawbacks (based on Silva et al. [23])—I am concerned about the ineffectiveness of the influenza vaccine; I am concerned about the limited information available about the influenza vaccine; I think the influenza vaccine is not safe. Cronbach’s α for reliability was 0.90.Participants rated their agreement with each statement using a Likert scale ranging from 1 (“not at all”) to 5 (“strongly agree”).
- Subjective norms: Do your parents usually get vaccinated against the flu? Do you trust your doctor’s recommendations? Do you trust the medical professionals’ recommendations?
- Perceived behavioral control: I can get vaccinated against the flu if I choose to; It is easy for me to find time to get vaccinated during the academic year; The flu vaccine is accessible to me.Participants rated their agreement with each statement using a Likert scale ranging from 1 (“not at all”) to 5 (“strongly agree”). Cronbach’s α for reliability was 0.70.
2.3. Data Analysis
Data were analyzed using SPSS 29.0 (IBM, Armonk, NY, USA). In alignment with the TPB, hierarchical logistic regression models were employed to predict influenza vaccination behavior. This approach was chosen due to its ability to examine the relative contribution of different predictor variables while accounting for potential confounders.
Hierarchical logistic regression is instrumental in behavioral health research, as it allows for the stepwise inclusion of demographic factors, attitudinal variables, subjective norms, and perceived behavioral control, the core components of the TPB framework. By structuring the model hierarchically, we assessed the incremental explanatory power of each predictor set, providing insight into the specific factors that most strongly influence vaccination decisions. In the analysis, predictor variables were entered in sequential blocks, beginning with demographic characteristics (e.g., gender, age, and religion), followed by attitudinal beliefs (both perceived benefits and concerns regarding the influenza vaccine), subjective norms (e.g., parental vaccination behavior and trust in medical professionals), and finally, perceived behavioral control (e.g., vaccine accessibility and ease of scheduling vaccination). The use of hierarchical logistic regression was chosen due to its suitability for modeling binary outcome variables and its ability to assess the incremental explanatory power of conceptually distinct predictor blocks. This method aligns with the TPB structure, which organizes behavioral determinants into theoretical components (attitudes, subjective norms, perceived behavioral control), allowing for a stepwise evaluation of their contribution to vaccination behavior. Statistical significance was determined using p-values < 0.05, with effect sizes interpreted via odds ratios (Exp(B)) and 95% confidence intervals (CIs).
3. Results
3.1. Sample Characteristics
In total, 591 students participated in the study, of whom 40% were men, 60% were women, and 84% were Jewish. About half of the students studied in the Faculty of Social Sciences (46%), followed by 35% in Health Sciences, and 19% in Computer Science and Management. Half of the students were in the first year of studies, 33% in the second year, and 17% in the third or fourth year. The mean age was 27.69 ± 7.19 years. A detailed overview of the sample characteristics is presented in Table 1.

Table 1.
Sample characteristics.
3.2. Influenza Vaccination Behavior
Among the participants, 13% were vaccinated (n = 76), 45% intended to get vaccinated (n = 266), 8% were undecided (n = 47), and 34% did not intend to get vaccinated (n = 202). In terms of past behavior, more than half (57%, n = 337) were vaccinated against influenza in the past, 37% (n = 220) were not vaccinated against influenza in the past, and 6% did not remember (n = 34).
3.3. Hierarchical Logistic Regression Model for the Prediction of Influenza Vaccination Behavior
The results of hierarchical logistic regression models to predict influenza vaccine behavior are presented in Table 2. Demographic factors (e.g., age, year of study, past vaccination) accounted for an initial portion of the variance, but the addition of attitudinal beliefs (e.g., perceived benefits and concerns) significantly improved model fit. Subjective norms, particularly trust in healthcare professionals and parental vaccination behavior, further enhanced predictive accuracy, demonstrating the social influence on vaccination decisions. Finally, perceived behavioral control, including ease of access and the ability to find time for vaccination, contributed meaningfully to the final model, suggesting that logistical barriers remain a critical factor.

Table 2.
Hierarchical logistic regression model results to predict influenza vaccine behavior.
In the final model, which includes all the variables found to be significant in the previous models, the predictive ability of age, vaccination history, year of studies, believing that getting a flu shot is the best way to protect from getting the flu, thinking the influenza vaccine is not safe, can get vaccinated if he chooses to, easy to find time to get vaccinated during the academic year, and the vaccine is accessible- were all found to predict vaccination behavior. The final model explained 68% of the variance in vaccination behavior (Nagelkerke R2 = 0.68, p < 0.001).
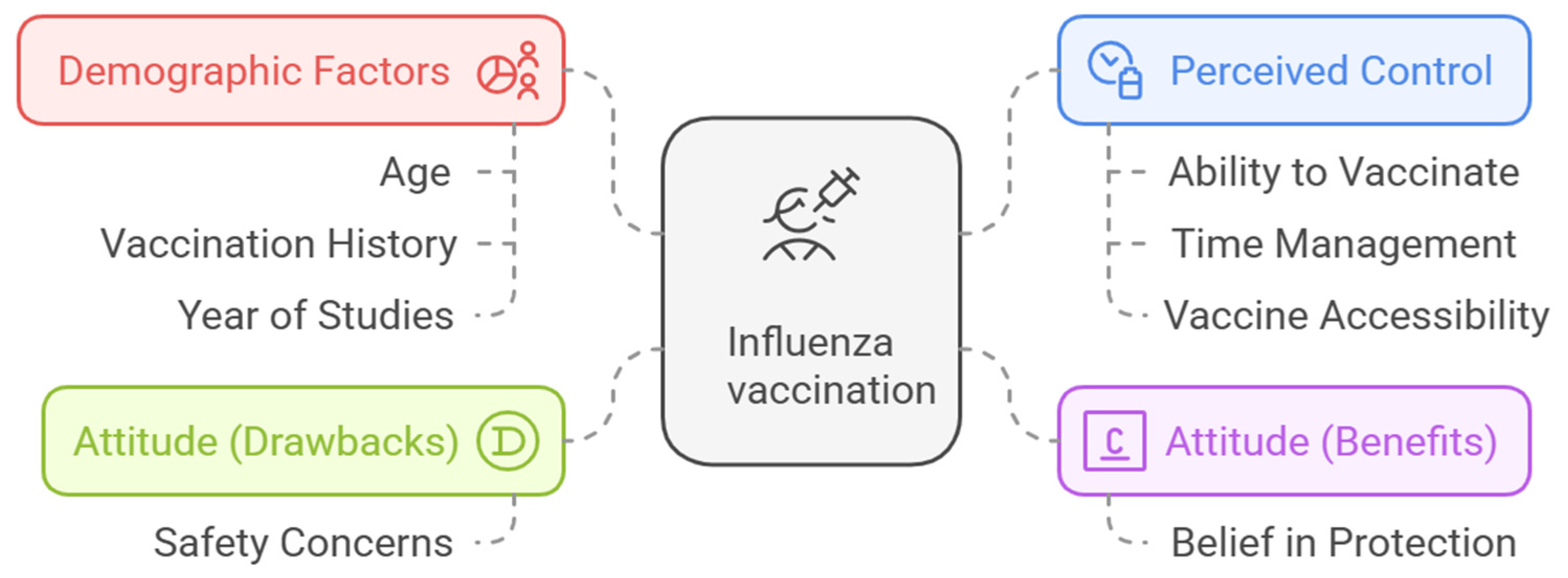
A summary of the significant predictors of influenza vaccination uptake among college students, as identified through the TPB, is presented in Figure 2.
Figure 2.
Key factors associated with influenza vaccination behavior (empirical model).
4. Discussion
This study examined the factors associated with influenza vaccination behavior among college students through the lens of the TPB. The results indicate that past vaccination history was the strongest predictor of influenza vaccination behavior. Students who had been vaccinated in the past exhibited significantly higher vaccination rates in the current season. This finding is consistent with previous research suggesting that habitual vaccination behaviors are critical determinants of vaccine uptake [10,24,25,26]. Behavioral science research suggests that repeated exposure to behavior in stable contexts reinforces automaticity, making it more likely that individuals will continue engaging in the behavior without extensive deliberation [27,28]. In the case of influenza vaccination, habitual vaccination behavior may develop through prior positive experiences, established healthcare routines, and reduced psychological barriers over time. These findings underscore the importance of embedding vaccination within long-term public health policies and educational frameworks that promote sustained immunization behaviors across the lifespan.
Uddin et al. [10] explained that Individuals vaccinated in previous seasons are more likely to overcome psychological and logistical barriers associated with vaccination, making them significantly more inclined to get vaccinated again. This tendency may be attributed to several factors. First, past vaccination fosters habit formation, turning influenza immunization into a routine health behavior. Second, prior experience reduces uncertainty, as individuals who have navigated the vaccination process once are already familiar with the procedure and access points. Third, social and environmental influences, such as parental vaccination behavior or healthcare recommendations, may reinforce continued vaccine adherence. Additionally, students who previously received the flu vaccine without adverse effects may experience positive reinforcement, increasing their confidence in vaccine safety and effectiveness. These mechanisms collectively support the broader concept of societal resilience, suggesting that sustained vaccination habits at the individual level contribute to community-wide health security and pandemic preparedness [29,30].
Among demographic factors, age and year of study were associated with vaccination behavior. Older students and those in advanced academic years demonstrated higher vaccination rates, possibly due to increased health awareness and greater exposure to health-related information over time [31,32]. These findings align with prior studies indicating that maturity and accumulated health knowledge contribute to vaccine uptake [17,33]. However, they also highlight a potential challenge: Younger students, who may lack extensive healthcare experience, could benefit from tailored intervention programs that normalize vaccination behaviors early in their academic journey, reinforcing long-term immunization habits.
Regarding attitudes, both perceived benefits and concerns about the influenza vaccine played significant roles. Students who believed in the protective benefits of vaccination were more likely to receive the flu shot. At the same time, those with safety concerns or doubts about vaccine efficacy exhibited lower vaccination rates. These results are in line with previous studies emphasizing the role of risk perception in shaping vaccination decisions [16,21]. Given the rise of vaccine misinformation on digital platforms, addressing risk perception through evidence-based health communication is crucial. Policymakers and public health officials should integrate behavioral science insights into strategic messaging campaigns that build trust and counteract misinformation [34].
Subjective norms also emerged as an influential factor, with trust in healthcare professionals and parental vaccination behavior positively associated with vaccine acceptance. These findings highlight the importance of social and institutional trust in overcoming vaccine hesitancy, reinforcing prior research demonstrating that individuals who perceive vaccines as socially normative and endorsed by trusted figures are more likely to get vaccinated [35,36,37,38]. Trust in institutions is a key determinant of compliance with public health recommendations, particularly in times of crisis [39]. Strengthening institutional credibility through transparent communication, proactive community engagement, and responsive healthcare policies can further promote vaccine acceptance at the societal level.
Finally, perceived behavioral control, including vaccine accessibility, time availability, and ease of vaccination, significantly impacted students’ decisions. Those who perceived the vaccination process as convenient and accessible were more likely to get vaccinated, supporting the idea that logistical barriers are a critical determinant of vaccine hesitancy [40,41]. The current study reinforces Fall et al. [11], which emphasized the importance of self-efficacy as a strong determinant of vaccination intention and actual behavior. Students who perceive themselves as capable of getting vaccinated are more likely to do so, underscoring the role of perceived control in decision-making. These insights suggest that simplifying the vaccination process, such as integrating vaccinations into routine university health services, offering mobile vaccination units, or implementing automated appointment reminders, could significantly increase student uptake.
These results support the notion that the intrinsic belief in the personal health benefits of vaccination is a key driver of actual vaccination behavior, whereas external pressures or social expectations do not necessarily lead to action. They are also consistent with Ajzen’s TPB model [12,14], which posits that behavioral intentions and ultimately behaviors are shaped by attitudes, subjective norms, and perceived control [14]. Similar studies on college students’ vaccination behaviors have identified comparable patterns, particularly regarding the influence of trust, habit, and accessibility on vaccination rates [8,42,43].
However, some deviations were observed. While previous research has suggested that perceived behavioral control might not be a strong predictor of vaccination behavior in certain contexts [21], it played a significant role in this study. This divergence may stem from differences in healthcare system accessibility and vaccination policies between countries, highlighting the need for context-specific intervention strategies. In Israel, influenza vaccines are free to all residents through the public healthcare system, and students can receive the vaccine without an appointment at designated healthcare centers and clinics. Such high accessibility reduces structural barriers that may exist in other countries, where factors such as financial cost, lack of insurance coverage, or complex scheduling procedures limit vaccine uptake. Given this context, Israeli students likely perceive vaccination as a personal choice rather than a logistical challenge, making perceived behavioral control a more influential factor in their decision-making process. This finding underscores the importance of healthcare infrastructure and ease of access in shaping vaccination behaviors. It also suggests that in settings with minimal logistical barriers, public health interventions should prioritize motivational and attitudinal factors over accessibility. These findings reinforce the importance of public health policy in shaping individual health behaviors. Countries with universal vaccine access may need to shift their focus from accessibility improvements to behavioral interventions that strengthen vaccine confidence and address hesitancy drivers.
The findings have important implications for public health interventions to increase influenza vaccination rates among college students. Interventions should focus on encouraging first-time vaccination among students who have never been immunized, as this could lead to long-term compliance. Efforts should prioritize removing psychological barriers, increasing trust in health authorities, and ensuring seamless access to establish lifelong vaccination habits. Targeted awareness campaigns emphasizing the protective benefits of influenza vaccination while addressing concerns about safety and efficacy can help reduce vaccine hesitancy [44]. Leveraging trusted sources and encouraging healthcare professionals, universities, and family members to promote vaccination could increase vaccine uptake. Ensuring convenient on-campus access to vaccination, with flexible scheduling and minimal administrative burdens, is also likely to improve coverage. Beyond individual interventions, multi-sector collaborations between universities, healthcare providers, and policymakers can support integrated approaches that promote vaccine sustainability and resilience within broader public health infrastructures.
Study Limitations
This study has several limitations that should be acknowledged. First, the cross-sectional design limits the ability to infer causal relationships between TPB constructs and vaccination behavior. While hierarchical logistic regression was employed to control for potential confounding variables such as age, gender, and year of study, the absence of randomization or temporal sequencing prevents definitive conclusions about the directionality of effects. Future studies should consider longitudinal designs to assess changes in behavior over time and establish stronger causal links. Second, data collection relied on self-reported responses, which may introduce recall or social desirability bias. Although the questionnaire was anonymous, self-administered, and based on validated TPB measures to minimize such biases, using objective vaccination records in future research could improve data accuracy and reduce subjectivity. Third, the study used a convenience sample drawn from a single academic institution, which may affect the generalizability of findings to broader student populations. Expanding future research to multiple universities and more diverse demographic groups could enhance external validity and provide a more comprehensive picture of vaccination behaviors among young adults. Finally, although the TPB framework accounted for a substantial portion of variance in vaccination behavior (Nagelkerke R2 = 0.68), additional psychological and sociopolitical factors—such as exposure to misinformation, conspiracy beliefs, and political orientation—were not examined in the present study. Future research should explore integrative behavioral models that incorporate these elements to understand the complex dynamics underlying vaccine hesitancy better. Future research should explore integrative models incorporating these factors for a more comprehensive understanding of vaccination decisions.
5. Conclusions
This study provides empirical support for the TPB in predicting influenza vaccination uptake among college students, reinforcing the role of habitual vaccination behavior, attitudes, and perceived behavioral control as key determinants. The findings highlight the importance of previous vaccination experience in shaping future immunization decisions, suggesting that sustained vaccination patterns may be more effectively promoted through long-term behavioral reinforcement strategies rather than short-term interventions. By emphasizing the interaction between individual beliefs and structural accessibility, this study contributes to a deeper understanding of how public health efforts can be tailored to increase vaccine uptake in young adult populations.
Moreover, the study highlights the need to expand the TPB framework by explicitly incorporating habitual vaccination history as a moderating or independent factor in predicting health-related decisions. Given the well-documented role of automaticity, past behavior, and social learning in shaping vaccination habits [27,28,45], incorporating these elements into TPB could enhance its predictive validity, particularly in contexts where vaccination is becoming a socio-behavioral norm rather than a one-time decision [46,47]. This expansion is particularly relevant in public health policy, where strategies aimed at normalizing vaccination behaviors could contribute to long-term population-wide immunity and resilience.
These findings carry important implications for public health policy and intervention design. Encouraging first-time vaccination among students who have never been immunized could foster habitual vaccination patterns, increasing compliance in future seasons. Public health strategies should prioritize evidence-based communication campaigns to counter misinformation, promote trust in healthcare professionals, and reinforce the societal value of vaccination. Additionally, universities and healthcare providers can play a crucial role by integrating vaccination services into routine student healthcare programs, thereby normalizing immunization as a standard preventive practice.
This study underscores the need for a multidisciplinary and sustainability-oriented approach to vaccine uptake, recognizing that immunization behavior is not only an individual health decision but also a crucial component of community resilience, public health sustainability, and societal adaptation. Promoting habitual vaccination through integrated healthcare policies, institutional trust, and equitable access to immunization services can contribute to long-term public health security and strengthen collective preparedness against infectious disease threats. By embedding vaccination within broader frameworks of health equity, social responsibility, and sustainable healthcare infrastructure, policymakers and public health stakeholders can foster a culture of immunization that transcends immediate seasonal concerns and becomes a cornerstone of long-term global health resilience.
Future research should examine how broader sociopolitical, economic, and technological transformations, including digital health communication, misinformation dynamics, global vaccine equity, and the evolving role of public institutions, shape vaccination behaviors over time. Investigating how systemic factors such as climate change, migration patterns, and economic instability impact immunization uptake could provide critical insights into the resilience of public health systems in times of crisis. Expanding TPB frameworks to incorporate habit formation, trust mechanisms, and structural facilitators could enhance their predictive power, offering a more holistic and sustainability-oriented model for fostering long-term immunization behaviors across diverse and transitioning societies.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was approved by the Ashkelon Academic College Ethics Committee (approval #42-2023). All procedures were performed in accordance with the Declaration of Helsinki. The questionnaire was anonymous and voluntary, and the information gathered did not put the participants at risk in any form.
Informed Consent Statement
Informed consent was obtained from all participants.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The author declares no conflict of interest.
References
- Cassini, A.; Colzani, E.; Pini, A.; Mangen, M.J.; Plass, D.; McDonald, S.A.; Maringhini, G.; van Lier, A.; Haagsma, J.A.; Havelaar, A.H.; et al. Impact Of Infectious Diseases on Population Health Using Incidence-Based Disability-Adjusted Life Years (DALYs): Results from The Burden of Communicable Diseases in Europe Study, European Union And European Economic Area Countries, 2009 to 2013. Eurosurveillance 2018, 23, 17–00454. [Google Scholar] [CrossRef] [PubMed]
- Zou, H.; Huang, Y.; Chen, T.; Zhang, L. Influenza vaccine hesitancy and influencing factors among university students in China: A multicenter cross-sectional survey. Ann. Med. 2023, 55, 2195206. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.H.; Lee, H.; Jung, M.; Kim, S.H.; Sung, H.K.; Oh, M.D.; Lee, J.Y. Incidence, Severity, and Mortality of Influenza During 2010–2020 in Korea: A Nationwide Study Based on the Population-Based National Health Insurance Service Database. J. Korean Med. Sci. 2023, 38, e58. [Google Scholar] [CrossRef] [PubMed]
- The Center for Disease Control (CDC). Preliminary Estimated Flu Disease Burden 2023–2024 Flu Season. 2024. Available online: https://www.cdc.gov/flu-burden/php/data-vis/2023-2024.html (accessed on 20 February 2025).
- Israeli Ministry of Health. The Ministry of Health Issues a Weekly Summary of Influenza and RSV in Israel. 2023. Available online: https://www.gov.il/en/pages/09022023_01 (accessed on 17 April 2025).
- The Center for Disease Control (CDC). Flu Vaccination Coverage, United States, 2023–2024 Influenza Season. 2024. Available online: https://www.cdc.gov/fluvaxview/coverage-by-season/2023-2024.html (accessed on 20 February 2025).
- Chotpitayasunondh, T.; Fischer, T.K.; Heraud, J.M.; Hurt, A.C.; Monto, A.S.; Osterhaus, A.; Shu, Y.; Tam, J.S. Influenza and COVID-19: What Does Co-Existence Mean? Inluenza Other Respir. Viruses 2021, 15, 407–412. [Google Scholar] [CrossRef]
- Benjamin, S.M.; Bahr, K.O. Barriers Associated with Seasonal Influenza Vaccination Among College Students. Influenza Res. Treat. 2016, 2016, 4248071. [Google Scholar] [CrossRef]
- Dopelt, K.; Yukther, S.; Shmukler, T.; Abudin, A. Vaccine Hesitancy in Israel: Exploring the Relationships with Vaccination History, Knowledge, and Attitudes towards Influenza Vaccines. Eur. J. Investig. Health Psychol. Educ. 2024, 14, 37–48. [Google Scholar] [CrossRef]
- Uddin, M.; Cherkowski, G.C.; Liu, G.; Zhang, J.; Monto, A.S.; Aiello, A.E. Demographic and Socioeconomic Determinants of Influenza Vaccination Disparities Among University Students. J. Epidemiol. Community Health 2010, 64, 808–813. [Google Scholar] [CrossRef]
- Fall, E.; Izaute, M.; Chakroun-Baggioni, N. How Can the Health Belief Model and Self-Determination Theory Predict Both Influenza Vaccination and Vaccination Intention? A Longitudinal Study Among University Students. Psychol. Health 2018, 33, 746–764. [Google Scholar] [CrossRef]
- Ajzen, I. From Intentions to Actions: A Theory of Planned Behavior. In Action-Control: From Cognition to Behavior; Kuhl, J., Beckman, J., Eds.; Springer: Heidelberg, Germany, 1985; pp. 11–39. [Google Scholar]
- Paul, B.; Kirubakaran, R.; Isaac, R.; Dozier, M.; Grant, L.; Weller, D.; RESPIRE collaboration. Theory of planned behavior-based interventions in chronic diseases among the low health-literacy population: Protocol for a systematic review. Syst. Rev. 2022, 11, 127. [Google Scholar] [CrossRef]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Hum. Decis. Process 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Myers, L.B.; Goodwin, R. Using a Theoretical Framework to Determine Adults’ Intention to Vaccinate Against Pandemic Swine Flu in Priority Groups in the UK. Public Health 2012, 126, S53–S56. [Google Scholar] [CrossRef] [PubMed]
- Chu, H.; Liu, S. Light at the End of The Tunnel: Influence of Vaccine Availability and Vaccination Intention on People’s Consideration of the COVID-19 Vaccine. Soc. Sci. Med. 2021, 286, 114315. [Google Scholar] [CrossRef] [PubMed]
- Kan, T.; Zhang, J. Factors Influencing Seasonal Influenza Vaccination Behavior Among Elderly People: A Systematic Review. Public Health 2018, 156, 67–78. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Hou, Z.; Tu, S.; Liu, M.; Chantler, T.; Larson, H. Factors Influencing Childhood Influenza Vaccination: A Systematic Review. Vaccines 2024, 12, 233. [Google Scholar] [CrossRef]
- Mussetto, I.; Bernucci, M.C.; Kaminska, A.E.; Isonne, C.; Sciurti, A.; Migliara, G.; Renzi, E.; Massimi, A.; Marzuillo, C.; De Vito, C.; et al. Prevalence and Determinants of Vaccination Intention towards Routine Immunizations in University Students: A Systematic Review and Meta-Analysis. BMC Public Health 2025, 25, 1443. [Google Scholar] [CrossRef]
- Liu, C.C.; Ling, J.; Zahry, N.R.; Liu, C.; Ammigan, R.; Kaur, L. Using the Theory of Planned Behavior to Determine COVID-19 Vaccination Intentions and Behavior Among International and Domestic College Students in the United States. PLoS ONE 2024, 19, e0293130. [Google Scholar] [CrossRef]
- Mongeau, P.A.; Liu, Y.; Hashi, E.C.; Roberto, A.J. College Students’ Influenza Vaccine Hesitation: A Reasoned Action Investigation with Quantitative and Qualitative Data. J. Behav. Med. 2023, 46, 65–75. [Google Scholar] [CrossRef]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef]
- Silva, J.; Bratberg, J.; Lemay, V. COVID-19 and influenza vaccine hesitancy among college students. J. Am. Pharm. Assoc. 2021, 61, 709–714.e1. [Google Scholar] [CrossRef]
- Gai, Y. Relationship Between Influenza-Related Experience and Current Vaccination Outcome. BMC Public Health 2025, 25, 174. [Google Scholar] [CrossRef]
- Nichol, K.L.; D’Heilly, S.; Ehlinger, E.P. Influenza vaccination among college and university students: Impact on influenzalike illness, health care use, and impaired school performance. Arch. Pediatr. Adolesc. Med. 2008, 162, 1113–1118. [Google Scholar] [CrossRef] [PubMed]
- Walsh, M.M.; Parker, A.M.; Vardavas, R.; Nowak, S.A.; Kennedy, D.P.; Gidengil, C.A. The Stability of Influenza Vaccination Behavior Over Time: A Longitudinal Analysis of Individuals Across 8 Years. Ann. Behav. Med. 2020, 54, 783–793. [Google Scholar] [CrossRef] [PubMed]
- Gardner, B. A Review and Analysis of The Use Of ‘Habit’ In Understanding, Predicting and Influencing Health-Related Behavior. Health Psychol. Rev. 2015, 9, 277–295. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, P.; Roback, K.; Broström, A.; Ellström, P.E. Creatures of habit: Accounting for the role of habit in implementation research on clinical behavior change. Implement. Sci. 2012, 7, 53. [Google Scholar] [CrossRef]
- May, S.; Roach, M.; Maravic, M.; Mitrovich, R.; Wilson, R.; Prood, N.; Eiden, A.L. Understanding the factors that shape vaccination ecosystem resilience: A qualitative assessment of international expert experiences and perspectives. BMJ Public Health 2024, 2, e000381. [Google Scholar] [CrossRef]
- Pennisi, F.; Genovese, C.; Gianfredi, V. Lessons from the COVID-19 Pandemic: Promoting Vaccination and Public Health Resilience, a Narrative Review. Vaccines 2024, 12, 891. [Google Scholar] [CrossRef]
- Kroese, F.; van den Boom, W.; Buskens, V.; van Empelen, P.; Hulscher, M.; Ruiter, R.A.C.; Timmermans, D.R.M.; de Vries, M.; de Bruin, M.; Lambooij, M. When and Why Do People Change Their Minds in Favor of Vaccination? Longitudinal Analyses of Switching COVID-19 Vaccination Preferences. BMC Public Health 2024, 24, 3392. [Google Scholar] [CrossRef]
- Lièvre, G.; Sicsic, J.; Galmiche, S.; Charmet, T.; Fontanet, A.; Mueller, J. Are Psychological Attitudes Towards Vaccination An Expression Of Personality? A Cross-Sectional Study On COVID-19 Vaccination in France. BMC Public Health 2025, 25, 209. [Google Scholar] [CrossRef]
- Atanasova, S.; Kamin, T.; Perger, N. Predictors of COVID-19 Vaccination Intention and Behavior Among Young People in a European Union Country with Low COVID-19 Vaccination Rates: Cross-Sectional Study. JMIR Public Health Surveill. 2025, 11, e64653. [Google Scholar] [CrossRef]
- Goje, O.; Kapoor, A. Meeting the challenge of vaccine hesitancy. Cleve Clin. J. Med. 2024, 91 (Suppl. S1), S50–S56. [Google Scholar] [CrossRef]
- Dopelt, K.; Abudin, A.; Yukther, S.; Shmukler, T.; Davidovitch, N. The Association between Levels of Trust in the Healthcare System and Influenza Vaccine Hesitancy among College Students in Israel. Vaccines 2023, 11, 1728. [Google Scholar] [CrossRef] [PubMed]
- Jamison, A.M.; Quinn, S.C.; Freimuth, V.S. “You don’t trust a government vaccine”: Narratives of institutional trust and influenza vaccination among African American and white adults. Soc. Sci. Med. 2019, 221, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Larson, H.J.; Clarke, R.M.; Jarrett, C.; Eckersberger, E.; Levine, Z.; Schulz, W.S.; Paterson, P. Measuring trust in vaccination: A systematic review. Hum. Vaccin. Immunother. 2018, 14, 1599–1609. [Google Scholar] [CrossRef] [PubMed]
- Williamson, L.D.; Tarfa, A. Examining the Relationships Between Trust in Providers and Information, Mistrust, and COVID-19 Vaccine Concerns, Necessity, and Intentions. BMC Public Health 2022, 22, 2033. [Google Scholar] [CrossRef]
- Souvatzi, E.; Katsikidou, M.; Arvaniti, A.; Plakias, S.; Tsiakiri, A.; Samakouri, M. Trust in Healthcare, Medical Mistrust, and Health Outcomes in Times of Health Crisis: A Narrative Review. Societies 2024, 14, 269. [Google Scholar] [CrossRef]
- Rogers, C.J.; Bahr, K.O.; Benjamin, S.M. Attitudes and Barriers Associated with Seasonal Influenza Vaccination Uptake Among Public Health Students; A Cross-Sectional Study. BMC Public Health 2018, 18, 1131. [Google Scholar] [CrossRef]
- Skyles, T.J.; Stevens, H.P.; Obray, A.M.; Jensen, J.L.; Miner, D.S.; Bodily, R.J.; Nielson, B.U.; Poole, B.D. Changes in Attitudes and Barriers to Seasonal Influenza Vaccination from 2007 to 2023. J. Community Health 2024, 49, 207–217. [Google Scholar] [CrossRef]
- Shon, E.-J.; Lee, L. Effects of Vaccine Literacy, Health Beliefs, and Flu Vaccination on Perceived Physical Health Status among Under/Graduate Students. Vaccines 2023, 11, 765. [Google Scholar] [CrossRef]
- Shon, E.-J.; Choe, S.; Lee, L.; Ki, Y. Influenza Vaccination Among U.S. College or University Students: A Systematic Review. Am. J. Health Promot. 2021, 35, 708–719. [Google Scholar] [CrossRef]
- Dopelt, K.; Mordehay, N.; Goren, S.; Cohen, A.; Barach, P. “I Believe More in the Ability of the Small Person to Make Big Changes”: Innovation and Social Entrepreneurship to Promote Public Health in Israel. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 1787–1800. [Google Scholar] [CrossRef]
- Hagger, M.S.; Hamilton, K. Progress on Theory of Planned Behavior Research: Advances in Research Synthesis and Agenda for Future Research. J. Behav. Med. 2025, 48, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T.; Chapman, G.B.; Rothman, A.J.; Leask, J.; Kempe, A. Increasing Vaccination: Putting Psychological Science into Action. Psychol. Sci. Public Interest 2017, 18, 149–207. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R. Modeling Health Behavior Change: How to Predict and Modify the Adoption and Maintenance of Health Behaviors. Appl. Psychol. Int. Rev. 2008, 57, 1–29. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).