Analgesic Efficacy of Quadratus Lumborum Block in Infants Undergoing Pyeloplasty
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Related Variables
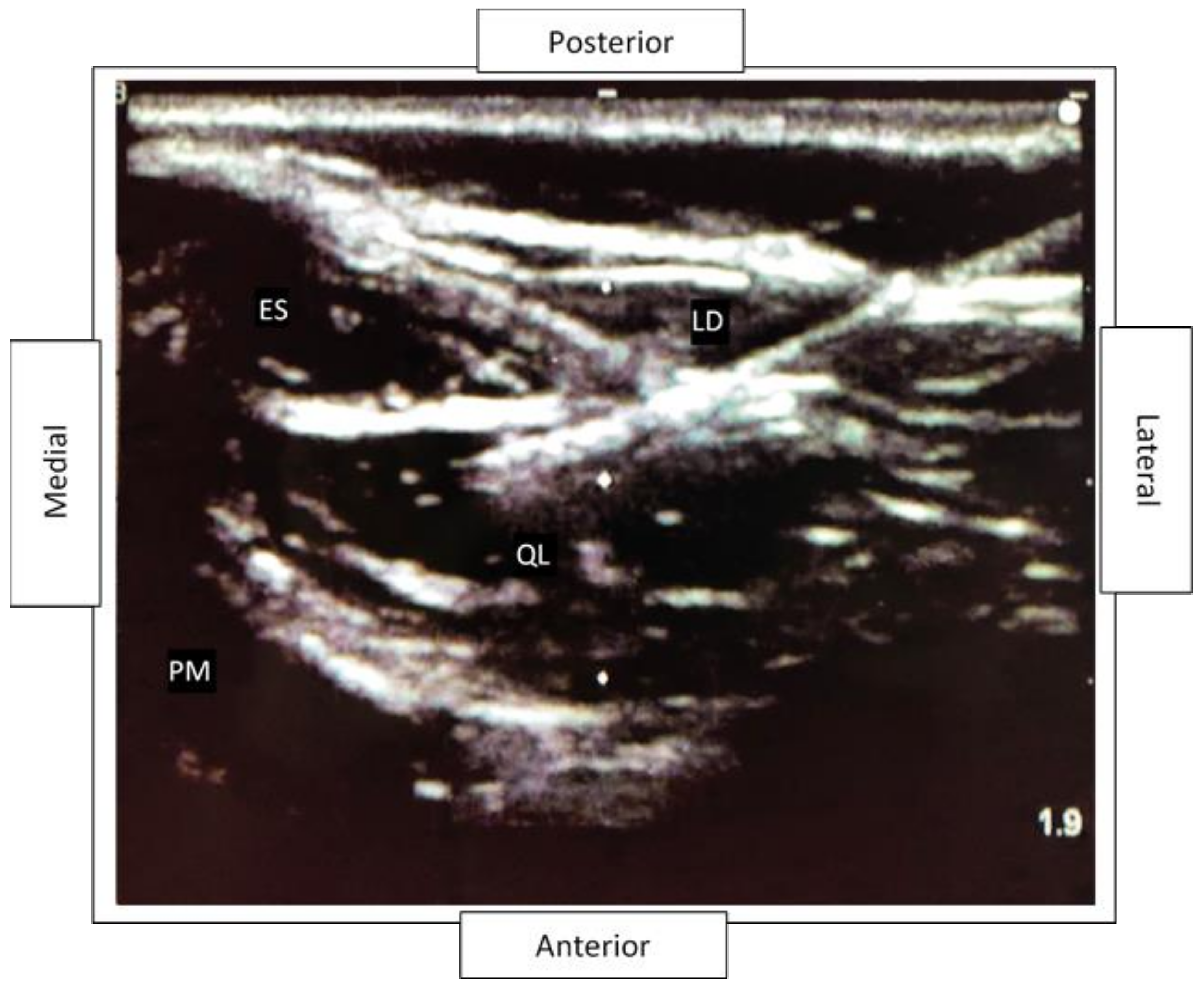
2.2. Quadratus Lumborum Block Details
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rubenwolf, P.; Ziesel, C.; Beetz, R.; Kamal, M.M.; Thüroff, J.W.; Stein, R. Presentation, Management and Long-Term Outcome of Ureteropelvic Junction Obstruction in Duplex Kidneys. J. Urol. 2015, 194, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Krajewski, W.; Wojciechowska, J.; Dembowski, J.; Zdrojowy, R.; Szydełko, T. Hydronephrosis in the course of ureteropelvic junction obstruction: An underestimated problem? Current opinions on the pathogenesis, diagnosis and treatment. Adv. Clin. Exp. Med. Off. Organ Wroc. Med Univ. 2017, 26, 857–864. [Google Scholar] [CrossRef] [Green Version]
- Garimella, V.; Cellini, C. Postoperative pain control. Clin. Colon Rectal Surg. 2013, 26, 191–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Obladen, M. Lethal Lullabies: A History of Opium Use in Infants. J. Hum. Lact. 2016, 32, 75–85. [Google Scholar] [CrossRef]
- Thigpen, J.C.; Odle, B.L.; Harirforoosh, S. Opioids: A Review of Pharmacokinetics and Pharmacodynamics in Neonates, Infants, and Children. Eur. J. Drug Metab. Pharm. 2019, 44, 591–609. [Google Scholar] [CrossRef]
- Desai, A.; Aucott, S.; Frank, K.; Silbert-Flagg, J. Comparing N-PASS and NIPS: Improving Pain Measurement in the Neonate. Adv. Neonatal Care 2018, 18, 260–266. [Google Scholar] [CrossRef]
- Whitaker, E.E.; Wiemann, B.Z.; DaJusta, D.G.; Alpert, S.A.; Ching, C.B.; McLeod, D.J.; Tobias, J.D.; Jayanthi, V.R. Spinal anesthesia for pediatric urological surgery: Reducing the theoretic neurotoxic effects of general anesthesia. J. Pediatr. Urol. 2017, 13, 396–400. [Google Scholar] [CrossRef] [PubMed]
- Jayanthi, V.R.; Spisak, K.; Smith, A.E.; Martin, D.P.; Ching, C.B.; Bhalla, T.; Tobias, J.D.; Whitaker, E. Combined spinal/caudal catheter anesthesia: Extending the boundaries of regional anesthesia for complex pediatric urological surgery. J. Pediatr. Urol. 2019, 15, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Polaner, D.M.; Taenzer, A.H.; Walker, B.J.; Bosenberg, A.; Krane, E.J.; Suresh, S.; Wolf, C.; Martin, L.D. Pediatric Regional Anesthesia Network (PRAN): A multi-institutional study of the use and incidence of complications of pediatric regional anesthesia. Anesth. Analg. 2012, 115, 1353–1364. [Google Scholar] [CrossRef] [Green Version]
- Walter, C.M.; Abbasian, N.; Olbrecht, V.A. Trends in Pediatric Pain: Thinking Beyond Opioids. Anesthesiol. Clin. 2020, 38, 663–678. [Google Scholar] [CrossRef]
- Walker, B.J.; Long, J.B.; Sathyamoorthy, M.; Birstler, J.; Wolf, C.; Bosenberg, A.T.; Flack, S.H.; Krane, E.J.; Sethna, N.F.; Suresh, S.; et al. Complications in Pediatric Regional Anesthesia: An Analysis of More than 100,000 Blocks from the Pediatric Regional Anesthesia Network. Anesthesiology 2018, 129, 721–732. [Google Scholar] [CrossRef] [PubMed]
- Genç Moralar, D.; Tok Cekmecelioglu, B.; Aslan, M.; Hergünsel, G.O. Effect of quadratus lumborum block on postoperative analgesic requirements in pediatric patients: A randomized controlled double-blinded study. Minerva Anestesiol. 2020, 86, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Ivani, G.; DeNegri, P.; Conio, A.; Grossetti, R.; Vitale, P.; Vercellino, C.; Gagliardi, F.; Eksborg, S.; Lonnqvist, P.A. Comparison of racemic bupivacaine, ropivacaine, and levo-bupivacaine for pediatric caudal anesthesia: Effects on postoperative analgesia and motor block. Reg. Anesth. Pain Med. 2002, 27, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Astuto, M.; Disma, N.; Arena, C. Levobupivacaine 0.25% compared with ropivacaine 0.25% by the caudal route in children. Eur. J. Anaesthesiol. 2003, 20, 826–830. [Google Scholar] [CrossRef]
- Ivani, G.; De Negri, P.; Lonnqvist, P.A.; L’Erario, M.; Mossetti, V.; Difilippo, A.; Rosso, F. Caudal anesthesia for minor pediatric surgery: A prospective randomized comparison of ropivacaine 0.2% vs levobupivacaine 0.2%. Paediatr. Anaesth. 2005, 15, 491–494. [Google Scholar] [CrossRef]
- Calculating Morphine Miligram Equivalents (MME). Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf (accessed on 23 June 2021).
- Hadjistavropoulos, T.; Craig, K.D.; Duck, S.; Cano, A.; Goubert, L.; Jackson, P.L.; Mogil, J.S.; Rainville, P.; Sullivan, M.J.L.; Williams, A.C.C.; et al. A biopsychosocial formulation of pain communication. Psychol. Bull. 2011, 137, 910–939. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Öksüz, G.; Bilal, B.; Gürkan, Y.; Urfalioğlu, A.; Arslan, M.; Gişi, G.; Öksüz, H. Quadratus Lumborum Block Versus Transversus Abdominis Plane Block in Children Undergoing Low Abdominal Surgery: A Randomized Controlled Trial. Reg. Anesth. Pain Med. 2017, 42, 674–679. [Google Scholar] [CrossRef]
- Sato, M. Ultrasound-guided quadratus lumborum block compared to caudal ropivacaine/morphine in children undergoing surgery for vesicoureteric reflex. Paediatr. Anaesth. 2019, 29, 738–743. [Google Scholar] [CrossRef]
- Blount, R.L.; Loiselle, K.A. Behavioural assessment of pediatric pain. Pain Res. Manag. 2009, 14, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Suraseranivongse, S.; Kaosaard, R.; Intakong, P.; Pornsiriprasert, S.; Karnchana, Y.; Kaopinpruck, J.; Sangjeen, K. A comparison of postoperative pain scales in neonates. Br. J. Anaesth. 2006, 97, 540–544. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahn, Y.; Kang, H.; Shin, E. Pain assessment using CRIES, FLACC and PIPP in high-risk infants. J. Korean Acad. Nurs. 2005, 35, 1401–1409. [Google Scholar] [CrossRef]
- Verma, A.; Bajpai, M.; Baidya, D.K. Lumbotomy approach for upper urinary tract surgeries in adolescents: Feasibility and challenges. J. Pediatr. Urol. 2014, 10, 1122–1125. [Google Scholar] [CrossRef]
- Hussein, M.M. Ultrasound-guided quadratus lumborum block in pediatrics: Trans-muscular versus intra-muscular approach. J. Anesth. 2018, 32, 850–855. [Google Scholar] [CrossRef] [PubMed]
- Elsharkawy, H.; El-Boghdadly, K.; Kolli, S.; Esa, W.A.S.; DeGrande, S.; Soliman, L.M.; Drake, R.L. Injectate spread following anterior sub-costal and posterior approaches to the quadratus lumborum block: A comparative cadaveric study. Eur. J. Anaesthesiol. 2017, 34, 587–595. [Google Scholar] [CrossRef]
- Hockett, M.M.; Hembrador, S.; Lee, A. Continuous Quadratus Lumborum Block for Postoperative Pain in Total Hip Arthroplasty: A Case Report. A A Case Rep. 2016, 7, 129–131. [Google Scholar] [CrossRef]
- Elsharkawy, H.; El-Boghdadly, K.; Barrington, M. Quadratus Lumborum Block: Anatomical Concepts, Mechanisms, and Techniques. Anesthesiology 2019, 130, 322–335. [Google Scholar] [CrossRef]
- Chakraborty, A.; Goswami, J.; Patro, V. Ultrasound-guided continuous quadratus lumborum block for postoperative analgesia in a pediatric patient. A A Case Rep. 2015, 4, 34–36. [Google Scholar] [CrossRef]
- Jin, Z.; Liu, J.; Li, R.; Gan, T.J.; He, Y.; Lin, J. Single injection Quadratus Lumborum block for postoperative analgesia in adult surgical population: A systematic review and meta-analysis. J. Clin. Anesth. 2020, 62, 109715. [Google Scholar] [CrossRef] [PubMed]
- Menser, C.; Smith, H. Emergence Agitation and Delirium: Considerations for Epidemiology and Routine Monitoring in Pediatric Patients. Local Reg. Anesth. 2020, 13, 73–83. [Google Scholar] [CrossRef]
- Mason, K.P. Paediatric emergence delirium: A comprehensive review and interpretation of the literature. Br. J. Anaesth. 2017, 118, 335–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variables | All | QL Block | Non-QL Block | p-Value |
|---|---|---|---|---|
| (n = 34) | (n = 13) | (n = 21) | ||
| Male, n (%) | 24 (70.6) | 9 (69.2) | 15 (71.4) | 1.0 |
| Age at presentation, mean (SD), months | 6.2 (3.2) | 5.8 (3.2) | 6.4 (3.2) | 0.62 |
| Total OR Time, mean (range), minutes | 256.6 (171–412) | 279.4 (171–412) | 243.6 (171–343) | 0.09 |
| Length of hospital stay, mean (range), days | 2.32 (0–8) | 2.16 (1–5) | 2.42 (0–8) | 0.66 |
| Complications, n (%) | ||||
| Fever | 1 (7.7) | 1 (7.7) | 0 | |
| Emesis | 1 (7.7) | 0 | 1 (7.7) |
| Variables | All | QL Block | Non-QL Block | p-Value |
|---|---|---|---|---|
| (n = 34) | (n = 13) | (n = 21) | ||
| MME Administered, mean (SD) | ||||
| Intraoperatively | 2.0 (1.5) | 1.8 (1.3) | 2.1 (1.7) | 0.68 |
| Postoperatively | 0.9 (1.8) | 0.8 (1.4) | 0.9 (2.0) | 0.82 |
| Discharge a | 26.6 (5.0) | 13.3 (-) | 27.8 (3.2) | 0.14 |
| Acetaminophen- 24 Hours Post-operatively, milligrams, mean (SD) | 184.4 (115.3) | 233.1 (137.0) | 154.2 (90.4) | 0.09 |
| NSAIDs- 24 Hours Post-operatively, milligrams, mean (range) | 49.3(0–390) | 84.0 (0–390) | 25.5 (0–300) | 0.12 |
| Number of Pts. With Discharge Opioid Prescriptions Written, n (%) | 17 (50) | 5 (38) | 12 (57) | 0.29 |
| Number of Written Opioid Prescriptions Filled, n (%) | 13/17 (77) | 1/5 (20) | 12/12 (100) | 0.002 * |
| Variables | All | QL Block | Non-QL Block | p-Value |
|---|---|---|---|---|
| (n = 34) | (n = 13) | (n = 21) | ||
| Pulse, mean (SD) | 135.5 (13.9) | 136.3 (15.9) | 135.0 (13.0) | 0.67 |
| Systolic Blood Pressure, mean (SD) | 108.3 (7.3) | 107.5 (9.7) | 108.8 (5.7) | 0.56 |
| Diastolic Blood Pressure, mean (SD) | 59.0 (4.4) | 59.3 (3.7) | 58.8 (4.8) | 0.86 |
| CRIES Pain Score, mean (SD) a | 1.0 (0.8) | 0.9 (0.8) | 1.1 (0.9) | 0.53 |
| FLACC Pain Score, mean (SD) b | 1.0 (1.1) | 0.8 (0.8) | 1.1 (1.2) | 0.79 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chisolm, P.F.; Singh, N.P.; Cummins, I.; Oster, R.A.; Cox, D.; Dangle, P.P. Analgesic Efficacy of Quadratus Lumborum Block in Infants Undergoing Pyeloplasty. Surgeries 2021, 2, 278-285. https://doi.org/10.3390/surgeries2030028
Chisolm PF, Singh NP, Cummins I, Oster RA, Cox D, Dangle PP. Analgesic Efficacy of Quadratus Lumborum Block in Infants Undergoing Pyeloplasty. Surgeries. 2021; 2(3):278-285. https://doi.org/10.3390/surgeries2030028
Chicago/Turabian StyleChisolm, Paul F., Nikhi P. Singh, Ian Cummins, Robert A. Oster, Damon Cox, and Pankaj P. Dangle. 2021. "Analgesic Efficacy of Quadratus Lumborum Block in Infants Undergoing Pyeloplasty" Surgeries 2, no. 3: 278-285. https://doi.org/10.3390/surgeries2030028
APA StyleChisolm, P. F., Singh, N. P., Cummins, I., Oster, R. A., Cox, D., & Dangle, P. P. (2021). Analgesic Efficacy of Quadratus Lumborum Block in Infants Undergoing Pyeloplasty. Surgeries, 2(3), 278-285. https://doi.org/10.3390/surgeries2030028







